Abstract
A reduced estimated glomerular filtration rate (eGFR) has been described as a predictor of heart failure (HF). However, the increased risk across eGFR categories has not been fully evaluated, which is especially relevant in older individuals in whom both the prevalence of HF and decreased eGFR are higher. Furthermore, this association has not been studied in Mediterranean populations, where coronary heart disease (CHD), a frequent cause of HF, has a low prevalence. We performed a retrospective cohort study using the electronic medical records from primary and hospital settings in northeastern Spain. We included 125,053 individuals ≥60 years old with the determination of creatinine and without diagnosis or previous admission due to HF. The eGFR was calculated according to the CKD-EPI formula and classified by clinical categories. The association between eGFR, as a continuous and categorical variable, and the risk of admission due to HF was assessed by Cox proportional risk analysis, considering death as a competitive risk. During a median follow-up of 38.8 months, 2,176 individuals (1.74%) were hospitalized due to HF. The unadjusted admission rates were 4.02, 13.0, 26.0, and 48.6 per 1000 person-years for eGFR > 60, 45–59, 30–44, and 15–29 ml/min/1.73 m2, respectively. The corresponding hazard ratios (95% confidence interval; reference eGFR 60–89) were 1.38 (95% CI 1.23–1.55), 2.02 (95% CI 1.76–2.32) and 3.46 (95% CI 2.78–4.31). In this Mediterranean community-based cohort of individuals ≥60 years old without previous HF, the risk of admission due to HF gradually increased with decreasing eGFR.
Similar content being viewed by others
Introduction
In individuals with decreased estimated glomerular filtration rate (eGFR), cardiovascular diseases (CVDs) are one of the most frequent complications, with heart failure (HF) being the most prevalent [1, 2]. HF is the leading cause of hospitalization in people over 65 years of age in Spain; the number of admissions due to HF in this age group increased by 26% during the period from 2003 to 2011 [3]. The prevalence of decreased eGFR below 60 ml/min/1.73 m2 and HF increase with age, and represent 29% and 10–20%, respectively, of individuals older than 75 years [3, 4].
Some studies suggest that decreased eGFR is a predictor of the development of HF [5,6,7], and a threefold incidence of HF has been described in individuals with an eGFR < 60 [8]. However, the risk of HF across the clinical categories of eGFR < 60 has not been fully evaluated, which is especially relevant in older individuals, where 95% of individuals present moderately decreased eGFR (30–59 ml/min/1.73 m2) [4], and there is ongoing debate about the clinical significance of this parameter [9, 10]. Furthermore, the association between eGFR and HF has been mainly studied in Anglo-Saxon populations [5,6,7,8, 11], and there are no studies in Mediterranean populations, where coronary heart disease (CHD), a frequent cause of HF, has a lower incidence [12]. In addition, previous studies did not calculate eGFR by using the currently recommended CKD-EPI formula [13, 14].
Given the current trend in population aging and the high prevalence of decreased eGFR in older individuals, the impact on HF risk and the burden on the healthcare system in the coming years are expected to increase.
The objectives of this study were to analyze the risk of first hospital admission due to HF across eGFR categories in individuals ≥60 years old without previous diagnosis of HF in a community-based population from the Mediterranean region.
Methods
Data sources and participants
The present analysis is a part of a larger project that evaluates the association between eGFR and the incidence of cardiovascular events in individuals over 60 years of age. The methodology has been previously published [4], but a concise summary follows. We performed a retrospective study of a community-based cohort using primary care and hospital electronic medical records. We included 130,233 individuals born before 1951 who were registered in 1 of 40 Primary Health Centers in Costa de Ponent Primary Care Service (Catalonia, northeastern Spain) and whose creatinine was measured between 1st January 2010 and 31st December 2011. We excluded individuals with chronic kidney disease stage 5 (eGFR < 15, kidney transplant or on dialysis treatment), those in a home care program and those with less than 30 days of follow-up.
