Abstract
High-sensitivity C-reactive protein (hsCRP), a marker of inflammation, can promote atherosclerosis and predict cardiovascular events. However, no data are currently available about the combined effects of hsCRP and hypertension on cardiovascular risk. This study sought to elucidate this matter. A total of 7325 consecutive patients with angina-like chest pain undergoing coronary angiography were evaluated, and 4291 patients with stable, newly diagnosed coronary artery disease (CAD) were enrolled. They were subdivided into three groups according to baseline hsCRP levels (<1, 1–3, and >3 mg/L) and further stratified by hypertension status. The severity of CAD was assessed by the Gensini score and number of diseased vessels. All participants were followed for the occurrence of cardiovascular events. The coronary severity and cardiovascular outcomes were compared among these groups. We observed 530 (12.35%) incident cardiovascular events over 14,210 person-years. Elevated hsCRP was associated with more severe coronary lesions (p < 0.05) and an elevated but nonsignificant increased risk of cardiovascular events (p > 0.05). When hypertension was included as a stratifying factor, both patients with high hsCRP and normal blood pressure and hypertensive patients with any level of hsCRP had more severe coronary lesions compared with the reference group with low hsCRP and normotension. However, compared with the reference group, the cardiovascular event risk was only significantly elevated in patients with high hsCRP and hypertension (p < 0.05). The combination of elevated hsCRP and hypertension greatly increased the cardiovascular risk in patients with stable, newly diagnosed CAD, supporting that hsCRP could be treated as a marker for stratification in high-risk patients.
Similar content being viewed by others
Introduction
Inflammation plays an important role in the initiation and progression of atherosclerosis [1, 2]. Along with the recent publications of several large-scale clinical trials results [3,4,5,6], the contribution of inflammation to cardiovascular risk has again sparked great interest in the cardiovascular field. Among the numerous inflammatory biomarkers that have been studied, high-sensitivity C-reactive protein (hsCRP) has emerged as a leading biomarker for predicting cardiovascular risk [2, 7]. Meanwhile, it has gained the most attention for its use in screening and risk reclassification [8].
However, in the epidemiological studies examining the correlation between hsCRP and adverse cardiovascular outcomes, the data in various populations or different clinical settings has been inconsistent [7, 9,10,11,12,13]. Moreover, whether the measurement of hsCRP concentrations consistently provides clinically meaningful elevated predictive values regarding risk and reclassification beyond conventional risk factors also remains disputed [8]. A clear consensus regarding the optimal clinical use of hsCRP is lacking, despite the publication of guidelines on the use of hsCRP in cardiovascular risk prediction by several leading professional organizations [8]. Thus, it is worth further exploring how to make better and more appropriate use of hsCRP for cardiovascular disease (CVD) risk prediction in clinical practice.
To date, some studies have been conducted to determine the association between hsCRP and cardiovascular events with the consideration of the effects of diabetes mellitus [7, 10], cholesterol [3, 14, 15], and so on. Nevertheless, to the best of our knowledge, excepting a report of the association between hsCRP and stroke stratified by hypertension status among men [13], there have been no studies to detect the combined effect of elevated hsCRP and hypertension on cardiovascular risk. Therefore, we carried out this prospective study in a large cohort of stable, newly diagnosed CAD patients aiming to clarify whether there is a positive synergistic effect between hsCRP and hypertension on coronary severity and cardiovascular outcomes.
Methods
The data that support the findings of this study are available from the corresponding author on reasonable request.
Study design and population
This study complied with the Declaration of Helsinki and Title 45, US Code of Federal Regulations, Part 46, Protection of Human Subjects, Revised November 13, 2001, effective December 13, 2001, and it was approved by the hospital’s ethics review board (Fu Wai Hospital & National Center for Cardiovascular Diseases, Beijing, China). Each participant provided written, informed consent before enrollment.
