Abstract
It remains unknown which surrogate markers can predict diagnostic test results for primary hyperaldosteronism (PA). The Secondary Hypertension Registry Investigation in Mie Prefecture (SHRIMP) study has sequentially and prospectively recruited 128 patients with hypertension with an aldosterone-to-renin ratio (ARR) greater than 20, evaluated the differences among essential hypertension (EHT), idiopathic hyperaldosteronism (IHA), and aldosterone-producing adenoma (APA), and analyzed the predictors for the confirmatory tests. The patients underwent saline-loading, captopril-challenge, and upright furosemide-loading tests. Carotid, renovascular, and cardiac echography, brachial ankle pulse wave velocity (baPWV), endothelial function, nocturnal blood pressure decline, and the apnea hypopnea index were evaluated. Multivariate regression analyses showed that the plasma aldosterone concentration (PAC) at screening was a strong predictor of the saline and captopril test results. The plasma renin activity (PRA) at screening, urine β2-microglobulin, and left ventricular mass index (LVMI) were independent predictors for the captopril test. The estimated saline PAC and captopril 60 and 90 min ARRs predicted by the equations were highly correlated with the real values. The ROC curve analysis showed PAC at screening among each of predictors for the diagnostic tests and PAC after the saline-loading test had the highest diagnostic abilities of APA. Patients with IHA were older and had glucose intolerance and increased U-Alb/gCre and resistive indices. In patients with APA, the levels of U-Alb/gCre and urine β2-microglobulin were increased, and levels of insulin and the HOMA-IR were decreased. In conclusion, our proposed equations may be useful for estimating saline PAC and captopril ARR. Diagnostic predictors may differ for each confirmatory test.
Similar content being viewed by others
Introduction
Recently, primary aldosteronism (PA) has been a focus of interest because it is the most frequent cause of secondary hypertension and accounts for more than 10% of all patients with hypertension in cross-sectional and prospective studies [1]. Patients with PA suffer from cardiovascular events more frequently than patients with essential hypertension (EHT) and comparable blood pressure [2]. PA is a heterogeneous entity that is characterized by hypertension, aldosterone overproduction, and inhibition of renin activity. The major subgroups are idiopathic hyperaldosteronism (IHA), also known as bilateral adrenal hyperplasia, and aldosterone-producing adenoma (APA). Previously, APA was considered the major form of PA because it was easier to detect due to the existence of an adrenal tumor and the higher prevalence of hypokalemia [3]. However, IHA has been recognized recently as a major form of PA, accounting for more than 60% of PA cases [4]. Thus, diagnosing PA and effectively dividing it into its subgroups is important in hypertensive patients with or without an adrenal tumor [3].
The differences in surrogate markers in cardiovascular diseases compared with those of EHT and which surrogate markers should be checked and followed carefully to prevent cardiovascular events in patients with IHA and APA are unknown. Furthermore, the determinants of the results of confirmatory tests for the diagnosis of PA are not known. The Secondary Hypertension Registry Investigation in Mie Prefecture in Japan (SHRIMP) study has sequentially and prospectively recruited patients with hypertension with an aldosterone-to-renin ratio (ARR) greater than 20, evaluated differences among EHT, IHA, and APA, and evaluated the predictors of confirmatory test results in these patients.
Methods
Study population
The SHRIMP study protocol was approved by the Ethics Committee of Mie University Hospital (reference no. 2903), and written informed consent was obtained from all patients participating in the study.
Hypertension was diagnosed by three consecutive BP measurements taken in the sitting position using a mercury sphygmomanometer according to the Japan Society of Hypertension guidelines [5].
Consecutive patients with hypertension and an ARR ratio greater than 20 who were prescribed only calcium channel antagonists and/or alpha-blockers as antihypertensive drugs were prospectively recruited from Mie University Hospital from 2012 to 2018. Generally, we add alpha-blockers to the calcium channel antagonists when hypertensive control is inadequate. All patients underwent confirmatory tests and imaging for the diagnosis of PA. The Japan Society of Hypertension (JSH) and the Japan Endocrine Society (JES) recommend three confirmatory tests: the captopril-challenge test, the saline-loading test, and the upright furosemide-loading test [5, 6]. In the captopril-challenge test, the ARR is measured 60 and 90 min after oral administration of 50 mg of captopril; the cut-off value is an ARR > 20 (Supplementary Table 1). In the saline-loading test, after intravenous infusion of 2 L of saline over 4 h, the plasma aldosterone concentration (PAC) is measured; the cut-off value is a PAC > 6.0 ng/dl. In the upright furosemide-loading test, the plasma renin activity (PRA) is measured after 2 h of standing (walking is permitted) following intravenous injection of 40 mg of furosemide; the cut-off value is PRA < 2.0 ng/mL/h. Supplementary Table 1 shows the similarities and differences in the screening and confirmatory tests in Japan [6], the USA [1], Canada [7], and France [8].
