Abstract
The lack of a decrease in nocturnal blood pressure is a risk factor for the progression of chronic kidney disease (CKD); however, it currently remains unknown whether it is a risk factor in normotensive CKD patients. We conducted a retrospective cohort study and enrolled 676 CKD patients who underwent ambulatory blood pressure monitoring (ABPM). According to their nocturnal blood pressure dipping pattern (>10%: dipper or <10%: non-dipper) and average 24-h systolic blood pressure (>130/80 mmHg: hypertension or <130/80 mmHg: normotension), patients were divided into four groups. The estimated glomerular filtration rate (eGFR) decline over 2 years and relevant clinical parameters were analyzed among groups. Among all participants, 82.7% were non-dippers and half of them were normotensive. The eGFR decline was the most rapid in hypertensive non-dipper patients (4.73 ± 0.45 ml/min/1.73 m2/2 years), and was not significantly different between normotensive non-dipper (1.31 ± 0.49 ml/min/1.73 m2/2 years) and dipper patients (1.69 ± 0.80 ml/min/1.73 m2/2 years). A multivariate regression analysis revealed that the amount of urinary protein (95% confidence interval (CI): 1.51–2.63), 24-h systolic blood pressure (95% CI 1.13–1.45), and eGFR (95% CI 1.02–1.44) were associated with a rapid eGFR decline. We conclude that, according to the ABPM-based analysis, a non-dipping blood pressure pattern in normotensive CKD patients does not predict the risk of a rapid decline in eGFR. This suggests that the control of blood pressure, rather than its circadian rhythm, is essential for the preservation of eGFR.
Similar content being viewed by others
Introduction
Due to an aging society and the high prevalence of patients with hypertension and diabetes mellitus (DM), the number of patients with chronic kidney disease (CKD) is increasing [1]. Previous epidemiological observations showed that CKD is a risk factor not only for developing end-stage kidney disease, but also cardiovascular diseases [2]. Various risk factors for alterations in kidney function in CKD patients have already been proposed [3], and high blood pressure (BP) is regarded as a strong predictor among these factors.
International guidelines from different organizations have highlighted the importance of lowering BP in CKD patients in order to prevent the progression of CKD as well as cardiovascular diseases [4,5,6,7]. However, the establishment of a target BP is still being debated, particularly the reliability or reproductivity of conventional clinical BP measurements, which most previous clinical trials used. Previous studies showed that BP measured outside the clinic, such as self-measurements at home or ambulatory BP monitoring (ABPM), correlated better with the incidence of cardiovascular diseases and the future decline of kidney function [8, 9]. In particular, nocturnal BP measured by ABPM is the strongest predictor of renal and cardiovascular events [10,11,12,13].
ABPM allows not only the detection of white-coat or masked hypertension, but also the classification of the daily BP profile [14]. BP generally decreases during nighttime, and is termed the “dipper” pattern; however, some populations exhibited less or an absence of dipping BP during nighttime, and, thus, it is termed the “non-dipper” pattern which is frequently observed in patients with CKD [15,16,17]. In addition, clinical observations showed that the non-dipper BP profile pattern, which is frequently complicated by a nocturnal high BP, predicted end-organ damage, including left ventricular hypertrophy [18] and urinary albumin excretion [19], a potent predictor of the progression of renal insufficiency [20].
However, due to the lack of sufficient evidence, particularly interventional clinical trials with ABPM-based controls, the target BP of ABPM has not yet been established. Furthermore, although the non-dipper BP pattern is regarded as a risk factor for the progression of kidney disease and cardiovascular diseases in CKD patients [21,22,23,24], it currently remains unclear whether a normotensive non-dipper pattern is still a risk factor for the progression of CKD. Given the recent studies demonstrating that non-dipping pattern of BP is associated with renal arteriosclerosis even in normotensive patients with IgA nephropathy, it is possible that normotensive non-dipper is a risk for developing kidney disease [25, 26]. In the present study, according to ABPM findings, i.e., 24-h BP values and BP dipping patterns, we divided CKD patients into four categories and compared the estimated glomerular filtration rate (eGFR) decline among these groups.