From March 2011 to September 2016, 7369 consecutive Chinese patients undergoing coronary angiography because of angina-like chest pain or a positive treadmill exercise test or significant stenosis indicated by coronary computed tomography angiography were considered for inclusion in this study. On admission, 44 patients declined to participate. Furthermore, based on elevated myocardial enzyme levels (cardiac troponin I [cTnI], creatine kinase [CK], and creatine kinase isoenzyme [CK-MB]), typical ECG changes, positive findings by coronary angiography, and medical history, 802 non-CAD patients and 2018 CAD patients who had acute coronary syndrome, previous percutaneous coronary intervention, coronary artery bypass grafting, or myocardial infarction were excluded. Next, 184 patients were excluded on the basis of the exclusion criteria as described in our previous study [16, 17]: missing detailed laboratory data; unstable hemodynamic status; uncontrolled decompensated heart failure; infectious or systematic inflammatory disease; severe liver or renal dysfunction; and thyroid dysfunction or malignant disease. During the study period, 30 patients were lost to follow-up. Therefore, a total of 4291 subjects with stable, newly diagnosed CAD were included in the final analysis. Patients were divided into three groups according to the Centers for Disease Control (CDC) and the American Heart Association (AHA) recommended hsCRP cutoff points (<1, 1–3, >3 mg/L; Fig. 1) [18] and hsCRP tertiles. Then, they were further stratified by the presence or absence of hypertension. The enrolled CAD patients were assigned to take optimal medical treatment or combined percutaneous coronary intervention/coronary artery bypass grafting and medical treatment.
Measurements, biochemical analysis, and clinical assessment
At the baseline, information on demographic factors, personal health habits, medication use, and medical history was collected from each participant through a personal interview. Anthropometric measurements were taken, and blood pressure (BP, first and fifth Korotkoff sounds) was measured three times consecutively in the first 3 days using a standard mercury sphygmomanometer by trained physicians, as stated in our previous study [17]. An appropriately sized cuff was selected after measuring each participant’s arm circumference. Subjects needed to sit for 5 min with their arm resting on the desk before the first measurement. There was a 30-s rest between BP measurements. The average of the 2nd and 3rd BP measurements of the 3 days was used in the final analysis.
Blood samples for the measurement of hsCRP and other biomarkers were collected from each patient into ethylene diamine tetraacetic acid (EDTA)-containing tubes in the morning after at least 12 h of fasting. After centrifugation at 3000 rpm for 15 min at 4 °C, all plasma samples were stored in our laboratory at −80 °C and were not thawed until use. The concentrations of hsCRP were determined twice using immunoturbidimetry (Beckmann Assay 360, Bera, Calif., USA), and the mean value was used in the final analysis. Lipid profiles of total cholesterol (TC), triglycerides, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), etc. were measured using an automatic biochemistry analyzer (Hitachi 7150, Tokyo, Japan) and enzymatic assay. The other relevant biomarkers were analyzed by standard commercial kits.
The traditional risk factors were defined as follows. Hypertension was defined as repeated BP measurements ≥140/90 mmHg or self-reported hypertension and currently taking anti-hypertensive drugs. Diabetes Mellitus (DM) was defined as a fasting plasma glucose level ≥7 mmol/L (126 mg/dL), or a 2-h plasma glucose level on the oral glucose tolerance test ≥11.0 mmol/L (200 mg/dL), or a glycosylated hemoglobin level ≥6.5%, or currently using hypoglycemic medications. Body mass index was calculated as weight (kg) divided by height (m) squared. Smoking was defined as subjects who had smoked regularly within the previous 12 months. Statin use was defined as taking moderate-intensity or high-intensity statins at least 3 months prior to admission.
Evaluation of CAD severity
All subjects received coronary angiography at baseline, and angiographic data were collected from catheter laboratory records by three interventional cardiologists. The coronary severity was evaluated by calculating the number of total vessels with lesions and the Gensini score (GS) according to our previous study [17]. The GS was calculated by assigning a severity score to each coronary lesion according to the degree of luminal narrowing and the importance of the location, and the total score equaled the sum of the severity score times the location score for all diseased segments [19].
Follow-up
After the initial appointment, all patients were actively followed-up at 6-month intervals through telephone communications and/or face-to-face interviews after discharge by well-trained cardiologists or nurses who were blinded to the aim of this study. The follow-up time interval was counted from the time of enrollment until the last traceable hospital inpatient or outpatient record or telephone interview before March 2018. The composite endpoint events included all-cause death (death mainly caused by CVDs), nonfatal myocardial infarction, stroke, unplanned revascularization and hospitalized unstable angina. Meanwhile, to better clarify the association between hsCRP and cardiovascular outcomes, the former 3 more reliable endpoint events (hard endpoint events) were analyzed separately in this study. All available relevant data from any reported possible event were collected. Death of a participant was reported by the relatives, the general practitioner, or the specialist medical professional of the participant. Three experienced cardiologists who were masked to the study data classified the events independently.