Variables
The creatinine concentration was measured in a centralized laboratory using the standardized Jaffé kinetic method calibrated to an isotope dilution mass spectrometry (IDMS) reference method. We calculated the eGFR using the formula CKD-EPI [13]. The eGFR was classified according to the following clinical categories: 15–29, 30–44, 45–59, 60–89, and 90–119ml/min/1.73 m2) [14].
We also collected data on age, sex, smoking status (nonsmoker, smoker, former smoker), hypercholesterolemia (total cholesterol >6.4 mmol/l or statin treatment), diagnosis of hypertension (HTN, International Classification of Diseases—ICD, 10th revision: I10, I15), diabetes mellitus (DM, ICD10: codes E11, E12, E14), previous cardiovascular disease (CVD, CHD: myocardial infarction [ICD10: I21–I23 and ICD9: 410, 412], angina [ICD10: I20 and ICD9: 411, 413], revascularization [ICD9: 36.0, 36.1], cerebrovascular disease: stroke [ICD10: I61–I64 and ICD9: 433.01, 433.11, 433.21, 433.31, 433.81, 433.91, 434.01, 434.11, 434.91] and transient ischemic attack [ICD10: G45–G46 and ICD9: 435] and peripheral arterial disease [ICD10: I70, I73, I74, and ICD9: 440.2X, 440.3, 443.9]), atrial fibrillation (ICD10: I48), and drugs acting on the renin–angiotensin system (DRAS: angiotensin-converting enzyme inhibitors, angiotensin II receptor antagonists and direct renin inhibitors). Data on diuretic drugs were not available.
We considered the date of the first creatinine determination during the inclusion period as the index date. Baseline characteristics were those registered from the previous year to 1 month after the index date.
For this analysis, individuals with a previous diagnosis or admission due to HF were excluded.
Outcomes
We considered the primary endpoint as the first hospital admission due to HF as the main diagnosis registered in the hospital admission database (ICD9-CM codes: 402.01, 402.11, 402.91, 404.01, 404.11, 404.91, 404.03, 404.13, 404.93, and 428.xx). Individuals were followed up from 1 month after the index date until admission due to HF, death, transfer, or end of the study (December 31, 2013). All-cause mortality data were obtained from hospital and administrative records without specifying the cause.
Statistical analysis
We performed a descriptive analysis. Continuous variables were summarized as the mean and standard deviation or as the median and interquartile range when their distribution departed from normal and categorical variables as absolute and relative frequencies. To evaluate differences in continuous variables between eGFR groups, we used Student’s t or Kruskal–Wallis tests with normal and nonnormal distributions, respectively. We used the chi square test to examine differences in categorical variables between eGFR groups. We also performed linear trend tests through eGFR categories.
Due to the low number of subjects with eGFR ≥ 120 (n = 14) and the diminished precision of estimates over this point, we excluded these individuals from further analyses.
The cumulative incidence of HF admissions per 1000 person-year was calculated in eGFR ≥ 60 and eGFR < 60 groups according to KDIGO 2012 clinical categories [14].
We evaluated the association between eGFR, as a continuous and categorical variable, and the risk of admission due to HF was calculated with the Cox proportional hazards model using competitive risk techniques (Fine-Gray) to consider the possible effect of death in estimating the risk of admission. We defined eGFR = 80 as a reference because this value represents the median eGFR of the population and was classified in the 60–90 clinical category because it included the largest number of individuals; notably, this values were clinically relevant [4]. The models were adjusted for the relevant available variables according to the literature review: age, sex, smoking, hypercholesterolemia, DM, HTN, previous CVD, and atrial fibrillation. A further adjustment was performed with DRAS treatment.
The assumption of proportionality of risk over time was evaluated using Schoenfeld residuals for the exposure variable (eGFR).
