Abstract
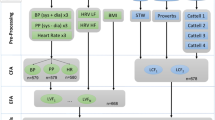
Cognitive impairment is prevalent in patients with chronic kidney disease (CKD), but its underlying mechanisms are obscure. Here, we test the hypothesis that exaggerated orthostatic blood pressure reduction mediates the effects of renal failure on global cognition and memory. A total of 160 study subjects were recruited, including 80 dialysis patients and 80 controls. Global cognition was evaluated using the Montreal Cognitive Assessment (MoCA), and episodic memory was evaluated using the auditory verbal learning test (AVLT). Autonomic function was evaluated via the low-frequency to high-frequency ratio (LF/HF) through heart rate variability analysis. Compared with the controls, the dialysis patients had significantly lower MoCA and AVLT scores (including learning memory, short recall memory, and delayed recall memory) (all p < 0.001). They also showed exaggerated orthostatic systolic blood pressure reductions (all p ≤ 0.001). The maximum orthostatic systolic blood pressure reduction was independently and negatively associated with short (β = −0.05, p = 0.029) and delayed (β = −0.05, p = 0.035) recall memory in dialysis patients but not in controls. Mediation analysis demonstrated that maximum orthostatic systolic blood pressure reduction mediates 13.8% of the effect of end-stage renal disease (ESRD) on short recall memory (p = 0.04). After adjustment for LF/HF, the negative association between maximum orthostatic blood pressure reduction and short recall score remained significant (p = 0.049), while the association between maximum orthostatic blood pressure reduction and delayed recall score became nonsignificant, with a marginal p value of 0.062. Our study reveals that exaggerated orthostatic blood pressure reduction is a possible explanation for ESRD-associated memory deficits.
Similar content being viewed by others
Introduction
Over the past decade, considerable literature has reported on the increased risk of cognitive impairment in patients with chronic kidney disease (CKD). Accumulating evidence suggests that this condition is highly prevalent in CKD patients. The reported prevalence of cognitive impairment, as measured by several cognitive tests including the Montreal Cognitive Assessment (MoCA), is 30–60% in patients with advanced renal failure (CKD stage 3 or above) [1,2,3]. In those on maintenance hemodialysis, a study by Murray et al. suggested that nearly 90% of the patients had cognitive impairment of varying severity [4]. The increased prevalence of cognitive impairment in CKD patients poses a critical threat to their quality of life, adherence to medications and decision-making ability, while it also increases the burden on family members and health caregivers. Most importantly, prior data indicate that it may also worsen a patient’s prognosis [5, 6].
Despite multiple lines of epidemiologic evidence, there remains a paucity of investigations on the mechanisms underlying CKD-associated cognitive impairment. It is well known that CKD populations have an increased burden of cardiovascular disease and that cardiovascular health is a major determinant of cognitive status [7, 8]. Therefore, cardiovascular injury seems to be a reasonable explanation for cognitive impairment in CKD. However, it remains unclear how cardiovascular injury leads to cognitive impairment in these patients.
Patients with renal failure are at increased risk for impaired orthostatic blood pressure stabilization. A previous study examined the determinants of orthostatic hypotension in over 5000 middle-aged men and found that reduced eGFR is independently associated with systolic orthostatic impairment [9]. Similarly, a more recent report from a cohort study noted a graded association between renal function and the prevalence of orthostatic hypotension in the elderly [10]. Although relevant data are limited in patients with end-stage renal disease (ESRD), it is likely that these patients are extremely prone to developing exaggerated orthostatic blood pressure reduction because reduced baroreflex sensitivity and autonomic dysfunction, two of the most important physiologic mechanisms for the maintenance of orthostatic homeostasis, are prevalent as renal function declines [11, 12]. Meanwhile, it is intuitive to link cognitive impairment to exaggerated orthostatic blood pressure reduction, as the latter could result in cerebral hypoperfusion. However, evidence for this relationship among ESRD patients is scarce. In this study, we tested the hypothesis that exaggerated orthostatic blood pressure reduction mediates the effect of renal failure on global cognition and memory.