Materials and methods
Patients and study protocol
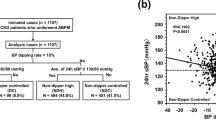
This is a retrospective cohort study that was conducted in the Omihachiman Community Medical Center in Shiga Prefecture, Japan. We consecutively enrolled 937 CKD patients who underwent ABPM between October 2006 and May 2014. CKD was diagnosed according to the criteria of the National Kidney Foundation defined as eGFR < 60 ml/min/1.73 m2 [27]. A total of 261 patients were excluded from the present study due to the lack of results for blood or urine examinations 6, 12, or 24 months after the ABPM procedure. As a result, 676 patients were recruited for this study (Fig. 1). All clinical characteristics were collected from medical records, including age, gender, complications, laboratory results, and the measurement of BP. eGFR was calculated according to the following formula, which was provided by the Japanese Society of Nephrology [28] “194 × [age (years)]−0.287 × [serum creatinine (mg/dl)]−1.094 × [0.739 if female]”. Body mass index (BMI) was calculated as [weight (kg)]/[height (meter)] [2]. We calculated eGFR decline from baseline in each group 6, 12, and 24 months after the ABPM procedure. The protocol for this study was approved by the Ethics Committee of the Omihachiman Community Medical Center. The entire protocol of this study was designed in accordance with the Declaration of Helsinki.
ABPM procedure and definition of BP profiles
ABPM devices (FB-270, Fukuda Denshi Co., Ltd., Tokyo, Japan) were fit between 15:00 and 16:00 and removed at 15:30 the next day. During the day (07:00–22:00), measurements were taken at 30-min intervals, whereas night measurements (22:00–07:00) were taken hourly.
The average 24-h BP was measured by ABPM. Non-dipper or dipper and high or low BP were classified by the guidelines submitted by American Heart association [4]. Non-dipper was defined when the average diurnal systolic BP (sBP) was not 10% higher than the average nocturnal sBP. Hypertension was defined when the average 24-h BP was higher than 130/80 mmHg (Fig. 1).
Statistical analysis
Data are expressed as the mean ± standard error (SE). Comparisons of two groups were performed by Welch’s t-test for continuous variables and by Fisher’s exact test for categorical variables. Multiple comparisons among the four groups were performed by the Steel-Dwass test for continuous variables and by the Bonferroni correction for categorical variables.
Multiple regression analyses were performed in order to assess variables associated with a faster eGFR decline using gender, age, the nocturnal sBP dipping rate, and factors considered to have a significant relationship. We defined the cutoff value as the mean value of the eGFR decline by aging in healthy Japanese adults aged 40 years or older [29]. We examined the relationship between the eGFR decline over 2 years and the sBP dipping rate or average 24 h, daytime and nighttime sBP using a linear correlation model. A P value <0.05 was considered to be significant. Statistical analyses were performed using JMP version 9.0.3 for Windows (SAS Institute Inc., Cary, NC, USA).
Results
High prevalence of the non-dipping BP profile in CKD patients
We consecutively enrolled 937 CKD patients who underwent ABPM between October 2006 and May 2014 (Fig. 1). Due to the lack of follow-up data 6, 12, or 24 months after ABPM, 261 patients were excluded from this analysis. The reasons for the loss of data were as follows: reaching end-stage renal disease for 73 patients, death by any cause for 25, lost to the follow-up during the observation period for 122, and lacking data at the indicated time points for 41. The baseline characteristics and ABPM profile of patients with end-stage renal disease and death during the observational period were summarized in Supplementary Table 1 and Supplementary Table 2. After the exclusion of these patients from the analysis, 676 patients were recruited in the present study (Fig. 1).