Adrenal venous sampling
Adrenal venous sampling (AVS) was performed via the femoral vein approach. Blood samples were obtained from the inferior vena cava (IVC) and the right and left adrenal veins. Successful AVS was determined by a cortisol concentration in the adrenal vein greater than 200 μg/dl after synthetic adrenocorticotropic hormone (ACTH) stimulation [6]. For each sample, the aldosterone concentration was divided by the cortisol concentration to correct for dilutional effects of adrenal vein drainage. The APA diagnosis was based on the assumption that the ratio of dominant to nondominant normalized aldosterone (lateralized ratio) would be 4 or greater, the aldosterone concentration would be more than 1400 ng/dl after ACTH stimulation, and the nondominant normalized aldosterone would be less than or equal to the normalized aldosterone in the IVC. To meet the definition of IHA, at least one of the adrenal venous blood aldosterone measurements is greater than 1400 ng/dl and the lateralized ratio is less than 4 after ACTH stimulation.
Renal, cardiac, and carotid artery ultrasonography
First, the renal aortic ratio (RAR) was determined after the flow velocities in the aorta and renal arteries were evaluated to rule out morphological abnormalities or renal artery stenosis. Second, the renal resistive index (Rl) was determined in the interlobar arteries of both kidneys and expressed as the mean of these values. The digital diagnostic ultrasound systems used were the Aplio XG SSA-790A with a PVT-375BT convex array transducer (Toshiba Medical Systems, Otawara, Tochigi, Japan) operating at a frequency of 3.5 MHz and the LOGIQ P6 with a 4C convex array transducer (GE Medical Systems, Milwaukee, WI, USA) operating in the frequency range of 4.0–5.5 MHz. The ultrasound examinations were performed by two well-trained technicians. The renal RI was calculated as follows: renal RI = (peak systolic velocity − end-diastolic velocity)/peak systolic velocity [9].
Cardiac ultrasonography was performed using the Vivid 7 (GE-Vingmed Ultrasound AS, Horten, Norway). The interventricular septal and left ventricular (LV) posterior wall thicknesses (IVST and PWT), LV end-diastolic dimension (LVEDD), LV end-systolic dimension (LVESD), and fractional shortening were assessed from the parasternal long-axis view. The LV volume indices and ejection fraction were assessed using the biplane Simpson’s rule. The LV mass index (LVMI) was normalized by the body surface area from the LV mass calculated as follows: LV mass (g) = 0.8{1.04[([LVEDD + IVST + PWT]3 – LVEDD3)]} + 0.6. The ratio of the peak early to late diastolic transmitral flow velocity (mitral E/A) and the deceleration time (DT) of the E velocity were calculated using pulsed Doppler echocardiography. The averaged peak early diastolic mitral annular velocity (E’) at the inferior-septal and LV lateral site was used as a marker of the LV diastolic function. The E/E’ ratio was calculated as a Doppler parameter reflecting the LV filling pressure.
Carotid artery echography was performed using high-resolution, real-time ultrasonography with an 11–12 MHz transducer (GE Logic S8). The carotid artery intima media thickness (IMT) was defined as the distance from the leading edge of the first echogenic line to the leading edge of the second echogenic line on a sonographic image. The IMT and the vascular thickness were determined at one site and at two additional points located 1 cm downstream and upstream [10]. The mean of these three determinations was taken as the IMT value. The IMT was measured in both the right and left carotid arteries. The max IMT was defined based on six IMT measurements.
Other physiological studies: ABI, AHI, RHI, and ABPM
The ankle brachial pressure index (ABI) and brachial ankle pulse wave velocity (baPWV) were obtained using a BP-203RPE III (Fukuda Colin, Tokyo, Japan).
The apnea hypopnea index (AHI) was obtained using an SAS-3200 (Nihon Kohden, Tokyo, Japan) according to the manufacturer’s protocol. Moderate to severe SAS was defined as an AHI ≥ 15 [11].
Reactive hyperemia signals were obtained using the EndoPAT 2000 device (Itama Medical Inc., Caesarea, Israel), which was validated and used previously to assess the peripheral arterial tone. Endothelial function was measured via the RH-PAT index [12] using the manufacturer’s protocol. Generally, an RHI cut-off < 1.67 has been used to indicate endothelial dysfunction.
Ambulatory blood pressure monitoring (ABPM) recordings were performed using a validated device (Oscar 2 Classic; Suntech Medical Inc., Morrisville, NC, USA). The overnight reduction in systolic blood pressure was automatically calculated.
