Abstract
Purpose
Exome sequencing (ES) is an efficient tool to diagnose genetic disorders postnatally. Recent studies show that it may have a considerable diagnostic yield in fetuses with structural anomalies on ultrasound. We report on the clinical impact of the implementation of prenatal ES (pES) for ongoing pregnancies in routine care.
Methods
We retrospectively analyzed the impact of pES on pregnancy outcome and pre- or perinatal management in the first 22 patients counseled for pES because of one or more structural anomalies on fetal ultrasound.
Results
In two cases, a diagnosis was made by chromosomal microarray analysis after ES counseling. The remaining 20 cases were divided in three groups: (1) pES to aid parental decision making (n = 12), (2) pES in the context of late pregnancy termination requests (n = 5), and (3) pES to guide pre- or perinatal management (n = 3). pES had a clinical impact in 75% (9/12), 40% (2/5), and 100% (3/3) respectively, showing an overall clinical impact of pES of 70% (14/20).
Conclusion
We show that clinical implementation of pES is feasible and affects parental decision making or pre- and perinatal management supporting further implementation of ES in the prenatal setting.
Similar content being viewed by others
INTRODUCTION
Congenital anomalies affect 2–3% of births1 and are a leading cause of perinatal mortality.2 Most countries have implemented ultrasound screening programs to detect congenital anomalies. It is essential to know if an anomaly is isolated or part of a genetic syndrome, as this may greatly affect the prognosis. At present, widely used prenatal diagnostic tools include karyotyping, aneuploidy screening using quantitative fluorescent polymerase chain reaction (QF-PCR), chromosomal microarray analysis (CMA), and when indicated, detection of infections. Karyotyping identifies chromosome abnormalities and imbalances between 5–10 Mb, depending on the location and chromosome quality, while QF-PCR detects trisomy 13, 18, 21, and aneuploidy of the sex chromosomes. With the implementation of CMA, diagnostic yield increased with 5–7% (refs. 3,4) over standard karyotyping in fetuses with structural malformations on ultrasound. Although CMA is able to detect copy-number variations (CNV’s) as small as 10–100 kb, smaller variants remain undetected and these represent a considerable part of the causes of genetic disorders.5
Exome sequencing (ES) is gaining momentum as a diagnostic tool for genetic disorders. By sequencing all protein encoding genes, ES is able to detect single-nucleotide variants and small duplications or deletions.6 Wright et al. investigated the diagnostic yield of ES in infants with severe undiagnosed developmental disorders, establishing a molecular diagnosis in 27% of their cohort.7 Recent studies investigated the diagnostic utility of ES on prenatally identified cases and reported diagnostic yields ranging from 8.5% to 81% (refs. 8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24), where higher yields are identified in more stringently selected cohorts. So far however, only Chandler et al.,15 Pangalos et al.,17 and Normand et al.22 reported on the results of prenatal ES (pES) during pregnancy, but these studies focus on diagnostic yield and not on the clinical impact of pES. Retrospective studies have stressed the potential difficulties faced when implementing pES, such as the relatively high risk of finding variants of unknown significance (VUS) and the limited information about the phenotype, which can make interpretation of the pES results complex. Other potential implementation issues of pES can only be assessed by actual clinical implementation, such as limited availability of fetal material, the ad hoc need of multidisciplinary meetings to rapidly interpret gene variants, and the robustness of ES protocols with short turnaround times. We report our experiences with the first 22 consecutive referrals for pES in a clinical setting, focusing on the impact of pES on the parental decision process during pregnancy and on guiding pre- and perinatal management.
MATERIALS AND METHODS
Patient selection and data collection
We performed a retrospective analysis of the clinical impact in the first 22 consecutive pregnancies referred for pES counseling. In our hospital, pregnancies are eligible for pES when fetuses show one or more structural anomalies on ultrasound, with an increased risk of an underlying genetic cause based on clinical experience or literature. In addition, the upper limit of the gestational age is 22 + 0 weeks to achieve a result before 24 + 0 weeks (which is the upper limit for termination of pregnancy [TOP] in the Netherlands). Patients with a TOP request after 24 + 0 weeks of gestation (which can be performed in the Netherlands in a strictly regulated setting, and requires a confident diagnosis and an extremely poor prognosis) are eligible for pES as well, as are patients for whom pES could have consequences on pre- or perinatal management. pES is not offered to patients who had already decided on continuation or termination of pregnancy based solely on the imaging results.