According to the general definition of dipper and ABPM-based hypertension as an average 24-h BP of higher than 130/80 mmHg [4], we divided 676 patients into four groups as follows: non-dipper with high BP (NDH 42.3%), non-dipper with low BP (NDL 40.4%), dipper with high BP (DH 6.1%), and dipper with low BP (DL 11.2%) (Fig. 1). The average nocturnal BP decline was 2.7 ± 7.8%, and a high prevalence of the non-dipping BP pattern (82.7%) was observed (Table 1).
Regarding the clinical characteristics of participants, no significant differences were observed in age, sex, renal function, hemoglobin values, or the usage rate of RAS inhibitors, diuretics, and β-blockers among each group (Table 2). The percentage of patients with DM, the usage rate of the calcium blocker, and values for the body mass index, serum calcium, and albumin were significantly lower in DL and NDL patients than in NDH patients. Regarding the urinary protein, one of the strong predictor of future eGFR decline in CKD patients, the NDH group exhibited the highest value (1.53 ± 0.13 g/day), and that of NDL group (0.54 ± 0.07 g/day) was similar to that of DL group (0.51 ± 0.13 g/day) were similar.
BP profiles in each group (Table 1) showed that the average sBP was similar in NDH and DH patients (143.9 ± 12.4 mmHg vs. 140.0 ± 8.8 mmHg, P = 0.16). The average sBP in DL and NDL patients were also similar (116.4 ± 9.3 mmHg vs. 116.9 ± 8.9 mmHg, P = 0.99). Due to the lack of a BP decline during the nighttime in non-dipper patients, the average nocturnal BP was significantly higher in NDH and NDL patients than in DH and DL patients, respectively.
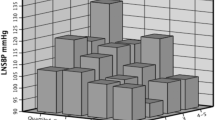
Non-dipping BP with appropriate controls does not accelerate the eGFR decline
Changes in eGFR from baseline were calculated 6, 12, and 24 months after the ABPM procedure. In the all patient analysis, eGFR decreased by 2.93 ± 0.30 ml/min/1.73 m2 during the observational period (Fig. 2a). In the separate analysis according to BP dipping and 24-h BP, a significant difference in the eGFR decline was observed between the NDH and normotensive groups (DL and NDL) 6 months after recruitment, and these differences became larger over the observational period (Fig. 2b). No significant difference was noted between the DL and NDL groups throughout the observational period. These results indicate that the 24-h BP value is more important for detecting the future progression of kidney disease. Of note, in contrast to previous findings showing the risk of the non-dipping BP profile on the progression of kidney disease [21], our results indicated that the normotensive non-dipper BP profile is not a risk factor for the progression of kidney disease.
Change in eGFR from baseline over the observational period. a Average eGFR in all patients gradually decreased over 2 years. b The separate analysis demonstrated that the eGFR decline was significantly more rapid in the NDH group than in the NDL group. Asterisks indicate P < 0.05 vs. NDH at each timepoint
Since a previous study demonstrated that the average eGFR decline rate in a Japanese general population was 0.36 ml/min/1.73 m2/year [29], we performed a logistic regression analysis adjusted by gender, age, the nocturnal BP decline rate, and factors considered to have a significant relationship with a faster eGFR decline than this value. The analysis identified the average 24-h sBP (95% CI 1.13–1.45), proteinuria (95% CI 1.51–2.63), and eGFR at baseline (95% CI 1.02–1.44) as significant factors associated with the worsening of eGFR (Fig. 3). We also examined the linear correlation between the eGFR decline over 2 years and BP dipping rate or average 24-h sBP. The eGFR decline correlated linearly with 24-h sBP (P < 0.001, r = 0.26, Fig. 4a), whereas no correlation was observed between the BP dipping rate and eGFR decline (P = 0.074, r = −0.069, Fig. 4b). Given the previous observational investigation demonstrating the nighttime BP was strongest correlation with future incidence of cardiovascular diseases [10,11,12], we further analyzed the linear relationship between the eGFR decline and average nighttime of daytime BP. eGFR decline correlated linearly with both nighttime and daytime BP (P < 0.0001, r = 0.251, P = 0.0001, r = 0.254, Suppl Fig) and there was no big difference between these linearities.
