Abstract
The aim of this study, enrolling 118 patients, was to clinically evaluate the accuracy of carotid pulse waveform acquisition with a new non-invasive optical fiber probe using invasive and non-invasive pressure readings as references. Pulse waves were acquired simultaneously in the ascending aorta and right common carotid; for the non-invasive study, the pulses were sequentially acquired using the optical fiber device and the Complior Analyse® (Alam Medical, France) device in the right carotid artery. For all subjects, the pulse waveforms assessed using the optical fiber sensor and the references were superimposed to analyze the deviation and point-by-point correlation. Augmentation index and central pressure were compared using intraclass correlation and Bland–Altman analyses with a confidence interval of 95%. For the invasive study, the acquired waves presented a mean deviation of 11 ± 3% and a mean intraclass correlation of 0.97 ± 0.02. Concerning the augmentation index and central systolic pressure, correlations of 0.79 (p < 0.001) and 0.94 (p < 0.001) were found, respectively. In the non-invasive comparison, the assessed mean deviation between the morphologies of the waves was 13 ± 5%, with correlation coefficients of 0.91 (p < 0.001) for the augmentation index and 0.98 (p < 0.001) for central systolic pressure. The results show that the optical fiber probe results were highly correlated with those obtained using the reference techniques in terms of the pulse waveforms, central systolic pressure (cSP), and augmentation index assessment.
Similar content being viewed by others
Introduction
The progression of central arterial stiffness results in several changes in arterial pulse morphology, velocity, and pressure [1]; therefore, these features can be used as stiffness surrogates [2].
Systolic (SPs) and pulse (PPs) pressures in the ascending aorta and in the brachial artery are not equivalent, and the latter are typically used to assess non-invasive blood pressure [3]. SP increases from the aorta to peripheral arteries, although mean arterial pressure (MAP) and diastolic pressure (DP) show only 1–2 mmHg decreases toward the periphery [4]. This phenomenon is usually termed “pulse pressure amplification” and is explained by changes in arterial stiffness and diameter, which alter the timing and extent of wave reflection [5, 6].
Central systolic pressure (cSP) assessment, although not yet considered a variable worth monitoring in cardiovascular risk evaluation, is an important parameter that can help in understanding real pressure loads in the brain, heart, and kidneys [7]. For instance, at the coronary level, in addition to atherosclerotic lesions, this central pressure increase can led to ischemia due to the impairment of the left ventricle function [6].
The common carotid is a superficial artery closer to the aorta; the SP in this artery is approximately only 3 mmHg higher than that of the aorta [8], and for this reason, provides a good estimate of the aortic pulse waveform and cSP. The calculation of cSP is usually performed based on carotidograms, which are scaled up to pressure using brachial DP and MAP [5]. MAP can be calculated directly from the brachial pulse wave; however, it is usually calculated as DP plus one-third of PP.
In studies of reflected waves, the most straightforward index used to quantify the reflected wave impact on the cSP is the augmentation index (AIx), which can be calculated as follows [9]:
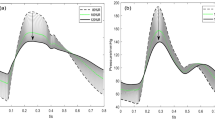
where cSP1 and cSP2 are the first and second critical points (cSP or inflexion) of the pulse waves, respectively. Young subjects with healthy central arteries usually have negative values of AIx, because cSP2 corresponds to the inflexion caused by the late arrival of the reflective wave, as shown in Fig. 1a, and has a lower amplitude than cSP1. As arterial stiffness increases, the pulse wave travels faster, and its reflected components, which also have higher amplitudes, overlap the original wave in such way that the cSP2 has a higher amplitude than the forward wave peak, as illustrated in Fig. 1b.
The gold standard technique for central PP and morphology evaluation is intra-aortic acquisition [10]. This procedure has limitations related to its invasiveness; therefore, the risk/benefit relationship does not recommend its regular application. For this reason, transcutaneous non-invasive approaches are used, allowing the detection of the pulse wave in superficial arteries, such as carotid and radial arteries. SphygmoCor® (AtCor Medical, Australia) and Complior Analyze® (Alam Medical, France) devices are the reference non-invasive devices for pulse wave analysis and cSP assessment [11].
