Abstract
With the advent of precision and genomic medicine, a critical issue is whether a disease gene variant is pathogenic or benign. Such is the case for the three autosomal dominant acute hepatic porphyrias (AHPs), including acute intermittent porphyria, hereditary coproporphyria, and variegate porphyria, each resulting from the half-normal enzymatic activities of hydroxymethylbilane synthase, coproporphyrinogen oxidase, and protoporphyrinogen oxidase, respectively. To date, there is no public database that documents the likely pathogenicity of variants causing the porphyrias, and more specifically, the AHPs with biochemically and clinically verified information. Therefore, an international collaborative with the European Porphyria Network and the National Institutes of Health/National Center for Advancing Translational Sciences/National Institute of Diabetes and Digestive and Kidney Diseases (NIH/NCATS/NIDDK)-sponsored Porphyrias Consortium of porphyria diagnostic experts is establishing an online database that will collate biochemical and clinical evidence verifying the pathogenicity of the published and newly identified variants in the AHP-causing genes. The overall goal of the International Porphyria Molecular Diagnostic Collaborative is to determine the pathogenic and benign variants for all eight porphyrias. Here we describe the overall objectives and the initial efforts to validate pathogenic and benign variants in the respective heme biosynthetic genes causing the AHPs.
Similar content being viewed by others
INTRODUCTION
The acute hepatic porphyrias
The acute hepatic porphyrias (AHPs) include four inherited genetic disorders of heme biosynthesis, which are characterized by acute life-threatening attacks of nonspecific neurologic symptoms.1,2,3,4 Each of the AHPs results from the deficient activity of a distinct enzyme in the heme biosynthetic pathway. Table 1 summarizes the specific enzymatic deficiencies that cause the four AHPs: the three autosomal dominant disorders, acute intermittent porphyria (AIP), hereditary coproporphyria (HCP), variegate porphyria (VP), and the very rare autosomal recessive aminolevulinic acid dehydratase deficient porphyria (ADP). The autosomal dominant AHPs are distinct from other porphyrias because of their common overproduction of the porphyrin precursors, 5-aminolevulinic acid (ALA) and porphobilinogen (PBG), which are understood to mediate the acute attack symptoms through a neurotoxic mechanism.1,2,5 The major manifestations of the acute porphyrias are therefore neurologic, including excruciating abdominal pain, a progressive peripheral neuropathy, and mental disturbances (e.g., confusion, fatigue, insomnia, etc.).1,2,4 The AHP neurovisceral attacks generally occur after puberty, are more common in women, and are currently most efficiently treated by intravenously restoring hepatic heme homeostasis with human hemin (Panhematin, Recordati Rare Diseases) or heme arginate (Normosang, Orphan Europe Recordati Group). Photosensitive skin lesions are not a feature of AIP, whereas patients with VP or HCP can present with either cutaneous or neurovisceral symptoms or both.
Although the specific enzyme and gene defects for each disorder were identified decades ago,1 diagnosis of these disorders still presents formidable challenges because their symptoms and signs may mimic other, more common conditions and the correct diagnosis depends on specialized laboratory services. Notably, delaying diagnosis and treatment of acute porphyric attacks can be fatal or cause long-term permanent neurological damage.
Biochemical and molecular diagnosis of the AHPs
A porphyria diagnosis depends on laboratory investigations to demonstrate the pattern of heme precursor accumulation and excretion specific for each type of porphyria. Acute attacks of porphyria are diagnosed by showing marked elevation of urinary PBG and ALA, the diagnostic “gold standard” of these diseases, with analysis of plasma and fecal porphyrins necessary to differentiate among the different AHPs.6,7,8 Elevated levels of the plasma porphyrin precursors can also be detected by more sensitive mass spectrometry methods, although these are not yet widely available.9 With the isolation and characterization of the heme biosynthetic genes and identification of the pathogenic variants causing these diseases,1,2 genetic analyses provide confirmatory diagnoses and identify the specific pathogenic AHP gene variants, enabling the screening of asymptomatic at-risk family members (i.e., “latent heterozygotes”) who should be counseled to avoid factors that are known to precipitate acute attacks.1,2,4,7,10
RATIONALE FOR AN INTERNATIONAL DIAGNOSTIC DATABASE OF VERIFIED PATHOGENIC AND BENIGN VARIANTS
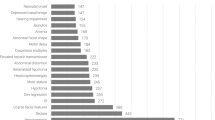
The advent of genetic-based diagnoses of the AHPs presents additional challenges, specifically in determining whether a gene variant is pathogenic or benign. This is a common issue in gene-based diagnostics, as benign variants are common.11 In the past, studies often included a few hundred “normal individuals” as controls to estimate the frequency of newly identified variants, with the assumption that purported pathogenic variants for rare AHPs did not occur in the populations studied. More recently, the availability of exome/genome databases (e.g., gnomAD12) with tens of thousands of alleles from different ethnic and demographic groups has assisted in the confirmation or reclassification of previously diagnosed “pathogenic” variants as either pathogenic or more common benign variants. Table 2 summarizes the reported numbers of the missense, nonsense, and consensus splice-site variants and their allele frequencies (AF) in various ethnic and demographic populations in the gnomAD database12 for the three autosomal dominant AHP-causing genes: hydroxymethylbilane synthase (HMBS), coproporphyrinogen oxidase (CPOX), and protoporphyrinogen oxidase (PPOX).