Discussion
CKD patients are more likely to exhibit a non-dipping BP profile pattern [15,16,17], as observed in our investigation. The non-dipper profile is a risk factor for the development of kidney disease [21]; however, it is challenging to normalize not only the actual BP value, but also its diurnal rhythm. Thus, our experiment was performed in order to elucidate the impact of the non-dipping BP pattern on the decline in kidney function in normotensives. Three major results were obtained in the present study: ABPM data in our analysis showed an extremely high prevalence of the non-dipping BP profile pattern in CKD patients. The non-dipping BP profile pattern did not predict future declines in kidney function in normotensive CKD patients. 24 h BP, rather than its circadian rhythm, is more important for predicting future eGFR decline.
Regarding the relationship between the BP diurnal rhythm and renal outcomes in normotensive subjects, few studies have focused only on urinary albumin excretion and the actual decline in kidney function remains unknown. Previous studies showed that the dipping BP pattern slightly correlated with the left ventricular mass index [30], but not with urinary albumin excretion [31, 32] in normotensives. Consistent with these findings, the present results showed that there was no significant difference in proteinuria between NDL and DL. Regarding the eGFR decline, previous studies demonstrated that nocturnal BP was the strongest predictor of the progression of kidney disease [19, 21, 22, 33]. In the present study, although average nocturnal BP was higher in the NDL group than in the DL group, no significant difference was noted in the eGFR decline between these groups. This result indicates that there is a certain threshold of nocturnal BP and that a lower BP than the threshold does not appear to be a risk factor for developing kidney disease; however, the present results did not provide an actual value for this.
Due to the lack of sufficient evidence, it currently remains unclear whether shifting the BP from non-dipper to dipper by the administration of anti-hypertensives potentiates renoprotective effects. Regarding the change in the BP profile, Crespo et al. showed that a bedtime hypertension treatment for CKD patients lowered the average nocturnal BP as well as the percentage of non-dipper patients [34]. Several clinical observations have revealed that normalizing the diurnal rhythm of BP by the administration of anti-hypertensives not only improved urinary albumin excretion for early diabetic kidney disease [35, 36], but also reduced the incidence of cardiovascular diseases [37,38,39]. However, concerning actual renal outcomes, only one study showed that ABPM-based BP control for pediatric CKD patients reduced the incidence of end-stage renal disease or ameliorated the eGFR decline [40]. Although our ABPM-based analysis is an observational investigation, the results obtained suggest that shifting from non-dipper to dipper in normotensive patients might not be beneficial for preventing the progression of kidney disease.
The present study includes several limitations. We only assessed ABPM once for each patient on recruitment. The reproducibility of ABPM is sometimes a limiting factor because ABPM itself disturbs the sleeping status and reduces daytime activity, which induces a higher nocturnal BP and lower daytime BP than usual. Previous studies showed that some individuals exhibited a different circadian BP pattern in serial ABPM, even with intervals of several weeks [41, 42]. The 48-h ABPM may reflect the BP status more reliably [43]; however, it is less convenient for usual clinical practice. In addition, because we did not assess BP control using ABPM or other methods for BP measurements at later time points during the observational period, the impact of BP control at the later time points on the future eGFR decline remains unclear.
Another limitation is the low prevalence of patients with the dipping BP pattern; the small sample size may have affected the significance of differences. Furthermore, although we found that the non-dipping profile in normotensive patients was not a risk factor for developing kidney disease, we did not provide the actual value of the risk threshold for BP. In order to establish a target BP, a prospective interventional study that includes multiple tests of ABPM is necessary. Previous studies showed that the self-measurement of home BP correlated well with ABPM and is an alternative method for predicting end-organ damage [8, 44]. However, the timing of BP measurements that precisely reflect the dipping BP pattern as well as the average values of BP during daytime and nighttime remains unclear.
