Abstract
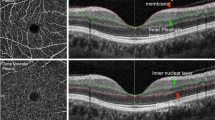
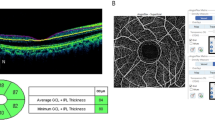
Hypertension is a serious global health problem. Hypertensive retinopathy is generally considered to be a predictor of vascular disease elsewhere in the human body. In the past few decades, a variety of grading systems have been proposed for hypertensive retinopathy. However, these grading systems have some limitations. This study utilized optical coherence tomography angiography (OCTA) to investigate the morphological changes and macular retinal microvasculature in depth among 100 patients with hypertensive retinopathy and 66 healthy participants. Five main pathological changes were discovered in hypertensive retinopathy, as follows: focal capillary sparsity, scattered microangioma, focal macular arch ring defects, focal capillary disorder, and focal capillary nonperfusion at the levels of the superficial and deep vascular networks. In addition, we have found that the number of various pathological changes shows an increasing trend as hypertensive retinopathy progresses and may be related to renal damage. Finally, deep vessel density tended to decrease with progressive stages of hypertensive retinopathy and could be the best indicator to predict the risk of hypertensive retinopathy. Our study, therefore, proposes 3 stages of hypertensive retinopathy without macular edema according to the pathophysiology found by OCTA: stage 1 (only focal capillary sparsity), taking the place of KWB grade I; stage 2 (focal capillary sparsity and scattered microangioma), taking the place of KWB grade II; and stage 3 (focal capillary sparsity, scattered microangioma, focal capillary disorder, and nonperfusion), taking the place of KWB grade III. Hence, OCTA may be a potentially useful tool for evaluating the pathophysiology and staging of hypertensive retinopathy. Further longitudinal prospective studies are needed to confirm our findings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Li D, Lv J, Liu F, Liu P, Yang X, Feng Y, et al. Hypertension burden and control in mainland China: analysis of nationwide data 2003-2012. Int J Cardiol. 2015;184:637–44.
Li Z, Fu C, Yang F, Mao Z. Prevalence and risk factors of hypertension for the middle-aged population in China—results from the China health and retirement longitudinal study (charls). Clin Exp Hypertens. 2019;41:80–86.
Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population-based screening study (China peace million persons project). Lancet. 2017;390:2549–58.
Kolman SA, van Sijl AM, van der Sluijs FA, van de Ree MA. Consideration of hypertensive retinopathy as an important end-organ damage in patients with hypertension. J Hum Hypertens. 2017;31:121–5.
Schmieder RE. Hypertensive retinopathy: a window to vascular remodeling in arterial hypertension. Hypertension. 2008;51:43–44.
Fraser-Bell S, Symes R, Vaze A. Hypertensive eye disease: a review. Clin Exp Ophthalmol. 2017;45:45–53.
Harjasouliha A, Raiji V, Garcia, Gonzalez JM. Review of hypertensive retinopathy. Dis-a-Mon: DM. 2017;63:63–69.
Konstantinidis L, Guex-Crosier Y. Hypertension and the eye. Curr Opin Ophthalmol. 2016;27:514–21.
Aissopou EK, Papathanassiou M, Nasothimiou EG, Konstantonis GD, Tentolouris N, Theodossiadis PG, et al. The Keith-Wagener-Barker and mitchell-wong grading systems for hypertensive retinopathy: association with target organ damage in individuals below 55 years. J Hypertens. 2015;33:2303–9.
Keith NM, Wagener HP, Barker NW. Some different types of essential hypertension: their course and prognosis. Am J Med Sci. 1974;268:336–45.
Ahn SJ, Woo SJ, Park KH. Retinal and choroidal changes with severe hypertension and their association with visual outcome. Investigative Ophthalmol Vis Sci. 2014;55:7775–85.
Kashani AH, Chen CL, Gahm JK, Zheng F, Richter GM, Rosenfeld PJ, et al. Optical coherence tomography angiography: a comprehensive review of current methods and clinical applications. Prog Retinal Eye Res. 2017;60:66–100.
Ang M, Tan ACS, Cheung CMG, Keane PA, Dolz-Marco R, Sng CCA, et al. Optical coherence tomography angiography: a review of current and future clinical applications. Graefe’s Arch Clin Exp Ophthalmol. 2018;256:237–45.
Samara WA, Shahlaee A, Adam MK, Khan MA, Chiang A, Maguire JI, et al. Quantification of diabetic macular ischemia using optical coherence tomography angiography and its relationship with visual acuity. Ophthalmology 2017;124:235–44.
Balaratnasingam C, Inoue M, Ahn S, McCann J, Dhrami-Gavazi E, Yannuzzi LA, et al. Visual acuity is correlated with the area of the foveal avascular zone in diabetic retinopathy and retinal vein occlusion. Ophthalmology. 2016;123:2352–67.
Spaide RF, Klancnik JM Jr., Cooney MJ. Retinal vascular layers imaged by fluorescein angiography and optical coherence tomography angiography. JAMA Ophthalmol. 2015;133:45–50.
Lim HB, Lee MW, Park JH, Kim K, Jo YJ, Kim JY. Changes in ganglion cell-inner plexiform layer thickness and retinal microvasculature in hypertension: an optical coherence tomography angiography study. Am J Ophthalmol. 2019;199:167–76.