New systems have been investigated to assess central arterial pulse in order to ease the acquisition process and reduce device cost, thereby promoting the generalization of pulse waveform analysis and cSP assessment. One of these devices is based on a plastic optical fiber (POF) and combines low cost and robustness, referred to hereafter as the POFpen [12,13,14]. Features such as immunity to electromagnetic radiation and electric insulation from the patient make optical fiber sensors uniquely qualified to meet medical instrumentation requirements. This technology improves the safety of medical devices and allows the monitoring of physiological signals during magnetic resonance imaging [15].
The main goal of this study was to clinically evaluate the POFpen. The Artery Society has created guidelines and standards for validating new devices, for example, for pulse wave velocity (PWV) devices, for which certification and calibration methods are well stablished [16]. The task has been more difficult to accomplish for pulse waveform analysis (PWA) and cSP devices, for which the best calibration algorithm and validation techniques have not yet been agreed upon. Similar to that of other commercial devices, the clinical evaluation of the POFpen was performed by comparing its results to those obtained using invasive and non-invasive techniques; more specifically, using the intra-aortic pressure waves and tonometric pulses acquired with the Complior Analyse® device as references.
As a non-invasive technique, the Complior device has been extensively used to measure pulse wave velocity, cSP, and AIx; therefore, recent data are available on the validation of the Complior device for use in invasive and non-invasive measurements. In 2013, Sztrymf et al. reported a validation study involving 12 patients, in which radial pulses obtained with the Complior device and invasive pressure acquisition were compared; no significant difference was found in the amplitude of the harmonics between both signals, and the difference in form factor (FF) between the techniques was 4.2 ± 2.8% [17]. Previous cSP and AIx comparisons with invasive pressure waves presented mean differences in pressure of −1.8 ± 4.2 mmHg and in AIx of 0.2 ± 0.8% [18]. Regarding non-invasive validation using the Sphygmocor device, a difference in measurements obtained between the techniques of −0.7 ± 5.6 mmHg was found [11]. This study stated that Complior and SphygmoCor can be considered interchangeable; as the devices are more often used in epidemiologic studies, it was considered that either of the devices could be used as a reference device in this validation study. Therefore, this study used the Complior device as the non-invasive reference.
Methods
POFpen
The optical fiber probe used in this study consists of a plastic pen supporting a 2.2-mm outer diameter (1-mm core) step-index POF [13, 14]. For pulse acquisition, the probe applies a visible optical signal to a small round adhesive reflector placed on the left carotid surface, where the highest pulsatility is felt. The reflected signal is collected by the same fiber and is detected by a photodiode, and the signal intensity is modulated by arterial micromovements. The probe end is hollow, allowing stabilization of the surrounding area without pressing the artery in the acquisition location, as seen in Fig. 2. The system is portable and acquires data at 500 Hz; data are transmitted via bluetooth to a tablet or computer.
Patients exclusion criteria
In total, 118 patients were enrolled in the study, 37 for the invasive, and 81 for the non-invasive studies. Clinical information was obtained from the patients and their clinical files, including age, sex, weight, height, personal clinical history, smoking habits, and pharmacological treatment. The volunteers were included in the study unless they fulfilled any of the following exclusion criteria: arrhythmia, premature ventricular beats, respiratory problems, movement artifacts, and/or severe mental problems. The study was approved by the local ethics committees.
Invasive study
This cross-sectional study evaluated the similarity between carotid pulse waves assessed with the POFpen and aortic invasive pulse waves and was performed at “Unidade de Intervenção Cardiovascular - Centro Hospitalar da Universidade de Coimbra” (Coimbra, Portugal). The data were collected on 7 days chosen at random within a period of ~4 months. A total of 37 patients with suspected coronary artery disease who underwent cardiac catheterization were included in the study; of these, 29 complied with the inclusion criteria.