The Human Gene Mutation Database
To date, the Human Gene Mutation Database (HGMD) has been the most reliable resource for variant data in the AHP genes.13 However, porphyria diagnostic laboratories worldwide frequently identify additional novel pathogenic or benign variants that are not published, and as such are not available in the HGMD.
In addition, the HGMD curation policy includes most published variants,13 although some variants’ pathogenicity may be questionable. In the case of AIP, of the total 423 HMBS variants in version 2019.1, 141 (33%) were missense variants, many of which were reported as disease-causing without sufficient supportive evidence for verification. Several of those initially reported as pathogenic missense variants were subsequently reclassified as “questionably pathogenic” based on subsequent studies of allele frequency, in vitro expression, and in silico prediction analyses.12,14
Intronic variants that alter splicing can also be difficult to assess unless there is clear clinical and biochemical documentation of their pathogenicity. For example, HMBS c.613–31A>G, also known as IVS10–31A>G, was initially reported as a pathogenic variant,15 but subsequently found to be very common in individuals of African or Afro-Caribbean descent.12,16 Although HGMD currently classifies c.613–31A>G as questionably pathogenic,13 recent data in the United States indicate that c.613–31A>G heterozygotes or homozygotes have a benign HMBS polymorphism (gnomAD frequency in Africans: 0.43, Latinos: 0.021, and Caucasians: 0.0023). If it were pathogenic, all homozygotes would be expected to have infantile- or juvenile-onset of homozygous dominant AIP, which is a severe neurodegenerative disorder with early demise.17 Further support for its benign status is the finding of individuals with a known HMBS pathogenic variant and markedly elevated ALA and/or PBG, who were also heterozygous or homozygous for c.613–31A>G, but without severe early-onset symptoms (Table 3). Therefore, there is a need to establish a collaborative database to collect and verify previously reported, as well as currently unreported, AHP pathogenic and benign variants identified in expert porphyria diagnostic laboratories.
Direct-to-consumer testing and variant interpretation services
Another important development in support of a verified database of pathogenic variants is the recent availability of relatively inexpensive direct-to-consumer (DTC) genetic testing. These companies (e.g., 23andMe, AncestryDNA, MyHeritage DNA, FamilyTreeDNA) typically use relatively inexpensive chip-based assays of ~700,000 single-nucleotide polymorphisms (SNPs) to assess ancestry, and determine a very limited number of disease-causing variants, if any. In fact, the US Food and Drug Administration limits the type of health-related information that DTC companies can market. Recently, individuals who have negative biochemical test results for the AHPs have obtained their underlying DTC genotype data and used third-party companies to interrogate the SNPs in the heme biosynthetic genes. Most of these SNPs are intronic, and the few exonic alterations are typically benign common polymorphisms that do not cause porphyria, including the CPOX4 variant (rs1131857, NM_000097.5:c.814>C) that reduces enzyme activity, but not sufficiently to cause HCP. In particular, these SNPs are also limited in number, with fewer than ten pathogenic variants screened for the HMBS, CPOX, and PPOX genes whose messenger RNA (mRNA) transcripts are over 1000 nucleotides. The DTC test analyses are therefore not designed to diagnose the porphyrias. In contrast, certified diagnostic laboratories sequence the entire coding sequence, the exon–intron boundaries, and the upstream promoter (5′) and downstream (3′) regions of each heme biosynthetic gene, and can identify all pathogenic and benign variants by Sanger sequencing, or by RNA or multiple ligation-dependent probe amplification (MLPA) analysis.
