Abstract
Increased blood pressure (BP) variability (BPV) is associated with high cardiovascular risk in hemodialysis. Studies on the effects of antihypertensive drugs on BPV in hemodialysis are scarce. This study examines the effects of nebivolol and irbesartan on short-term BPV in patients with intradialytic hypertension. This randomized-cross-over study included 38 patients (age: 60.4 ± 11.1 years, male: 65.8%) with intradialytic hypertension (intradialytic-SBP increase ≥ 10 mmHg at ≥4 over 6 consecutive sessions). After the baseline evaluation, participants were randomized to nebivolol 5 mg and subsequently irbesartan 150 mg, or vice versa, with a two-week wash-out period before initiation of the second drug. Patients underwent three respective 24 h-ABPM sessions starting before a midweek-session. We calculated the standard deviation (SD), weighted SD (wSD), coefficient of variation (CV), and average real variability (ARV) of BP with validated formulas. The post-hemodialysis and 24 h-SBP and DBP levels were significantly lower after treatment with both drugs. The systolic-BPV indices were marginally lower after nebivolol but not after irbesartan compared to baseline (SD: baseline 15.70 ± 4.69; nebivolol 14.45 ± 3.37, p = 0.090; irbesartan 15.39 ± 3.85, p = 0.706; wSD: 14.62 ± 4.36 vs 13.40 ± 3.07, p = 0.053 vs 14.36 ± 3.47, p = 0.805, respectively). The diastolic-BPV indices decreased with nebivolol and increased with irbesartan, resulting in significant differences between the two drugs (SD: baseline 10.56 ± 2.50; nebivolol 9.75 ± 2.12; irbesartan 10.84 ± 1.98, between-drug p = 0.014; wSD: baseline 9.86 ± 2.12; nebivolol 9.34 ± 2.01; irbesartan 10.25 ± 2.01, between-drug p = 0.029). The diastolic-BPV during intradialytic and day-time periods was marginally lower with nebivolol than with irbesartan. During nighttime, the BPV indices were unchanged with either drug. The short-term BPV was reduced after nebivolol but not after irbesartan treatment in patients with intradialytic hypertension. These findings suggest that sympathetic-overdrive may be a major factor that affects BPV in intradialytic hypertension patients.
Similar content being viewed by others
Introduction
Hypertension is highly prevalent in patients with end-stage-renal-disease (ESRD) undergoing hemodialysis, with the prevalence estimated at 85% based on a recent report using ambulatory blood pressure monitoring (ABPM) in a large European hemodialysis cohort [1]. Most hemodialysis patients present a specific pattern of blood pressure (BP) changes, with BP progressively increasing during the interdialytic interval and rapidly decreasing during session [2]. However, approximately 5–15% of hemodialysis patients present an abnormal hemodynamic response to ultrafiltration with BP increasing during or immediately after sessions, a phenomenon known as “intradialytic hypertension” [3, 4].
In general, BP is characterized by high variability over time, including changes from beat-by-beat to visits spaced by weeks, months or years, under the effect of a complex homeostatic response of neural, vascular, humoral and rheological mechanisms to environmental, emotional and behavioral stimuli [5]. The wider availability of noninvasive home BPM and ABPM has made the assessment of one of the most important types of blood pressure variability (BPV) feasible, i.e., short-term and mid-term (during or between days) [6]. Data on short-term BPV in hemodialysis patients are limited. In a previous cross-sectional study of 160 hemodialysis patients, we showed that the BPV increased from Day 1 to Day 2 of a standard 2-day interdialytic interval [7]. Moreover, in a recent case-control study, we compared the 48-h BPV in patients with and without intradialytic hypertension and observed that while most BPV indices did not differ significantly between the two groups, patients with intradialytic hypertension exhibited sustained BP levels over the intradialytic interval [8].