The patients studied in this work were prescribed heart catheterization, during which the intra-aortic pressure was assessed using a 6-Fr Judkins right catheter connected to a pressure transducer and a saline infusion system. A Siemens Artis Zee with an AXIOM Sensis hemodynamic recording system were used. Simultaneously, non-invasive carotid waves were acquired using the POFpen.
Each acquisition took no longer than 2 min. Based on the assessed data sequence, the average arterial wave was calculated for all subjects using eight consecutive pulses. The value of AIx measured using both techniques was also calculated for the patients, whose pulse waves presented two systolic peaks in both the intra-aortic and POFpen-assessed waves (21 patients). cSP assessment with the POFpen device was performed in all subjects (29 patients) using data obtained from the invasive procedure for calibration. AIx and cSP were estimated according to the procedures presented in the introduction.
Non-invasive study
Measurements were recorded in subjects with prescribed PWV and cSP using the Complior device by two experienced technicians using the regular tonometry protocol [19]. After the prescribed tests, the carotid pulse was assessed using the POFpen; the data were always acquired after the prescribed examinations for logistical reasons to avoid delaying the regular examination routine. The brachial BP values used for pulse calibration were recorded between both measures using a sphygmomanometer (M6 Comfort, OMRON).
Based on the assessed data sequences, the average arterial pulse waveform was calculated for all subjects using eight consecutive pulses. AIx was measured only for patients in whom inflexion was distinguishable in the waves assessed by both technologies (53 subjects). cSP was compared for 71 subjects since the pressure of the remaining 5 patients was miscalculated by the software of one or both devices.
Data analysis and statistics
The mean normalized arterial pulse waveforms assessed using both techniques were superimposed for all subjects. The pulse similarity estimation was performed in the time domain by assessing RMSD (root-mean-square deviation) and point-by-point intraclass correlations.
Values of FF%, AIx%, and cSP obtained using both techniques were also compared. All values are expressed as the mean ± SD. Differences between techniques were tested using the sample student’s t-test, and two-tailed values of p < 0.05 were considered to indicate significance.
Intraclass correlation coefficients (ICCs), which are usually used to evaluate the outputs of different techniques for acquiring the same variable in the same subject, and Bland–Altman plots were also used to analyze the accuracy of the POFpen measurements. An ICC between 0.7 and 0.8 was considered to represent a strong agreement between the techniques, and an ICC higher than 0.8 was considered to indicate very strong agreement. The statistical calculations were performed using IBM SPSS Statistics 23.
Results
Invasive study
The baseline characteristics of the cohort that entered the invasive study are shown in Table 1. The group mainly comprised male subjects (69%) between 47 and 88 years old. Regarding risk factors, the subjects were slightly overweight, with a mean body mass index (BMI) of 26 ± 4 kg/m2; dyslipidemia was seen in 69% of the patients, diabetes in 24%, and hypertension in 59%, and 24% of the patients were smokers or ex-smokers. Of the patients, 24% had past coronary artery bypass grafting, and 17 had been subjected to coronary angioplasty; 28 and 21% had suffered at acute myocardial infarction and/or stroke, respectively. The subjects’ average cSP was 131 ± 22 mmHg, and the average brachial SP was 145 ± 28 mmHg.
Figure 3 presents examples of invasive and POFpen waveforms recorded in three patients, showing the similar morphology of the pulses assessed with both techniques. Potential differences in the average pulse wave morphology were studied in the time domain. The RMSD obtained was 11 ± 3%, and the difference in FF between the methods was 7 ± 3%. The point-by-point ICC evaluation of the pulses showed a very strong mean correlation of 0.97 ± 0.02.
Linear regression was performed to compare AIx values obtained by both techniques, and the results are shown in Fig. 4a. A strong ICC of 0.79 (p < 0.001) was found between the results obtained using both techniques, even though the AIx values assessed using the POFpen had less variability than the intra-aortic values. Figure 4b shows that the POFpen underestimates AIx by 3.7 ± 12.5%.
The cSP results can be seen in Fig. 5. The scatter plot (Fig. 5a) shows a linear tendency with a very strong ICC of 0.99 (p < 0.001). The Bland–Altman plot (Fig. 5b) demonstrates that the POFpen underestimated cSP by 11 ± 5 mmHg.