Statistics
The data are reported as the means ± standard deviations (SDs) of the mean. A value of P < 0.05 was considered significant. One-way analysis of variance or the chi-square test was used to compare the baseline characteristics. For post hoc analysis, Tukey’s honestly significantly different test, the Games–Howell test or the Mann–Whitney test was used. Multivariate regression analyses were performed to identify factors from among the risk factors and laboratory data that were associated with PAC, ARR, and PRA at screening and in the definitive diagnostic tests. Linear correlations between the variables were parametrically evaluated using Pearson’s product moment correlation coefficient. Receiver operating characteristic (ROC) analysis was performed to evaluate the diagnostic ability. The optimal cut-off points of each predictor were set at the closest point to the upper left corner of the ROC curve plot. The data were processed using the SPSS version 21 software (IBM Inc., Chicago, IL, USA).
Results
Patient characteristics
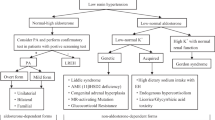
In this study, 128 hypertensive patients with an ARR greater than 20 were recruited (Fig. 1). In Japan, generally confirmatory tests are performed after screening and finding an ARR > 20, including the saline-loading test, captopril-challenge test, and upright furosemide-loading test, each of which has its own threshold (Supplementary Table 1) [1, 6,7,8]. After undergoing 2 or 3 confirmatory tests, 101 patients were diagnosed with PA. Computed tomography scanning showed an adrenal tumor in 47 patients. AVS was not performed in nine patients with PA and an adrenal tumor, and two AVS tests were not diagnostic (Fig. 1). Additionally, AVS was not performed in 15 patients with PA and no adrenal tumor. Figure 1 shows the PA subtypes, including 27 EHT, 59 IHA, and 16 APA analyzed cases. Table 1 shows the characteristics of the patients in the three groups. The mean ages were 57, 57, and 52 years in the EHT, IHA, and APA groups, respectively. Significant differences among the three groups were observed in serum potassium, PAC, the ARR, the PAC after the saline-loading test, the PRA after the upright furosemide-loading test, the ARR 60 and 90 min after the captopril-challenge test, and the prevalence of an adrenal tumor (Table 1 and Fig. 2). Subclinical Cushing’s syndrome was observed only in patients with IHA and APA. No differences were found in age and the systolic and diastolic blood pressures under hypertensive medication. The duration of hypertension was longer in the patients with IHA than in those with EHT. Alpha-blockers were added to the calcium antagonists to control blood pressure more frequently in the APA group than in the EHT group (Table 1).
Study flow chart. A final subtype diagnosis was achieved by CT and adrenal vein sampling in 102 patients. APA aldosterone-producing adenoma, ARR aldosterone-to-renin ratio, AVS adrenal vein sampling, CT computed tomography, EHT essential hypertension, IHA idiopathic hyperaldosteronism, PAC plasma aldosterone concentration, PRA plasma renin activity
PAC and ARR in EHT, IHA, and APA patients. Dot plot showing the distribution of the PAC (a) and ARR (b) with the mean value ± SD. *P < 0.05 vs. EHT, **P < 0.05 vs. IHA. APA aldosterone-producing adenoma, ARR aldosterone-to-renin ratio, EHT essential hypertension, IHA idiopathic hyperaldosteronism, PAC plasma aldosterone concentration
Among the three groups, the IVST and LVMI were higher in the APA group than in the EHT group (Table 2). Conversely, the RAR and RI was significantly higher in the patients with IHA than in those with EHT (Table 2). In the laboratory measurements, fasting glucose, HbA1c, and the urine albumin to creatinine ratio (U-Alb/gCre) were higher in the patients with IHA than in those with EHT (Table 3). The levels of insulin and the HOMA-IR were lower in the APA group than in the IHA group.
Predictors for the PAC, PRA, and ARR at screening
Univariate and multivariate regression analyses were performed to identify determinants of the PAC, PRA, and ARR at screening for PA in EHT, IHA, and APA patients (Table 4). The addition of alpha-blockers was the strongest predictor of the PAC after adjusting for the ABI, IVST, PWT, LVMI, HbA1c, prevalence of an adrenal tumor, and serum potassium.
DBP was the only predictor of the PRA at screening after adjusting for weight, SBP, RAR, and homeostasis model assessment insulin resistance (HOMA-IR) (Table 4).
The addition of alpha-blockers was an independent predictor of the ARR at screening in the EHT, IHA, and APA patients after adjusting for the IVST, serum potassium, HbA1c, and prevalence of an adrenal tumor (Table 4).
These results suggest that the PAC, PRA, and ARR at screening can be determined by different predictors.