Patients underwent invasive procedures (mostly amniocentesis and in two cases chorionic villi sampling [CVS]) to obtain fetal samples for prenatal diagnostics including QF-PCR, CMA, and ES. Prior to ES initiation, written informed consent for clinical testing was collected of all patients. When CMA results were not available before 22 + 0 weeks of gestation, pES was initiated in parallel to report pES results before 24 weeks of gestation.
Data on clinical impact were collected retrospectively from patient files. A waiver to obtain approval was obtained from the institutional review board of the Leiden University Medical Center (LUMC). Clinical impact of pES is defined as:
-
The pES result significantly influencing the decision on TOP, or
-
The pES result supported the request for late TOP, or
-
The pES result changed intended pre- or perinatal management.
Exome sequencing
Details on laboratory procedures and bioinformatics can be found in the Supplementary Materials and Methods. When available, trio samples of the fetus and both parents were used for sequencing to shorten turnaround times and optimize variant filtering. First the DDG2P gene panel (www.ebi.ac.uk/gene2phenotype) was analyzed, which is one of the most comprehensive publicly available gene panels focused on postnatal setting and developed by the European Bioinformatics Institute, directly followed by a full exome analysis if no pathogenic variant was found in the panel. Turnaround time (TAT) was defined as days between request of pES until final diagnostic report.
Variants were classified according to the American College of Medical Genetics and Genomics (ACMG) guidelines.25 Variants classified as VUS and (likely) pathogenic were submitted to the DECIPHER database. VUS were discussed between laboratory specialists and clinical specialists and only reported to the patient if considered potentially relevant.
Secondary findings (likely pathogenic variants in disease genes) were discussed between clinical and laboratory specialists and relayed to the parents depending on their consent.
RESULTS
Clinical implementation
Potential pES candidates were discussed in a multidisciplinary team with obstetricians, clinical geneticists, clinical laboratory geneticists, and fetal medicine subspecialists on an ad hoc basis or during the weekly fetal rounds. In total, 23 couples were approached for pES and 22 consented.
In two pregnancies, a genetic diagnosis was obtained by CMA. In the first (findings: tetralogy of Fallot), a 22q11.2 deletion was detected using CMA prior to pES initiation. In the second pregnancy (findings: bilateral choroid plexus cysts, cardiac asymmetry, suspected hypospadias, contractures of the extremities, micrognathia, and prenasal edema), pES did not identify a causative variant, but CMA detected a large de novo interstitial deletion on chromosome 5 (q11.2q13.2), which was considered causal. Because this study is focused on the clinical impact of pES, we are not including these pregnancies in the following paragraphs.
Of the remaining 20 pES cases, TAT was less than 17 days in all except one case in which the diagnosis was initially missed (case 14). Most of the identified variants were clearly pathogenic and did not require extensive multidisciplinary team discussions, except for the SHH variant in case 11, which is discussed in detail below. No Sanger confirmation of variants was performed because all variants fulfilled required criteria.
Case 11 was the only case to require a second amniocentesis, because there was insufficient DNA and no time to wait for the slowly growing backup cultures. Most tests were performed directly on DNA isolated from amniocentesis or CVS, except in case 20 where amniocentesis was performed at 16 weeks, and in case 1 were CVS was performed at 11 weeks.
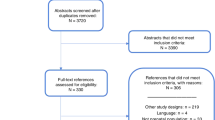
Diagnostic impact
Broadly, three groups of patients can be discerned. In group 1, pES was performed mainly to aid parents in their decision process, mandating a result before the legal limit for TOP (24 + 0 weeks of gestation in the Netherlands). Typically, the anomalies were operable or carried a moderate to good prognosis in the absence of a genetic syndrome. The defects in this group were, however, known or suspected to be associated with genetic syndromes in general. This situation caused uncertainty and doubt about continuation of the pregnancy in the parents. In group 2, pES was performed in the context of a request for late TOP. In group 3 pES was performed to guide pre- or perinatal management typically concerning cases with severe anomalies, not lethal in itself, in which parents decided not to terminate the pregnancy. In Fig. 1, the turnaround time of pES from request to reported result is depicted per subgroup. Urgency was most important in group 1, as reflected by the shortest reporting times (Fig. 1). Details about each case including prenatal phenotype and pES results are described in Table 1.