Methods
Study population
The current study enrolled 80 dialysis patients and 80 controls. The two groups were frequency-matched by age, sex, and years of education. For the patient group, subjects aged ≥18 years and who had been on maintenance hemodialysis (4 h per treatment and thrice weekly) for over 3 months were recruited from the dialysis center of the Second Affiliated Hospital of Nanjing Medical University. Patients meeting any of the following criteria were excluded: (1) Previous history of stroke or any other neurologic diseases (determined by self-report or medical records); (2) implantation of pacemakers or high-degree (II/III degree) atrioventricular blocks unsuitable for heart rate variability (HRV) analysis; (3) acute infection or any other condition that precludes the patients from immediate participation; (4) illiteracy, visual impairment or any other cause that leads to the inability to complete cognitive tests; (5) contraindications to magnetic resonance imaging; (6) malignancy with life expectancy <1 year; and (7) plans to transfer to other dialysis centers or receive kidney transplant within 1 year. For the control group, 80 subjects without any history of cardiovascular, neurologic, or CKDs were enrolled. The control group was recruited from the community via advertisement or referral by individuals who were aware of this study. Prior to enrollment, all subjects were screened for possible unrecognized CKDs (defined as eGFR < 60 mL/min/1.73 m2 or protein ≥ 1 + in a dipstick test).
All participants provided written informed consent prior to their inclusion in the study. The study was approved by the Institutional Ethical Committee of the Second Affiliated Hospital of Nanjing Medical University.
Study process
All the following procedures were performed in the morning (usually 0800–1000 hours). For patients, the tests were conducted on the nondialysis day following the second dialysis treatment in a week.
Blood pressure
Subjects rested quietly in a sitting position for at least 5 min before blood pressure measurement. Three seated blood pressure measurements were taken by a research nurse using an automatic monitor (HEM-7130, Omron Healthcare Co. Ltd, Kyoto, Japan), with a 1-min interval between each measurement. After the last seated measurement, the participants were asked to stand up immediately, and standing blood pressure was measured three times at 1-min intervals. Any symptoms of orthostatic hypotension (i.e., dizziness) reported by the participants while standing were also recorded. Participants were allowed to sit or lie down if they felt they could not keep standing during the process, although all participants underwent the three standing blood pressure measurements successfully in our study.
Seated blood pressure levels were calculated as the mean of the second and third seated blood pressure measurements. The first measurement was not included, as it is suggested that the combination of the second and third reading is more favorable for the estimate of true underlying blood pressure [13].
We defined orthostatic blood pressure change as the following:
Maximum orthostatic systolic blood pressure reduction: seated systolic blood pressure minus the minimum of the three standing systolic blood pressures;
Average orthostatic systolic blood pressure reduction: seated systolic blood pressure minus the mean of the three standing systolic blood pressures;
Immediate orthostatic systolic blood pressure reduction: seated systolic blood pressure minus the first standing systolic blood pressure;
Delayed orthostatic systolic blood pressure reduction: seated systolic blood pressure minus the third standing systolic blood pressure.
Cognition and memory
Cognition and memory tests were administered by a trained research staff member (LW) in a quiet test room. Global cognition was assessed using the Chinese (Mandarin) translation of the MoCA (Version 7). The MoCA is a comprehensive tool for cognitive assessment that is widely used both in the general population and in patients with CKD [2, 14]. In particular, it has been shown to be a sensitive test for detecting cognitive impairment in patients on hemodialysis [15]. The total possible MoCA score is 30 points.
Episodic memory was evaluated using the auditory verbal learning test (AVLT) (Huashan Version). The AVLT consists of 12 two-character words from three categories, including flowers, occupations, and apparel. First, the word list was read out by a research staff member to the participant, and the subjects were asked to recall as many words as they could in any order (Test 1). The same procedure was repeated for another two cycles (Test 2 and Test 3) and then followed by a 5-min interval. After this interval, the subjects were asked to recall the words freely (Test 4) as a short recall test. The delayed recall test was performed 20 min later (Test 5). During the intervals of AVLT, all participants were interviewed by the research staff to collect general information. The following items were calculated for each participant and were used for analysis in the current study:
Learning memory = Test 1 + Test 2 + Test 3 (maximum score: 36);
Short recall memory = Test 4 (maximum score: 12);
Delayed recall memory = Test 5 (maximum score: 12).