Statistical analysis
Data are expressed as the means ± standard deviation (SD) or medians and interquartile ranges for continuous variables and as proportions for categorical variables. Differences between groups were analyzed by analysis of variance or a nonparametric test for continuous measures and the chi-squared or Fisher exact test for categorical variables. Linear regression was used to estimate the independent predictors of coronary severity as measured by GS. The collinearity between each risk factor in the multivariate analyses was assessed by correlation coefficients and the tolerance/variance inflation factor. The event-free survival rates among subgroups according to hsCRP levels and/or hypertension status were estimated by the Kaplan–Meier method and compared by the log-rank test. Multivariate Cox proportional hazard models were used to calculate hazard ratios (HRs) for CVD events of subjects with average (1–3 mg/L) or high (>3 mg/L) hsCRP levels compared with those with low hsCRP levels (<1 mg/L) and for those of hypertensive patients compared with patients with normal BP. HRs for CVD events were also computed for patients with average or high hsCRP levels, with or without the presence of hypertension, compared with participants with low hsCRP and normal BP. The analyses were initially adjusted for age and sex in models 1 and 3; further adjustments were subsequently made for current smoking, diabetes mellitus, GS, left ventricular ejection fraction, triglyceride, LDL-C, statin use and antihypertensive drug use in model 4. Model 2 included all the adjusted variables in model 4 plus hsCRP categories and hypertension.
All statistical analyses were performed with SPSS version 22.0 software (SPSS Inc., Chicago, IL). In the chi-squared test, for comparisons between any two of the three groups according to hsCRP levels, two tailed p values < 0.017 were considered statistically significant, while for comparisons between any two of the six groups according to both hsCRP and hypertension status, two tailed p values < 0.003 were considered statistically significant. A two-sided p value of 0.05 was considered significant for all other tests.
Role of the funding source
The funding organizations did not participate in the design of the study; the collection, analysis, and interpretation of the data; or the decision to approve publication of the finished manuscript.
Results
Baseline characteristics
According to the CDC/AHA recommended hsCRP cutoff points, the study population comprised 1520 (35.4%) patients with low hsCRP (<1 mg/L), 1709 (39.8%) with average hsCRP (1–3 mg/L), and 1062 (24.7%) with high hsCRP (>3 mg/L) concentrations (Fig. 1). The baseline characteristics stratified according to hsCRP levels are shown in Table 1. Higher baseline hsCRP levels were significantly associated with traditional cardiovascular risk factors such as hypertension, DM, current smoking, and higher body mass index (all p < 0.05). The fasting plasma glucose, glycosylated hemoglobin, TC, LDL-C, triglyceride, creatinine, fibrinogen, ESR (all p < 0.001), and lipoprotein (a) (p = 0.021) levels were positively associated with the hsCRP levels. Lower baseline hsCRP levels were associated with higher left ventricular ejection fraction and HDL-C levels and were observed in patients taking statins (all p < 0.001). The baseline characteristics stratified according to hsCRP tertiles (<0.95, 0.95–2.29, and ≥2.30 mg/L) were similar to the above results.
HsCRP and coronary severity
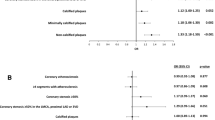
The coronary severity was assessed in three categories according to hsCRP levels. As shown in Fig. 2a, b, the high hsCRP group had significantly higher log-transformed GS and more patients with multivessel disease than any other group (all p < 0.05), while the average hsCRP group only had higher log-transformed GS compared with the low hsCRP group (p < 0.01). Furthermore, after adjusting for sex, age, hypertension, DM, current smoking, family history of CAD, HDL-C, LDL-C, lipoprotein (a) and creatinine (the collinearity had been excluded between each of them), only baseline hsCRP >3 mg/L was independently associated with GS compared with hsCRP <1 mg/L (p = 0.023). When the subjects were categorized according to hsCRP tertiles, tertiles 2 and 3 had significantly higher log-transformed GS and more patients with multivessel disease than tertile 1 (both p < 0.01). HsCRP tertile 3 had significantly more multivessel lesions compared with tertile 2 (p < 0.05), while the increase in GS did not reach statistical significance (p > 0.05; Supplemental Fig. 1A, B). However, in the further multivariate regression analysis, the association between hsCRP tertile 3 and GS was attenuated (p = 0.070).