Importantly, the inaccuracy of DTC gene testing and misinterpretation of the underlying sequence data were highlighted in a recent article18 and editorial titled “Attention: direct-to-consumer patrons: proceed with caution.”19 The authors call attention to the fact that often the DTC test results were inaccurate as they were not confirmed by a certified diagnostic laboratory. Moreover, many SNPs that were confirmed were actually benign. These findings further support the need for a public database of verified pathogenic variants that is curated by disease-specific experts.
ACMG and AMP guidelines for sequence variant classification
To address the problem of sequence variant classification, the American College of Medical Genetics and Genomics (ACMG) and the Association for Molecular Pathology (AMP) produced guidelines that take into account population, computational, functional, and segregation data.20 This provides a framework to enable classification of variants as “pathogenic,” “likely pathogenic,” “uncertain significance,” “likely benign,” or “benign.” It has been noted that more focused guidance regarding the classification in specific genes is required as the applicability of certain criteria may vary by disease and gene.21,22 This supports the need to establish a disease-specific criteria and public database providing up-to-date information that will allow porphyria specialists to make informed decisions on the classification of variants in the AHP genes. The guidelines will continue to develop so that the reclassification of variants will be ongoing. Classification within the database will therefore be advisory and it will remain the responsibility of individual reporting laboratories to confirm the classification.
Rationale for a database of validated porphyria variants
The importance of human variant databases for identifying pathogenic and likely pathogenic variants causing specific genetic disorders has been the subject of several previous publications (e.g., refs. 23,24,25). Efforts have primarily focused on the assessment of variants that have been identified by exome and genome sequencing or by targeted sequencing of specific genes in patients with Mendelian or complex traits.26 Variant databases such as ClinVar (www.ncbi.nlm.nih.gov/clinvar) have been established to document the validity of gene–disease associations, and in particular, the pathogenicity of variants within genes to inform accurate diagnosis and guide patient care. For ClinVar, Clinical Domain Working Groups were established by the Clinical Genome Resource Consortium (ClinGen) of the National Human Genome Research Institute in conjunction with the National Center for Biotechnology Information to provide a public resource for diagnostic laboratories, researchers, and clinicians to collect and share genomic data, to ultimately determine the pathogenicity of specific variants identified with genome/exome and targeted sequencing by research investigators and commercial laboratories.27
Clearly, for a given disease or disease group, validation of a variant’s pathogenicity can optimally be assessed by disease experts working together with disease-specific diagnostic laboratories. Here, an international group of porphyria experts has established a consensus statement for the validation of pathogenic variants in the heme biosynthetic genes causing the AHPs. In addition, we outline the efforts of the International Porphyrias Molecular Diagnostic Consortium to verify the published and currently unreported variants detected by expert porphyria laboratories in patients with the eight major porphyrias based on their diagnostic biochemical findings.
FORMATION OF THE INTERNATIONAL PORPHYRIA MOLECULAR DIAGNOSTIC COLLABORATIVE
At the 2017 International Congress on Porphyrins and Porphyrias (ICPP) in Bordeaux, France, one of the authors (R.J.D.) proposed an International Collaborative to bring together experts in the biochemical and molecular diagnosis of the porphyrias to establish porphyria-specific evidence criteria and a public database of the validated pathogenic and benign variants in the heme biosynthesis genes, as well as an updated diagnostic consensus by international experts. Genetic alterations that cause porphyrias will be classified as pathogenic or likely pathogenic variants, whereas genetic alterations that have high allele frequency or that lack supportive biochemical and in vitro evidence will be classified as benign or likely benign variants. Genetic alterations with inconclusive evidence for pathogenicity will be classified as variants of unknown significance (VUS). Table 4 provides some examples of the evidence criteria for variant classification.
The database will validate as many of the published genetic alterations as possible for each porphyria based on de-identified clinical and biochemical data. In addition, benign variants identified by gene sequencing or genomic/exomic sequencing databases can be verified by high enzyme activity levels when expressed in vitro, in silico predictive algorithms, and/or relatively high frequencies in genomic/exomic databases. The database will be regularly updated with new pathogenic and benign variants identified by the participating expert laboratories. The International Collaborative will leverage participants’ cumulative clinical expertise and biochemical data to rigorously assess each variant’s pathogenicity. To pilot this International Collaborative, the initial goal will focus on collating pathogenic and benign variants in the genes causing the three autosomal dominant AHPs.