Several sensitivity analyses were performed. The use of administrative data to identify HF patients may lead to some misdiagnosis, and accurate adjudication of cause-specific hospitalization is difficult. Therefore, the main analysis was repeated, including HF hospital codes in primary and secondary positions [15]. Then, we excluded individuals with HF risk factors (DM, HTN, and CVD) [16] to evaluate the impact of eGFR on individuals with lower risk of HF. Finally, we excluded individuals with DM to evaluate the possible effects of hypoglycemic drugs on glomerular function [17].
Results
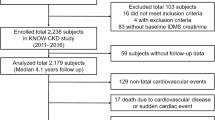
Of the 130,233 individuals included in the cohort [4], we excluded those with a diagnosis or previous admission due to HF (n = 5,166) and individuals with eGFR ≥ 120 (n = 14). The 125,053 individuals finally included had a median age of 70 years [interquartile range: 64.0; 76.0], and 56% were women (Table 1). The overall prevalence of eGFR 15–59 ml/min/1.73 m2 was 12.5%, reaching 27.5% in individuals ≥75 years old; most of these individuals (71.5%) had moderate renal dysfunction (eGFR 45–59). The prevalence of cardiovascular risk factors in the cohort at baseline was high: 61.0% of individuals had HTN, 23.9% had DM, 50.1% had hypercholesterolemia, 14.8% were diagnosed with CVD and 49.3% were under treatment with DRAS. The prevalence of risk factors and cardiovascular comorbidity increased significantly with decreasing eGFR.
During follow-up (median 38.8 months [1–48.7]), 1.74% of individuals (n = 2,176) were admitted due to HF, and 4.40% (n = 5,503) died.
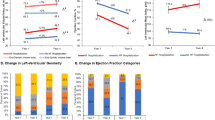
The association between eGFR and the risk of HF admission was first analyzed as a continuous variable (Fig. 1). The risk increased significantly and gradually from eGFR 60 (adjusted hazard ratio-HR- point estimate 1.16; confidence interval-CI- 95% 1.04–1.29) to eGFR 15 (HR 4.90; 95% CI 3.34–7.18). The unadjusted admission rates for those with eGFR > 60 and eGFR < 60 were 4.02 and 17.4 per 1,000 person-years, respectively (Table 2). This rate increased with the severity of renal dysfunction from 12.97/1,000 person-years in eGFR 45–59 to 48.62/1,000 person-years in eGFR 15–29. The adjusted risk of hospital admission is shown in Table 3 (see Supplementary Table 1 for nonadjusted analysis). The HR for eGFR clinical categories were 1.38 (95% CI 1.23–1.55), 2.02 (95% CI 1.76–2.32), and 3.46 (95% CI 2.78–4.31) for eGFR 45–59, 30–44, and 15–29 ml/min/1.73 m2 respectively. These values were comparable to the corresponding HR for HTN (1.46; CI 95% 1.31–1.63), DM (1.92; CI 95% 1.76–2.09) or established CVD (1.82; CI 95% 1.65–2.00). The cumulative incidence of HF admission according to eGFR clinical categories is shown in Fig. 2. The model was not substantially modified when the treatment variable (DRAS) was added (Supplementary Table 2).
Association between estimated glomerular filtration rate (eGFR), as a continuous variable, and the risk of admission due to heart failure. Global p-value global <0.001. Adjusted hazard ratio (HR) point estimation (95% confidence interval) at an eGFR = 60 (reference eGFR 80): eGFR = 15 4.90 (3.34–7.18), eGFR = 30 2.80 (2.40–3.27), eGFR = 45 1.72 (1.52–1.95), eGFR = 60 1.16 (1.04–1.29). Adjusted for age, sex, smoking status, hypertension, diabetes mellitus, hypercholesterolemia, cardiovascular disease, and atrial fibrillation
The sensitivity analyses showed similar results (Supplementary Tables 3–5).