Coronary severity according to hsCRP levels (mg/L) or both hsCRP levels and HTN status. a Log-transformed Gensini score according to hsCRP levels; b Coronary lesion vessels according to hsCRP levels; c Log-transformed Gensini score according to both hsCRP levels and HTN status; d Coronary lesion vessels according to both hsCRP levels and HTN status. HsCRP high-sensitivity C-reactive protein, HTN hypertension. #Reference group; *p < 0.05; **p < 0.01
The results for the groups evaluated according to both baseline hsCRP and hypertension status are shown in Fig. 2c, d [HsCRP <1/−hypertension (HTN) as reference, HsCRP 1–3/−HTN, HsCRP >3/−HTN, HsCRP <1/+HTN, HsCRP 1–3/+HTN, and HsCRP >3/+HTN]. Compared with the reference group (HsCRP<1/−HTN group), all the other groups had significantly higher log-transformed GS (p < 0.05, respectively). Meanwhile, with the exception of the HsCRP 1–3/−HTN group (p > 0.05), all the other groups (p < 0.01) had significantly more patients with multivessel disease than the reference group. After adjusting for sex, age, DM, current smoking, family history of CAD, HDL-C, LDL-C, lipoprotein (a) and creatinine, the HsCRP >3/−HTN, HsCRP <1/+HTN, HsCRP 1–3/+HTN, and HsCRP >3/+HTN groups still had positive associations with GS compared with the reference group (all p < 0.05). Similarly, compared with the reference group (HsCRP tertile 1/-HTN), the HsCRP tertile 3/-HTN, HsCRP tertile 1/+HTN, HsCRP tertile 2/+HTN and HsCRP tertile 3/+HTN groups had higher log-transformed GS and more multivessel lesions (all p < 0.01; Supplemental Fig. 1C, D). Moreover, these associations persisted after adjusting for the covariates (all p < 0.05).
HsCRP and CVD events
During 14,210 person-years of follow-up, 530 composite endpoint events were recorded [60 died, 49 suffered nonfatal myocardial infarction, 109 had strokes, 192 underwent unplanned revascularization procedures (the median time was 14.07 months; the interquartile range was 7.70–31.58 months), and 120 were hospitalized for unstable angina], representing 37.3 events per 1000 person-years. Of importance, nearly half (n = 218, 41.1%) of them were hard endpoint events (all-cause death, nonfatal myocardial infarction and stroke). The patients who suffered acute coronary syndrome and underwent revascularization procedures were assigned only once in the analysis. The incidences of the corresponding composite endpoint events per 1000 person-years in the low, average, and high hsCRP groups were 33.5 (95% CI 24.0–41.9), 38.1 (95% CI 28.9–47.1), and 43.4 (95% CI 31.2–55.7), respectively. Meanwhile, the corresponding occurrence of hard endpoint events per 1000 person-years in the three subgroups according to hsCRP levels from low to high were 12.2 (95% CI 6.7–17.7), 15.0 (95% CI 9.2–20.8), and 21.1 (95% CI 12.5–29.7), respectively. Kaplan-Meier analysis with the log-rank test (Fig. 3a) showed that participants with hsCRP >3 mg/L had significantly lower cumulative event-free survival rates for all endpoint events compared with those with hsCRP <1 mg/L (p = 0.016), whereas there was no significant difference between the average and low hsCRP groups or between the high and average hsCRP groups (both p > 0.05). In addition, patients with hsCRP >3 mg/L had the lowest cumulative event-free survival rate for hard endpoint events among the three groups (p < 0.05 for all comparisons), while there was no significant difference between the average and low hsCRP groups (p > 0.05; Fig. 3b). As shown in Fig. 3c, d, patients with hypertension had worse cardiovascular outcomes than those with normal BP (both p < 0.05). When the participants were categorized according to both hsCRP and hypertension status (Fig. 3e, f), the HsCRP <1/+HTN, HsCRP 1–3/+HTN, and HsCRP >3/+HTN groups had significantly lower cumulative event-free survival rates for all endpoint events compared with the reference group (HsCRP<1/−HTN group; all p < 0.05). Meanwhile, for the hard endpoint events, the HsCRP >3/−HTN, HsCRP 1–3/+HTN, and HsCRP>3/+ HTN groups had significantly lower cumulative event-free survival rates compared with the reference group (HsCRP <1/−HTN group; all p < 0.05). When subjects were grouped based on hsCRP tertiles, the results were exactly the same as above. The tertile 3 group had a significantly lower cumulative event-free survival rate for all endpoint events compared with tertile 1 (p = 0.011) and the lowest cumulative event-free survival rate for hard endpoint events (all p < 0.05, Supplemental Fig. 2A, B). Furthermore, compared with the HsCRP tertile 1/-HTN group (reference), the three groups with hypertension had a significantly higher incidences of all endpoint events, while the HsCRP tertile 3/-HTN, tertile 2/+ HTN and tertile 3/+ HTN groups had significantly higher incidences of hard endpoint events (all p < 0.05, Supplemental Fig. 2C, D).