Lee WH, Park JH, Won Y, Lee MW, Shin YI, Jo YJ, et al. Retinal microvascular change in hypertension as measured by optical coherence tomography angiography. Sci Rep. 2019;9:156.
Liu LS. Writing Group of Chinese Guidelines for the Management of H. [2010 chinese guidelines for the management of hypertension]. Zhonghua xin xue guan bing za zhi. 2011;39:579–615.
Pilotto E, Frizziero L, Crepaldi A, Della Dora E, Deganello D, Longhin E, et al. Repeatability and reproducibility of foveal avascular zone area measurement on normal eyes by different optical coherence tomography angiography instruments. Ophthalmic Res. 2018;59:206–11.
Penno G, Solini A, Zoppini G, Orsi E, Zerbini G, Trevisan R, et al. Cardiovascular Events Study G. Rate and determinants of association between advanced retinopathy and chronic kidney disease in patients with type 2 diabetes: The renal insufficiency and cardiovascular events (riace) italian multicenter study. Diabetes Care. 2012;35:2317–23.
Tso MO, Jampol LM. Pathophysiology of hypertensive retinopathy. Ophthalmology. 1982;89:1132–45.
Wong TY, Mitchell P. Hypertensive retinopathy. N Engl J Med. 2004;351:2310–7.
Tsai SH, Xie W, Zhao M, Rosa RH Jr, Hein TW, Kuo L. Alterations of ocular hemodynamics impair ophthalmic vascular and neuroretinal function. Am J Pathol. 2018;188:818–27.
Reichhart N, Haase N, Crespo-Garcia S, Skosyrski S, Herrspiegel C, Kociok N, et al. Hypertensive retinopathy in a transgenic angiotensin-based model. Clin Sci. 2016;130:1075–88.
Yu DY, Yu PK, Cringle SJ, Kang MH, Su EN. Functional and morphological characteristics of the retinal and choroidal vasculature. Prog Retinal Eye Res. 2014;40:53–93.
Yu DY, Cringle SJ, Su EN. Intraretinal oxygen distribution in the monkey retina and the response to systemic hyperoxia. Investigative Ophthalmol Vis Sci. 2005;46:4728–33.
Takayama K, Kaneko H, Ito Y, Kataoka K, Iwase T, Yasuma T, et al. Novel classification of early-stage systemic hypertensive changes in human retina based on octa measurement of choriocapillaris. Sci Rep. 2018;8:15163.
Chua J, Chin CWL, Hong J, Chee ML, Le TT, Ting DSW, et al. Impact of hypertension on retinal capillary microvasculature using optical coherence tomographic angiography. J Hypertens. 2019;37:572–80.
Kumagai K, Furukawa M, Suetsugu T, Ogino N. Foveal avascular zone area after internal limiting membrane peeling for epiretinal membrane and macular hole compared with that of fellow eyes and healthy controls. Retina. 2018;38:1786–94.
Dogan B, Akidan M, Erol MK, Coban DT, Suren E. Optical coherence tomography angiography findings in malignant hypertensive retinopathy. Arquivos brasileiros de oftalmologia. 2019;82:72–77.
Lee HM, Lee WH, Kim KN, Jo YJ, Kim JY. Changes in thickness of central macula and retinal nerve fibre layer in severe hypertensive retinopathy: a 1-year longitudinal study. Acta Ophthalmol. 2018;96:e386–92.
Lee SH, Lee WH, Lim HB, Jo YJ, Kim JY Thicknesses of central macular, retinal nerve fiber, and ganglion cell inner plexiform layers in patients with hypertension. Retina. 2018.
Downie LE, Hodgson LA, Dsylva C, McIntosh RL, Rogers SL, Connell P, et al. Hypertensive retinopathy: comparing the Keith-Wagener-Barker to a simplified classification. J Hypertens. 2013;31:960–5.
Wangsa-Wirawan ND, Linsenmeier RA. Retinal oxygen: fundamental and clinical aspects. Arch Ophthalmol. 2003;121:547–57.
Birol G, Wang S, Budzynski E, Wangsa-Wirawan ND, Linsenmeier RA. Oxygen distribution and consumption in the macaque retina. Am J Physiol Heart Circ Physiol. 2007;293:H1696–704.
Wakabayashi T, Sato T, Hara-Ueno C, Fukushima Y, Sayanagi K, Shiraki N, et al. Retinal microvasculature and visual acuity in eyes with branch retinal vein occlusion: Imaging analysis by optical coherence tomography angiography. Investig Ophthalmol Vis Sci. 2017;58:2087–94.
Funding
This research was supported by the Wenzhou Science & Technology Bureau under Grant No. Y20190631 (to YL) and No. Y20180168 (ZJ).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, Y., Li, J., Pan, J. et al. Morphological changes in and quantitative analysis of macular retinal microvasculature by optical coherence tomography angiography in hypertensive retinopathy. Hypertens Res 44, 325–336 (2021). https://doi.org/10.1038/s41440-020-00583-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-020-00583-0
Keywords
This article is cited by
-
Hypertensive eye disease
Nature Reviews Disease Primers (2022)
-
Quantifying the pattern of retinal vascular orientation in diabetic retinopathy using optical coherence tomography angiography
Scientific Reports (2021)