Heart rate variability (HRV)
Autonomic function was assessed by HRV analysis using a three-channel 24-h ECG recorder (Lifecard CF; SpaceLabs Healthcare, WA, USA) [16, 17]. The recorder was attached to the participants following the completion of the other study procedures and was removed 24 h later (for dialysis patients, it was removed prior to the next dialysis session). An experienced technician reviewed the signals and manually deleted artifacts using the Impresario Holter system (SpaceLabs Healthcare, WA, USA). The low-frequency to high-frequency ratio (LF/HF), a frequency domain index, was calculated and used in further analysis. The power spectrum density was set at 0.04–0.15 Hz for low frequency and 0.15–0.4 Hz for high frequency. A total of six LF/HF values were analyzed from six 10-min ECG segments recorded between 1400 and 1500 hours. The average value was calculated after the exclusion of the highest and lowest values.
Laboratory and other data
Fasting blood samples were drawn from all the participants and shipped to a core laboratory of a third-party testing company (DIAN Diagnostics; Nanjing, China) for routine laboratory tests. The hemoglobin levels of the patients were determined using their most recent test results in our center within 3 months. Demographic and medical information were acquired by the research staff through structured interviews with the participant.
Statistical analyses
Numerical data were expressed as means ± standard deviations, and categorical data were expressed as counts (%). Student’s t test, the Mann−Whitney U test or the chi-square test were used for variable comparisons between the two groups as appropriate. Pearson’s correlation analysis was used to explore whether orthostatic blood pressure reduction was related to cognitive/memory test scores (MoCA, AVLT-learning memory, AVLT-short recall memory, AVLT-delayed recall memory) in patients and in controls. With the significant relationship found between short/delayed recall memory and orthostatic blood pressure reduction in the univariate analysis, independent predictors of the recall memory scores were determined using the following methods: Variables were first selected if they were correlated with memory scores (using a cut-off p value of 0.10) in Pearson’s correlation analyses and were then entered into stepwise regression analyses to construct the explanatory models based on Akaike information criteria. Models were constructed for patients and controls separately and for patients and controls in combination. To further determine the role of orthostatic blood pressure reduction in dialysis-associated memory deficits, we performed mediation analyses using maximum orthostatic systolic blood pressure reduction as the mediator, group (patients vs. controls) as the predictor and short/delayed recall memory scores as the outcome variables. Independent predictors for memory scores in the whole sample, excluding maximum orthostatic systolic blood pressure reduction and group, were treated as confounders. The bootstrapping approach was used to determine the significance of the mediation effect (sims = 1000) [18].
All statistical analyses were performed using R software, version 3.4.3 (R Foundation for Statistical Computing, www.R-project.org). A two-tailed p value of 0.05 was considered statistically significant.
Results
General characteristics of the participants
The demographic and general medical information of the study participants are presented in Table 1. The mean (±SD) age was 50.7 (±10.7) years for patients and 50.6 (±8.9) years for controls. There were 45 (56.3%) males in both groups. The average years of education were 10.2 (±3.1) and 10.2 (±2.5) for the patients and controls, respectively. The body mass index was significantly lower in the patient group (p < 0.001). The prevalence of current smokers and individuals with diabetes was comparable between groups. We did not note any differences in the blood pressures between the groups, except for a higher heart rate (p < 0.0001) in the patient group. Laboratory test results were in accordance with the characteristics of ESRD patients (anemia and lipid abnormality, Table 1).
Cognitive/memory test scores and orthostatic blood pressure changes
Cognitive and memory test scores, as well as orthostatic systolic blood pressure changes, are displayed in Table 2. Compared with the controls, patients received significantly lower scores on the MoCA (p < 0.001) and AVLT tests (including learning memory, short recall memory, and delayed recall memory; all p < 0.001). Orthostatic systolic blood pressure reductions were significantly higher in the patient group (all p ≤ 0.006). Distributions of orthostatic systolic blood pressure reductions in the two groups are shown in Supplementary Figure 1. Compared with controls, more patients showed orthostatic blood pressure reduction (positive reduction in the histograms), and the reduction magnitudes tended to be higher in the patient group.