Kaplan–Meier survival curves for a the categories of hsCRP for all endpoint events, b the categories of hsCRP for hard endpoint events, c the presence of hypertension or not for all endpoint events, d the presence of hypertension or not for hard endpoint events, e the categories of hsCRP and hypertension for all endpoint events, and f the categories of hsCRP and hypertension for hard endpoint events. HsCRP high-sensitivity C-reactive protein, HTN hypertension
The adjusted HRs and 95% confidence interval (CI) of hsCRP concentrations and hypertension for CVD endpoint events are shown in Table 2. A baseline hsCRP > 3 mg/L had a 1.30× higher risk of all CVD events occurring in the crude model compared with the reference group (hsCRP <1 mg/L). Additional adjustment for age and sex only slightly attenuated this association, while further adjustment for more confounding factors made this association disappear. Similarly, a baseline hsCRP >3 mg/L had a 1.71× higher risk of hard endpoint events occurrence in the crude model compared with the reference group, whereas this association disappeared after adjusting for multiple confounding factors. In addition, an average level of hsCRP (1–3 mg/L) did not increase either all or separate hard CVD events risk significantly compared with the reference group in any adjusted model. However, the association between hypertension and cardiovascular outcomes, including both all endpoint events and hard endpoint events, persisted in all three models (all p < 0.05). Furthermore, the results for the hsCRP categories stratified by hypertension status are shown in Table 3. After adjusting for potential confounding factors in Cox models, compared with the reference group (HsCRP <1/−HTN group), average or high hsCRP concentrations alone, isolated hypertension, or the average hsCRP plus hypertension was not associated with an elevated risk for either all or separate hard endpoint events (p > 0.05, all). Only high hsCRP (>3 mg/L) combined with hypertension significantly increased the risk for developing CVD events compared with the reference group, with an adjusted HR of 1.51 (95% CI, 1.09–2.11) for all composite endpoint events and 1.89 (95% CI, 1.10–3.27) for hard endpoint events. In further analysis according to hsCRP tertiles, we observed similar results (Supplemental Tables 1 and 2).
Discussion
In this prospective study with a large cohort of stable, newly diagnosed CAD patients who received coronary angiography, we found that clinically elevated hsCRP or hypertension alone was associated with more severe coronary lesions. Cox regression analysis indicated that high hsCRP levels were related to an elevated but nonsignificant increased risk for cardiovascular outcomes, while hypertension was significantly correlated with the CVD events risk. Nevertheless, when patients were categorized according to both hsCRP levels and hypertension status, only patients with hypertension plus elevated hsCRP levels had a 1.51-fold higher risk for all endpoint events and a 1.89-fold increased risk for hard endpoint events compared with subjects with normal BP and low hsCRP levels.