Group 1: prenatal exome sequencing to aid parental decision making
pES was performed around 20–21 weeks of gestation to guide a decision to continue or terminate the pregnancy in 12 pregnancies. A genetic diagnosis was obtained in four pregnancies (33.3%). Parents decided on TOP in all four pregnancies. In cases 1, 2, and 3, parents indicated they would have continued the pregnancy in the absence of a certain diagnosis. For example, in case 1, an increased nuchal translucency (NT) was detected in the first trimester. CMA did not identify any anomalies. Later, isolated agenesis of the corpus callosum was identified and subsequently hypospadias. Although these separate findings have good prognoses, we considered that the combination increased the susceptibility of a syndromic cause. pES was therefore offered and detected a pathogenic variant in ZEB2 confirming Mowat–Wilson syndrome (OMIM 235730). The parents rejected TOP solely based on suspicion of a genetic syndrome, but upon this diagnosis, they requested TOP (Supplementary Material). Similarly, in case 2, a Blake’s pouch cyst and a hypoplasia of the corpus callosum were identified. Both findings have a relatively good prognosis when isolated, but the combination was considered to raise the chance of an underlying genetic cause. The results of pES identified Joubert syndrome (OMIM 616490) and led parents to request TOP. Again in this case, parents clearly indicated that TOP based solely on the ultrasound findings would not have been an option (Supplementary Material).
In case 4, in which gyration was delayed, parents indicated they would opt for TOP in the absence of a genetic diagnosis, if no clear progression in gyration was seen on the US that was made just before the legal limit of TOP. Because progression of gyration would be difficult to show with great certainty in just two weeks, we therefore considered that pES did not have a clinical impact in case 4.
In eight pregnancies pES did not reveal a definitive genetic cause. In case 11, the fetus had a cardiac anomaly and a secondary finding in SHH was identified. This case was the only pregnancy where paternal DNA was not available because this fetus was conceived with an anonymous sperm donor, which complicated interpretation. The identified SHH variant changed an amino acid that was previously mutated in a large pedigree with holoprosencephaly.26 The fetus underwent neurosonography, without abnormal findings. Because cardiac malformations are not regularly described in patients with pathogenic variants in SHH, this variant was classified as a secondary finding. The pregnancy was continued, but postnatally there was an evident micrognathia, reminiscent of the mild end of the agnathia–otocephaly spectrum. This complicated ventilation and eventually contributed to his death. After the pregnancy, paternal DNA was obtained and the variant was shown to be de novo. In case 12, a paternally inherited pathogenic variant in PMS2 was detected and reported as a secondary finding.
In one of the other six pregnancies without a detected causative variant, the fetus suffered from skeletal dysplasia and eventually, with increasing severity of the skeletal anomalies, the parents chose TOP based on the ultrasound findings (case 5). The pregnancy of case 8 ended in intrauterine fetal demise at 21 weeks of gestation. The five other pregnancies in which pES did not result in a diagnosis were continued, and the pES results were cited as a key factor in this decision by most of the patients (Supplementary Material). Three pregnancies are still ongoing, and the other two fetuses presented postnatally with operable anomalies (Table 1). Thus, pES had an impact on parental decision making in 9 of the 12 cases (75%).
Group 2: prenatal exome sequencing in the context of late pregnancy termination requests
In five pregnancies pES was performed in cases where parents indicated they might consider requesting late TOP. In two cases, the pES results supported this request because the diagnoses were associated with an extremely poor neonatal prognosis and the pES results narrowed the uncertainty about the prognoses based on imaging alone. The homozygous deletion of the ATAD3A and ATAD3B genes27 in case 14 was initially not detected by CMA (due to the presence of pseudogenes) or ES (because we had not implemented a pipeline to detect CNVs). Based on the pre- and postnatal clinical findings in an earlier affected child of this couple, ATAD3A was suggested as a potentially causal gene. ES data were manually interrogated and a homozygous deletion was visually identified.