Predictors of the PAC after the saline-loading test, the ARR 60 and 90 min after the captopril-challenge test, and the PRA after the upright furosemide-loading test
Next, univariate and multivariate regression analyses were performed to identify the determinants of the PAC after the saline-loading test, the ARR 60 and 90 min after the captopril-challenge test, and PRA after the upright furosemide-loading test in the EHT, IHA, and APA patients (Table 5). The PAC at screening, ARR at screening, and serum potassium were independent predictors of the PAC after the saline-loading test after adjusting for male sex, PRA, IVST, PWT, LVDs, LVMI, E/E’, urine β2-microglobulin, the prevalence of an adrenal tumor and ischemic heart disease and the addition of alpha-blockers.
The PAC and PRA at screening, LVMI and urine β2-microglobulin were independent predictors of the ARR 60 min after the captopril-challenge test in the EHT, IHA, and APA patients after adjusting for male sex, ABI, the ARR at screening, serum potassium, RV5 + SV1 in the ECG, IVST, PWT, LVMI, HbA1c, U-Alb/gCre, the prevalence of an adrenal tumor and chronic kidney disease, and the addition of alpha-blockers (Table 5). Similar results were obtained regarding independent predictors of the ARR 90 min after the captopril-challenge test (Table 5).
The renal RI was the only predictor of the PRA after the upright furosemide-loading test in all patients after adjusting for the baPWV, PAC, ARR at screening, E/E’, HbA1c, HOMA-IR, and addition of alpha-blockers (Table 5).
These results suggest that the PAC after the saline-loading test, the ARR after the captopril-challenge test, and the PRA after the upright furosemide-loading test can be determined by different predictors.
Finally, we examined whether the four equations obtained from the multivariate regression analysis of surrogate markers could estimate the PAC after the saline-loading test, the 60 and 90 min ARRs after the captopril-challenge test, and the PRA after the upright furosemide-loading test. The equations were as follows: (1) saline PAC = 13.3 + 0.485*PAC−3.38*K + 0.024*ARR; (2) 60 min ARR = −46.92 + 0.0363*β2-microglobulin + 4.302*PAC + 0.5815*LVMI−108.7*PRA; (3) 90 min ARR = −35.01 + 0.0708*β2-microglobulin + 3.631*PAC + 0.3746*LVMI−90.0*PRA; and (4) furosemide PRA = 3.855−4.342*RI. The estimated saline PAC and the captopril 60 and 90 min ARRs were highly correlated with the real saline PAC and the captopril 60 and 90 min ARRs (r = 0.800, P < 0.000001; r = 0.833, P < 0.000001; and r = 0.898, P < 0.000001, respectively; Fig. 3a–c). However, the estimated PRA after the upright furosemide-loading test was only mildly correlated with the real values (r = 0.361, P < 0.001), and the values were underestimated compared with the real values (Fig. 3d).
Scatterplots showing the relationships between the real values and estimated values calculated by surrogate markers for each diagnostic test. a Estimated and real PAC after the saline-loading test, b, c estimated and real ARR after the captopril-challenge test, and d estimated and real PRA after the upright furosemide-loading test. APA aldosterone-producing adenoma, ARR aldosterone-to-renin ratio, captopril 60 or 90 min ARR ARR 60 or 90 min after the captopril-challenge test, EHT essential hypertension, IHA idiopathic hyperaldosteronism, PAC plasma aldosterone concentration, saline PAC PAC after the saline infusion test, PRA plasma renin activity, furosemide PRA PRA after the upright furosemide-loading test
Diagnostic ability of the APA with the PAC, PRA and ARR at screening, serum potassium, LVMI, urine β2-microglobulin, and RI and each of confirmatory tests
ROC curve analyses based on the areas under the ROC curves (AUCs) were performed to compare the diagnostic abilities of each of the predictors for the confirmatory tests and the PAC, ARR, and PRA in each of the diagnostic tests (Table 6 and Fig. 4). In these indices, the PAC values at screening and after the saline-loading test were demonstrated to have the highest diagnostic abilities, with AUCs of 0.851 and 0.908 at cut-off values of 21.6 and 15.2 ng/dl, respectively; these values corresponded to sensitivities of 75.0 and 90.0% and specificities of 80.2 and 90.0%, respectively (Table 6).