For decades, there has been a broad consensus that inflammation plays a critical role in all stages of the atherosclerotic process, from the onset of initial lesions to plaque progression and complications occurrence [1, 2]. Along with the publications of the results of several large-scale clinical trials in recent 3 years [5, 6, 20], the role of inflammation in cardiovascular risk has become a hot topic again. There are numerous diverse markers for systemic inflammation, but among them, hsCRP is a sensitive and nonspecific marker with good biological stability [21]. Many studies have demonstrated a significant and independent association between elevated hsCRP levels and cardiovascular events in multiple clinical settings [7, 12, 13, 22, 23]. Furthermore, the Canakinumab anti-inflammatory Thrombosis Outcomes Study (CANTOS) randomized controlled trial provided collateral evidence for the correlation between improvement of hsCRP levels and risk reduction for cardiovascular outcomes [5, 6]. Therefore, a patient’s initial hsCRP level may prove to be a simple and readily available biomarker that could help the emergency care staff identify CVD patients who may be at a high risk of cardiovascular events and could benefit from inflammation modulation therapy to reduce cardiovascular risk [24]. However, some other studies found that this association did not always exist. Ridker et al. [9] conducted a nested case–control study with 391 participants in the Cholesterol and Recurrent Events (CARE) trial who subsequently developed recurrent nonfatal myocardial infarction or a fatal coronary event and an equal number of age-matched and sex-matched participants who remained free of these events during the 5-year follow-up. They found that although a significant association of elevated C-reactive protein and serum amyloid A with CVD events was observed among those randomly assigned to the placebo, this risk was attenuated and no longer significant among those randomized to pravastatin. Another study of 1246 patients with angiographically diagnosed CAD with a median of 2.9 years of follow-up also showed that hsCRP lost its predictive ability for cardiovascular events in participants receiving statin therapy [11]. Additionally, Biasucci et al. [10] performed a study on patients with unstable angina and found that hsCRP was not associated with the 1-year follow-up events, including myocardial infarction and death, in diabetic patients. Moreover, there have been conflicting data regarding the consistent increased value of hsCRP beyond that of conventional risk factors for the prediction of cardiovascular events. Some studies showed modest improvement in predictive ability [25, 26], but others found little or no increased value of adding hsCRP to the risk prediction model consisting of traditional risk factors [27,28,29], since the association of hsCRP with CVD may be partly attributed to its strong correlation with traditional risk factors [8]. As a result, although several leading organizations have published related guidelines on the use of hsCRP in CVD risk prediction, there is a lack of consensus regarding the appropriate clinical application of hsCRP [8].
Considering the possible impacts of traditional risk factors, many efforts have been made in the exploration of the best use of hsCRP to predict CVD events in clinical work [3, 7, 10, 14, 15]. However, no studies have been performed to determine the combined effects of elevated hsCRP and hypertension on CVD prognosis, with the exception of a recent study by Jimenez et al. [13] examining the association between hsCRP and stroke by hypertension status. Given the predictive role of elevated hsCRP for incident hypertension [30] and the largest contribution of inflammatory markers and BP to the inverse association between physical activity and cardiovascular events in a previous report [31], we speculated that the combination of hsCRP and hypertension may provide more stable and greater predictive value for CVD risk than either one alone. Indeed, in this study, our data showed that the cardiovascular events risk was greatly and significantly elevated in patients with both high hsCRP and hypertension compared with the reference group with low hsCRP and normal BP, while patients with either elevated hsCRP or hypertension alone did not have a significantly increased risk for CVD events. Moreover, compared with the reference group, the risk of elevated hsCRP plus hypertension for all-cause death, nonfatal myocardial infarction and stroke was more clearly increased than for all end point events (all-cause death, nonfatal myocardial infarction, stroke, unplanned revascularization and hospitalization for unstable angina). Importantly, our study may provide novel information regarding the interactions of inflammation and hypertension in the prediction of cardiovascular outcomes in patients with stable CAD.
Although our data suggested a potential association between hsCRP and hypertension in predicting CVD outcomes, the exact underlying mechanisms are not fully understood. According to previous reports [13, 32], hsCRP, as the most representative inflammatory marker, may induce atherogenesis by activating the inflammatory cascade and interacting with endothelial and smooth muscle cells, leading to foam cell formation, endothelial dysfunction, and plaque destabilization. At the same time, hypertension, as a significant metabolic disease carrying a powerful risk for CVD, can damage endothelial function through hemodynamic changes, resulting in endothelial dysfunction, increased circulating inflammatory markers and oxidative stress, and upregulated adhesion molecule expression [17, 33]. Their similar and overlapping effects are the key initiators for atherosclerosis, thrombosis, and the corresponding complications [1, 33]. Thus, it is obvious that there is a close association between inflammation and hypertension, which may contribute to the significant and potent influence of elevated hsCRP plus hypertension on cardiovascular events. In addition, previous studies indicated that elevated hsCRP concentrations may exacerbate the underlying proatherothrombotic environment of hypertension [13], which may also partially explain the combined effects of hsCRP and hypertension. To further clarify the specific mechanisms, more experiments are needed in the future.