Several studies have shown that short- and mid-term BPV is associated with cardiovascular events and mortality independently of BP levels in hypertensive individuals [9, 10], as well as in hemodialysis patients [11, 12]. For this reason, interventions to reduce BPV could be helpful to reduce adverse outcomes; this could be of particular importance in patients with intradialytic hypertension, as patients with this distinct BP phenotype have been suggested to exhibit a higher mortality risk compared to the average hemodialysis population [13]. Evidence regarding the effect of antihypertensive drugs on BPV derives from studies in essential hypertensives and suggests significant reductions of BPV with dihydropyridine calcium-channel-blockers (CCB), thiazides [14], olmesartan in combination with CCB and/or thiazides [15], or selective β1-adrenergic receptor blockers [16], with an opposite effect from non-selective β-blockers [17]. In hemodialysis patients, one study showed beneficial effects of dry-weight probing on BPV [18]. whereas evidence regarding drug effects is also scarce, with one Japanese study showing a beneficial effect of angiotensin II-receptor-blockers (ARBs) in hemodialysis and one study in peritoneal dialysis [19, 20]. To date, no study has evaluated the effect of pharmacological interventions on BPV in patients with interdialytic hypertension. We have previously shown that nebivolol and irbesartan, dosed acutely, significantly reduce post-hemodialysis SBP and have a beneficial trend in interdialytic and ambulatory BP in patients with intradialytic hypertension [21]. Thus, this study aimed to evaluate the effects of treatment with nebivolol and irbesartan on short-term BPV, using ABPM in this population.
Materials and methods
Study population
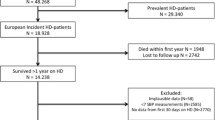
This study is a secondary analysis of a randomized cross-over study comparing the effects of nebivolol and irbesartan on BP in patients with intradialytic hypertension, as previously described in detail [21]. In brief, the inclusion criteria for patients to be eligible were: (1) age > 18 years; (2) ESRD treated with thrice-weekly maintenance hemodialysis for >3 months; and (3) presence of intradialytic hypertension, defined as intradialytic SBP increase ≥ 10 mmHg in ≥4 over 6 consecutive sessions. The exclusion criteria were: (1) existing comorbidity requiring treatment with RAAS-blockers or β-blockers (e.g., congestive heart failure, previous acute myocardial infraction, etc.); (2) existing contraindications to receive the previously described drug classes; (3) antihypertensive treatment with RAAS-blockers or β-blockers during one month prior to study enrollment; (4) pre- or post-hemodialysis SBP levels < 130 mmHg in 4 out of 6 sessions during the two weeks of the diagnosis of intradialytic hypertension; (5) nonfunctional arteriovenous fistula in the contralateral arm of the one used as vascular access for the hemodialysis that could interfere with proper ABPM; (6) active malignant disease or other advanced comorbidity resulting in particularly poor prognosis; or (7) inability to understand and provide written informed consent to participate in the study. The study protocol was approved by the Ethics Committee of the School of Medicine, Aristotle University of Thessaloniki. All evaluations were performed according to the Declaration of Helsinki (2013 Amendment). The study is registered with the ISRCTN registry (http://www.isrctn.com, Nr 13587185).
Study protocol
After the baseline evaluation, patients were randomly assigned to two different sequences of drug intake: (a) nebivolol 5 mg, 2-week washout period, irbesartan 150 mg or (b) irbesartan 150 mg, 2-week washout period, nebivolol 5 mg. These drugs were selected based on their known antihypertensive efficacy and the fact that they are not dialyzable during hemodialysis [22, 23]. Patients were unaware of the sequence and the specific substance of the two drugs administered. Moreover, two modes of drug administration were pre-specified to study the ability of administered agents to reduce BP when dosed acutely or not; i.e., the first 19 consecutive patients who entered the study received a single drug-dose one hour prior to the dialysis session, whereas the remaining 19 patients received the drug for a whole week before the evaluation. We chose to separately study these two modes of administration, as both single intake (before dialysis) or continuous intake are used in practice for patients with intradialytic hypertension, hence with scarce evidence on the effects of any antihypertensive agent on various BP parameters in this population. For the single-drug study, all tablets were administered by a single investigator, 1 h before the start of each hemodialysis session. For the weekly-dosing, the participants were supplied with 7 tablets of each studied drug, which were to be taken at the same time each day, matching the clock time of 1 h before dialysis start.
The participants were evaluated on 3 different time-points, all starting before the second weekly session (Wednesday or Thursday). The first time-point was the baseline evaluation. A period of 1 week took place between the baseline and the second evaluation, that with the first drug. A 2-week wash-out period took place before the initiation of the second drug in both occasions. The subjects with the single study intake were evaluated again 2-weeks after the second evaluation (total study time 3 weeks), whereas the participants with the weekly drug intake started the relevant drug after the two-week wash out period and were evaluated after another week (total study time 4 weeks). Predialysis blood specimens were sampled for routine tests. After blood sampling, 24-h ABPM started. The participants underwent their regular hemodialysis session, during which the volume withdrawal was programmed based on their dry weight, which was pre-specified by treating physicians, as previously described [21]. The dry weight, dialysate conductivity and background antihypertensive medications were not altered during the course of the study.