Porphyria experts from countries worldwide indicated their support of the International Collaborative, including the European Porphyria Network (EPNET) and the US Porphyrias Consortium. To date, EPNET and Porphyrias Consortium members have established the following objectives for the International Collaborative: (1) establish a database of validated porphyria pathogenic variants, initially for the three autosomal dominant AHPs; (2) determine qualifying criteria for expert contributing diagnostic laboratories; (3) determine the validation requirements for each porphyria; and (4) enroll qualified porphyria diagnostic laboratories.
Database information
The database will provide two main features related to the diagnosis of the porphyrias: (1) a genetic variant search tool that will list validated pathogenic and benign variants classified according to current guidelines, and (2) a submission form to facilitate the contribution of new variants. The variant search tool will allow users to search for a gene alteration and provide information that supports its pathogenic or benign determination or its undetermined status. The electronic submission form provides the opportunity to submit novel genetic variants, which will be incorporated into the database after curation.
The database will follow the latest recommendations from the Human Genome Variation Society (HGVS) for the sequence nomenclature28 but will also include “historical/legacy nomenclature” (e.g., IVS for intronic variants). The description is generally in reference to the respective standard sequence in the RefSeq collection (e.g., for HMBS, NM_000190.3, for CPOX, NM_000097.5, and for PPOX, NM_000309.4) or the stable Locus Reference Genomic identifier (e.g., for HMBS, LRG_1076, and for CPOX, LRG_1077). For alterations that are in the coding region, additional descriptions at the protein level will be provided, including the exon number and the protein reference ID (e.g., for HMBS, NP_000181.2; for CPOX, NP_000088.3; and for PPOX, NP_000300.1). If a variant has been reported in the literature, hyperlinks to the publications will be available for users to find additional information about the variant. For a pathogenic variant, clinical and/or biochemical information associated with the variant, together with additional data from in vitro assays, will be presented. For variants that have been identified in multiple probands, individual clinical, biochemical, and in vitro data will be summarized.
For variant data submission, the database will require, wherever possible, that the submitter provide de-identified clinical (i.e., cyclic, multiple, or sporadic attacks) and biochemical information (i.e., urinary and/or plasma ALA and/or PBG concentrations, fecal and plasma porphyrin data) to document the variant’s pathogenicity, or classification as benign or likely benign. Additional data from other analyses such as in vitro assays (e.g., enzyme assay, luciferase activity, or reverse transcription polymerase chain reaction [RT-PCR] studies), or in silico prediction algorithms will be recorded.
Criteria for contributing laboratories
The database aims to collect variant data submitted from expert diagnostic laboratories worldwide. Therefore, it is important to ensure that contributing laboratories perform genetic testing under an internationally recognized standard (ISO), such as ISO 15189 (ref. 8). All contributing laboratories will be expected to participate in the quality assurance program of the European Molecular Genetics Quality Network (EMQN) and in the EPNET External Quality Assessment Scheme for the porphyrias or other similar quality assurance programs. At this writing, the Collaborative is in the process of establishing the full criteria for contributing laboratories.
Genetic variant validation
The major activity of the International Collaborative will be to validate the pathogenicity of variants in the AHP-causing genes using clinical, biochemical, and other supporting data (Table 4) in line with current guidelines.20
The gold standard for validating the pathogenicity of an AHP gene alteration for patients presenting with acute symptoms is the demonstration of markedly elevated urinary and/or plasma ALA and PBG concentrations when the patient is symptomatic,6 positive concentrations being at least fourfold greater than the upper limit of normal values for a given laboratory. In the above situation, and in VP or HCP patients presenting with skin lesions only, and where urine and plasma PBG and ALA are likely normal, unequivocal biochemical confirmation will rely on plasma and fecal porphyrin analysis to distinguish among the AHPs.8,29 Porphyrin biochemistry diagnostic of a specific AHP can be used within the Association for Clinical Genomic Science (ACGS) guidelines as strong evidence toward pathogenicity, as it is an aspect of the disease that is measurable and is pathognomonic of a defect in one of the AHPs.21,22
It is important to note that a major focus of validation will be directed toward variants that are challenging to distinguish if they are pathogenic or benign. These variants primarily include missense and nonconsensus splice-site alterations, other intronic changes that can cause alternative splicing, and in-frame deletions or insertions that delete or insert amino acids without changing the rest of the encoded amino acid sequence.
