Abstract
The effect of dietary sodium (salt) on cardiovascular disease (CVD) has been debated for a long time. The present study aims to explore whether salt intake affects the risk of cardiovascular disease in the Chinese population. Data from a prospective cohort study that included 954 men and women aged 35–59 years at baseline from four urban and rural population samples in China were used. Each participant collected their overnight urine for three consecutive days during two seasons to estimate sodium intake. CVD events, including incidences of coronary heart disease (CHD), stroke, and death from CVD, and all-cause mortality were tested by Cox proportional hazards models. After a median of 18.6 years of follow-up, CVD events occurred in 81 (8.5%) participants, including 20 CHD and 64 stroke events. All-cause deaths occurred in 149 (15.6%) participants, including 31 CVD-related deaths, 56 cancer-related deaths and 62 other-cause deaths. The hazard ratios and 95% confidence intervals for CVD events in each of the sodium excretion tertiles were 1.00, 1.66 (0.79–3.47) and 3.04 (1.46–6.34), P for trend = 0.001. This trend was also found for stroke incidence (P for trend < 0.001). The cardiovascular mortality risk increased as the sodium excretion levels rose after adjusting for confounding factors (P for trend = 0.043). However, this trend was not significant after adjusting for the baseline systolic blood pressure and antihypertensive medication use (P for trend = 0.171). No significant associations were found between sodium excretion and all-cause, cancer-related or other-cause mortality. High urinary sodium excretion was independently associated with an increased risk of cardiovascular disease in the general Chinese population.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is a major public health problem worldwide and accounts for the largest fraction of deaths related to noncommunicable disease [1]. Hypertension, as an important and modifiable risk factor for CVD, has been widely confirmed as having a strong positive association with dietary sodium intake [2,3,4]. The Trials of Hypertension Prevention (TOHP) study has confirmed that reducing dietary sodium intake could effectively lower blood pressure and incidence of hypertension among persons with high-normal blood pressure [5]. The DASH-Sodium (Dietary Approaches to Stop Hypertension) trial found a significant direct relationship between sodium intake and blood pressure that was evident among subjects with and without hypertension [3]. However, the effect of dietary sodium on the risk of CVD events remains controversial. Some studies have identified that high salt intake is an important risk factor for CVD and is associated with a significantly higher risk of CVD events [6,7,8,9,10], but results from other studies have argued that these positive associations may not exist and that a low sodium intake might even be harmful [11,12,13]. Inconsistent results regarding the link between dietary sodium intake and CVD events have received considerable media attention and have stirred controversy and confusion in the general population. Considering the high level of salt intake in China and the lack of prospective studies on the relationship between salt intake and risk of CVD morbidity and mortality in this population, we aim to explore the associations of sodium intake and the risk of CVD events, all-cause and cause-specific mortality in the Chinese population.
Methods
Study population
Participants included in the analysis were from a subsample of the People’s Republic of China-United States (PRC-USA) Collaborative Study of Cardiovascular and Cardiopulmonary Epidemiology. The study was initiated in 1981 under the PRC-USA Governmental Cooperation in Science and Technology and aimed to evaluate the prevalence of cardiovascular risk factors in the Chinese urban and rural populations. The details of the baseline survey and follow-up methods were explained in prior publications [14, 15]. Briefly, this study focused on four PRC population samples selected in clusters from urban and rural populations in Beijing (the north of China) and Guangzhou (the south of China), with a sample of at least 2000 adults (1000 men and 1000 women) between 35 and 54 years of age from each population. To remain consistent with other relevant studies in China, the Chinese task force decided to extend the age of participants to 59 years old. All interviewers received centralized training and passed a qualification test. All participants signed consent forms.