Discussion
In this community cohort of individuals ≥60 years old without previous HF diagnosis in a region with low incidence of CHD, the risk of admission due to HF increased gradually with decreasing eGFR, independent of other risk factors, even in individuals with the mild-moderate and more prevalent disease stage (eGFR 45–59). The magnitude of risk was comparable with that of other well-known risk factors, such as HTN, DM, or other CVDs [16].
The association between eGFR < 60 and hospital admission for HF in individuals with a prior diagnosis of HF is clearly established [18]. In a recent study in a general population including individuals with HF [19], the risk of HF admission increased gradually with decreasing eGFR and the presence of albuminuria.
However, there are few studies analyzing this risk across eGFR categories in individuals without a prior diagnosis of HF [20]. In population-based studies performed in the United States, creatinine elevation [5, 21] and decreased creatinine clearance [6] were associated with an increased risk of HF admission up to 40%. The attributable risk of creatinine > 1.4 mg/dl was 6.3% in individuals over 65 years of age [21]. Kottgen et al. [8] described an overall adjusted relative hazard of developing HF of 1.94 (CI 95% 1.49–2.53) for individuals 45–64 years old with eGFR < 60, which, however, was not confirmed in Caucasians aged 70–79 years [22]. The effect across clinical categories of eGFR < 60 was not analyzed in these studies. The Physicians Health Study [7], which included only men, reported a 2.5 times higher risk of HF in eGFR 45–59 with respect to eGFR ≥ 60. The risk of HF was not statistically significant in individuals with eGFR < 45, perhaps due to the low number of individuals in this category.
To our knowledge, this study is the first to assess the risk of incident HF across eGFR categories in individuals from a Mediterranean population with a low incidence of CHD, which has been described as the main etiologic factor (>50%) in patients with incident HF [23]. The unadjusted rate of HF admission in individuals with eGFR < 60 was 17.4, which was lower than the rate described in the recently published three Communities Study (22.0; 95% CI 19.3–24.8) in an Anglo-Saxon population [24]. In addition to the incidence of CHD, other factors can explain these differences, such as the design of the study, the inclusion of a nonwhite population with a higher risk race and an earlier study period. Despite these results, the difference in risks between individuals with and without an eGFR < 60 is similar (13%), which suggests a comparable eGFR attributable risk in both populations.
The results update and confirm the importance of an eGFR < 60 in the incidence of HF using the recommended CKD-EPI formula and add relevant information regarding the gradual relationship between decreased eGFR and the risk of HF admission. The magnitude of the risk was already evident in the mild-moderate population (eGFR 45–59), which represented 71.5% of individuals with decreased eGFR; the risk increased gradually across eGFR clinical categories, and doubled in the moderate–severe category (eGFR 30–44).
The risk of developing HF throughout life has been calculated as 26% [25]. In individuals ≥65 years old, the risk of admission due to HF is higher than that for CHD or stroke [24]. Clinical practice guidelines recognize the importance of classical cardiovascular risk factors in the development of HF [16, 26]. In the population study, the risk of admission associated with eGFR 45–59 was similar to that of HTN, while the risk of admission associated with eGFR 30–44 was equivalent to that of DM or previous CVD, which are all recognized as important risk factors in the development of HF. Similar to previous studies, this increased risk was maintained after the exclusion of individuals with DM, HTN, and CVD [7].
The role of renal dysfunction in the pathophysiology of HF remains a matter of debate. Renal dysfunction has been associated with an increased incidence of both reduced [27] and preserved ejection fraction (PEF) HF [28]. Renal dysfunction has also been associated with volume overload, which generally accompanies HF with PEF in older individuals [29]. In this study, the HF type was not available, but the characteristics of the population (predominance of elderly women and HTN) suggest a high proportion of HF with PEF, which is the more prevalent HF type in primary care [30].
As strengths of the study, we highlight the large number of individuals included, representative of the population attended in primary care. In addition, the determination of creatinine was performed according to the method standardized to IDMS and in a single centralized laboratory, which further reduces variability. Finally, the eGFR was calculated using the currently recommended CKD-EPI formula [13, 14].