METHODS FOR VARIANT VALIDATION
Porphyrin precursor measurements
When a patient is clinically suspected of having an acute neurovisceral attack, the first-line diagnostic test is an urgent spot urinary ALA and/or PBG determination, which should be normalized to the urine creatinine. A normal urinary PBG or near normal ALA and/or PBG excretion before treatment with human hemin or heme arginate excludes the diagnosis of an AHP in symptomatic new patients. In AIP patients, PBG and ALA may decrease after an attack but often remain somewhat elevated for years,30 while in HCP and VP, PBG and ALA excretion may decline more rapidly. A proportion of AHP patients may also have constantly elevated ALA and PBG levels in the absence of symptoms and are termed chronic high excretors.30,31
Since precursor levels during an attack are markedly elevated, preanalytical factors (e.g., exposure to light, lack of refrigeration) and/or shipping conditions (e.g., unfrozen, prolonged transit time) are unlikely to reduce the high levels of excretion into the normal range. However, with spot samples it is important to normalize values to the urine creatinine concentration. A subsequent measurement of total fecal porphyrins, the fecal coproporphyrin isomer III:I ratio, and the fluorescence emission spectrum of plasma porphyrins will distinguish among VP, HCP, and AIP.29,32 Table 5 summarizes key porphyrin biochemical findings characteristic of active acute AHPs.
Enzyme assays
Measurements of erythrocyte HMBS activity have been used in the past to help confirm the diagnosis of AIP.33 For HCP and VP, the leukocyte enzyme assays from blood samples are technically challenging and are not widely used.34,35,36 A major issue with the enzyme assays is the significant overlap of HMBS, CPOX, or PPOX enzymatic activity between high heterozygote and low normal ranges, which can lead to inconclusive results.37,38,39,40,41,42,43 HMBS activity is affected by the average age of the red cells in the collected sample, being higher in younger cells. In addition, for the diagnosis of AIP, HMBS variants in the codons of exon 1 and in intron 1 that alter normal splicing of the housekeeping transcript will markedly decrease the activity of the housekeeping HMBS isozyme (for review, see ref. 44) but will not alter the normal expression of the erythroid-specific isozyme, thereby leading to missed diagnoses if used in isolation.43,45,46
In vitro expression of missense variants and in-frame deletions and insertions helps classify these variants identified in patients or in exome/genome databases (e.g., ref. 12). In vitro expression of questionable missense variants can confirm pathogenicity when the enzyme activity is markedly deficient (<10%) and benign variants when the enzyme activity is >50%. Most deleterious variants showed very low or no residual activity;47 nevertheless, there is no consensus as to what the cutoff is for a few variants with activity between 10% and 40% of the wildtype expressed activity. For variants with significant residual activity, it is useful to determine the stability of the expressed enzyme, for example, by heat inactivation analysis.14
RNA analysis
Routine Sanger sequencing should identify >98% of HMBS, CPOX, PPOX, or ALAD variants in AHP patients.29 However, “cryptic” variants do occur rarely, in which the alterations are intronic, creating an alternative splice site, or occur in the promoter region altering expression. mRNA analysis, MLPA, or expression reporter assays (e.g., luciferase reporter assays) can be used to determine the effects of such variants.
In silico analysis
In silico predictive programs can also aid in the determination of pathogenicity for novel genetic variants. Although individual programs use different sets of principles for their prediction, many include sequence conservation and biophysical and biochemical properties of the amino acids as part of their criteria. It should be noted that current prediction accuracy plateaus at approximately 80% (ref. 48) and many programs have low specificity, resulting in overprediction of genetic variants as pathogenic.49 As such these programs cannot be used alone.
CONCLUSIONS
The AHPs are rare disorders of heme biosynthesis. Accurate diagnosis of an acute porphyria presenting with an acute attack, or cutaneous symptoms in HCP or VP, depends on biochemical testing to confirm active porphyria by demonstrating abnormal porphyrin biochemistry consistent with the specific AHP. Genetic testing is now an established part of managing the families of patients with an AHP diagnosis worldwide. However, predictive genetic testing of at-risk family members requires identification of the symptomatic proband’s specific pathogenic variant. As we move into the era of genomic medicine, genetic testing–based diagnostics will become an ever more common practice and will require disease-specific databases to assist in distinguishing pathogenic from benign variants. Thus, the International Porphyria Molecular Diagnostic Collaborative will provide the combined expertise of an international group of experts to facilitate accurate diagnosis for the porphyria community.
