Abstract
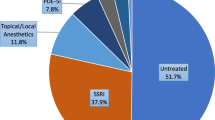
Recently, the ICD-11 for Mortality and Morbidity Statistics (ICD-11-MMS, 2018 Version) has been published with a new definition of premature ejaculation (PE), including a third PE subtype. This definition differs from Diagnostic and Statistical Manual of Mental Disorders (DSM-5) definition of PE. We hereby address the similarities and differences between ICD-11-MMS and DSM-5 definition of PE and call attention to the illogical policy of some European (EU) National Regulatory Agencies to remain with a 1-min cut-off point of ejaculation time for Lifelong, Acquired and Subjective PE. The advantage of ICD-11-MMS is the inclusion of a third PE subtype, which is congruent with Subjective PE. A serious disadvantage of DSM-5 is that a 1-min criterion is used for both Lifelong and Acquired PE, and that a third PE subtype is not mentioned. Despite the incomplete DSM-5 definition of PE, some EU regulatory agencies adhere to a definition of PE which relies only on the 1-min ejaculation time cut-off point of DSM-5, and do not recognize the more recent PE definitions of ICD-11-MMS and International Society for Sexual Medicine. There is no scientific evidence for this illogical position. The continued use of a 1-min cut-off point for all subgroups of PE ignores the existence of Acquired PE (Intravaginal Ejaculation Latency Time (IELT) <3 min) and Subjective PE (IELT <approx. 6 min), both of which have been shown to be clinically and psychologically important. In conclusion, some EU regulatory agencies are not recognizing ongoing developments in the definition of three different subgroups of PE. We propose combining the DSM-5 and ICD-11 MMS definitions to optimize the whole PE spectrum for future registered drug treatment studies, so that it properly reflects patient needs.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Abraham K. Ueber Ejaculatio Praecox. Zeit Aerztl Psychoanal. 1917;4:171–86.
Schapiro B. Premature ejaculation: a review of 1130 cases. J Urol. 1943;50:374–9.
Waldinger MD, Hengeveld MW, Zwinderman AH, Olivier B. An empirical operationalization study of DSM-IV diagnostic criteria for premature ejaculation. Intern. J Psychiatry Clin Pract. 1998;2:287–93.
Waldinger MD, Zwinderman AH, Schweitzer DH, Olivier B. Relevance of methodological design for the interpretation of efficacy of drug treatment of premature ejaculation: a systematic review and meta-analysis. Int J Impot Res. 2004;16:369–81.
McMahon CG, Touma K. Treatment of premature ejaculation with paroxetine hydrochloride. Int J Impot Res. 1999;11:241–5.
Assalian P. Premature ejaculation: Is it really psychogenic? J Sex Educ Ther. 1994;20:1–4.
Waldinger MD. Premature ejaculation: state of the art. Urol Clin N Am. 2007;34:591–9.
World Health Organization. International Classification of Diseases 11th Revision for Mortality and Morbidity Statistics (ICD-11-MMS). The global standard for diagnostic health information. Geneva: World Health Organization; 2018.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5). Washington: American Psychiatric Association; 2013. p. 443–446.
McMahon CG, Althof S, Waldinger MD, Porst H, Dean J, Sharlip I, et al. An evidence-based definition of lifelong premature ejaculation: report of the International Society for Sexual Medicine (ISSM) ad hoc committee for the definition of premature ejaculation. J Sex Med. 2008;5:1590–606.
Serefoglu EC, McMahon CG, Waldinger MD, Althof SE, Shindel A, Adaikan G, et al. An evidence-based unified definition of lifelong and acquired premature ejaculation: report of the second international society for sexual medicine ad hoc committee for the definition of premature ejaculation. J Sex Med. 2014;11:1423–41.
World Health Organization. The ICD-10 classification of mental and behavioural disorders; clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992.
World Health Organization. The ICD-10 classification of mental and behavioural disorders; diagnostic criteria for research. Geneva: World Health Organization; 1993.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (4th edition, Text Revision) (DSM-IV-TR). Washington: American Psychiatric Association; 2000.
Waldinger MD, Schweitzer DH. Changing paradigms from an historical DSM-III and DSM-IV view towards an evidence based definition of premature ejaculation. Part I: Validity of DSM-IV-TR. J Sex Med. 2006;3:682–92.
Waldinger MD, Schweitzer DH. Changing paradigms from an historical DSM-III and DSM-IV view towards an evidence based definition of premature ejaculation. Part II: Proposals for DSM-V and ICD-11. J Sex Med. 2006;3:693–705.
Waldinger MD. Ejaculatio praecox, erectio praecox, and detumescentia praecox as symptoms of a hypertonic state in lifelong premature ejaculation: a new hypothesis. Pharmacol Biochem Behav. 2014;121:189–94.
Serefoglu EC, Yaman O, Cayan S, Asci R, Orhan l, Usta MF, et al. Prevalence of the complaint of ejaculating prematurely and the four premature ejaculation syndromes: results from the Turkish Society of Andrology Sexual Health Survey. J Sex Med. 2011;8:540–8.
Gao J, Zhang X, Su P, et al. Prevalence and factors associated with the complaint of premature ejaculation and the four premature ejaculation syndromes: a large observational study in China. J Sex Med. 2013;10:1874–81.
Serefoglu EC, Cimen HI, Atmaca AF, Balbay MD. The distribution of patients who seek treatment for the complaint of ejaculation prematurely according to the four premature ejaculation syndromes. J Sex Med. 2010;7:810–5.