Data collection
The baseline survey was performed in autumn of 1983–1984. All the items surveyed were carried out according to internationally standardized methods stipulated in a uniform working manual. Blood pressure was measured with a standard mercury sphygmomanometer with three consecutive readings on the right arm after the participant had rested for 5 min. The average of the three readings was used for analysis. Hypertension was defined as systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, or taking antihypertensive drugs in the past two weeks. An overnight fasting blood specimen was obtained from each participant for measurement of serum total cholesterol, triglycerides, high-density lipoprotein cholesterol, and glucose.
Subsample, urine, and dietary data collection
Overnight urine and dietary data were obtained from a random subsample of approximately 10 percent of the participants from each population at baseline. The data collected included timed overnight urine specimens obtained over three consecutive days and 24-h dietary recalls for the assessment of nutrient intakes. Participants were instructed to void immediately before going to bed and to discard the voided urine. The time of voiding was to be recorded. All urine was collected during the night and upon arising in the morning, at which point the time was recorded once again. Dietary nutrients were calculated according to the China Food Composition guidelines. All participants in the subgroup were targeted for repeated urine and diet collection in the spring of 1985–1986 [14]. All urine specimens were transported to the laboratory of Beijing and Guangzhou and were analyzed for urinary sodium, potassium, and creatinine excretions in the laboratory of the Department of Epidemiology, Fuwai Hospital in Beijing and in the Guangzhou Provincial Cardiovascular Institute. Urinary excretions were standardized to 8 h. Sodium and potassium were analyzed by flame photometry, and creatinine was analyzed by a modified Jaffe method.
Follow-up measurements
We referenced the diagnostic criteria of the WHO-MONICA study (World Health Organization monitoring trends and determinants in CVD project) to define the endpoint events [16]. The first follow-up for coronary heart disease (CHD), stroke events, and all-cause deaths was in 1987 and 1988. After the first follow-up, the cohort underwent a follow-up every 2 years until December 31, 2005. Total CVD events included CHD (including non-fatal myocardial infarction and death from CHD) and fatal or non-fatal stroke. During the follow-up survey, a standardized form was used to collect the data for CHD, stroke events, and other information, recording the occurrence of disease or death, onset time, symptoms, and other disease characteristics. Hospital records, autopsy results, as well as death certificates were reviewed to ascertain disease diagnoses [15]. All this crucial information was verified by an endpoint assessment committee.
Statistical analysis
The daily sodium intake level was represented by the mean of 6 days of 8-h overnight urinary sodium excretion during two seasons. Participants were divided into tertiles based on mean overnight urinary sodium excretion. The baseline characteristics among study participants were presented as the mean (SD) or median (interquartile range) for continuous variables and as percentages for categorical variables. The differences in the baseline characteristics among tertiles were assessed with analysis of variance or Kruskal-Wallis rank test for continuous variables and χ2-test for categorical variables. We performed a Cox proportional hazard regression model to determine the association between 8-h overnight urinary sodium excretion and cardiovascular events, all-cause and cause-specific mortality; the lowest sodium group was used as the reference. After adjusting for socio-demographic status, physical measurements, conventional lifestyle factors, systolic blood pressure, and use of antihypertensive medication, hazard ratios (HRs) and 95% confidence intervals (CI) for CVD events and deaths in each group were determined. Trend tests were conducted by calculating the median values of 8-h overnight urinary sodium at baseline within each group and then modeling these median values as a continuous variable in all models to test the significance of this variable. A two-tailed P value < 0.05 was considered significant. All analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
A total of 1130 participants were randomly selected for urine and diet information collection during the baseline autumn survey. For the current analysis, we excluded participants for the following reasons: absence of the repeated survey in spring (n = 107); urine specimens were collected only during one season (n = 19); no dietary data were collected (n = 1); history of CHD or stroke at baseline (n = 14); and failed to attend any follow-up visits (n = 35). In total, 954 participants were included in the present study, of whom 459 were male and 495 were female. Participants had a mean (SD) age of 46.4 (6.2) years and the median (interquartile range) 8-h overnight urinary sodium excretion was 54.5 (40.0, 75.2) mmol. A total of 15.5% of participants had hypertension, and 23.7% (35/148) of patients were taking antihypertensive drugs. After a median follow-up of 18.6 years, 81 (8.5%) cardiovascular events occurred during the follow-up period, including 64 strokes and 20 CHD events. All-cause deaths occurred in 149 participants (15.6%), including 31 CVD deaths, 56 cancer deaths, and 62 other-cause deaths. The baseline characteristics of the study population separated by urinary sodium excretion tertiles are shown in Table 1. Participants in the highest sodium excretion group tended to consume a higher percentage of energy from saturated fat (P = 0.003) and a lower percentage of energy from carbohydrates (P < 0.001). Compared to the participants in the lowest sodium tertile category, those with a higher sodium excretion were more likely to live in an urban area or in the northern region. Participants with a higher sodium excretion also had a higher education level, a higher body mass index, a higher glucose level (P = 0.002), and a higher prevalence of hypertension (P < 0.001) compared with participants from the lowest sodium tertile.