Group 3: prenatal exome sequencing to guide pre- or perinatal management
In two of three pregnancies (66.6%) in which pES was performed to guide pre- or perinatal management, a genetic cause was identified. In case 19, the prognosis based on the genetic diagnosis was severe enough to warrant a decision to restrict care after birth, but the pregnancy ended in intrauterine fetal demise at 35 weeks of gestation. In case 18, Kabuki syndrome (OMIM 147920) was diagnosed, which led to the decision of optimal postnatal care in a case of multilevel left heart obstruction (Shone complex). In spite of this, the neonate demised at the age of 17 days, due to cardiac failure after aortic coarctation repair. In case 20, pES was performed in a fetus with severe hydrops in a consanguineous couple where multiple regions of homozygosity (ROH) were detected by CMA. The distribution of the hydrops was slightly atypical for the diagnosis chylothorax, therefore the fetal therapy team was reluctant to place thorax shunts because of a high suspicion of an underlying genetic syndrome. No causative variant was identified, but a homozygous VUS in UQCRC2 was reported as a secondary finding. After these results, shunts were placed and the fetal hydrops disappeared. This pregnancy resulted in live birth at 30 weeks of gestation when a coronary fistula was noted. At 6 months, several mild dysmorphic features were noted and development seemed normal.
DISCUSSION
Clinical impact
To our knowledge, this is the first report to focus on the clinical impact of pES. The clinical impact in cases where a diagnosis was established is evident, but also in the absence of a diagnosis parents cited the pES result as one of the key factors in their decision (Supplementary Material), although we cannot be sure if all of these couples would have also continued the pregnancy if pES had not been offered.
Following this reasoning, we consider that pES had a significant clinical impact on parental decision making in 75% of the cases where pES was performed to aid the parental decision process on pregnancy continuation (three chose TOP based on pES diagnosis, six continued pregnancy after negative pES). Additionally, in two of five cases in which pES was performed in the context of late pregnancy termination, the pES result supported the request, which was important both for the parents and the involved clinicians. Finally, in two of the three cases in which pES was performed to guide intended pre- or perinatal management, a diagnosis was made. In the third case, although a secondary finding was detected, the absence of a genetic diagnosis by pES supported the intervention to perform fetal shunting. This shows an overall clinical impact of pES of 70% (14/20). Interestingly, although our eligibility criteria excluded cases with multiple congenital anomalies in which parents already made a decision based on the ultrasound anomalies alone, pES had a high diagnostic yield of 40%.
The high clinical impact is partially explained by our pES eligibility criteria, which we designed to maximize impact considering the costs of pES. For this manuscript we have defined clinical impact very narrowly as having a decisive influence on parental decision on TOP or pre- or perinatal management. However, pES can also have significant impact on the psychological wellbeing of parents. For example, in case 4, although parents expressed that they would probably have terminated the pregnancy given the poor prognosis based on the second ultrasound, they did spontaneously indicate on multiple occasions that their decision was helped by the genetic diagnosis. Indeed, the mother stated that she felt much calmer after having the diagnosis, which gave her comfort during the process. Other parents also indicated that having a genetic diagnosis took away doubts and worries of depriving a life of a potentially healthy child.