Zhang X, Gao J, Liu J, Xia J, Hao Z, et al. Distribution and factors associated with four premature ejaculation syndromes in outpatients complaining of ejaculating prematurely. J Sex Med. 2013;10:1603–11.
Waldinger MD. Lifelong premature ejaculation: from authority-based to evidence-based medicine. Br J Urol Int. 2004;93:201–7.
Masters WH, Johnson VE. Premature ejaculation. In: Masters WH, Johnson VE, editors. Human sexual inadequacy. Boston: Little, Brown; 1970. p. 92–115.
Kaplan HS. Chapter 1. The anatomy and physiology of the sexual response. In: Kaplan HS, editor. The new sex therapy. London: Bailliere Tindall; 1974. p. 15–21.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (3rd edition) (DSM-III). Washington: American Psychiatric Association; 1980.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (3rd edition, revised) (DSM-III-R). Washington: American Psychiatric Association; 1987.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (4th edition) (DSM-IV). Washington: American Psychiatric Association; 1994.
Cooper AJ, Magnus RV. A clinical trial of the betablocker propranolol in premature ejaculation. J Psychosom Res. 1984;28:331–6.
World Health Organization. International Classification of Diseases (ICD-9). Manual of the International statistical classification of diseases, injuries, and causes of death. Volume 1. Geneva: World Health Organization; 1977.
World Health Organization. International Classification of Diseases (ICD-9-CM). Manual of the International statistical classification of diseases, 9th revision, clinical modification. Volume 2. Geneva: World Health Organization; 1978.
Vroege JA, Gijs L, Hengeveld MW. Classification of sexual dysfunctions: towards DSM-V and ICD-11. Compr Psychiatry. 1998;39:333–7.
Waldinger MD, Hengeveld MW, Zwinderman AH. Paroxetine treatment of premature ejaculation: a double-blind, randomized, placebo-controlled study. Am J Psychiatry. 1994;151:1377–9.
Waldinger MD, Quinn P, Dilleen M, Mundayat R, Schweitzer DH, Boolell M. A multi-national population survey of intravaginal ejaculation latency time. J Sex Med. 2005;2:492–7.
Waldinger MD, McIntosh J, Schweitzer DH. A five-nation survey to assess the distribution of the intravaginal ejaculatory latency time among the general male population. J Sex Med. 2009;6:2888–95.
Waldinger MD, Schweitzer DH, Olivier B. On-demand SSRI treatment of premature ejaculation: pharmacodynamic limitations for relevant ejaculation delay and consequent solutions. J Sex Med. 2005;2:120–31.
Waldinger MD. Drug treatment options for premature ejaculation. Expert Opin Pharmacother. 2018;19:1077–85.
Olivier B, van Oorschot R, Waldinger MD. Serotonin, serotonergic receptors, selective serotonin reuptake inhibitors and sexual behaviour. Int Clin Psychopharmacol. 1998;13 Suppl 6:S9–S14.
Mondaini N, Fusco F, Cai T, Benemei S, Mirone V, Bartoletti R. Dapoxetine treatment in patients with lifelong premature ejaculation: the reasons of a “Waterloo”. Urology. 2013;82:620–4.
Park HJ, Park NC, Kim TN, Baek SR, Lee KM, Choe S. Discontinuation of dapoxetine treatment in patients with premature ejaculation: a 2-year prospective observational study. Sex Med. 2017;5:99–105.
Waldinger MD, Schweitzer DH, Olivier B. Dapoxetine treatment of premature ejaculation (Letter). Lancet. 2006;368:1869–70.
Waldinger MD, Schweitzer DH. Method and design of drug treatment research of subjective premature ejaculation in men differs from that of lifelong premature ejaculation in males: proposal for a new objective measure (Part 1)
Althof SE, McMahon CG, Waldinger MD, Serefoglu EC, Shindel AW, Adaikan PG, et al. An update of the International Society of Sexual Medicine’s guidelines for the diagnosis and treatment of premature ejaculation (PE). J Sex Med. 2014;11:1392–422.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr Waldinger is an adviser of Emotional Brain B.V. and Sapphire Pharmaceuticals.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Waldinger, M.D., Schweitzer, D.H. Differences between ICD-11 MMS and DSM-5 definition of premature ejaculation: a continuation of historical inadequacies and a source of serious misinterpretation by some European Regulatory Agencies (PART 2). Int J Impot Res 31, 310–318 (2019). https://doi.org/10.1038/s41443-018-0108-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-018-0108-5
This article is cited by
-
Current and emerging treatment options for premature ejaculation
Nature Reviews Urology (2022)
-
Management of premature ejaculation: a clinical guideline from the Italian Society of Andrology and Sexual Medicine (SIAMS)
Journal of Endocrinological Investigation (2021)
-
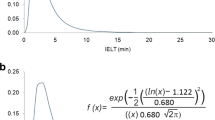
Use of a confirmed mathematical method for back-analysis of IELT distributions: ejaculation time differences between two continents and between continents and men with lifelong premature ejaculation (Part 1)
International Journal of Impotence Research (2019)
-
Men with subjective premature ejaculation have a similar lognormal IELT distribution as men in the general male population and differ mathematically from males with lifelong premature ejaculation after an IELT of 1.5 minutes (Part 2)
International Journal of Impotence Research (2019)