Ambulatory BP monitoring
ABPM was performed with the Mobil-O-Graph NG (IEM, Stolberg, Germany), an oscillometric device, which has a brachial BP-detection unit that has been validated according to standard protocols [24, 25] and was shown to provide practically identical values compared to a widely used ABPM device [26]. ABPM was fitted on the non-fistula arm, with a cuff of appropriate size, and lasted for 24 h. Patients were instructed to follow their usual activities and maintain their usual interdialytic weight gain until the next session. The device was monitoring BP every 20 min during the daytime (7:00–23:00) and every 30 min during the nighttime (23:00–7:00). Patients with invalid measurements, according to current guidelines [27], were invited to undertake the ABPM again in another week. To minimize the possible effect of manual BP measurements on BPV, only measurements recorded at the pre-specified time intervals at which the device was set to take measurements were used in this analysis.
Blood pressure variability parameters
The following BPV parameters of the brachial SBP and DBP were calculated based on the ambulatory recordings extracted from the Mobil-O-Graph device:
-
1.
The standard deviation (SD), calculated as: \(SD = \sqrt {\frac{1}{{{\mathrm{N}} - 1}}\mathop {\sum }\limits_{k = 1}^N ({\mathrm{BP}}_{{\mathrm{k}} + 1} - \overline {{\mathrm{BP}}} )^2}\); N, the number of valid BP measurements, and \(\overline {{\mathrm{BP}}}\), the average of ABPM readings.
-
2.
The coefficient of variation (CV), defined as the ratio of the SD to the mean BP and calculated as: \(CV = \frac{{{\mathrm{SD}}}}{{{\mathrm{mean}}\,{\mathrm{BP}}}} \times 100\).
-
3.
The weighted SD (wSD), defined as the average of the daytime and nighttime SD of BP, each weighted for the duration of the day- and nighttime periods, respectively, and calculated as: \(wSD = \frac{{\left( {{\mathrm{daytime}}\,{\mathrm{SD}}\,{\mathrm{x}}\,{\mathrm{daytime}}\,{\mathrm{hrs}}} \right) + ({\mathrm{nighttime}}\,{\mathrm{SD}}\,{\mathrm{x}}\,{\mathrm{nighttime}}\,{\mathrm{hrs}})}}{{24{\mathrm{hour}}\,{\mathrm{period}}}}\)
-
4.
The average real variability (ARV), defined as the average of the absolute differences between consecutive BP measurements and calculated as: \(ARV = \frac{1}{{{\mathrm{N}} - 1}}\mathop {\sum }\limits_{{\mathrm{k}} = 1}^{{\mathrm{N}} - 1} |{\mathrm{BP}}_{k + 1} - {\mathrm{BP}}_{\mathrm{k}}\); N, the number of valid BP measurements, and BPk, BP at measurement number k.
All BPV parameters were calculated for the period starting with the beginning of hemodialysis and included the subsequent first interdialytic day (i.e., 24-h period including dialysis or 20-h period outside dialysis period). The daytime period was between 07:00 and 22:59, and the nighttime period was between 23:00 and 06:59. For patients dialyzing in the first shift, the start of the 24-h period coincided with the start of the daytime period, including consecutive hours. For patients dialyzing in the second or third dialysis shifts, the daytime period did not include consecutive time (i.e., for a patient starting dialysis in the second shift at 12:00 noon, the daytime was considered the time between 12:00 and 22:59, followed by the time of the following morning between 07:00 and 11:59). The nighttime period was constant (23:00–06:59).
Statistical analysis
For the statistical analysis, we used the Statistical Package for Social Sciences 23 (SPSS Inc., Chicago, IL). Categorical variables are presented as absolute frequencies and percentages (n, %). Continuous variables are expressed as mean values ± standard deviation (SD) or median [interquartile range] according to the normality of the distribution with the Shapiro-Wilk test. Comparisons for continuous variables were performed with the paired Student’s t-test or the non-parametric Wilcoxon’s Signed Rank test, according to the normality of the distribution. For the purposes of this analysis, we have examined the effects of the two drugs on the BPV in the total population, as well as in the two sub-groups of different administration modes. A p value < 0.05 (two-tailed) was considered statistically significant.