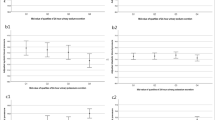
Urinary sodium excretion and CVD events
Table 2 shows the morbidity and HRs for CVD associated with urinary sodium excretion. CVD morbidity rates per 1000 person-years from the lowest to highest sodium excretion categories were 2.21, 4.26, and 8.75, and the rates for stroke events were 1.29, 3.33, and 7.38. After adjusting for multiple confounding factors in model 2, higher sodium excretion significantly increased the risk of total CVD events compared with the lowest sodium excretion category. The HRs and 95% CI for total CVD events from the lowest to the highest sodium excretion category were 1.00, 1.64 (0.79–3.42), and 3.74 (1.79–7.79), P for trend < 0.001. When we adjusted for baseline systolic blood pressure and antihypertensive drug use in model 3, these hazard ratios became somewhat attenuated but were still significant (P for trend = 0.001). This relationship was also found in stroke events (P for trend < 0.001), but no significant association was shown in CHD (P for trend = 0.806).
Urinary sodium excretion and mortality
In total, 31 participants died from CVD events. CVD mortality rates per 1000 person-years in the three sodium excretion categories from the lowest excretion to the highest excretion were 1.10, 1.65, and 2.93. After adjusting for potential confounding factors in model 2, the highest tertile of sodium excretion had a HR (95% CI) of 2.67 (0.90–7.89) for CVD mortality compared with the lowest tertile. In addition, there was a trend toward an increased risk of CVD mortality along with increasing sodium excretion levels (P for trend = 0.043), but this trend was no longer significant when we further adjusted for systolic blood pressure and taking antihypertensive drugs in model 3 (P for trend = 0.171). No significant association was found between sodium excretion and all-cause, cancer or other-cause mortality in our study. The results are shown in Table 3.
Discussion
The main finding of our study was that a high sodium intake was significantly associated with an increased risk of CVD, independently of other cardiovascular risk factors, including blood pressure. These findings were consistent with the results of the Trials of Hypertension Prevention (TOHP) [8], which reported that there was a linear 17% increase in risk per 1000 mg/d increase in sodium excretion. In the Northern Manhattan Study [9], Gardener et al. reported that sodium intake was significantly associated with stroke during a mean follow-up of 10 years. Compared with the lowest sodium group, there was a 1.59-fold increase in risk for stroke in the highest sodium group (HR, 2.59; 95% CI, 1.27–5.28), and this study also found that high sodium intake was associated with an elevated risk of combined vascular events (stroke, MI, or vascular death). However, no association was observed for the risk of MI, which was in agreement with our study. In contrast with our findings, Aijala et al. reported that sodium intake, as a continuous variable, predicted CVD (P = 0.031) and CHD (P = 0.014) events independently, but failed to reach statistical significance in predicting stroke events (P = 0.85) after a 19-year follow-up [10]. These inconsistent results might be explained by the fact that risk factor patterns and profiles of CVD are different in China [17]. Compared to CHD events, stroke is much more prevalent in China, and because of the small number of cases, the HRs for CHD events in our study were not significant. In our analysis, the association between high sodium intake and the risk of CVD and stroke events was consistent, even when we adjusted for baseline blood pressure and use of antihypertensive medication, which indicates that there might be some mechanistic effect on CVD, independent of blood pressure.