Receiver operating characteristic (ROC) curves for analysis of the diagnostic value of each predictor for differentiation of APA patients from patients with EHT and IHA with an ARR greater than 20. APA aldosterone-producing adenoma, ARR aldosterone-to-renin ratio, captopril 60 or 90 min ARR ARR 60 or 90 min after the captopril-challenge test, EHT essential hypertension, IHA idiopathic hyperaldosteronism, LVMI left ventricle mass index, PAC plasma aldosterone concentration, saline PAC PAC after the saline infusion test, PRA plasma renin activity, furosemide PRA PRA after the upright furosemide-loading test, RI resistive index, ABI ankle brachial index, ABPM ambulatory blood pressure monitoring, ACTH adrenocorticotropic hormone, AHI apnea and hypopnea index, ARR aldosterone-to-renin ratio, AUC area under the ROC curves, AVS adrenal venous sampling, baPWV brachial ankle pulse wave velocity, BNP brain natriuretic peptide, DM diabetes mellitus, ECG electrocardiography, eGFR estimated glomerular filtration rate, HOMA-IR homeostasis model assessment insulin resistance, IHA idiopathic hyperaldosteronism, IMT intima medial thickness, IVST interventricular septal wall thickness, LAD left atrial dimension, LVMI left ventricle mass index, PAC plasma aldosterone concentration, PRA plasma renin activity, PWT posterior wall thickness, RAR renal aortic ratio, RHI reactive hyperemia index, RI resistive index, ROC receiver operating characteristic, U-Alb/gCre urine albumin to gram creatinine ratio
Discussion
A total of 128 consecutive hypertensive patients with an ARR > 20 were recruited, of whom 102 patients, including 27 EHT, 59 IHA, and 16 APA cases, were analyzed (Fig. 1). The PAC at screening was found to be a strong independent predictor of the results of two representative confirmatory tests for PA: the saline-loading test and the captopril-challenge test (Table 5). Conversely, the renal RI was the only independent predictor of the upright furosemide-loading test result (Table 5). This test is not usually used in the USA and European countries, but a significant elevation of the aldosterone concentration (>1400 ng/dl [6] after stimulation by adrenocorticotropic hormone, ACTH) was observed in all patients who underwent adrenal venous sampling after diagnosis with PA by a positive result only in the upright furosemide-loading test (data not shown). Thus, the determinants can differ among confirmatory examinations.
Left ventricular hypertrophy is a well-known surrogate marker for cardiovascular events caused by hypertension [13]. Indeed, the IVST and LVMI were increased in APA compared with EHT patients (Table 2). This increase was not accompanied by the diagnostic criteria for LVH on the ECG (Table 2). Furthermore, LVMI was an independent predictor of the ARR 60 and 90 min after the captopril-challenge test in all patients (Table 5). LVH leads to a decreased E’ wave velocity, LA dilatation, and E/E’ elevation via diastolic dysfunction [14]. Indeed, the univariate regression analysis showed that E/E’ was a predictor for the PA confirmatory test results, including the saline-loading test and the upright furosemide-loading test (Table 5). Yang et al. reported that PA patients had a higher E/E’ than EHT patients despite having similar LV dimensions and wall thicknesses [15]. We observed that the E/E’ was more increased in APA than in EHT and IHA patients with marginal significance (p = 0.10, Table 2). Thus, diastolic dysfunction may progress earlier in APA than in IHA patients. These results may be of interest, given that PA patients have a higher prevalence of AF, with an adjusted odds ratio of 5.0 in a controlled cross-sectional study [16].
Urinary excretion of proteins, such as albumin and β2-microglobulin, is known to be a renal surrogate marker of hypertension [17]. How PA induces renal damage is unknown, but mineralocorticoid receptor blockers have been shown to prevent the progression of mild-to-moderate chronic kidney disease [18]. U-Alb/gCre was more increased in the APA and IHA patients than in the EHT patients (Table 3). The level of β2-microglobulin was more increased in the APA group than in the IHA and EHT groups and was an independent predictor of the ARR 60 and 90 min after the captopril-challenge test (Table 5). Interestingly, for the PA diagnostic test, urine β2-microglobulin was a stronger predictor than albumin (Table 5). Thus, measuring the urinary excretion of both albumin and β2-microglobulin is important when evaluating the possibility of PA in hypertensive patients.
Renal vascular flow estimated by the RI and RAR is also important when assessing hypertensive renal organ damage in patients with hypertension [19]. An increased RI has been reported to be associated with an increased risk of cardiovascular and renal events in hypertensive patients [20]. The RI was an independent predictor of the PRA results after the upright furosemide-loading test (Table 5). The RI was higher in IHA patients than in those with EHT (Table 2). An increased RI and RAR without renal arterial stenosis leads to glomerular hyperfiltration. Indeed, in patients with PA, urinary albumin excretion has been reported to occur in association with a state of decreased intrarenal vascular resistance and glomerular hyperfiltration resulting from aldosterone-induced sodium retention [21]. Furthermore, recently RI was reported to be an independent predictor of blood pressure in patients with APA after adrenalectomy [22]. Therefore, we should assess and follow-up renal vascular flow in patients with PA.