To explore the association between orthostatic blood pressure reduction and cognitive/memory impairment, we first performed Pearson’s correlation analysis in the control and patient groups. The results are shown in Supplementary Table 1. In the controls, there were no significant correlations between orthostatic systolic blood pressure reductions and cognitive and memory test scores. However, orthostatic systolic blood pressure reductions were significantly and negatively correlated with short/delayed recall test scores in the patients, except for immediate systolic blood pressure reduction and delayed recall memory.
To further confirm the association between orthostatic blood pressure reduction and memory deficits, we performed multiple linear stepwise regression analysis with short and delayed recall scores as the dependent variables in the patient group. We used maximum orthostatic systolic blood pressure reduction in the following analyses because it had the strongest correlation with recall test scores among the four calculated orthostatic blood pressure parameters. After variable selection using univariate correlation analysis (the variables for short recall memory were age, education, maximum orthostatic systolic blood pressure reduction, calcium, sex, and diabetes; the variables for delayed recall were age, education, maximum orthostatic systolic blood pressure reduction, sex, diabetes, and previous cardiovascular diseases), predictive models for short and delayed recall scores were constructed based on the Akaike information criteria, as shown in Table 3. The results demonstrate that maximum orthostatic blood pressure reduction is a significant and independent predictor of both short recall memory (β = −0.05, s.e. = 0.02, p = 0.029) and delayed recall memory (β = −0.05, s.e. = 0.02, p = 0.035).
Orthostatic blood pressure reduction mediates the association between ESRD and memory deficits
We next attempted to explore whether orthostatic blood pressure reduction mediates the association between ESRD and memory deficits. First, predictive models for short and delayed recall test scores were constructed via stepwise regression analysis to test the association between ESRD and memory deficits. The final models revealed that ESRD is independently and negatively associated with both short recall scores (β = −1.23, p < 0.001) and delayed recall scores (β = −1.94, p < 0.001) (Supplementary Table 2). Mediation analyses were then performed, and the results are presented in Table 4. It was shown that 13.8% of the effects between ESRD and short recall scores were mediated by maximum systolic blood pressure reduction (p = 0.040). For ESRD and delayed recall scores, the percentage of the effect mediated was 8.7%, but this mediation was not significant, with a marginal p value of 0.07.
Adjustment for HRV
A possible explanation for the association between orthostatic blood pressure reduction and memory deficits in dialysis patients may be that this association reflects common brain injuries involving both memory-associated areas and the autonomic nervous system in these patients. Therefore, adjustment for LF/HF with the two predicting models in Table 3 was analyzed to test if this could negate the association between orthostatic blood pressure reduction and memory deficits. The results demonstrated that after adjustment for LF/HF, the negative association between maximum orthostatic blood pressure reduction and short recall scores remained significant (p = 0.049), while it became nonsignificant for delayed recall scores with a marginal p value of 0.062 (Supplementary Table 3).
Discussion
In the current study, we aimed to explore the role of orthostatic blood pressure reduction in ESRD-associated cognitive and memory impairment. Our analyses demonstrate the following: (1) patients on maintenance hemodialysis show significant global cognitive impairment and memory deficits compared to controls with normal renal function; (2) ESRD is an independent predictor for lower scores in cognitive and memory tests; (3) orthostatic blood pressure homeostasis is impaired in dialysis patients, with exaggerated blood pressure reduction upon standing; (4) orthostatic systolic blood pressure reduction is independently and negatively associated with short and delayed recall memory in dialysis patients, and it mediates the effect of ESRD on short recall memory; and (5) the association between orthostatic systolic blood pressure reduction and short recall memory remained significant even after adjustment for the autonomic function index, namely, LF/HF.
Patients with chronic renal insufficiency are at increased risk for the development of cognitive impairment. Previous reports have found that lower eGFR is independently associated with worse performance in multiple cognitive tests [19,20,21,22]. Our data support this evidence by demonstrating that ESRD is an independent predictor for lower scores on the MoCA and AVLT tests. The reason for the development of cognitive impairment and memory deficits in the context of renal dysfunction remains unclear, and a vascular hypothesis has been suggested as the major cause [23, 24]. However, the exact role of cardiovascular injury in ESRD-associated cognitive impairment has not yet been thoroughly explored. Our data reveal that orthostatic blood pressure reduction possibly serves as an important contributor to memory deficits in ESRD patients.