References
Anderson KE, Sassa S, Bishop DF, Desnick RJ. Disorders of heme biosynthesis: X-linked sideroblastic anemia and the porphyrias. In: Beaudet AL, Vogelstein B, Kinzler KW, et al., eds. The online metabolic and molecular bases of inherited disease. New York, NY: McGraw-Hill; 2014. https://ommbid.mhmedical.com/content.aspx?bookid=971§ionid=62638866#1102890723. Accessed 8 May 2019.
Puy H, Gouya L, Deybach JC. Porphyrias. Lancet. 2010;375:924–937.
Bonkovsky HL, Maddukuri VC, Yazici C, et al. Acute porphyrias in the USA: features of 108 subjects from porphyrias consortium. Am J Med. 2014;127:1233–1241.
Bissell DM, Anderson KE, Bonkovsky HL. Porphyria. N Engl J Med. 2017;377:862–872.
Bonkovsky HL, Guo JT, Hou W, Li T, Narang T, Thapar M. Porphyrin and heme metabolism and the porphyrias. Compr Physiol. 2013;3:365–401.
Anderson KE, Bloomer JR, Bonkovsky HL, et al. Recommendations for the diagnosis and treatment of the acute porphyrias. Ann Intern Med. 2005;142:439–450.
Aarsand AK, Petersen PH, Sandberg S. Estimation and application of biological variation of urinary delta-aminolevulinic acid and porphobilinogen in healthy individuals and in patients with acute intermittent porphyria. Clin Chem. 2006;52:650–656.
Woolf J, Marsden JT, Degg T, et al. Best practice guidelines on first-line laboratory testing for porphyria. Ann Clin Biochem. 2017;54:188–198.
Zhang J, Yasuda M, Desnick RJ, Balwani M, Bishop D, Yu C. A LC-MS/MS method for the specific, sensitive, and simultaneous quantification of 5-aminolevulinic acid and porphobilinogen. J Chromatogr B Analyt Technol Biomed Life Sci. 2011;879:2389–2396.
Whatley SD, Badminton MN. Role of genetic testing in the management of patients with inherited porphyria and their families. Ann Clin Biochem. 2013;50:204–216.
The 1000 Genomes Project Consortium. A global reference for human genetic variation. Nature. 2015;526:68–74.
Lek M, Karczewski KJ, Minikel EV, et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature. 2016;536:285–291.
Stenson PD, Mort M, Ball EV, et al. The Human Gene Mutation Database: towards a comprehensive repository of inherited mutation data for medical research, genetic diagnosis and next-generation sequencing studies. Hum Genet. 2017;136:665–677.
Chen B, Solis-Villa C, Hakenberg J, et al. Acute intermittent porphyria: predicted pathogenicity of HMBS variants indicates extremely low penetrance of the autosomal dominant disease. Hum Mutat. 2016;37:1215–1222.
Puy H, Deybach JC, Lamoril J, et al. Molecular epidemiology and diagnosis of PBG deaminase gene defects in acute intermittent porphyria. Am J Hum Genet. 1997;60:1373–1383.
Robreau-Fraolini AM, Puy H, Aquaron C, et al. Porphobilinogen deaminase gene in African and Afro-Caribbean ethnic groups: mutations causing acute intermittent porphyria and specific intragenic polymorphisms. Hum Genet. 2000;107:150–159.
Solis C, Martinez-Bermejo A, Naidich TP, et al. Acute intermittent porphyria: studies of the severe homozygous dominant disease provides insights into the neurologic attacks in acute porphyrias. Arch Neurol. 2004;61:1764–1770.
Tandy-Connor S, Guiltinan J, Krempely K, et al. False-positive results released by direct-to-consumer genetic tests highlight the importance of clinical confirmation testing for appropriate patient care. Genet Med. 2018;20:1515–1521.
Friez MJ. Attention: direct-to-consumer patrons: proceed with caution. Genet Med. 2018;20:1508–1509.
Richards S, Aziz N, Bale S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–424.
Ellard S, Baple EL, Owens M, et al. ACGS Best Practice Guidelines for Variant Classification. 2018. http://www.acgs.uk.com/media/1092626/uk_practice_guidelines_for_variant_classification_2017.pdf. Accessed 27 July 2018.
Ellard S, Baple EL, Owens M, et al. ACGS Best Practice Guidelines for Variant Classification. 2017. http://www.acgs.uk.com/media/1140458/uk_practice_guidelines_for_variant_classification_2018_v1.0.pdf.
Cotton RG, Al Aqeel AI, Al-Mulla F, et al. Capturing all disease-causing mutations for clinical and research use: toward an effortless system for the Human Variome Project. Genet Med. 2009;11:843–849.