In the analysis of all-cause and cause-specific mortality, we found that there was a trend of increased risk of CVD mortality (P for trend = 0.043), but no significant associations were found between sodium excretion and all-cause, cancer-related or other-cause mortality. In a large prospective Japanese study [7] of participants between 40 and 79 years of age with an average follow-up of 12.7 years, sodium intake was identified as an independent risk factor for total CVD mortality. The HR for the highest versus the lowest quintiles of sodium intake was 1.42 (95%CI, 1.20–1.69), after adjusting for confounding factors including hypertension history. However, our results show that when controlling for baseline systolic blood pressure and use of antihypertensive medication, the HRs for CVD mortality increased by sodium excretion categories, but the trend did not reach statistical significance. Possible explanations may be the ethnic and regional differences between Japanese and Chinese populations or the differences in adjustment factors. Our results indicated that the relationship between sodium intake and CVD mortality was mediated mainly by blood pressure. The TOHP study conducted by Cook et al. [18] reported that there was a positive linear relationship between sodium intake and all-cause mortality after 20 years of follow-up, but this study did not assess the risk for cardiovascular mortality.
In addition to the abovementioned research, some studies have reported an inverse relationship between sodium intake and mortality [12, 19]. For example, Ekinci et al. [19] used the data from 638 patients with type 2 diabetes mellitus, and reported that for every 100 mmol rise in 24-h urinary sodium, cardiovascular mortality was 35% lower. However, in this study, participants had a significant burden of preexisting CVD at baseline. Participants in the lowest urinary sodium excretion tertile were older, had a longer duration of diabetes, and exhibited more multiple clinical comorbidities when compared with participants in the highest tertile.
Possible mechanisms linking sodium to CVD include the association between sodium intake and blood pressure, which has been confirmed by a number of studies [3, 20,21,22]. In addition, high sodium intake may lead to adverse effects through BP-independent mechanisms, including massive albumin excretion, oxidative stress, severe renal arteriolar damage, and impaired vascular endothelial function. These factors result in large elastic artery stiffness, arterial dysfunction, and left and right ventricular hypertrophy, which eventually lead to CVD [23,24,25,26,27].
Our study has two strengths. First, we used the mean of 6 days of 8-h overnight urinary sodium excretion during two seasons to represent daily sodium intake, which can reduce the variability within individuals, provide more valid data, and accurately reflect the usual sodium intake level. Second, to the best of our knowledge, this is the first long-term follow-up prospective study to explore the relationship between salt intake and the risk of CVD in the Chinese general population, which can provide more evidence for salt reduction policies in China.
The present study also has several potential limitations. First, we used overnight urinary sodium excretion instead of 24-h urinary sodium to estimate dietary sodium intake. However, previous validation studies have reported a strong correlation between overnight and 24-h urinary sodium excretion [28,29,30,31], and considering that the collection of an overnight urine sample is easier than that of a 24-h urine sample, overnight urinary sodium can be regarded as an alternative indicator of dietary sodium intake. Second, although we have followed rigorous standards to collect overnight urine, the possibility of incomplete urine collection may still exist. To control for the quality of urine specimens and the completeness of urine collection, we further adjusted for creatinine and added the ratio of sodium/creatinine in the model, and there was no essential change in the results (data are shown in supplementary files). Taking into account the smaller sample size of our study, it is impossible to segment more groups to analyze the effects of low salt intake on CVD. An additional limitation is that we did not collect the information for renal function at baseline, so we could not control for these potential confounding factors in the Cox proportional hazard regression models.