However, some limitations must be mentioned. Although inclusion bias cannot be completely excluded, we believe that it is not important, as 93.1% of individuals ≥60 years of age assigned to the Costa de Ponent health centers were attended during the study period. In addition, eligible individuals represented 73% of these individuals, and there were no differences in age and sex compared with noneligible individuals [4]. Second, the eGFR category was assigned with a single creatinine determination, which, due to regression to the mean, could underestimate the effect. Moreover, eGFR was estimated from serum creatinine using the CKD-EPI formula. Although creatinine-based estimation has limitations [13], and other formulas have been proposed in older individuals, this formula is the usual method in clinical settings and the currently recommended formula [14]. Third, data on albuminuria were not available, and we were unable to evaluate its effect on HF admission risk. However, eGFR and albumin have shown independent prognostic implications [14], and the results add valuable information about the effect of eGFR. Fourth, comorbidity baseline data were obtained from primary care electronic medical records, and some infraregistration can exist. However, CVD data have better quality than those for other pathologies and showed validity in epidemiological studies in our area [31, 32]. Published studies suggest that controlling blood glucose levels with some newer drugs can improve glomerular function in DM [17]. A sensitivity analysis excluding individuals with diabetes was performed with similar results. Fifth, the use of administrative data to identify HF patients may lead to misdiagnosis, and the decision for hospitalization can differ depending on facilities and physicians. The present study was performed in a region with a health department that provides public universal healthcare coverage to all residents. The identification of new cases of HF was based on hospital admissions, which more reliably identifies new diagnoses of HF and more severe cases, although this parameter may underestimate the total incidence of HF. HF codes in administrative databases have been shown to be highly predictive of true HF cases [15]. Accurate adjudication of cause-specific hospitalization is difficult, and studies in administrative databases suggest that hospitalizations with HF diagnosis in primary diagnostic positions are decreasing, while those with HF coding in secondary diagnostic positions are increasing [15]. The main analysis was repeated, including HF hospital codes in primary and secondary positions, which did not modify the main results. Finally, other covariates that may interfere with eGFR determination and be associated with the outcome, such as infections and other clinical events, socioeconomic level or drugs with possible renal effect less frequently used in individuals without HF (e.g., spironolactone), were not available. To reduce this effect, we excluded individuals with <30 days of follow-up, and although some residual confounding may exist, this effect would be minimized by the large sample size.
Despite these limitations, we believe that the study provides relevant data on the relationship between decreased eGFR and HF incidence in individuals ≥60 years.
Conclusions
In this community cohort of individuals ≥60 years old without prior diagnosis of HF from a Mediterranean area with low incidence of coronary disease, the risk of admission for HF increased independently and gradually with decreasing eGFR, even at the more moderate and frequent stages of renal dysfunction.
These results highlight the importance of eGFR, which is easily available in primary care, as a risk factor for the development of HF equivalent to other well-recognized risk factors, such as HTN, DM, or previous CVD. In clinical practice, it is therefore important to identify individuals with decreased eGFR to prioritize the control of other risk factors for the onset of HF.
Although the association between the eGFR and HF is clear, more studies are needed to address its specific role in the development of HF and to determine its value to predict the risk of developing HF.
References
Segall L, Nistor I, Covic A. Heart failure in patients with chronic kidney disease: a systematic integrative review. Biomed Res Int. 2014;2014:937398.
Martínez-Gallardo R, Ferreira-Morong F, García-Pino G, Cerezo-Arias I, Hernández-Gallego R, Caravaca F. Congestive heart failure in patients with advanced chronic kidney disease: association with pre-emptive vascular access placement. Nefrologia. 2012;32:206–12.
Sayago-Silva I, García-López F, Segovia-Cubero J. Epidemiology of heart failure in Spain over the last 20 years. Rev Esp Cardiol. 2013;66:649–56.