Non-invasive study
Measurements were performed in 76 patients with an average age of 53 years old. The demographic and clinical characteristics of the patients are presented in Table 2. The population was overweight; 40% had dyslipidemia, 16% diabetes and 93% hypertension, and 34% were smokers or ex-smokers. Not all the subjects were hypertensive; some patients with suspected hypertension were also seen during the consultations. Of the patients who entered the study, 7% had previous acute myocardial infarction, and 12% had a cerebrovascular event, defined as a transient ischemic attack or a hemorrhagic or ischemic stroke. The mean pulse wave velocity of the cohort was 9.0 ± 2.7 m/s.
In Fig. 6, three examples of superimposed waves detected with Complior and POFpen are shown. All the presented waves are very similar and superimposable, with an average acquisition RMSD of 13 ± 1% and an ICC of 0.96 ± 0.03. The POFpen and Complior wave FFs differed by 9 ± 4%; the Complior waves had a FF of 40 ± 4%, and POFpen waves had an FF of 49 ± 4%.
A scatter plot of AIx values assessed using both techniques is presented in Fig. 7; the slope of the line is 0.80, and an ICC of 0.91 was obtained (p < 0.001). As seen on the corresponding Bland–Altman graph, a mean difference of −1.9 ± 12.2% was found.
The mean cSP pressure difference was 9 ± 5 mmHg. The dispersion profile was calculated, and as shown in Fig. 8, the resulting linear fit had a slope of 0.9 ± 0.0 and an ICC of 0.98 (p < 0.001).
In this work, correlations between arterial stiffness (PWV assessed with the Complior device) and AIx and cSP were assessed using both techniques. As shown in Table 3, the cSP data obtained using both techniques were highly correlated with arterial stiffness. On the other hand, only AIx values calculated from the POFpen-acquired waves were significantly correlated with PWV.
Discussion
The results obtained for both the invasive and non-invasive evaluations are shown in Table 4. The results are discussed according to the studied variables, as follows.
Arterial pulse superimposition
Overlapping the arterial pulses obtained using the POFpen with the invasive and non-invasive techniques resulted in RMSDs of 13 ± 1% and 11 ± 3%, and FF of 9 ± 4% and 7 ± 3%, respectively. During the POFpen application, the probe slightly stretches the skin above the carotid artery; because the probe end is hollow, it allows a certain degree of arterial distension. Due to the viscoelastic properties of arteries, the pulses assessed using the POFpen presented a higher FF than those obtained using the reference techniques, consistent with the RMSD values.
Nonetheless, the point-by-point correlation between the POFpen-obtained waves and the references presented strong correlation coefficients, 0.96 ± 0.03 and 0.97 ± 0.02 for the non-invasive and invasive studies, respectively. These results indicate that the differences in FF do not prejudice the correlation between the techniques.
AIx
For the invasive study, a correlation coefficient of 0.79 (p < 0.001) was found, with a mean difference between techniques of <4%. However, a positive bias was noticed, with POFpen underestimating AIx. This fact may be due to the lower coefficient of variance of the POFpen-obtained results, 1.04 vs 1.36 for the invasive waves, and this bias was probably caused by the viscoelastic properties of the arteries and the different arterial acquisition locations used. Nonetheless, the results are within the range presented for the validation of other commercial devices [20].
In the non-invasive study, an ICC coefficient of 0.91 (p < 0.001) was found, with a mean difference of 1.9 ± 12.2%. Bland–Altman plots showed a good accuracy profile without bias. AIx is a cardiovascular parameter with known high variability; apart from the high SD, the results were within the range of validation results obtained for other commercial devices [11, 20].
cSP
In the invasive study, cSP values were compared for 28 subjects. The statistical analysis showed an ICC of 0.99 (p < 0.001), and the Bland–Altman approach resulted in a mean difference of 11 ± 5 mmHg with an absence of bias. The POFpen seems to underestimate cSP in a similar manner to other commercial techniques [21, 22].