In conclusion, in this long-term follow-up study, we showed that high sodium intake was associated with an increased risk of CVD in the Chinese population. Our results support the implementation of a salt reduction policy at the population level to achieve potential cardiovascular benefits.
References
Hunter DJ, Reddy KS. Noncommunicable diseases. N Engl J Med. 2013;369:1336–43.
Geleijnse JM, Kok FJ, Grobbee DE. Blood pressure response to changes in sodium and potassium intake: a metaregression analysis of randomised trials. J Hum Hypertens. 2003;17:471–80.
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10.
He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013;346:f1325.
Trials of Hypertension Prevention Collaborative Research Group. The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels. Results of the Trials of Hypertension Prevention, phase I. JAMA. 1992;267:1213–20.
Tuomilehto J, Jousilahti P, Rastenyte D, Moltchanov V, Tanskanen A, Pietinen P et al. Urinary sodium excretion and cardiovascular mortality in Finland: a prospective study. Lancet. 2001;357:848–51.
Umesawa M, Iso H, Date C, Yamamoto A, Toyoshima H, Watanabe Y et al. Relations between dietary sodium and potassium intakes and mortality from cardiovascular disease: the Japan Collaborative Cohort Study for Evaluation of Cancer Risks. Am J Clin Nutr. 2008;88:195–202.
Cook NR, Appel LJ, Whelton PK. Lower levels of sodium intake and reduced cardiovascular risk. Circulation. 2014;129:981–9.
Gardener H, Rundek T, Wright CB, Elkind MS, Sacco RL. Dietary sodium and risk of stroke in the Northern Manhattan study. Stroke. 2012;43:1200–5.
Aijala M, Malo E, Santaniemi M, Bloigu R, Silaste ML, Kesaniemi YA et al. Dietary sodium intake and prediction of cardiovascular events. Eur J Clin Nutr. 2015;69:1042–7.
O’Donnell M, Mente A, Rangarajan S, McQueen MJ, Wang X, Liu L et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014;371:612–23.
Stolarz-Skrzypek K, Kuznetsova T, Thijs L, Tikhonoff V, Seidlerova J, Richart T et al. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA. 2011;305:1777–85.
Taylor RS, Ashton KE, Moxham T, Hooper L, Ebrahim S. Reduced dietary salt for the prevention of cardiovascular disease: a meta-analysis of randomized controlled trials (Cochrane review). Am J Hypertens. 2011;24:843–53.
People’s Republic of China--United States Cardiovascular and Cardiopulmonary Epidemiology Research Group.. An epidemiological study of cardiovascular and cardiopulmonary disease risk factors in four populations in the People’s Republic of China. Baseline report from the P.R.C.-USA Collaborative Study. Circulation. 1992;85:1083–96.
Wu Y, Liu X, Li X, Li Y, Zhao L, Chen Z et al. Estimation of 10-year risk of fatal and nonfatal ischemic cardiovascular diseases in Chinese adults. Circulation. 2006;114:2217–25.
The World Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. WHO MONICA Project Principal Investigators. J Clin Epidemiol. 1988;41:105–14.
Zhou BF, Zhang HY, Wu YF, Li Y, Yang J, Zhao LC et al. Ecological analysis of the association between incidence and risk factors of coronary heart disease and stroke in Chinese populations. CVD Prev. 1998;1:207–16.
Cook NR, Appel LJ, Whelton PK. Sodium intake and all-cause mortality over 20 years in the Trials of Hypertension Prevention. J Am Coll Cardiol. 2016;68:1609–17.
Ekinci E, Clarke S, Thomas M, Moran J, Cheong K, MacIsaac R et al. Dietary salt intake and mortality in patients with type 2 diabetes. Diabetes Care. 2011;34:703–9.
Johnson A, Nguyen T, Davis D. Blood pressure is linked to salt intake and modulated by the angiotensinogen gene in normotensive and hypertensive elderly subjects. J Hypertens. 2001;19:1053–60.