Additionally, although a previous community-based cohort study demonstrated that the eGFR decline over 1 year was associated with an increased risk of end-stage renal disease [45], the eGFR decline over 2 years in our analysis may be less accurate for predicting future renal outcomes. Moreover, since it is impossible to calculate the precise eGFR decline rate, we excluded patients who progressed to end-stage renal disease or died during the observation period. Among these populations, there were a few DL patients, and a lower frequency of NDL patients and higher frequency of NDH patients than those in the main analysis were noted. Thus, although the results of the DL and NDL groups in the main analysis were not affected by this exclusion, we may have underestimated the eGFR decline rate in the NDH group. Since data collection in the present study was retrospective and the eGFR decline over only two years was a surrogate marker of future kidney dysfunction, prospective observations for a longer period using a hard endpoint such as end-stage renal disease, renal death, or a 40% increase in serum creatinine may be required to resolve this limitation.
In conclusion, according to our ABPM-based analysis, a non-dipping BP pattern in normotensive CKD patients does not predict a risk for a rapid decline in eGFR. In hypertensive CKD patients, the non-dipping BP pattern is a higher risk factor for developing kidney disease than in dipping patients. These results suggest that the control of BP, rather than its circadian rhythm, is essential for the preservation of eGFR. A larger scale study and longer period of observation are required in order to elucidate the impact of the diurnal rhythm of BP on the future prognosis of kidney disease in normotensives.
References
Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298:2038–47.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–305.
Yamagata K, Ishida K, Sairenchi T, Takahashi H, Ohba S, Shiigai T, et al. Risk factors for chronic kidney disease in a community-based population: a 10-year follow-up study. Kidney Int. 2007;71:159–66.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APHA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for The Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–19.
Group KDIGOKBPW. KDIGO clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int Suppl. 2012;2:337–414.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–20.
Gaborieau V, Delarche N, Gosse P. Ambulatory blood pressure monitoring versus self-measurement of blood pressure at home: correlation with target organ damage. J Hypertens. 2008;26:1919–27.
Bliziotis IA, Destounis A, Stergiou GS. Home versus ambulatory and office blood pressure in predicting target organ damage in hypertension: a systematic review and meta-analysis. J Hypertens. 2012;30:1289–99.
Dolan E, Stanton A, Thijs L, Hinedi K, Atkins N, McClory S, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension. 2005;46:156–61.
Staessen JA, Thijs L, Fagard R, O’Brien ET, Clement D, de Leeuw PW, et al. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. Systolic Hypertens Eur Trial Invest Jama. 1999;282:539–46.
Eguchi K, Pickering TG, Hoshide S, Ishikawa J, Ishikawa S, Schwartz JE, et al. Ambulatory blood pressure is a better marker than clinic blood pressure in predicting cardiovascular events in patients with/without type 2 diabetes. Am J Hypertens. 2008;21:443–50.
Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate E Loro Associazioni (PAMELA) study. Circulation. 2005;111:1777–83.
Gorostidi M, Sarafidis PA, de la Sierra A, Segura J, de la Cruz JJ, Banegas JR, et al. Differences between office and 24-hour blood pressure control in hypertensive patients with CKD: a 5,693-patient cross-sectional analysis from spain. Am J Kidney Dis: Off J Natl Kidney Found. 2013;62:285–94.
Andersen MJ, Khawandi W, Agarwal R. Home blood pressure monitoring in CKD. Am J Kidney Dis: Off J Natl Kidney Found. 2005;45:994–1001.
Mojon A, Ayala DE, Pineiro L, Otero A, Crespo JJ, Moya A, et al. Comparison of ambulatory blood pressure parameters of hypertensive patients with and without chronic kidney disease. Chronobiol Int. 2013;30:145–58.