Salvador-González B, Gil-Terrón N, Cerain-Herrero M, Subirana I, Güell-Miró R, Rodriguez-Latre L, et al. Estimated glomerular filtration rate, cardiovascular events and mortality across age groups among individuals over 60 years of age in Southern Europe. Rev Esp Cardiol. 2018;71:450–7.
Fried LF, Shlipak MG, Crump C, Bleyer AJ, Gottdiener JS, Kronmal RA, et al. Renal insufficiency as a predictor of cardiovascular outcomes and mortality in elderly individuals. J Am Coll Cardiol. 2003;41:1364–72.
Chae CU, Albert CM, Glynn RJ, Guralnik JM, Curhan GC. Mild renal insufficiency and risk of congestive heart failure in men and women >70 Years of Age. Am J Cardiol. 2003;92:682–6.
Dhingra R, Gaziano JM, Djoussé L. Chronic kidney disease and the risk of heart failure in men. Circ Heart Fail. 2011;4:138–44.
Kottgen A, Russell SD, Loehr LR, Crainiceanu CM, Rosamond WD, Chang PP, et al. Reduced kidney function as a risk factor for incident heart failure: the atherosclerosis risk in communities (ARIC) study. JASN. 2007;18:1307–15.
Levey AS, Inker LA, Coresh J. Chronic kidney disease in older people. JAMA. 2015;314:557–8.
Glassock RJ, Delanaye P, El-Nahas M. An age-calibrated classification of chronic kidney disease. JAMA. 2015;314:559–60.
Chirinos JA, Khan AM, Bansal N, Dries DL, Feldman HI, Ford V, et al. CRIC study investigators. arterial stiffness, central pressures and incident hospitalized heart failure in the chronic renal insufficiency cohort (CRIC) study. Circ Heart Fail. 2014;7:709–16.
Piepoli M, Hoes A, Agewall S, Albus C, Brotons C, Catapano A, et al. ESC Scientific Document Group. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and other societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J. 2016;37:2315–81.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:4.
McCormick N, Lacaille D, Bhole V, Avina-Zubieta JA. Validity of heart failure diagnoses in administrative databases: a systematic review and meta-analysis. PLoS ONE. 2014;9(Aug):e104519.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure. A report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Circulation. 2013;128:e240–327.
Prischl FC, Wanner C. Renal outcomes of antidiabetic treatment options for type 2 diabetes. Kidney Int Rep. 2018;3:1030–8.
Damman K, Valente MAE, Voors AA, O’Connor CM, Van Veldhuisen DJ, Hillege HL. Renal impairment, worsening renal function, and outcome in patients with heart failure: an updated meta-analysis. Eur Heart J. 2014;35:455–69.
Wiebe N, Klarenbach SW, Allan GM, Manns BJ, Pelletier R, James MT, et al. Alberta kidney disease network. potentially preventable hospitalization as a complication of CKD: a cohort study. Am J Kidney Dis. 2014;642:230–8.
Ärnlöv J. Diminished renal function and the incidence of heart failure. Curr Cardilogy Rev. 2009;5:223–7.
Gottdiener JS, Arnold AM, Aurigemma GP, Polak JF, Tracy RP, Kitzman DW, et al. Predictors of congestive heart failure in the elderly: the cardiovascular health study. J Am Coll Cardiol. 2000;35:1628–37.
Kalogeropoulos A. Epidemiology of incident heart failure in a contemporary elderly cohort. the health, aging, and body composition study. Arch Intern Med. 2009;169:708.
Flaherty JD, Bax JJ, De Luca L, Rossi JS, Davidson CJ, Filippatos G, et al. Acute Heart Failure Syndromes International Working Group. Acute heart failure syndromes in patients with coronary artery disease early assessment and treatment. J Am Coll Cardiol. 2009;53:254–63.