In our study, blood pressure fluctuation induced by postural change was very limited in the control group, whereas significant blood pressure decline upon standing was noted in the dialysis group. In healthy individuals, the maintenance of orthostatic homeostasis is a meticulously orchestrated physiologic process that depends on several mechanisms, including the baroreceptor reflex and autonomic regulation [25]. Disruption of any of these mechanisms could result in exaggerated orthostatic blood pressure reduction or even orthostatic hypotension. As mentioned above, reduced baroreflex sensitivity and autonomic dysfunction, which are associated with renal failure, could predispose ESRD patients to impaired orthostatic blood pressure stabilization. Sasaki et al. noted that orthostatic hypotension was present in 42% of subjects among 304 dialysis patients [26]. Their data and our findings are in line with the results from previous population-based studies [9, 10].
The association between orthostatic hypotension and cognitive impairment has been examined in several previous studies, and the results appear to be inconclusive. In a study by Frewen et al., the authors studied nearly 6000 elderly subjects (54% female) and found an independent association between orthostatic hypotension and poorer global cognitive function and memory in women aged ≥65 [27]. The cross-sectional association between orthostatic hypotension and cognitive status has also been noted in the elderly by Mehrabian et al. [28]. Furthermore, in a prospective study with 6 years of follow-up, baseline orthostatic hypotension was predictive of the risk of future mild cognitive impairment [29]. Despite these positive findings, there are also studies, either cross-sectional or longitudinal, showing no significant association between orthostatic hypotension and cognitive impairment [30, 31]. These prior explorations have been limited to the geriatric population. In our study, exaggerated orthostatic systolic blood pressure reduction was significantly and independently associated with worse performance on memory tests in dialysis patients. To the best of our knowledge, this is the first study linking orthostatic blood pressure reduction to memory deficits in the ESRD population. The lack of a significant association between orthostatic blood pressure reduction and global cognition suggests that the effect of orthostatic blood pressure reduction on cognition is not universal but likely memory specific. Notably, the association between orthostatic blood pressure reduction and memory performance in our study was limited to short and delayed recall but not learning memory. The physiologic basis for episodic memory is not yet clearly understood but has been proven to involve different brain areas and different working mechanisms. Prior data have validated that various stimuli could differentially affect different types of memory [32, 33]. Animal studies have also demonstrated that an increased delay between item presentation and recall requires the adequate function of certain brain areas, suggesting that even the physiologic mechanisms underlying short-term episodic memory with different time intervals are not identical [34]. In light of the regional ischemic vulnerability of the brain to hypoperfusion [35], it is therefore possible for orthostatic blood pressure reduction to have a differential effect on memory. Moreover, since we only included MoCA and AVLT tests in our study, it is not clear whether orthostatic blood pressure reduction also affects other cognitive domains in the patients. This question warrants more specific exploration in future studies.
Notably, the insignificant association in the control group in our study does not necessarily mean that the association between orthostatic blood pressure reduction and memory deficits is limited to the ESRD population. The reason for this discrepancy between groups may be due to orthostatic blood pressure reduction being more prominent in dialysis patients but not in the relatively healthy controls; hence, the limited variability in the control group, together with a limited sample size, preclude us from finding a significant association.
It is also worth pointing out that we used “orthostatic blood pressure reduction”, rather than the term “orthostatic hypotension”, in our study. Orthostatic hypotension is defined based on orthostatic blood pressure reduction and is typically a decrease in systolic blood pressure ≥20 mmHg (or diastolic blood pressure ≥10 mmHg) within 3 min of standing [36]. Only a very small proportion of dialysis patients in our study met the criteria for this definition (Supplementary Figure 1). Most patients only manifested exaggerated orthostatic blood pressure reduction, which did not reach the threshold for the definition of orthostatic hypotension. In fact, there is no validated pathophysiologic evidence for the determination of the cut-off value for diagnosing orthostatic hypotension. Our data suggest that even a limited exaggerated hypoperfusion may exert effects on patients’ memory.