Results
Baseline characteristics
Table 1 presents the baseline characteristics of the total study population. Thirty-eight hemodialysis patients (25 men and 13 women) with a mean age of 60.7 ± 11.1 years were included in this study. Of these patients, 19 consecutive patients received a single-dose and 19 patients received a weekly-dose of both administered drugs, with no significant differences between these two subgroups, as previously presented [21]. As shown in Tables 1, 26.3% had diabetes, 23.7% had dyslipidemia, 5.3% had peripheral vascular disease, 13.2% had coronary heart disease, 7.9% had heart failure, 5.3% had a history of stroke and 23.7% were smokers. After the baseline evaluation, 20 patients were randomized to receive irbesartan first and nebivolol second, while 18 patients received the reverse order. Following our exclusion criteria, no patient was receiving RAAS or β-blockers; 97.4% were on CCBs, 57.9% were on loop diuretics and 50% were on centrally active agents.
24 h BPV parameters after administration of nebivolol or irbesartan
Table 2 and Fig. 1 present the comparisons for the BPV indices between the baseline and nebivolol or irbesartan intake in the total population. The ultrafiltration rate was not different between the baseline and nebivolol, between the baseline and irbesartan intake, or between the two drugs. The study participants had significantly lower post-hemodialysis and 24-h systolic (SBP) and diastolic (DBP) BP levels after treatment with both drugs. No significant differences were identified between the two drugs for post-hemodialysis BP and 24-h BP, as shown in Table 2. With regards to comparisons with the baseline, the brachial SBP variability indices were tendentially lower after nebivolol treatment, in some cases with borderline significance, i.e., for SBP-SD (baseline: 15.70 ± 4.69; nebivolol: 14.45 ± 3.37 mmHg, p = 0.090) and SBP-wSD (baseline: 14.62 ± 4.36; nebivolol: 13.40 ± 3.07 mmHg, p = 0.053). In contrast, the 24-h systolic BPV indices were all slightly increased after irbesartan intake compared with the baseline. No significant differences between the two drug groups were observed for the 24-h systolic BPV. The brachial diastolic BPV indices were again slightly lower after nebivolol treatment and slightly increased after irbesartan treatment compared with the baseline. All 24-h DBP variability indices, with the exception of the 24 h-DBP ARV, were significantly decreased with nebivolol compared to irbesartan treatment (SD: 9.75 ± 2.12 vs 10.84 ± 1.98, p = 0.014; wSD: 9.34 ± 2.01 vs 10.25 ± 2.01, p = 0.029; and CV: 11.73 ± 3.00 vs 12.99 ± 2.97, p = 0.022, respectively). As expected, the 24-h heart rate was significantly lower with nebivolol compared with either baseline or irbesartan use. Furthermore, during dialysis, there were no episodes of hypotension, defined as SBP < 90 mmHg, at the baseline evaluation or with nebivolol or irbesartan use; during the interdialytic period, there were 0 episodes of SBP < 90 mmHg at the baseline, 1 episode with nebivolol and 4 episodes with irbesartan (p = 0.314 for between-drugs comparison).
The relevant comparisons for the 24-h BPV parameters in the two subgroups studied are presented in Table 3. In general, patients receiving a single dose of nebivolol had insignificantly lower and those who received a single dose of irbesartan had insignificantly higher systolic and diastolic BPV, compared to baseline. These effects were more prominent after weekly administration of either drug. Nebivolol treatment was associated with significantly lower SBP-SD levels (baseline: 16.26 ± 4.14, nebivolol: 14.45 ± 3.49 mmHg, p = 0.036) and marginally lower SBP-wSD and DBP-SD levels compared with baseline. The between treatment comparisons for the participants on a weekly intake revealed lower diastolic BPV indices levels with nebivolol compared to irbesartan treatment; i.e., DBP-SD: 9.81 ± 1.87 vs 11.25 ± 1.93 mmHg, p = 0.022; DBP-wSD: 9.49 ± 1.80 vs 10.63 ± 1.79 mmHg, p = 0.054; and DBP-CV 11.67 ± 2.70 vs 13.43 ± 2.81%, p = 0.013.
Changes in intradialytic BPV parameters after nebivolol or irbesartan
The changes in BPV during the intradialytic period in the total population studied are presented in Table 4. Nebivolol produced slightly decreased levels of systolic and diastolic BPV indices compared with the baseline evaluation. In contrast, irbesartan produced insignificantly higher systolic BPV and significantly higher DBP-SD (6.94 ± 2.50 vs 8.38 ± 3.86 mmHg, p = 0.034) and DBP-CV (8.04 ± 3.49 vs 9.77 ± 4.51%, p = 0.028) levels compared to baseline.