Implementation
Our experiences show that pES is logistically feasible. Sufficient fetal material was available in all cases but one, and a result was obtained within two weeks in nearly all cases. Our experiences identified some other issues that are relevant for the implementation of pES. Although gene panel analysis might be preferable to reduce the risk of secondary findings (genetic predisposition for a late-onset disorder in particular, as in our case 12), such a gene panel would have to be specifically designed for prenatal studies. This is illustrated by case 13, because the causal ECHS1 gene is absent from the DDG2P gene panel (www.ebi.ac.uk/gene2phenotype), as well as from the more extensive list curated by the PAGE study.24 Therefore, we currently prefer to perform a complete exome analysis. Secondly, we found that a clinical view remains important when performing ES. At present, exon deletions can remain undetected because current CNV tools on ES data do not detect single-exon deletions. This is one of the reasons the variant in ATAD3A in case 14 was initially missed and would not have been identified if clinical suggestion had not arisen. Thirdly, and relatively unexpectedly, we found that most genetic diagnoses were straightforward explanations for the detected anomalies. Only case 11 presented with considerable interpretation difficulties as described in the results. Although prospectively, we did not anticipate the postnatal findings, retrospectively, the SHH variant is potentially responsible for the phenotype. We reason that because SHH gives a phenotype in the midline, and postnatal physical examination of the child, in particular its oropharyngeal anatomy, raised the suspicion of agnathia–otocephaly, which may be accompanied by holoprosencephaly, one could speculate that this particular variant might be causal of the oropharyngeal anatomy, even though SHH variants have thus far never been described in such patients. Similar situations are often encountered in postnatal exome sequencing, and the question remains whether this finding broadens the SHH-associated phenotype, or whether another pathogenic variant was missed. The knowledge that this variant was de novo would not have helped the interpretation, given the reported incomplete penetrance of SHH variants.
We noted that many of the diagnoses had a recessive inheritance pattern (4/9, 44.4%). In contrast, previous work in the postnatal setting shows that 12% of diagnoses have a recessive inheritance pattern, whilst 78% are dominant de novo cases.28 Although our numbers are too low to draw definitive conclusions, Normand et al.22 (19/46, 41%), Lord et al.24 (14/52, 27%), and Petrovski et al.23 (6/24, 25%) also find an increased incidence of recessive disorders, suggesting that recessive diseases may on average result in more severe phenotypes, which may explain enrichment of recessive diagnoses in pES.
In the course of this study we identified two secondary findings, a homozygous VUS in UQCRC2 (case 20) and a heterozygous pathogenic PMS2 variant (case 12). Heterozygous variants in PMS2 are associated with Lynch syndrome (OMIM 614337), but have low penetrance.29 No colorectal cancer was present in the paternal family. One homozygous variant in UQCRC2 has been described in two families with a mitochondrial complex III deficiency (OMIM 615160). Affected individuals had severe neonatal metabolic acidosis. We discussed the variant with a genetic laboratory with extensive expertise in metabolic disease and they advised us not to report the variant in the absence of a metabolic phenotype. We reasoned, however, that we could not exclude the presence of a metabolic phenotype in this fetus. Because screening for metabolic acidosis would be straightforward after birth, we discussed the variants with the parents, indicating a low likelihood of pathogenicity and recommended screening directly after birth. This screening test was negative.
Given the costs and analysis burden of pES, our eligibility criteria were aimed at obtaining a high clinical impact. If parents decide to terminate a pregnancy based on the ultrasound findings alone, or conversely, if pregnancy termination is not considered at all, ES can be performed after birth, except when pre- or perinatal management is likely to be influenced by a genetic diagnosis. This is more cost-effective because many syndromic diagnoses can be made by dysmorphological examination as we have previously shown.30 The real added value of pES is expected when ultrasound findings are associated with an increased risk for a genetic syndrome, but the prognosis of the findings themselves is favorable. Because ES has a much higher sensitivity than CMA its negative predictive value (NPV) is higher, but unknown since the prior probability is not known in most prenatal scenarios. Although we do explain to couples that the absence of a detected causative variant by pES does not exclude the possibility of a genetic syndrome, it does seem that such a result gives couples more confidence in their decision to continue the pregnancy, as we have seen in 7 of 8 cases (Supplementary Material). To allow more detailed counseling of couples, large-scale studies should be performed where all pregnancies with congenital anomalies are included and follow-up is performed for several years to determine the precise NPV of pES per congenital anomaly.
Ethical considerations
There are important ethical issues concerning pES, such as the extent of parental rights to information from exome sequencing regarding the long-term health of their fetus or child.31 On the one hand, the fetus may be considered to have autonomy, and freedom of choice to know about late-onset diseases, whilst on the other hand such information could play a role in the parental decision process about the pregnancy. In our clinical experience, the chance of a secondary finding with clear consequences for later life is relatively low and we therefore feel that pES can be performed, also in absence of a widely accepted protocol on how to deal with such findings. Reducing the risk of secondary findings by limiting analysis to a prespecified gene panel is preferable, but not feasible at this stage given the lack of comprehensive large-scale studies to confidently design such panels.