The cross-sectional association between orthostatic blood pressure reduction and memory deficits in our study has two possible explanations. First, it may be a causative association that orthostatic blood pressure reduction induces cerebral hypotension, resulting in brain parenchyma injury and hence associated memory impairment. Second, this association could be a reflection of general cerebral injury in the patients, affecting both memory-associated areas and the autonomic nervous system. In our analyses, the adjustment for LF/HF, an autonomic activity index, did not diminish the significance of the association between orthostatic blood pressure reduction and short recall. Therefore, this finding suggests a direct causative role of orthostatic blood pressure reduction in the development of memory deficits. Furthermore, the mediation analysis in our study distinctly elucidated the relationship among ESRD status, orthostatic blood pressure reduction, and memory deficits. The analysis indicates that orthostatic blood pressure reduction mediates 13.8% of the effect of ESRD on memory ability, validating the contributing role of orthostatic blood pressure reduction in ESRD-associated memory deficits. Possible explanations for the nonsignificant result for delayed recall might involve the following: (1) As previously mentioned, orthostatic blood pressure reduction could exert a differential effect on memory, which in our case indicates a more potent effect on short recall than on delayed recall; and (2) the nonsignificant result might also be due to the limited power of the small sample size, especially given the marginal p values.
Despite drawing increasing interest in the research field, cognitive impairment remains largely neglected in clinical practice. In light of the negative impact on patients’ quality of life and prognosis, as well as on the health-care system, our data can be of major real-world importance. The association between exaggerated orthostatic blood pressure reduction and memory deficits indicates that physicians should also consider a screen test for memory deficits in patients who present symptoms of orthostatic hypotension, since they are at increased risk of having concurrent memory deficits, as shown in our study. Furthermore, impaired orthostatic blood pressure stabilization may serve as a potential target for the preservation of memory ability or even the treatment of memory deficits in dialysis patients. Several strategies have been proven previously to be effective in restoring orthostatic blood pressure stabilization among these patients [37,38,39].
There are several limitations of this study. First, the cross-sectional observational design precludes us from establishing a causative association between orthostatic blood pressure reduction and memory deficits. However, the additional adjustment for LF/HF in our analyses highly supports a causative role for orthostatic blood pressure reduction. Second, patients who were willing to participate were relatively healthier than the general dialysis population was. This characteristic may limit the generalizability of our findings.
In conclusion, our study reveals that exaggerated orthostatic blood pressure reduction is a possible explanation for ESRD-associated memory deficits. This finding provides insights into the pathophysiologic mechanisms of memory impairment in dialysis patients and suggests potential treatment targets for preserving memory ability in patients with ESRD. Future studies are warranted to explore the underlying mechanisms of memory impairment in dialysis patients, especially with cerebral imaging data.
References
Seidel UK, Gronewold J, Volsek M, Todica O, Kribben A, Bruck H, et al. The prevalence, severity, and association with HbA1c and fibrinogen of cognitive impairment in chronic kidney disease. Kidney Int. 2014;85:693–702.
Foster R, Walker S, Brar R, Hiebert B, Komenda P, Rigatto C, et al. Cognitive impairment in advanced chronic kidney disease: the Canadian Frailty Observation and Interventions Trial. Am J Nephrol. 2016;44:473–80.
Rodriguez-Angarita CE, Sanabria-Arenas RM, Vargas-Jaramillo JD, Ronderos-Botero I. Cognitive impairment and depression in a population of patients with chronic kidney disease in Colombia: a prevalence study. Can J Kidney Health Dis. 2016;3:26.
Murray AM, Tupper DE, Knopman DS, Gilbertson DT, Pederson SL, Li S, et al. Cognitive impairment in hemodialysis patients is common. Neurology. 2006;67:216–23.
Griva K, Stygall J, Hankins M, Davenport A, Harrison M, Newman SP. Cognitive impairment and 7-year mortality in dialysis patients. Am J Kidney Dis. 2010;56:693–703.
Raphael KL, Wei G, Greene T, Baird BC, Beddhu S. Cognitive function and the risk of death in chronic kidney disease. Am J Nephrol. 2012;35:49–57.
Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation. 2003;108:2154–69.
Qiu C, Fratiglioni L. A major role for cardiovascular burden in age-related cognitive decline. Nat Rev Cardiol. 2015;12:267–77.