Pogue V, Rahman M, Lipkowitz M, Toto R, Miller E, Faulkner M, et al. African American Study of Kidney D, Hypertension Collaborative Research G. Disparate estimates of hypertension control from ambulatory and clinic blood pressure measurements in hypertensive kidney disease. Hypertension. 2009;53:20–27.
Tochikubo O, Hishiki S, Miyajima E, Ishii M. Statistical base value of 24-hour blood pressure distribution in patients with essential hypertension. Hypertension. 1998;32:430–6.
Lurbe E, Redon J, Kesani A, Pascual JM, Tacons J, Alvarez V, et al. Increase in nocturnal blood pressure and progression to microalbuminuria in type 1 diabetes. N Engl J Med. 2002;347:797–805.
Perkins BA, Ficociello LH, Ostrander BE, Silva KH, Weinberg J, Warram JH, et al. Microalbuminuria and the risk for early progressive renal function decline in type 1 diabetes. J Am Soc Nephrol: Jasn. 2007;18:1353–61.
Davidson MB, Hix JK, Vidt DG, Brotman DJ. Association of impaired diurnal blood pressure variation with a subsequent decline in glomerular filtration rate. Arch Intern Med. 2006;166:846–52.
Minutolo R, Agarwal R, Borrelli S, Chiodini P, Bellizzi V, Nappi F, et al. Prognostic role of ambulatory blood pressure measurement in patients with nondialysis chronic kidney disease. Arch Intern Med. 2011;171:1090–8.
Agarwal R, Andersen MJ. Blood pressure recordings within and outside the clinic and cardiovascular events in chronic kidney disease. Am J Nephrol. 2006;26:503–10.
Salles GF, Reboldi G, Fagard RH, Cardoso CR, Pierdomenico SD, Verdecchia P, et al. Prognostic effect of the nocturnal blood pressure fall in hypertensive patients: the ambulatory blood pressure collaboration in patients with hypertension (ABC-H) meta-analysis. Hypertension. 2016;67:693–700.
Isobe S, Ohashi N, Ishigaki S, Tsuji N, Tsuji T, Kato A, et al. Increased nocturnal blood pressure variability is associated with renal arteriolar hyalinosis in normotensive patients with iga nephropathy. Hypertens Res: Off J Jpn Soc Hypertens. 2017;40:921–6.
Ohashi N, Isobe S, Matsuyama T, Ishigaki S, Tsuji N, Fujikura T, et al. Night-time activation of the intrarenal renin-angiotensin system due to nocturnal hypertension is associated with renal arteriosclerosis in normotensive IgA nephropathy patients. Hypertens Res: Off J Jpn Soc Hypertens. 2018;41:334–41.
National Kidney F. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis: Off J Natl Kidney Found. 2002;39:S1–266.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Imai E, Horio M, Yamagata K, Iseki K, Hara S, Ura N, et al. Slower decline of glomerular filtration rate in the Japanese general population: a longitudinal 10-year follow-up study. Hypertens Res: Off J Jpn Soc Hypertens. 2008;31:433–41.
Mezue K, Isiguzo G, Madu C, Nwuruku G, Rangaswami J, Baugh D, et al. Nocturnal non-dipping blood pressure profile in black normotensives is associated with cardiac target organ damage. Ethn Dis. 2016;26:279–84.
Soylu A, Yazici M, Duzenli MA, Tokac M, Ozdemir K, Gok H. Relation between abnormalities in circadian blood pressure rhythm and target organ damage in normotensives. Circ J: Off J Jpn Circ Soc. 2009;73:899–904.
Hoshide S, Kario K, Hoshide Y, Umeda Y, Hashimoto T, Kunii O, et al. Associations between nondipping of nocturnal blood pressure decrease and cardiovascular target organ damage in strictly selected community-dwelling normotensives. Am J Hypertens. 2003;16:434–8.
Tamura K, Yamauchi J, Tsurumi-Ikeya Y, Sakai M, Ozawa M, Shigenaga A, et al. Ambulatory blood pressure and heart rate in hypertensives with renal failure: comparison between diabetic nephropathy and non-diabetic glomerulopathy. Clin Exp Hypertens. 2008;30:33–43.