Day-time and nighttime BPV changes in the total population
Table 4 also includes comparisons of the systolic and diastolic BPV indices between the baseline and nebivolol or irbesartan treatment in the total population during the day-time and nighttime periods of the 24-h recording. During the daytime, all BPV indices were insignificantly lower after treatment with nebivolol, with the exception of the DBP-CV compared to baseline. In general, the systolic BPV indices were similar after irbesartan intake compared to baseline, but diastolic BPV indices were generally higher, particularly the DBP-CV (p = 0.064). Again, the DBP variability indices were borderline lower after nebivolol intake compared with irbesartan; i.e., DBP-SD, 9.57 ± 2.20 vs 10.49 ± 2.28 mmHg, p = 0.051, and DBP-CV, 11.42 ± 3.06 vs 12.50 ± 3.27%, p = 0.068. During the nighttime, no significant changes in the BPV parameters were observed after drug treatment compared with baseline, with the exception of the SBP-SD for nebivolol. With regards to the between-group comparisons, both the SBP-SD and SBP-CV were significantly lower with nebivolol compared with irbesartan intake.
Discussion
This study is a hypothesis-generating study aiming to explore for the first time changes in short-term BPV indices after treatment with nebivolol and irbesartan in patients with intradialytic hypertension. We have found that both drugs in both modes significantly decreased post-hemodialysis and the 24-h SBP and DBP levels. However, during the 24-h, intradialytic and daytime periods, nebivolol administration was associated with generally decreased and irbesartan intake was associated with increased BPV compared with baseline, although without significant differences in most comparisons. These effects were more prominent for the diastolic BPV indices and for patients on continuous administration of the two agents. Accordingly, the between-group comparisons for the two drugs revealed significantly decreased diastolic BPV indices after nebivolol treatment compared with irbesartan treatment. No differences were observed in the nighttime SBP or DBP variability for all comparisons.
The pathophysiology of intradialytic hypertension is complex and not fully elucidated [4]. Volume overload, an abnormal endothelial response (increased endothelin-1 and decreased endothelial-derived NO release), excess activation of the RAAS during dialysis due to rapid intravascular volume reduction with ultrafiltration, a post-hemodialysis positive sodium balance and increased serum ionized calcium levels, as well as acute removal of dialyzable antihypertensive drugs are among several factors underlying BP increase during sessions in this subset of hemodialysis patients [4, 28,29,30]. Alongside these factors, the activation of the sympathetic nervous system (SNS) during dialysis leading to stroke volume and/or peripheral vascular tone increase is another significant factor for the development of intradialytic hypertension [31]. On the other hand, increased central SNS drive and deregulated sympathetic cardiovascular modulation are considered among key factors for the variability in cardiovascular parameters, such as BP and heart rate [5, 32]. In a recent case-control study by our group, we compared 48-h BPV in patients with and without intradialytic hypertension and observed that most BPV indices did not significantly differ between the two groups, with all patients having high levels of BPV indices and patients with intradialytic hypertension exhibiting higher BP levels over the intradialytic interval [8]. Although there are no specific studies on the prominent determinants of BPV in patients with intradialytic hypertension, or hemodialysis in general, it could be hypothesized that SNS overdrive is a common mechanistic pathway for the occurrence of both intradialytic hypertension and increased BPV. [4, 32] Along this line, in the main analysis in this cohort of intradialytic hypertension patients, we showed that β1-selective blockade with nebivolol resulted in significantly lower post-hemodialysis noradrenaline levels compared with baseline in patients who received continuous treatment [21].
Studies examining the effects of antihypertensive agents in patients with intradialytic hypertension are scarce. In an old uncontrolled trial in 6 patients with intradialytic hypertension, 60 mg captopril prior to dialysis attenuated the BP increase during dialysis [33]. A non-randomized study showed that carvedilol (initial dose of 6.25 mg b.i.d. and titrated every week up to 50 mg) twice daily produced a significant reduction of 7 mmHg in the 44-hour SBP after 12 weeks of treatment [34]. In the primary analysis of the present protocol, which was the first controlled study in this subset of patients, we observed that both nebivolol and irbesartan were able to effectively reduce the post-dialysis BP (15.8/3.6 and 16.5/9.6 mmHg for weekly administration), with nebivolol being slightly more potent on the 24-hour BP (9.1/5.2 and 5.2/5.1 mmHg, respectively) [21].