The cSP non-invasive pressure comparison was performed in 71 subjects, and a very strong intraclass coefficient of 0.98 (p < 0.001) was found. The Bland–Altman analysis showed a good accuracy profile for the device and an absence of bias.
In both studies, the difference in FF influenced the overall cSP values. However, the high correlations obtained between the different techniques showed that this difference can be corrected.
AIx, cSP, and PWV
cSP and AIx values measured using both techniques were statistically analyzed using intraclass correlations in relation to arterial stiffness, measured as PWV. cSP data obtained using both techniques were significantly correlated with arterial stiffness, with ICCs of 0.67 and 0.64 (p < 0.001) for the POFpen and Complior devices, respectively. However, for AIx, only the values calculated from the POFpen waves were significantly correlated with PWV. A possible explanation for this observation is that the value of AIx, when assessed by the POFpen, which allows some arterial distension during pulse acquisition, seems to be more strongly related to arterial wall stiffness than is AIx as usually inferred from pressure waves.
Study limitations and future perspectives
Both the invasive and non-invasive studies present inherent limitations. For the invasive comparison, the age and health conditions of the subjects should be noted; the great majority of these patients underwent catheterization in an urgent context. This restraint is universal to all invasive validations. A second limitation was the impossibility of performing intra-carotid readings, since it would be unethical to submit a subject undergoing heart catheterization to carotid exploration because pressure measurements at that location present a much higher risk to the patient than those measured at the aorta, which is part of the regular examination and represents a higher caliber artery.
The non-invasive study was subject to limitations, in that the acquisitions could not be performed in a random order for logistical issues and were performed only by one operator. In future work, the assessment of interoperator repeatability and data acquisition in a random order will be performed. Another limitation was that the compared waves were not obtained simultaneously; however, this is a general limitation of this type of clinical validation and is inherent to all similar studies.
Conclusion
The presented cross-sectional study had the aim of clinically evaluating a new device, based on optical fibers, in terms of its usefulness in assessing the central arterial pulse using intra-aortic and non-invasive pressure waves as references.
The strong correlations between the results obtained using the POFpen and those obtained using the references showed that this probe accurately acquires carotid pulse waveforms. This study showed the potential of this new device that, due to its advantages, such as its optical fiber basis, low cost, high portability, and ease of application, can empower the dissemination of cSP and AIx evaluations.
References
Mitchell G, Parise H, Benjamin E, Larson M, Keyes M, Vita J, et al. Changes in arterial stiffness and wave reflection with advancing age in healthy men and women: the Framingham Heart Study. Hypertension. 2004;43:1239–45.
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2003;27:2588–605.
Roman J, Devereux B, Kizer R, Okin P, Lee E, Wang W, et al. High central pulse pressure is independently associated with adverse cardiovascular outcome: the strong heart study. J Am Coll Cardiol. 2009;54:1730–4.
Chen C, Nevo E, Fetics B, Pak P, Yin F, Maughan W, et al. Estimation of central aortic pressure waveform by mathematical transformation of radial tonometry pressure: validation of generalized transfer function. Circulation. 1997;95:1827–36.
McEniery C, Cockcroft J, Roman M, Franklin S, Wilkinson I. Central blood pressure: current evidence and clinical importance. Eur Heart J. 2014;35:1719–25.
Weber T, Segers P. Changes in central hemodynamics, wave reflection, and heart-vessel coupling with normal and accelerated aging. In: Nilsson P, Olsen M, Laurent S, editors. Early vascular aging (EVA) – new directions in cardiovascular protection. Elsevier Inc.; 2014. p. 83–95.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension. Eur Heart J. 2013;34:2159–219.
Chen C, Ting C, Nussbacher A, Nevo E, Kass D, Pak P, et al. Validation of carotid artery tonometry as a means of estimating augmentation index of ascending aortic pressure. Hypertension. 1996;27:168–75.
O’Rourke M, Pauca A, Jiang X. Pulse wave analysis. Br J Clin Pharmacol. 2001;51:507–22.
Romagnoli S, Ricci Z, Quattrone D, Tofani L, Tujjar O, Villa G, et al. Accuracy of invasive arterial pressure monitoring in cardiovascular patients: an observational study. Crit Care. 2014;18:644–55.