MacGregor G, Markandu N, Sagnella G, Singer D, Cappuccio F. Double-blind study of three sodium intakes and long-term effects of sodium restriction in essential hypertension. Lancet. 1989;2:1244–7.
Law M, Frost C, Wald N. By how much does dietary salt reduction lower blood pressure? I--analysis of observational data among populations. BMJ. 1991;302:811–5.
Avolio AP, Deng FQ, Li WQ, Luo YF, Huang ZD, Xing LF et al. Effects of aging on arterial distensibility in populations with high and low prevalence of hypertension: comparison between urban and rural communities in China. Circulation. 1985;71:202–10.
Avolio A, Clyde K, Beard T, Cooke H, Ho K, O’Rourke M. Improved arterial distensibility in normotensive subjects on a low salt diet. Arteriosclerosis. 1986;6:166–9.
Jablonski K, Gates P, Pierce G, Seals D. Low dietary sodium intake is associated with enhanced vascular endothelial function in middle-aged and older adults with elevated systolic blood pressure. Ther Adv Cardiovasc Dis. 2009;3:347–56.
Frohlich ED, Gonzalez A, Diez J. Hypertensive left ventricular hypertrophy risk: beyond adaptive cardiomyocytic hypertrophy. J Hypertens. 2011;29:17–26.
Han W, Han X, Sun N, Chen Y, Jiang S, Li M. Relationships between urinary electrolytes excretion and central hemodynamics, and arterial stiffness in hypertensive patients. Hypertens Res. 2017;40:746–51.
Mill JG, Silva AB, Baldo MP, Molina MC, Rodrigues SL. Correlation between sodium and potassium excretion in 24- and 12-h urine samples. Braz J Med Biol Res. 2012;45:799–805.
Yamasue K, Tochikubo O, Kono E, Maeda H. Self-monitoring of home blood pressure with estimation of daily salt intake using a new electrical device. J Hum Hypertens. 2006;20:593–8.
Liu K, Dyer AR, Cooper RS, Stamler R, Stamler J. Can overnight urine replace 24-hour urine collection to asses salt intake? Hypertension. 1979;1:529–36.
Yasutake K, Horita N, Umeki Y, Misumi Y, Murata Y, Kajiyama T et al. Self-management of salt intake: clinical significance of urinary salt excretion estimated using a self-monitoring device. Hypertens Res. 2016;39:127–32.
Acknowledgements
We thank the participants in this study and all the staff of PRC-USA Collaborative Study for their support and assistance. This study was supported by the United States National Heart, Lung, and Blood Institute (grants NO-1HV12243 and NO-1HV8112), the People’s Republic of China Ministry of Science and Technology and the Ministry of Health from the 8th to 10th National Five-Year Plan projects (grants 85-915-01-01, 96-906-02-01 and 2001BA703B01).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None of the authors have any conflicts of interest to declare.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Liu, H., Gao, X., Zhou, L. et al. Urinary sodium excretion and risk of cardiovascular disease in the Chinese population: a prospective study. Hypertens Res 41, 849–855 (2018). https://doi.org/10.1038/s41440-018-0091-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0091-8
This article is cited by
-
Sex-specific associations between sodium and potassium intake and overall and cause-specific mortality: a large prospective U.S. cohort study, systematic review, and updated meta-analysis of cohort studies
BMC Medicine (2024)
-
Quantitative verification of the effect of using an umami substance (L-glutamate) to reduce salt intake
Hypertension Research (2020)
-
Umami and salt reduction
Hypertension Research (2020)
-
Relationship of household salt intake level with long-term all-cause and cardiovascular disease mortality in Japan: NIPPON DATA80
Hypertension Research (2020)
-
High-salt intake increases TRPC3 expression and enhances TRPC3-mediated calcium influx and systolic blood pressure in hypertensive patients
Hypertension Research (2020)