Current evidence on the effect of antihypertensive drug treatment on BPV derived from observational studies [35], a post-hoc analysis of a clinical trial [36], systematic reviews and meta-analyses [14,15,16,17] in essential hypertensives suggests that dihydropyridine CCBs, diuretics and β1-selective agents, but not non-selective β-blockers, reduce the short- and long-term BPV compared to other antihypertensive classes. However, evidence regarding pharmacological interventions to reduce BPV in hemodialysis patients originates only from one study, in which 40 patients were randomly assigned to losartan or antihypertensive treatment with any antihypertensive agent other than RAAS blocker. The results of this study showed lower SBP and DBP-CV values for patients in the losartan group after 6 and 12 months, based on 24-h ABPM [19]. In another study, 45 peritoneal dialysis patients were randomized to candesartan, valsartan or any other antihypertensive agent (excluding RAAS blockers) with the results showing decreased SBP and DBP-SD values after 6 months for patients in the ARB-treatment groups [20]. Our findings are in general agreement with the aforementioned studies in the general population as we found that β1-selective blockade can effectively reduce 24-h, intradialytic and daytime systolic, but mostly diastolic BPV in patients with intradialytic hypertension, while treatment with RAAS blocker insignificantly increases the BPV despite the similar effect of the two agents on the post-dialysis and 24-h BP levels. Overall, our findings suggest that selective β1-blockers may be preferred antihypertensive agents in patients with intradialytic hypertension, since they are also able to reduce the BPV, which seems to be an additional cardiovascular risk factor in this population.
Furthermore, in the seminal HDPAL study, Agarwal et al. [37] randomized 200 hemodialysis patients with hypertension and left ventricular hypertrophy to lisinopril or atenolol, each administered three times per week after hemodialysis. In contrast to the primary hypothesis of the study and despite comparable reductions in the 44-h ambulatory BP and left ventricular mass in both groups, atenolol was superior to lisinopril in reducing cardiovascular outcomes (incidence of MI, stroke, heart failure and cardiovascular death). Although the HDPAL study included unselected hemodialysis patients, in the light of our present findings, one could hypothesize that improved BPV with β-blockade could be one of many mechanisms explaining the better outcome observed in hemodialysis patients under treatment with β-blockers.
This pilot study has strengths and limitations. It is based on a secondary analysis of the only randomized controlled study to date on the effects of antihypertensive drug treatment on ambulatory BP in patients with intradialytic hypertension. Moreover, a rigorous definition of intradialytic hypertension was used to precisely identify patients presenting this phenomenon. Additional strengths are the use of ABPM in three different occasions in every patient and the estimation of all modern short-term BPV indices. The main limitation of this study is the relatively small sample size, which is likely responsible for some of the observed associations being borderline significance or falling short of statistical significance. This is a common limitation of studies in the field, and our study is clearly the largest clinical study in patients with intradialytic hypertension. Furthermore, in an attempt to overcome limitations related to the relatively small sample size of our study, we have combined the data obtained in patients from the two pre-specified treatment modality groups (single or weekly drug administration, respectively). It is likely that considering only one group with a longer treatment period (i.e., 3 months) would have provided more solid findings.
In conclusion, this study showed that nebivolol treatment was associated with trends towards decreased 24-h, intradialytic and daytime systolic and diastolic BPV in patients with intradialytic hypertension. In contrast, irbesartan intake resulted in unchanged or in a tendentially increased BPV compared to baseline. These data resulted in significant differences between the effects of these two drugs on diastolic BPV, with a greater efficacy by nebivolol. These pilot findings indirectly support the hypothesis that increased SNS activity, which is present in patients with intradialytic hypertension, is one of the major factors leading to increased short-term BP fluctuations and that the use of β1-selective blockers may be effective in reducing BPV in these difficult-to-treat patients. Additional research efforts are warranted to fully elucidate whether BPV reductions may translate into long-term benefits in cardiac function and the reduction of cardiovascular events in hemodialysis patients.
References
Sarafidis PA, Mallamaci F, Loutradis C, Ekart R, Torino C, Karpetas A, et al. Prevalence and control of hypertension by 48-h ambulatory blood pressure monitoring in haemodialysis patients: a study by the European Cardiovascular and Renal Medicine (EURECA-m) working group of the ERA-EDTA. Nephrol Dial Transplant (epub ahead of print 10 July 2018; https://doi.org/10.1093/ndt/gfy147).
Karpetas A, Sarafidis PA, Georgianos PI, Protogerou A, Vakianis P, Koutroumpas G, et al. Ambulatory recording of wave reflections and arterial stiffness during intra- and interdialytic periods in patients treated with dialysis. Clin J Am Soc Nephrol. 2015;10:630–8.
Chazot C, Jean G. Intradialytic hypertension: it is time to act. Nephron Clin Pract. 2010;115:c182–188.