The fasting glucose level was significantly higher in the IHA than in the EHT and APA patients (Table 3), and HbA1c and the prevalence of DM were higher in the IHA than in the EHT patients with marginal significance (Tables 1 and 3). These results are consistent with previous reports [23, 24]. In addition, the prevalence of PA has been reported to be higher in patients with DM [25]. However, these diabetic parameters were predictors of the upright furosemide-loading confirmatory test for the diagnosis of PA only in the univariate analysis (Table 5). Thus, further studies are needed to evaluate why and when DM is associated with PA.
The relationships of endothelial dysfunction as indicated by the RHI in the EndoPAT and sleep apnea syndrome as indicated by the AHI or nocturnal blood pressure dips, which have been reported to contribute to PA, with the confirmatory tests for PA were also examined [26, 27]. However, in this study, no relationships of these markers with the PAC, PRA, and ARR at screening and in the confirmatory tests were found (Tables 4 and 5). Further studies are necessary to show the relationships between PA and these conditions.
The ROC curve analysis showed that the PAC at screening among each of predictor for the diagnostic tests of PA and the PAC after the saline-loading test among each of the diagnostic tests had the highest diagnostic abilities for APA. The optimal cut-off points of 21.6 and 15.2 ng/dl may be useful. Interestingly, a recent report indicated that circadian variation in the PAC and the PAC at 6 a.m. had the highest diagnostic abilities for unilateral hyperaldosteronism from IHA, with an AUC of 0.922 at a cut-off point of 21.75 ng/dl [28]. Other important prediction scores have also been proposed, although these studies were retrospective [29,30,31].
In summary, the PAC at screening was a strong predictor for the diagnostic saline-loading and captopril-challenge test results. The PRA at screening and urine β2-microglobulin were also good predictors for the captopril-challenge test results. The equations used to estimate the saline PAC and the ARR 60 and 90 min after the captopril-challenge test appear useful. The RI in the renal interlobar arteries was the only predictor for the upright furosemide-loading test. However, the equation for the PRA after the upright furosemide-loading test was not acceptable. Further studies are necessary to derive better equations for these diagnostic tests. The IHA patients were older and frequently had impaired glucose tolerance, increased urinary excretion of albumin, and an elevated RI. Conversely, the APA patients had diastolic dysfunction (E/E’) and marked elevation of blood pressure, which was often uncontrollable without the addition of alpha-blockers to calcium channel antagonists, and contributed to the diagnostic test for PA. Thus, patient characteristics and diagnostic predictors may differ among diagnostic tests. We should take these differences into consideration and follow-up the different effects of aldosterone on the characteristics of patients in terms of the PA etiology.
References
Funder JW, Carey RM, Fardella C, Gomez-Sanchez CE, Mantero F, Stowasser, et al. Endocrine Society. Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2008;93:3266–81.
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005;45:1243–8.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101:1889–16.
Monticone S, Burrello J, Tizzani D, Bertello C, Viola A, Buffolo F, et al. Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice. J Am Coll Cardiol. 2017;69:1811–20.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension Guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Nishikawa T, Omura M, Satoh F, Shibata H, Takahashi K, Tamura N, et al. Task Force Committee on Primary Aldosteronism, The Japan Endocrine Society. Guidelines for the diagnosis and treatment of primary aldosteronism—the Japan Endocrine Society 2009. Endocr J. 2011;58:711–21.
Leung AA, Nerenberg K, Daskalopoulou SS, McBrien K, Zarnke KB, Dasgupta K, et al. Hypertension Canada's 2016 Canadian Hypertension Education Program Guidelines for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. Can J Cardiol. 2016;32:569–88.
Reznik Y, Amar L, Tabarin A. SFE/SFHTA/AFCE consensus on primary aldosteronism, part 3: Confirmatory testing. Ann Endocrinol (Paris). 2016;77:202–7.
Tanimura M, Dohi K, Matsuda M, Sato Y, Sugiura E, Kumagai N, et al. Renal resistive index as an indicator of the presence and severity of anemia and its future development in patients with hypertension. BMC Nephrol. 2015;16:45.
Matsumoto K, Yano Y, Gabazza EC, Araki R, Bruno NE, Suematsu M, et al. Inverse correlation between activated protein C generation and carotid atherosclerosis in Type 2 diabetic patients. Diabet Med. 2007;24:1322–8.
Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, et al. Sleep apnea and cardiovascular disease: an American Heart Association/american College Of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council On Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation . 2008;118:1080–111.
Kandhai-Ragunath JJ, Jorstad HT, de Man FH, Peters RJ, von Birgelen C. Approaches for non-invasive assessment of endothelial function: focus on peripheral arterial tonometry. Neth Heart J. 2013;21:214–8.