We also noticed that parents have limited time to make an informed decision on pES, and therefore experience time pressure. In two cases, parents indicated they did not want reporting of secondary findings during pregnancy, and we have therefore offered them a consultation to discuss potential secondary findings after the pregnancy. We did feel that parents could take the decision in the allotted time frame, but care needs to be taken not to rush patients into a decision.
Conclusion
Our results demonstrate that pES has a high clinical impact and yields many undisputable diagnoses with limited VUS and therefore warrants wider implementation. Challenges of pES remain, such as the need for adequate genetic counseling for couples and the need for guidelines on reporting of variants of unknown clinical significance.32 This cohort is small, and we do therefore recommend that pES is performed in a study setting, to determine whether the benefits of pES continue to outweigh the potential disadvantages.
References
European Surveillance of Congenital Anomalies (EUROCAT), cases and prevalence (per 10. 000 births) for all full member registries from 2012 to 2016. Prevalence tables. http://www.eurocat-network.eu/AccessPrevalenceData/PrevalenceTables. Accessed 1 October 2018.
Osterman MJ, Kochanek KD, MacDorman MF, et al. Annual summary of vital statistics: 2012–3. Pediatrics. 2015;135:1115–1125.
Wapner RJ, Martin CL, Levy B, et al. Chromosomal microarray versus karyotyping for prenatal diagnosis. N Engl J Med. 2012;367:2175–2184.
Callaway JL, Shaffer LG, Chitty LS, et al. The clinical utility of microarray technologies applied to prenatal cytogenetics in the presence of a normal conventional karyotype: a review of the literature. Prenat Diagn. 2013;33:1119–1123.
Prevalence and architecture of de novo mutations in developmental disorders. Nature. 2017;542:433–438.
Richardson A, Ormond KE. Ethical considerations in prenatal testing: genomic testing and medical uncertainty. Semin Fetal Neonatal Med. 2018;23:1–6.
Wright CF, Fitzgerald TW, Jones WD, et al. Genetic diagnosis of developmental disorders in the DDD study: a scalable analysis of genome-wide research data. Lancet. 2015;385:1305–1314.
Aarabi M, Sniezek O, Jiang H, et al. Importance of complete phenotyping in prenatal whole exome sequencing. Hum Genet. 2018;137:175–181.
Boissel S, Fallet-Bianco C, Chitayat D, et al. Genomic study of severe fetal anomalies and discovery of GREB1L mutations in renal agenesis. Genet Med. 2018;20:745–753.
Carss KJ, Hillman SC, Parthiban V, et al. Exome sequencing improves genetic diagnosis of structural fetal abnormalities revealed by ultrasound. Hum Mol Genet. 2014;23:3269–3277.
Drury S, Williams H, Trump N, et al. Exome sequencing for prenatal diagnosis of fetuses with sonographic abnormalities. Prenat Diagn. 2015;35:1010–1017.
Fu F, Li R, Li Y, et al. Whole exome sequencing as a diagnostic adjunct to clinical testing in fetuses with structural abnormalities. Ultrasound Obstet Gynecol. 2018;51:493–502.
Westerfield LE, Stover SR, Mathur VS, et al. Reproductive genetic counseling challenges associated with diagnostic exome sequencing in a large academic private reproductive genetic counseling practice. Prenat Diagn. 2015;35:1022–1029.
Alamillo CL, Powis Z, Farwell K, et al. Exome sequencing positively identified relevant alterations in more than half of cases with an indication of prenatal ultrasound anomalies. Prenat Diagn. 2015;35:1073–1078.
Chandler N, Best S, Hayward J, et al. Rapid prenatal diagnosis using targeted exome sequencing: a cohort study to assess feasibility and potential impact on prenatal counseling and pregnancy management. Genet Med. 2018;20:1430–1437.