Georgianos PI, Sarafidis PA, Zoccali C. Intradialysis hypertension in end-stage renal disease patients: clinical epidemiology, pathogenesis, and treatment. Hypertension. 2015;66:456–63.
Parati G, Ochoa JE, Bilo G, Agarwal R, Covic A, Dekker FW, et al. Hypertension in chronic kidney disease part 2: role of ambulatory and home blood pressure monitoring for assessing alterations in blood pressure variability and blood pressure profiles. Hypertension. 2016;67:1102–10.
Sarafidis PA, Persu A, Agarwal R, Burnier M, de Leeuw P, Ferro CJ, et al. Hypertension in dialysis patients: a consensus document by the European Renal and Cardiovascular Medicine (EURECA-m) working group of the European Renal Association-European Dialysis and Transplant Association (ERA-EDTA) and the Hypertension and the Kidney working group of the European Society of Hypertension (ESH). Nephrol Dial Transplant. 2017;32:620–40.
Karpetas A, Loutradis C, Bikos A, Tzanis G, Koutroumpas G, Lazaridis AA, et al. Blood pressure variability is increasing from the first to the second day of the interdialytic interval in hemodialysis patients. J Hypertens. 2017;35:2517–26.
Bikos A, Angeloudi E, Memmos E, Loutradis C, Karpetas A, Ginikopoulou E, et al. A comparative study of short-term BP variability in hemodialysis patients with and without intradialytic hypertension. Am J Nephrol. 2018;48:295–305.
Hansen TW, Thijs L, Li Y, Boggia J, Kikuya M, Bjorklund-Bodegard K, et al. Prognostic value of reading-to-reading blood pressure variability over 24 h in 8938 subjects from 11 populations. Hypertension. 2010;55:1049–57.
Johansson JK, Niiranen TJ, Puukka PJ, Jula AM. Prognostic value of the variability in home-measured blood pressure and heart rate: the Finn-Home Study. Hypertension. 2012;59:212–8.
Chang TI, Flythe JE, Brunelli SM, Muntner P, Greene T, Cheung AK, et al. Visit-to-visit systolic blood pressure variability and outcomes in hemodialysis. J Hum Hypertens. 2014;28:18–24.
Sarafidis PA, Loutradis C, Karpetas A, Tzanis G, Bikos A, Raptis V, et al. The association of interdialytic blood pressure variability with cardiovascular events and all-cause mortality in hemodialysis patients. Nephrol Dial Transplant (e-pub ahead of print 03 September 2018, https://doi.org/10.1093/ndt/gfy247).
Inrig JK, Patel UD, Toto RD, Szczech LA. Association of blood pressure increases during hemodialysis with 2-year mortality in incident hemodialysis patients: a secondary analysis of the Dialysis Morbidity and Mortality Wave 2 Study. Am J Kidney Dis. 2009;54:881–90.
Webb AJ, Rothwell PM. Blood pressure variability and risk of new-onset atrial fibrillation: a systematic review of randomized trials of antihypertensive drugs. Stroke. 2010;41:2091–3.
Omboni S, Kario K, Bakris G, Parati G. Effect of antihypertensive treatment on 24-h blood pressure variability: pooled individual data analysis of ambulatory blood pressure monitoring studies based on olmesartan mono or combination treatment. J Hypertens. 2018;36:720–33.
Webb AJ, Fischer U, Rothwell PM. Effects of beta-blocker selectivity on blood pressure variability and stroke: a systematic review. Neurology. 2011;77:731–7.
Webb AJ, Fischer U, Mehta Z, Rothwell PM. Effects of antihypertensive-drug class on interindividual variation in blood pressure and risk of stroke: a systematic review and meta-analysis. Lancet. 2010;375:906–15.
Flythe JE, Kunaparaju S, Dinesh K, Cape K, Feldman HI, Brunelli SM. Factors associated with intradialytic systolic blood pressure variability. Am J Kidney Dis. 2012;59:409–18.
Mitsuhashi H, Tamura K, Yamauchi J, Ozawa M, Yanagi M, Dejima T, et al. Effect of losartan on ambulatory short-term blood pressure variability and cardiovascular remodeling in hypertensive patients on hemodialysis. Atherosclerosis. 2009;207:186–90.
Shigenaga A, Tamura K, Dejima T, Ozawa M, Wakui H, Masuda S, et al. Effects of angiotensin II type 1 receptor blocker on blood pressure variability and cardiovascular remodeling in hypertensive patients on chronic peritoneal dialysis. Nephron Clin Pract. 2009;112:c31–40.