Aro AL, Chugh SS. Clinical diagnosis of electrical versus anatomic left ventricular hypertrophy: prognostic and therapeutic implications. Circ Arrhythm Electrophysiol. 2016;9:e003629.
Melenovsky V, Borlaug BA, Rosen B, Hay I, Ferruci L, Morell CH, et al. Cardiovascular features of heart failure with preserved ejection fraction versus nonfailing hypertensive left ventricular hypertrophy in the urban Baltimore community: the role of atrial remodeling/dysfunction. J Am Coll Cardiol. 2007;49:198–207.
Yang Y, Zhu LM, Xu JZ, Tang XF, Gao PJ. Comparison of left ventricular structure and function in primary aldosteronism and essential hypertension by echocardiography. Hypertens Res. 2017;40:243–50.
Savard S, Amar L, Plouin PF, Steichen O. Cardiovascular complications associated with primary aldosteronism: a controlled cross-sectional study. Hypertension. 2013;62:331–6.
Ruilope LM, Rodicio JL. Renal surrogates in essential hypertension. Clin Exp Hypertens. 1999;21:609–14.
Bolignano D, Palmer SC, Navaneethan SD, Strippoli GF. Aldosterone antagonists for preventing the progression of chronic kidney disease. Cochrane Database Syst Rev. 2014;4:CD007004.
Cauwenberghs N, Kuznetsova T. Determinants and prognostic significance of the renal resistive index. Pulse (Basel). 2016;3:172–8.
Doi Y, Iwashima Y, Yoshihara F, Kamide K, Hayashi S, Kubota Y, et al. Renal resistive index and cardiovascular and renal outcomes in essential hypertension. Hypertension. 2012;60:770–7.
Stowasser M, Gordon RD. Primary aldosteronism: changing definitions and new concepts of physiology and pathophysiology both inside and outside the kidney. Physiol Rev. 2016;96:1327–84.
Iwakura Y, Ito S, Morimoto R, Kudo M, Ono Y, Nezu M, et al. Renal resistive index predicts postoperative blood pressure outcome in primary aldosteronism. Hypertension. 2016;67:654–60.
Hanslik G, Wallaschofski H, Dietz A, Riester A, Reincke M, Allolio B, et al. Increased prevalence of diabetes mellitus and the metabolic syndrome in patients with primary aldosteronism of the German Conn's Registry. Eur J Endocrinol. 2015;173:665–75.
Chen W, Li F, He C, Zhu Y, Tan W. Elevated prevalence of abnormal glucose metabolism in patients with primary aldosteronism: a meta-analysis. Ir J Med Sci. 2014;183:283–91.
Murase K, Nagaishi R, Takenoshita H, Nomiyama T, Akehi Y, Yanase T. Prevalence and clinical characteristics of primary aldosteronism in Japanese patients with type 2 diabetes mellitus and hypertension. Endocr J. 2013;60:967–76.
Matsumoto T, Oki K, Kajikawa M, Nakashima A, Maruhashi T, Iwamoto Y, et al. Effect of aldosterone-producing adenoma on endothelial function and Rho-associated kinase activity in patients with primary aldosteronism. Hypertension. 2015;65:841–8.
Zacharieva S, Orbetzova M, Elenkova A, Stoynev A, Yaneva M, Schigarminova R, et al. Diurnal blood pressure pattern in patients with primary aldosteronism. J Endocrinol Invest. 2006;29:26–31.
Kobayashi H, Haketa A, Ueno T, Suzuki R, Aoi N, Ikeda Y, et al. Subtype prediction in primary aldosteronism: measurement of circadian variation of adrenocortical hormones and 24-h urinary aldosterone. Clin Endocrinol (Oxf). 2016;84:814–21.
Umakoshi H, Tsuiki M, Takeda Y, Kurihara I, Itoh H, Katabami T, et al. Significance of computed tomography and serum potassium in predicting subtype diagnosis of primary aldosteronism. J Clin Endocrinol Metab. 2018;103:900–8.
Nanba K, Tsuiki M, Nakao K, Nanba A, Usui T, Tagami T, et al. A subtype prediction score for primary aldosteronism. J Hum Hypertens. 2014;28:716–20.
Fujii Y, Umakoshi H, Wada N, Ichijo T, Kamemura K, Matsuda Y, et al. Subtype prediction of primary aldosteronism by combining aldosterone concentrations in the left adrenal vein and inferior vena cava: a multicenter collaborative study on adrenal venous sampling. J Hum Hypertens. 2017;32:12–9.
Acknowledgments
The authors thank Masumi Matsuda, Hidetomo Onuma, Hitomi Kurata, and Mayumi Furlong for their excellent technical assistance.