Several limitations of this study deserve consideration. First, inherent in the nature of any observational and prospective study, our findings are subject to confounding factors, and the baseline levels of risk factors may also change during follow-up. However, the data in our study were adjusted for a range of confounding factors to investigate the combined effect of elevated hsCRP and hypertension on cardiovascular risk. Second, our findings are based on one measurement of serum hsCRP, which may not accurately reflect the status of a study participant. Nevertheless, hsCRP levels appear to remain stable over time without the presence of acute infection, with within-person variability over time similar to that of LDL-C and systolic BP [2, 21]. Third, not all patients underwent coronary computed tomography angiography; therefore, we were not able to analyze the association of hsCRP and hypertension with the calcified plaque burden, which is also a good marker of CAD severity. Finally, the follow-up time and sample size in this study needed to be longer and larger to better examine the prognostic value of hsCRP alone or in addition to hypertension with regard to the long-term outcomes.
In conclusion, the present study for the first time demonstrated that the combination of elevated hsCRP levels and hypertension offers more predictive power for cardiovascular outcomes than simply using either one alone in patients with stable, newly diagnosed CAD. This finding may provide clinicians with new insight into the optimal clinical use of hsCRP in cardiovascular risk prediction and stratification because the ability to identify those with an elevated risk for subsequent events allows for the targeting of individuals who need increased monitoring and/or treatment.
References
Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352:1685–95.
Libby P, Ridker PM, Hansson GK, Leducq Transatlantic Network on A. Inflammation in atherosclerosis: from pathophysiology to practice. J Am Coll Cardiol. 2009;54:2129–38.
Bohula EA, Giugliano RP, Cannon CP, Zhou J, Murphy SA, White JA, et al. Achievement of dual low-density lipoprotein cholesterol and high-sensitivity C-reactive protein targets more frequent with the addition of ezetimibe to simvastatin and associated with better outcomes in IMPROVE-IT. Circulation 2015;132:1224–33.
Pradhan AD, Aday AW, Rose LM, Ridker PM. Residual inflammatory risk on treatment with PCSK9 inhibition and statin therapy. Circulation 2018;138:141–9.
Ridker PM, MacFadyen JG, Everett BM, Libby P, Thuren T, Glynn RJ, et al. Relationship of C-reactive protein reduction to cardiovascular event reduction following treatment with canakinumab: a secondary analysis from the CANTOS randomised controlled trial. Lancet 2018;391:319–28.
Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with Canakinumab for atherosclerotic disease. New Engl J Med. 2017;377:1119–31.
Hwang YC, Morrow DA, Cannon CP, Liu Y, Bergenstal R, Heller S, et al. High-sensitivity C-reactive protein, low-density lipoprotein cholesterol and cardiovascular outcomes in patients with type 2 diabetes in the EXAMINE (Examination of Cardiovascular Outcomes with Alogliptin versus Standard of Care) trial. Diabetes Obes Metab. 2018;20:654–9.
Yousuf O, Mohanty BD, Martin SS, Joshi PH, Blaha MJ, Nasir K, et al. High-sensitivity C-reactive protein and cardiovascular disease: a resolute belief or an elusive link? J Am Coll Cardiol. 2013;62:397–408.
Ridker PM, Rifai N, Pfeffer MA, Sacks FM, Moye LA, Goldman S, et al. Inflammation, pravastatin, and the risk of coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events (CARE) Investigators. Circulation 1998;98:839–44.
Biasucci LM, Liuzzo G, Della Bona R, Leo M, Biasillo G, Angiolillo DJ, et al. Different apparent prognostic value of hsCRP in type 2 diabetic and nondiabetic patients with acute coronary syndromes. Clin Chem. 2009;55:365–8.
Bickel C, Rupprecht HJ, Blankenberg S, Espiniola-Klein C, Schlitt A, Rippin G, et al. Relation of markers of inflammation (C-reactive protein, fibrinogen, von Willebrand factor, and leukocyte count) and statin therapy to long-term mortality in patients with angiographically proven coronary artery disease. Am J Cardiol. 2002;89:901–8.
Sabatine MS, Morrow DA, Jablonski KA, Rice MM, Warnica JW, Domanski MJ, et al. Prognostic significance of the Centers for Disease Control/American Heart Association high-sensitivity C-reactive protein cut points for cardiovascular and other outcomes in patients with stable coronary artery disease. Circulation 2007;115:1528–36.
Jimenez MC, Rexrode KM, Glynn RJ, Ridker PM, Gaziano JM, Sesso HD. Association between high-sensitivity C-reactive protein and total stroke by hypertensive status among men. J Am Heart Assoc. 2015;4:e002073.
Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. New Engl J Med. 1997;336:973–9.
Ridker PM, Hennekens CH, Buring JE, Rifai N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. New Engl J Med. 2000;342:836–43.
Liu HH, Guo YL, Wu NQ, Zhu CG, Gao Y, Qing P, et al. High-density lipoprotein cholesterol levels are associated with coronary severity but not with outcomes in new-onset patients with stable coronary artery disease. Atherosclerosis. 2017;263:104–11.
Liu HH, Cao YX, Li S, Guo YL, Zhu CG, Wu NQ, et al. Impacts of prediabetes mellitus alone or plus hypertension on the coronary severity and cardiovascular outcomes. Hypertension 2018;71:1039–46.
Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO, 3rd, Criqui M, et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 2003;107:499–511.
Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol. 1983;51:606.
Opotowsky AR, Valente AM, Alshawabkeh L, Cheng S, Bradley A, Rimm EB, et al. Prospective cohort study of C-reactive protein as a predictor of clinical events in adults with congenital heart disease: results of the Boston adult congenital heart disease biobank. Eur Heart J. 2018;39:3253–61.
Ridker PM. A test in context: high-sensitivity C-reactive protein. J Am Coll Cardiol. 2016;67:712–23.
Muhlestein JB, May HT, Galenko O, Knowlton KU, Otvos JD, Connelly MA, et al. GlycA and hsCRP are independent and additive predictors of future cardiovascular events among patients undergoing angiography: the intermountain heart collaborative study. Am Heart J. 2018;202:27–32.
Elesber AA, Conover CA, Denktas AE, Lennon RJ, Holmes DR,Jr., Overgaard MT, et al. Prognostic value of circulating pregnancy-associated plasma protein levels in patients with chronic stable angina. Eur Heart J. 2006;27:1678–84.
Yoshinaga R, Doi Y, Ayukawa K, Ishikawa S. High-sensitivity C reactive protein as a predictor of inhospital mortality in patients with cardiovascular disease at an emergency department: a retrospective cohort study. BMJ Open. 2017;7:e015112
Ridker PM, Buring JE, Rifai N, Cook NR. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds Risk Score. JAMA 2007;297:611–9.
Zethelius B, Berglund L, Sundstrom J, Ingelsson E, Basu S, Larsson A, et al. Use of multiple biomarkers to improve the prediction of death from cardiovascular causes. New Engl J Med. 2008;358:2107–16.
Ridker PM, Rifai N, Rose L, Buring JE, Cook NR. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. New Engl J Med. 2002;347:1557–65.
Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, O’Leary D, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA. 2012;308:788–95.
Kavousi M, Elias-Smale S, Rutten JH, Leening MJ, Vliegenthart R, Verwoert GC, et al. Evaluation of newer risk markers for coronary heart disease risk classification: a cohort study. Ann Intern Med. 2012;156:438–44.
Niskanen L, Laaksonen DE, Nyyssonen K, Punnonen K, Valkonen VP, Fuentes R, et al. Inflammation, abdominal obesity, and smoking as predictors of hypertension. Hypertension 2004;44:859–65.
Hamer M, Stamatakis E. Physical activity and risk of cardiovascular disease events: inflammatory and metabolic mechanisms. Med Sci sports Exerc. 2009;41:1206–11.
Hansson GK, Zhou X, Tornquist E, Paulsson G. The role of adaptive immunity in atherosclerosis. Ann N Y Acad Sci. 2000;902:53–62.
Huang Z, Chen C, Li S, Kong F, Shan P, Huang W. Serum markers of endothelial dysfunction and inflammation increase in hypertension with prediabetes mellitus. Genet Test Mol Biomark 2016;20:322–7.
Acknowledgements
This work was partially supported by the Capital Health Development Fund (201614035) and the CAMS Major Collaborative Innovation Project (2016-I2M-1–011) awarded to Dr. Jian-Jun Li, MD, PhD. The authors thank the staff of the Cardiac Catheterization Laboratory at Fu Wai Hospital for their assistance in performing the studies. The authors also thank all the study investigators, staff, and patients.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Liu, HH., Cao, YX., Sun, D. et al. High-sensitivity C-reactive protein and hypertension: combined effects on coronary severity and cardiovascular outcomes. Hypertens Res 42, 1783–1793 (2019). https://doi.org/10.1038/s41440-019-0293-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0293-8