Crespo JJ, Pineiro L, Otero A, Castineira C, Rios MT, Regueiro A, et al. Administration-time-dependent effects of hypertension treatment on ambulatory blood pressure in patients with chronic kidney disease. Chronobiol Int. 2013;30:159–75.
Minutolo R, Gabbai FB, Borrelli S, Scigliano R, Trucillo P, Baldanza D, et al. Changing the timing of antihypertensive therapy to reduce nocturnal blood pressure in CKD: an 8-week uncontrolled trial. Am J Kidney Dis: Off J Natl Kidney Found. 2007;50:908–17.
Hermida RC, Calvo C, Ayala DE, Lopez JE. Decrease in urinary albumin excretion associated with the normalization of nocturnal blood pressure in hypertensive subjects. Hypertension. 2005;46:960–8.
Hermida RC, Ayala DE, Mojon A, Fernandez JR. Bedtime dosing of antihypertensive medications reduces cardiovascular risk in CKD. J Am Soc Nephrol: Jasn. 2011;22:2313–21.
Hermida RC, Ayala DE, Mojon A, Fernandez JR. Decreasing sleep-time blood pressure determined by ambulatory monitoring reduces cardiovascular risk. J Am Coll Cardiol. 2011;58:1165–73.
Hermida RC, Ayala DE, Mojon A, Fernandez JR. Influence of circadian time of hypertension treatment on cardiovascular risk: results of the mapec study. Chronobiol Int. 2010;27:1629–51.
Group ET, Wuhl E, Trivelli A, Picca S, Litwin M, Peco-Antic A, et al. Strict blood-pressure control and progression of renal failure in children. N Engl J Med. 2009;361:1639–50.
Agarwal R, Light RP, Bills JE, Hummel LA. Nocturia, nocturnal activity, and nondipping. Hypertension. 2009;54:646–51.
Elung-Jensen T, Strandgaard S, Kamper AL. Longitudinal observations on circadian blood pressure variation in chronic kidney disease stages 3–5. Nephrol, Dial, Transplant: Off Publ Eur Dial Transplant Assoc - Eur Ren Assoc. 2008;23:2873–8.
Hermida RC, Ayala DE, Fontao MJ, Mojon A, Fernandez JR. Ambulatory blood pressure monitoring: Importance of sampling rate and duration—48 versus 24 h—on the accurate assessment of cardiovascular risk. Chronobiol Int. 2013;30:55–67.
Stergiou GS, Argyraki KK, Moyssakis I, Mastorantonakis SE, Achimastos AD, Karamanos VG, et al. Home blood pressure is as reliable as ambulatory blood pressure in predicting target-organ damage in hypertension. Am J Hypertens. 2007;20:616–21.
Turin TC, Coresh J, Tonelli M, Stevens PE, de Jong PE, Farmer CK, et al. Short-term change in kidney function and risk of end-stage renal disease. Nephrol, Dial, Transplant: Off Publ Eur Dial Transplant Assoc - Eur Ren Assoc. 2012;27:3835–43.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Kado, H., Kusaba, T., Matoba, S. et al. Normotensive non-dipping blood pressure profile does not predict the risk of chronic kidney disease progression. Hypertens Res 42, 354–361 (2019). https://doi.org/10.1038/s41440-018-0155-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0155-9
Keywords
This article is cited by
-
Association between short-term blood pressure variability and target organ damage in non-dialysis patients with chronic kidney disease
BMC Nephrology (2024)
-
Nocturnal systolic blood pressure dipping and progression of chronic kidney disease
Hypertension Research (2024)
-
Relationship between renal function and blood pressure dipping status in renal transplant recipients: a longitudinal study
BMC Nephrology (2021)
-
Ambulatory blood pressure monitoring-based analysis of long-term outcomes for kidney disease progression
Scientific Reports (2019)