Bikos A, Loutradis C, Aggeloudi E, Karpetas A, Raptis V, Kalaitzidis R, et al. The effects of nebivolol and irbesartan on postdialysis and ambulatory blood pressure in patients with intradialytic hypertension: a randomized cross-over study. J Hypertens (e-pub ahead of print 30 July 2018, https://doi.org/10.1097/HJH.0000000000001891).
Levin NW, Kotanko P, Eckardt KU, Kasiske BL, Chazot C, Cheung AK, et al. Blood pressure in chronic kidney disease stage 5D-report from a Kidney Disease: Improving Global Outcomes controversies conference. Kidney Int. 2010;77:273–84.
Ashley C and Currie A. The renal drug handbook. 3rd ed. Oxford, UK: Radcliffe Publishing; 2009.
Franssen PM, Imholz BP. Evaluation of the Mobil-O-Graph new generation ABPM device using the ESH criteria. Blood Press Monit. 2010;15:229–31.
Wei W, Tolle M, Zidek W, van der Giet M. Validation of the mobil-O-Graph: 24 h-blood pressure measurement device. Blood Press Monit. 2010;15:225–8.
Sarafidis PA, Lazaridis AA, Imprialos KP, Georgianos PI, Avranas KA, Protogerou AD, et al. A comparison study of brachial blood pressure recorded with Spacelabs 90217A and Mobil-O-Graph NG devices under static and ambulatory conditions. J Hum Hypertens. 2016;30:742–9.
Parati G, Stergiou G, O’Brien E, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014;32:1359–66.
Agarwal R, Light RP. Intradialytic hypertension is a marker of volume excess. Nephrol Dial Transplant. 2010;25:3355–61.
Chou KJ, Lee PT, Chen CL, Chiou CW, Hsu CY, Chung HM, et al. Physiological changes during hemodialysis in patients with intradialysis hypertension. Kidney Int. 2006;69:1833–8.
Movilli E, Camerini C, Gaggia P, Zubani R, Feller P, Poiatti P, et al. Role of dialysis sodium gradient on intradialytic hypertension: an observational study. Am J Nephrol. 2013;38:413–9.
Rubinger D, Backenroth R, Sapoznikov D. Sympathetic activation and baroreflex function during intradialytic hypertensive episodes. PLoS ONE. 2012;7:e36943.
Parati G, Esler M. The human sympathetic nervous system: its relevance in hypertension and heart failure. Eur Heart J. 2012;33:1058–66.
Bazzato G, Coli U, Landini S, Lucatello S, Fracasso A, Morachiello P, et al. Prevention of intra- and postdialytic hypertensive crises by captopril. Contrib Nephrol. 1984;41:292–8.
Inrig JK, Van Buren P, Kim C, Vongpatanasin W, Povsic TJ, Toto R. Probing the mechanisms of intradialytic hypertension: a pilot study targeting endothelial cell dysfunction. Clin J Am Soc Nephrol. 2012;7:1300–9.
Smith TR, Drozda JP Jr., Vanslette JA, Hoeffken AS, Nicholson RA. Medication class effects on visit-to-visit variability of blood pressure measurements: analysis of electronic health record data in the “real world”. J Clin Hypertens. 2013;15:655–62.
Rothwell PM, Howard SC, Dolan E, O’Brien E, Dobson JE, Dahlof B, et al. Effects of beta blockers and calcium-channel blockers on within-individual variability in blood pressure and risk of stroke. Lancet Neurol. 2010;9:469–80.
Agarwal R, Sinha AD, Pappas MK, Abraham TN, Tegegne GG. Hypertension in hemodialysis patients treated with atenolol or lisinopril: a randomized controlled trial. Nephrol Dial Transplant. 2014;29:672–81.
Funding
Dr. Athanasios Bikos received a scholarship from the Hellenic Society of Hypertension.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Loutradis, C., Bikos, A., Raptis, V. et al. Nebivolol reduces short-term blood pressure variability more potently than irbesartan in patients with intradialytic hypertension. Hypertens Res 42, 1001–1010 (2019). https://doi.org/10.1038/s41440-018-0194-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0194-2
Keywords
This article is cited by
-
Beta-blocker efficacy for intra- and interdialytic hypertension patients: a systematic review and meta-analysis
International Urology and Nephrology (2024)
-
Nebivolol is more effective than atenolol for blood pressure variability attenuation and target organ damage prevention in L-NAME hypertensive rats
Hypertension Research (2021)
-
Ambulatory blood pressure profile and blood pressure variability in peritoneal dialysis compared with hemodialysis and chronic kidney disease patients
Hypertension Research (2020)