Lei TY, Fu F, Li R, et al. Whole-exome sequencing for prenatal diagnosis of fetuses with congenital anomalies of the kidney and urinary tract. Nephrol Dial Transplant. 2017;32:1665–1675.
Pangalos C, Hagnefelt B, Lilakos K, Konialis C. First applications of a targeted exome sequencing approach in fetuses with ultrasound abnormalities reveals an important fraction of cases with associated gene defects. PeerJ . 2016;4:e1955.
Rasmussen M, Sunde L, Nielsen ML, et al. Targeted gene sequencing and whole-exome sequencing in autopsied fetuses with prenatally diagnosed kidney anomalies. Clin Genet. 2018;93:860–869.
Vora NL, Powell B, Brandt A, et al. Prenatal exome sequencing in anomalous fetuses: new opportunities and challenges. Genet Med. 2017;19:1207–1216.
Yates CL, Monaghan KG, Copenheaver D, et al. Whole-exome sequencing on deceased fetuses with ultrasound anomalies: expanding our knowledge of genetic disease during fetal development. Genet Med. 2017;19:1171–1178.
Leung GKC, Mak CCY, Fung JLF, et al. Identifying the genetic causes for prenatally diagnosed structural congenital anomalies (SCAs) by whole-exome sequencing (WES). BMC Med Genomics. 2018;11:93–93.
Normand EA, Braxton A, Nassef S, et al. Clinical exome sequencing for fetuses with ultrasound abnormalities and a suspected Mendelian disorder. Genome Med. 2018;10:74–74.
Petrovski S, Aggarwal V, Giordano JL, et al. Whole-exome sequencing in the evaluation of fetal structural anomalies: a prospective cohort study. Lancet. 2019;393:758–767.
Lord J, McMullan DJ, Eberhardt RY, et al. Prenatal exome sequencing analysis in fetal structural anomalies detected by ultrasonography (PAGE): a cohort study. Lancet. 2019;393:747–757.
Richards S, Aziz N, Bale S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–424.
Roessler E, El-Jaick KB, Dubourg C, et al. The mutational spectrum of holoprosencephaly-associated changes within the SHH gene in humans predicts loss-of-function through either key structural alterations of the ligand or its altered synthesis. Hum Mutat. 2009;30:E921–E935.
CMPCD Peeters-Scholte, Adama van Scheltema PN, Klumper FJCM, et al. Genotype-phenotype correlation in ATAD3A deletions: not just of scientific relevance. Brain. 2017;140:e66–e66.
Wright CF, McRae JF, Clayton S, et al. Making new genetic diagnoses with old data: iterative reanalysis and reporting from genome-wide data in 1,133 families with developmental disorders. Genet Med. 2018;20:1216–1223.
Ten Broeke SW, van der Klift HM, Tops CMJ, et al. Cancer risks for PMS2-associated Lynch syndrome. J Clin Oncol. 2018;36:2961–2968.
van der Sluijs EPJ, Aten E, Barge-Schaapveld D, et al. Putting genome-wide sequencing in neonates into perspective. Genet Med. 2018 Oct 5; doi:10.1038/s41436-018-0293-0 [Epub ahead of print].
Horn R, Parker M. Opening Pandora’s box?: ethical issues in prenatal whole genome and exome sequencing. Prenat Diagn. 2018;38:20–25.
Best S, Wou K, Vora N, et al. Promises, pitfalls and practicalities of prenatal whole exome sequencing. Prenat Diagn. 2018;38:10–19.
Acknowledgements
We received no funding. We would like to thank all medical staff who contributed to clinical care of the patients.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare no conflicts of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
de Koning, M.A., Haak, M.C., Adama van Scheltema, P.N. et al. From diagnostic yield to clinical impact: a pilot study on the implementation of prenatal exome sequencing in routine care. Genet Med 21, 2303–2310 (2019). https://doi.org/10.1038/s41436-019-0499-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-019-0499-9
Keywords
This article is cited by
-
Application of exome sequencing for prenatal diagnosis of fetal structural anomalies: clinical experience and lessons learned from a cohort of 1618 fetuses
Genome Medicine (2022)
-
Genetic diagnosis in the fetus
Journal of Perinatology (2020)