Fedorowski A, Stavenow L, Hedblad B, Berglund G, Nilsson PM, Melander O. Consequences of orthostatic blood pressure variability in middle-aged men (The Malmo Preventive Project). J Hypertens. 2010;28:551–9.
Canney M, O’Connell MDL, Sexton DJ, O’Leary N, Kenny RA, Little MA, et al. Graded association between kidney function and impaired orthostatic blood pressure stabilization in older adults. J Am Heart Assoc. 2017;6: pii: e005661.
Johansson M, Gao SA, Friberg P, Annerstedt M, Bergstrom G, Carlstrom J, et al. Reduced baroreflex effectiveness index in hypertensive patients with chronic renal failure. Am J Hypertens. 2005;18:995–1000. discussion 1016.
Jassal SV, Douglas JF, Stout RW. Prevalence of central autonomic neuropathy in elderly dialysis patients. Nephrol, Dial, Transplant. 1998;13:1702–8.
Schulze MB, Kroke A, Bergmann MM, Boeing H. Differences of blood pressure estimates between consecutive measurements on one occasion: implications for inter-study comparability of epidemiologic studies. Eur J Epidemiol. 2000;16:891–8.
Dale W, Kotwal AA, Shega JW, Schumm LP, Kern DW, Pinto JM, et al. Cognitive function and its risk factors among older US adults living at home. Alzheimer Dis Assoc Disord. 2018;32:207–13.
Tiffin-Richards FE, Costa AS, Holschbach B, Frank RD, Vassiliadou A, Kruger T, et al. The Montreal Cognitive Assessment (MoCA)—a sensitive screening instrument for detecting cognitive impairment in chronic hemodialysis patients. PLoS ONE. 2014;9:e106700.
Task Force of The European Society of Cardiology and The North American Society of Pacing and Electrophysiology. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J. 1996;17:354–81.
Pomeranz B, Macaulay RJ, Caudill MA, Kutz I, Adam D, Gordon D, et al. Assessment of autonomic function in humans by heart rate spectral analysis. Am J Physiol. 1985;248(1 Pt 2):H151–153.
Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods, Instrum, & Comput. 2004;36:717–31.
Szerlip HM, Edwards ML, Williams BJ, Johnson LA, Vintimilla RM, O’Bryant SE. Association between cognitive impairment and chronic kidney disease in Mexican Americans. J Am Geriatr Soc. 2015;63:2023–8.
Kurella Tamura M, Xie D, Yaffe K, Cohen DL, Teal V, Kasner SE, et al. Vascular risk factors and cognitive impairment in chronic kidney disease: the Chronic Renal Insufficiency Cohort (CRIC) study. Clin J Am Soc Nephrol. 2011;6:248–56.
Ruebner RL, Laney N, Kim JY, Hartung EA, Hooper SR, Radcliffe J, et al. Neurocognitive dysfunction in children, adolescents, and young adults with CKD. Am J Kidney Dis. 2016;67:567–75.
Hailpern SM, Melamed ML, Cohen HW, Hostetter TH. Moderate chronic kidney disease and cognitive function in adults 20 to 59 years of age: Third National Health and Nutrition Examination Survey (NHANES III). J Am Soc Nephrol. 2007;18:2205–13.
Bugnicourt JM, Godefroy O, Chillon JM, Choukroun G, Massy ZA. Cognitive disorders and dementia in CKD: the neglected kidney−brain axis. J Am Soc Nephrol. 2013;24:353–63.
Drew DA, Weiner DE. Cognitive impairment in chronic kidney disease: keep vascular disease in mind. Kidney Int. 2014;85:505–7.
Ricci F, De Caterina R, Fedorowski A. Orthostatic hypotension: epidemiology, prognosis, and treatment. J Am Coll Cardiol. 2015;66:848–60.
Sasaki O, Nakahama H, Nakamura S, Yoshihara F, Inenaga T, Yoshii M, et al. Orthostatic hypotension at the introductory phase of haemodialysis predicts all-cause mortality. Nephrol, Dial, Transplant. 2005;20:377–81.
Frewen J, Savva GM, Boyle G, Finucane C, Kenny RA. Cognitive performance in orthostatic hypotension: findings from a nationally representative sample. J Am Geriatr Soc. 2014;62:117–22.