Johnston JJ, Biesecker LG. Databases of genomic variation and phenotypes: existing resources and future needs. Hum Mol Genet. 2013;22:R27–R31.
Bennetts B, Caramins M, Hsu A, et al. Quality standards for DNA sequence variation databases to improve clinical management under development in Australia. Appl Transl Genom. 2014;3:54–57.
Adams DR, Eng CM. Next-generation sequencing to diagnose suspected genetic disorders. N Engl J Med. 2018;379:1353–1362.
Milko LV, Funke BH, Hershberger RE, et al. Development of Clinical Domain Working Groups for the Clinical Genome Resource (ClinGen): lessons learned and plans for the future. Genet Med. 2019;21:987–993.
den Dunnen JT, Dalgleish R, Maglott DR, et al. HGVS recommendations for the description of sequence variants: 2016 update. Hum Mutat. 2016;37:564–569.
Whatley SD, Mason NG, Woolf JR, Newcombe RG, Elder GH, Badminton MN. Diagnostic strategies for autosomal dominant acute porphyrias: retrospective analysis of 467 unrelated patients referred for mutational analysis of the HMBS, CPOX, or PPOX gene. Clin Chem. 2009;55:1406–1414.
Marsden JT, Rees DC. Urinary excretion of porphyrins, porphobilinogen and delta-aminolaevulinic acid following an attack of acute intermittent porphyria. J Clin Pathol. 2014;67:60–65.
Balwani M, Wang B, Anderson KE, et al. Acute hepatic porphyrias: recommendations for evaluation and long-term management. Hepatology. 2017;66:1314–1322.
Hift RJ, Davidson BP, van der Hooft C, Meissner DM, Meissner PN. Plasma fluorescence scanning and fecal porphyrin analysis for the diagnosis of variegate porphyria: precise determination of sensitivity and specificity with detection of protoporphyrinogen oxidase mutations as a reference standard. Clin Chem. 2004;50:915–923.
Nordmann Y, Puy H. Human hereditary hepatic porphyrias. Clin Chim Acta. 2002;325:17–37.
Guo R, Lim CK, Peters TJ. Accurate and specific HPLC assay of coproporphyrinogen III oxidase activity in human peripheral leucocytes. Clin Chim Acta. 1988;177:245–252.
Guo R, Lim CK, Peters TJ. High-performance liquid chromatographic assays for protoporphyrinogen oxidase and ferrochelatase in human leucocytes. J Chromatogr. 1991;566:383–396.
Schmitt C, Gouya L, Malonova E, et al. Mutations in human CPO gene predict clinical expression of either hepatic hereditary coproporphyria or erythropoietic harderoporphyria. Hum Mol Genet. 2005;14:3089–3098.
Mustajoki P. Normal erythrocyte uroporphyrinogen I synthase in a kindred with acute intermittent porphyria. Ann Intern Med. 1981;95:162–166.
McColl KE, Moore MR, Thompson GG, Goldberg A. Screening for latent acute intermittent porphyria: the value of measuring both leucocyte delta-aminolaevulinic acid synthase and erythrocyte uroporphyrinogen-1-synthase activities. J Med Genet. 1982;19:271–276.
Bonaiti-Pellie C, Phung L, Nordmann Y. Recurrence risk estimation of acute intermittent porphyria based on analysis of porphobilinogen deaminase activity: a Bayesian approach. Am J Med Genet. 1984;19:755–762.
Lamon JM, Frykholm BC, Tschudy DP. Family evaluations in acute intermittent porphyria using red cell uroporphyrinogen I synthetase. J Med Genet. 1979;16:134–139.
Meissner PN, Day RS, Moore MR, Disler PB, Harley E. Protoporphyrinogen oxidase and porphobilinogen deaminase in variegate porphyria. Eur J Clin Invest. 1986;16:257–261.
Lamoril J, Puy H, Whatley SD, et al. Characterization of mutations in the CPO gene in British patients demonstrates absence of genotype-phenotype correlation and identifies relationship between hereditary coproporphyria and harderoporphyria. Am J Hum Genet. 2001;68:1130–1138.
Mustajoki P, Desnick RJ. Genetic heterogeneity in acute intermittent porphyria: characterisation and frequency of porphobilinogen deaminase mutations in Finland. Br Med J (Clin Res Ed). 1985;291:505–509.