Stea F, Bozec E, Millasseau S, Khettab H, Boutourie P, Laurent S, et al. Comparison of the Complior Analyse device with Sphygmocor and Complior SP for pulse wave velocity and central pressure assessment. J Hypertens. 2014;32:873–80.
Leitão C, Antunes P, Bastos J, Pinto J, André P. Plastic optical fiber sensor for noninvasive arterial pulse waveform monitoring. IEEE Sens J. 2015;15:14–8.
Leitão C, Antunes P, Pinto J, Bastos J, André P. Optical fiber sensors for central arterial pressure monitoring. Opt Quant Electron J. 2016;48:218.
Leitão C, Antunes P, Pinto J, Bastos J, André P. Carotid distension waves acquired with a fiber sensor as an alternative to tonometry for central arterial systolic pressure assessment in young subjects. Measurement. 2017;95:45–9.
Alberto N, Bilro L, Antunes P, Leitao C, Lima H, André P, et al. Optical fiber technology for eHealthcare. In: Cruz-Cunha M, Miranda I, Goncalves P, editors. Handbook of research on ICTs and management systems for improving efficiency in healthcare and social care. Hershey: IGI Global; 2013. p. 180–200.
Wilkinson I, McEniery M, Schillaci G, Boutouyrie P, Segers P, Donald A, et al. On behalf of the ARTERY Society. ARTERY Society guidelines for validation of non-invasive haemodynamic measurement devices: part 1, arterial pulse wave velocity. Artery Res. 2010;4:34–40.
Sztrymf B, Jacobs F, Chemla D, Richard C, Millasseau S. Validation of the new Complior sensor to record pressure signals non-invasively. J Clin Monit Comput. 2013;27:613–9.
Pereira T, Maldonado J, Coutinho R, Cardoso E, Laranjeiro M, Andrade I, et al. Invasive validation of the Complior Analyse in the assessment of central artery pressure curves: a methodological study. Blood Press Monit. 2014;19:280–7.
Bortel L, Laurent S, Boutouyrie P, Chowienczyk P, Cruickshank J. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity. J Hypertens. 2012;30:445–8.
Zhang Y, Agnoletti D, Safar M, Wang JG, Topouchian J, Xu Y, et al. Comparison study of central blood pressure and wave reflection obtained from tonometry-based devices. Am J Hypertens. 2013;26:34–41.
Zuo J, Li Y, Yan Z, Zhang R, Shen W, Zhu D. Validation of the central blood pressure estimation by the SphygmoCor system in Chinese. Blood Press Monit. 2010;15:268–74.
Pucci G, Cheriyan J, Hubsch A, Hickson S, Gajendragadkar P, Watson T, et al. Evaluation of the Vicorder, a novel cuff-based device for the noninvasive estimation of central blood pressure. J Hypertens. 2013;31:77–85.
Acknowledgements
This work is funded by FEDER funds through the COMPETE 2020 Program and National Funds through FCT—the Portuguese Foundation for Science and Technology—under the project codes UID/EEA/50008/2013,UID/CTM/50025/2013 and UID/MAT/04106/2013. All authors are grateful for the extraordinary collaboration of the staff of the Unidade de Intervenção Cardiovascular – CHUC HG, and, in particular, to Dr. Marco Costa, Dr. Raquel Fernandes, Dr. Romeu Cação, Dr. Susana Margalho, Dr. Luís Paiva, Dr. Toni de Sousa, Dr. Joana Silva, Dr. Rafaela Ramos, and Prof. Lino Gonçalves. The authors are also grateful for the support received from the Serviço de Cardiologia - Centro Hospital do Baixo Vouga, and, in particular, to Dr. José António and Dr. Catarina Gabriel.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Leitão, C., Ribau, V., Afreixo, V. et al. Clinical evaluation of an optical fiber-based probe for the assessment of central arterial pulse waves. Hypertens Res 41, 904–912 (2018). https://doi.org/10.1038/s41440-018-0089-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0089-2