Mehrabian S, Duron E, Labouree F, Rollot F, Bune A, Traykov L, et al. Relationship between orthostatic hypotension and cognitive impairment in the elderly. J Neurol Sci. 2010;299:45–48.
Elmstahl S, Widerstrom E. Orthostatic intolerance predicts mild cognitive impairment: incidence of mild cognitive impairment and dementia from the Swedish general population cohort Good Aging in Skane. Clin Interv Aging. 2014;9:1993–2002.
Punchick B, Freud T, Press Y. The association between orthostatic hypotension and cognitive state among adults 65 years and older who underwent a comprehensive geriatric assessment. Medicine . 2016;95:e4264.
Curreri C, Giantin V, Veronese N, Trevisan C, Sartori L, Musacchio E, et al. Orthostatic changes in bood pressure and cognitive status in the elderly: the Progetto Veneto Anziani Study. Hypertens (Dallas, Tex: 1979). 2016;68:427–35.
Krishnan HC, Noakes EJ, Lyons LC. Chronic sleep deprivation differentially affects short and long-term operant memory in Aplysia. Neurobiol Learn Mem. 2016;134 Pt B:349–59.
Izquierdo LA, Vianna M, Barros DM, Mello e Souza T, Ardenghi P, Sant’Anna MK, et al. Short- and long-term memory are differentially affected by metabolic inhibitors given into hippocampus and entorhinal cortex. Neurobiol Learn Mem. 2000;73:141–9.
Petrides M. Dissociable roles of mid-dorsolateral prefrontal and anterior inferotemporal cortex in visual working memory. J Neurosci. 2000;20:7496–503.
Payabvash S, Souza LC, Wang Y, Schaefer PW, Furie KL, Halpern EF, et al. Regional ischemic vulnerability of the brain to hypoperfusion: the need for location specific computed tomography perfusion thresholds in acute stroke patients. Stroke. 2011;42:1255–60.
Shibao C, Lipsitz LA, Biaggioni I. Evaluation and treatment of orthostatic hypotension. J Am Soc Hypertens: Jash. 2013;7:317–24.
Yamamoto N, Sasaki E, Goda K, Nagata K, Tanaka H, Terasaki J, et al. Treatment of post-dialytic orthostatic hypotension with an inflatable abdominal band in hemodialysis patients. Kidney Int. 2006;70:1793–1800.
Fujisaki K, Kanai H, Hirakata H, Nakamura S, Koga Y, Hattori F, et al. Midodrine hydrochloride and L-threo-3,4-dihydroxy-phenylserine preserve cerebral blood flow in hemodialysis patients with orthostatic hypotension. Ther Apher Dial. 2007;11:49–55.
Iida N, Koshikawa S, Akizawa T, Tsubakihara Y, Marumo F, Akiba T, et al. Effects of L-threo-3,4-dihydroxyphenylserine on orthostatic hypotension in hemodialysis patients. Am J Nephrol. 2002;22:338–46.
Acknowledgements
We sincerely thank the following individuals: Ms. Changhong Li and Ms. Jie Xu for their contribution in the study organization and conduction; Zachary Miller for his help with language editing of the manuscript; and Dr. Qihao Guo for providing the Auditory Verbal Learning Test (AVLT) (Huashan Version).
Funding
This work was supported by a grant to Dr. Junwei Yang from the Jiangsu Science and Technology Department (BE2017762).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Part of this work was selected by the American Society of Nephrology to be presented at Kidney Week 2018. The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Liu, W., Wang, L., Huang, X. et al. Orthostatic blood pressure reduction as a possible explanation for memory deficits in dialysis patients. Hypertens Res 42, 1049–1056 (2019). https://doi.org/10.1038/s41440-019-0236-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0236-4
Keywords
This article is cited by
-
Postdialysis blood pressure is a better predictor of mortality than predialysis blood pressure in Japanese hemodialysis patients: the Japan Dialysis Outcomes and Practice Patterns Study
Hypertension Research (2020)
-
Ambulatory blood pressure profile and blood pressure variability in peritoneal dialysis compared with hemodialysis and chronic kidney disease patients
Hypertension Research (2020)