Funding
This work was supported in part by Grants-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology, Japan (No. 24591113 to R.O.), the Japan Vascular Disease Research Foundation, the Mie Medical Foundation, and the Okasan-Kato Foundation (to R.O.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The Department of Cardiology and Nephrology, Mie University Graduate School of Medicine, received research grants from Bristol-Myers Squibb, MSD K.K., Pfizer Japan Inc., Takeda Pharmaceutical Co., Ltd., Astellas Pharma Inc., Daiichi Sankyo Pharmaceutical Co., Ltd., Genzyme Japan, Shionogi & Co., Ltd., Sumitomo Dainippon Pharma Co., Ltd., Mitsubishi Tanabe Corporation, Otsuka Pharmaceutical Co., Ltd., Bayer Yakuhin, Ltd., AstraZeneca K.K., and Boehringer Ingelheim Co., Ltd. Masaaki Ito received lecture fees from Daiichi Sankyo Co. Pharmaceutical Co., Ltd., Mitsubishi Tanabe Corporation, Bayer Yakuhin, Ltd. and Takeda Pharmaceutical Co., Ltd.
Electronic supplementary material
Appendix
Appendix
The complete list of SHRIMP Study Investigators is as follows: Ryuji Okamoto, MD; Masaya Taniguchi, MD; Yuki Onishi, MD; Naoto Kumagai, MD; Junji Uraki, MD; Naoki Fujimoto, MD; Yasuhiro Hotta, MD; Ken Sasaki, MD; Noriko Furuta, MD; Eitato Fujii, MD; Yutaka Yano, MD; Norikazu Yamada, MD; Toru Ogura, PhD; Yoshiyuki Takei, MD; Hajime Sakuma, MD; Masaaki Ito, MD; Kaoru Dohi, MD; Kazuhito Eguchi, MD; Satoshi Fujita, MD; Shusuke Fukuoka, MD; Tomoyuki Fukuma, MD; Itaru Goto, MD; Rei Hashimoto, MD; Chisa Inoue, MD; Ryoichi Ishisu, MD; Junko Ishiura, MD; Masaki Ishiyama, MD; Yoshihiko Kagawa, MD; Kentaro Kakuta, MD; Akemi Kida, MD; Katsuhisa Konishi, MD; Manabu Kato, MD; Rikiya Kawarada, MD; Tairo Kurita, MD; Kanako Maki, MD; Akimasa Matsuda, MD; Hiroshi Matsuo, MD; Hana Mizutani, MD; Tatsuya Mori, MD; Keishi Moriwaki, MD; Yuki Muneyoshi, MD; Hiroshi Nakajima, MD; Shiro Nakamori, MD; Mashio Nakamura, MD; Tomoyuki Nakata, MD; Atsuhiro Nakatsuka, MD; Hitoshi Nakaya, MD; Kota Nishihama, MD; Shinya Okamoto, MD; Yuko Okano, MD; Yoshito Ogihara, MD; Taku Omori, MD; Masako Sakamoto, MD; Takeshi Sasaki, MD; Kei Sato, MD; Yuichi Sato, MD; Toshiki Sawai, MD Yoshiki Sugimura, MD; Yuichi Sugino, MD; Emiyo Sugiura, MD; Shinya Sugiura, MD; Toshinari Suzuki, MD; Yasuo Suzuki, MD; Takeo Takahashi, MD; Atsuro Takeshita, MD; Te-tsushiro Takeuchi, MD; Yasuyuki Tamai, MD; Muneyoshi Tanimura, MD; Yuji Ueda, MD; Mei Uemura, MD; Takashi Yamanaka, MD; Kiyotaka Watanabe, MD; and Taro Yasuma, MD.
Rights and permissions
About this article
Cite this article
Okamoto, R., Taniguchi, M., Onishi, Y. et al. Predictors of confirmatory test results for the diagnosis of primary hyperaldosteronism in hypertensive patients with an aldosterone-to-renin ratio greater than 20. The SHRIMP study. Hypertens Res 42, 40–51 (2019). https://doi.org/10.1038/s41440-018-0126-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0126-1
Keywords
This article is cited by
-
Associated factors and effects of comorbid atrial fibrillation in hypertensive patients due to primary aldosteronism
Journal of Human Hypertension (2022)
-
Diverse pathological lesions of primary aldosteronism and their clinical significance
Hypertension Research (2021)
-
Urinary sodium/potassium ratio as a screening tool for hyperaldosteronism in men with hypertension
Hypertension Research (2021)
-
Comparison of the shortened and standard saline infusion tests for primary aldosteronism diagnostics
Hypertension Research (2020)
-
Serum-soluble (pro)renin receptor concentration as a biomarker for organ damage in primary aldosteronism
Hypertension Research (2019)