Yasuda M, Chen B, Desnick RJ. Recent advances on porphyria genetics: inheritance, penetrance & molecular heterogeneity, including new modifying/causative genes. Mol Genet Metab. 2018;S1096-7192:30645.
Grandchamp B, De Verneuil H, Beaumont C, Chretien S, Walter O, Nordmann Y. Tissue-specific expression of porphobilinogen deaminase. Two isoenzymes from a single gene. Eur J Biochem. 1987;162:105–110.
Chen CH, Astrin KH, Lee G, Anderson KE, Desnick RJ. Acute intermittent porphyria: identification and expression of exonic mutations in the hydroxymethylbilane synthase gene. An initiation codon missense mutation in the housekeeping transcript causes “variant acute intermittent porphyria” with normal expression of the erythroid-specific enzyme. J Clin Invest. 1994;94:1927–1937.
Lenglet H, Schmitt C, Grange T, et al. From a dominant to an oligogenic model of inheritance with environmental modifiers in acute intermittent porphyria. Hum Mol Genet. 2018;27:1164–1173.
Riera C, Lois S, de la Cruz X. Prediction of pathological mutations in proteins: the challenge of integrating sequence conservation and structure stability principles. WIREs Comput Mol Sci. 2014;4:249–268.
Choi Y, Sims GE, Murphy S, Miller JR, Chan AP. Predicting the functional effect of amino acid substitutions and indels. PLoS ONE. 2012;7:e46688.
Acknowledgements
We acknowledge the support of the other members of the European Porphyria Network Executive Board: Eliane Sardh (Porphyria Centre Sweden, Centre for Inborn Errors of Metabolism, Karolinska Institutet, Karolinska University Hospital, Stockholm, Sweden) and Janneke Langendonk (Porphyria Center Rotterdam, Erasmus MC, University Medical Center Rotterdam, the Netherlands).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosure
K.E.A., R.J.D., and J.D.P. are consultants for Alnylam Pharmaceuticals, Recordati Rare Diseases, Mitsubishi Tanabe Pharma. R.J.D. and M.Y. are inventors of intellectual property licensed to Alnylam Pharmaceuticals. K.E.A., R.J.D., and M.Y. have received research grants from Alnylam Pharmaceuticals and Recordati Rare Diseases. J.-C.D. is a consultant for Alnylam Pharmaceuticals and Orphan Europe Recordati Group. H.L.B. is a consultant for Alnylam Pharmaceuticals, Recordati Rare Diseases, and Moderna Therapeutics, Inc. and has received research grants from Alnylam Pharmaceuticals and Gilead Sciences, Inc. E.C.H.F. has received lodging support from Alnylam Pharmaceuticals. The respective honorarium from Alnylam for participating in an advisory group has been paid to Erasmus MC. A.A.K. has received travel and accommodation support from Clinuvel Pharmaceuticals. L.G. has received travel and lodging support from Alnylam Pharmaceuticals and Clinuvel Pharmaceuticals (no honorarium). P.H. has received travel and lodging support from Alnylam Pharmaceuticals and Clinuvel Pharmaceuticals. The respective honorarium from Alnylam for participating in an advisory group has been paid to Karolinska University Hospital or Karolinska Institutet. R.K. received travel and lodging support from Alnylam Pharmaceuticals and Clinuvel Pharmaceuticals and holds stock in Orion Pharma. S.S. received an honorarium from Alnylam for participating in an advisory group. J.T.-F. was compensated for limited in time consulting services by Moderna Therapeutics and Alnylam Pharmaceuticals Spain, SL. This work was primarily supported by the Department of Genetics and Genomic Sciences of the Icahn School of Medicine at Mount Sinai. K.E.A., D.M.B., H.L.B., R.J.D., and J.D.P. receive salary support from the Porphyrias Consortium (U54DK083909), which is part of the National Center for Advancing Translational Sciences (NCATS) Rare Diseases Clinical Research Network (RDCRN) of the National Institutes of Health (NIH). RDCRN is an initiative of the Office of Rare Diseases Research (ORDR), NCATS, funded through collaboration between NCATS and the National Institute for Diabetes and Digestive and Kidney Diseases (NIDDK). The other authors declare no conflicts of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, B., Whatley, S., Badminton, M. et al. International Porphyria Molecular Diagnostic Collaborative: an evidence-based database of verified pathogenic and benign variants for the porphyrias. Genet Med 21, 2605–2613 (2019). https://doi.org/10.1038/s41436-019-0537-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-019-0537-7