Bansal N, Katz R, Robinson-Cohen C, Odden MC, Dalrymple L, Shlipak MG, et al. Absolute rates of heart failure, coronary heart disease and stroke in chronic kidney disease. an analysis of 3 community-based cohort studies. JAMA Cardiol. 2017;2:314–8.
Folsom AR, Shah AM, Lutsey PL, Roetker NS, Alonso A, Avery CL, et al. American Heart Association’s Life’s Simple 7: avoiding heart failure and preserving cardiac structure and function. Am J Med. 2015;128:970–6.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Rev Esp Cardiol. 2016;69:1167.
Moran A, Katz R, Smith NL, Fried LF, Sarnak MJ, Seliger SL, et al. Cystatin C concentration as a predictor of systolic and diastolyc heart failure. J Card Fail. 2008;14:19–26.
Brouwers FP, de Boer RA, van der Harst P, Voors AA, Gansevoort RT, Bakker SJ, et al. Incidence and epidemiology of new onset heart failure with preserved vs. reduced ejection fraction in a community-based cohort: 11-year follow-up of PREVEND. Eur Heart J. 2013;34:1424–31.
Fang JC. Heart failure with preserved ejection fraction. Circulation. 2016;134:435–7.
Andrea R, Falces C, Sanchis L, Sitges M, Heras M, Brugada J. Diagnosis of heart failure with preserved or reduced ejection fraction in a one-stop clinic. Aten Prima. 2013;45:184–92.
Violán C, Foguet-Boreu Q, Hermosilla-Pérez E, Valderas JM, Bolíbar B, Fàbregas-Escurriola M, et al. Comparison of the information provided by electronic health records data and a population health survey to estimate prevalence of selected health conditions and multimorbidity. BMC Public Health. 2013;13:251.
Ramos R, Balló E, Marrugat J, Elosua R, Sala J, Grau M, et al. Validity for use in research on vascular diseases of the SIDIAP (information system for the development of research in primary care): the EMMA study. Rev Esp Cardiol. 2012;65:29–37.
Acknowledgements
We would like to thank the members of the MACAP Renal Costa Ponent Research Group: Virtudes Álvarez-Funes, Eva Alonso-Bes, Esther Freixes-Villaró, Roser Güell-Miró, Laura Ruipérez-Guijarro and Maria Soler-Vila and the Institut Universitari d’Investigació en Atenció Primària Jordi Gol (IDIAP Jordi Gol), Barcelona, Spain.
Funding
This work was supported by a research grant from the Carlos III Institute of Health, Ministry of Economy and Competitiveness (Spain), awarded under the 2011 call of the Health Strategy Action, within the National Research Program oriented to Societal Challenges. This program is part of the Technical, Scientific and Innovation Research National Plan 2008–2011, co-funded with European Union ERDF funds (European Regional Development Fund) (PI11/02220). MG was funded by a Miguel Servet Grant (Carlos III Institute of Health, Ministry of Economy and Competitiveness (Spain)) (PI17/00012). IRD was funded by the Departament de Salut from the Catalan Government through a contract from the Acció instrumental d’incorporació de científics i tecnòlegs (SLT006/17/00029).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MC-A collaborates with RTI Health Solutions, an independent nonprofit research organization that works for government agencies and pharmaceutical companies. No other conflict of interest are declared.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Alcober-Morte, L., Barrio-Ruiz, C., Parellada-Esquius, N. et al. Heart failure admission across glomerular filtration rate categories in a community cohort of 125,053 individuals over 60 years of age. Hypertens Res 42, 2013–2020 (2019). https://doi.org/10.1038/s41440-019-0315-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0315-6
Keywords
This article is cited by
-
American Indian chronic Renal insufficiency cohort study (AI-CRIC study)
BMC Nephrology (2020)
-
Association between the number of hospital admissions and in-hospital outcomes in patients with heart failure
Hypertension Research (2020)