Abstract
Purpose
The identification of carriers of hereditary breast and ovarian cancer (HBOC) gene variants through family cancer history alone is suboptimal, and most population-based genetic testing studies have been limited to founder mutations in high-risk populations. Here, we determine the clinical utility of identifying actionable variants in a healthy cohort of women.
Methods
Germline DNA from a subset of healthy Australian women participating in the lifepool project was screened using an 11-gene custom sequencing panel. Women with clinically actionable results were invited to attend a familial cancer clinic (FCC) for post-test genetic counseling and confirmatory testing. Outcomes measured included the prevalence of pathogenic variants, and the uptake rate of genetic counseling, risk reduction surgery, and cascade testing.
Results
Thirty-eight of 5908 women (0.64%) carried a clinically actionable pathogenic variant. Forty-two percent of pathogenic variant carriers did not have a first-degree relative with breast or ovarian cancer and 89% pursued referral to an FCC. Forty-six percent (6/13) of eligible women pursued risk reduction surgery, and the uptake rate of cascade testing averaged 3.3 family members per index case.
Conclusion
Within our cohort, HBOC genetic testing was well accepted, and the majority of high-risk gene carriers identified would not meet eligibility criteria for genetic testing based on their existing family history.
Similar content being viewed by others
Introduction
The goal of testing for constitutional high-risk pathogenic variants (PV) in hereditary breast and ovarian cancer (HBOC) predisposition genes such as BRCA1 and BRCA2 is to (1) provide predictive information to women diagnosed with a HBOC gene–related tumor, and (2) identify unaffected relatives with PVs to target risk reduction or management strategies. Germline PVs in HBOC genes indicate a high individual lifetime breast and ovarian cancer risk, even in the absence of a family history1,2 and account for an important component of the inherited risk of breast and ovarian cancer. Identifying unaffected PV carriers and managing their risk has been shown to reduce breast and ovarian cancer and all-cause mortality.3
Testing for a PV in a HBOC gene typically occurs in response to a personal or family cancer history. In many health-care systems, women are initially referred to a familial cancer clinic (FCC) for assessment, and germline testing is offered based on having a personal history of breast and/or ovarian cancer, and a significant prior probability of harboring a BRCA1 or BRCA2 PV (commonly ≥10%) assessed by internationally validated algorithms such as BOADICEA.4,5,6 This approach is suboptimal as current evidence indicates that both high-risk family history is not recognized and assessed,7 and 50% of women with cancer who harbor a BRCA1 or BRCA2 PV report no significant cancer family history.8,9
With the significant recent cost reductions associated with multigene panel testing, it has been proposed that population-based genetic testing may provide a more clinically effective and cost-effective strategy for identification of individuals with a high genetic breast and ovarian cancer risk.10,11 Assessing this proposal against emerging principles guiding population screening for genetic susceptibility to common disease12 highlights the areas that require further evaluation prior to implementation, in particular (1) the frequency of actionable PVs and the acceptability of screening in the target population, (2) the framework and safeguards by which population-based genetic testing is offered, (3) the negative predictive value of a test and the clinical response to the identification of variants of uncertain clinical significance (VUS), and (4) the cost-effectiveness of this approach compared with standard practice.
Studies in population-based genetic testing for HBOC genes to date have been restricted to specific founder mutation in BRCA1 and BRCA2 genes in high-risk populations, namely the Ashkenazi Jewish or Polish populations.9,13,14,15,16 In these populations, the prevalence of founder mutations ranges from 1.1% to 4.5% and the issue of VUS is avoided. These studies addressed the acceptability and cost-effectiveness of population screening through a self-referral process demonstrating that population founder HBOC gene testing at age 30 years in the Ashkenazi population was highly cost-effective compared with current clinical practice9 and that this form of testing did not increase anxiety or psychological distress.17 Compared with a family history–based approach, Manchanda et al. estimated that a population-screening approach saved more life-years and quality-adjusted life-years and had the potential to lower the incidence of breast and ovarian cancer incidence in the Ashkenazi population.9 In more genetically diverse populations, the lower PV carrier frequency (approximately 0.22–0.37%)18,19,20 and wide spectrum of private PVs in BRCA1 and BRCA2, including the possibility of VUS, adds further complexity to the interpretation of results, and has potential to significantly impact on the cost-effectiveness of the model. Applying a decision-analytic model using a hypothetical non-Jewish population, Manchanda et al.11 estimated that a 7-gene HBOC gene panel test implemented at the population level was more cost-effective than a family history–based approach.
Here, we describe a population-based genetic testing study of germline PVs in 11 HBOC genes from 5908 cancer-free unselected women recruited into the lifepool cohort study (www.lifepool.org) primarily via attendance at a government-funded population breast surveillance program (BreastScreen Victoria). Women with pathogenic, clinically actionable PVs were notified that potentially important health information was available with the offer of FCC referral. The key aims of the study were to assess the frequency of actionable PVs in HBOC genes in a genetically diverse Western population, evaluate the acceptability of population germline testing through the uptake rate of FCC referral and cascade testing within families, and to determine the proportion of women with high-risk PVs who would not otherwise have presented to an FCC. This represents the most comprehensive, unselected, population-based approach to HBOC genetic testing to date.
Materials and methods
Sample cohort
Women were recruited into the lifepool study from 2012 to 2017 primarily via attendance at BreastScreen Victoria, the government-funded population-based mammographic screening program in the state of Victoria, Australia. BreastScreen Victoria actively invites all women aged 50–74 years for two-yearly breast mammograms; although screening is open to all self-referred women over the age of 40. The most recent statistics report a state-wide participation rate of 53.6% of women aged 50–74 (ref.21). Participating women are invited to join the lifepool study at or after their second mammographic screen, and currently over 53,500 women have been recruited, 48,700 of which were cancer-free at enrollment (90.8%). Twenty-five percent of women who were offered participation consented to recruitment. A small number of women over 18 years of age (<5% of entire cohort) contacted lifepool in response to the study publicity and were also recruited, regardless of age or mammographic screening status.
A random subset of lifepool participants was invited to donate a germline DNA sample for use in genetic research into breast cancer risk and development. Participants were informed that the research study would be studying genes that could be involved in development of breast cancer and genes that may have an effect on the risk of breast cancer, that there was a very small chance that information directly relevant to their health may be found, and that they would be contacted should this occur. No pretest genetic counseling was provided. Approximately 50% of invited participants donated a DNA sample. All women were cancer-free at DNA collection and completed an epidemiology and family cancer history questionnaire. In total, 5908 women with an average age of 59.2 ± 8.7 (SD) years provided a DNA sample from blood (90.9%) or saliva (9.1%). Ninety-four percent were of Caucasian background as confirmed by principal component analysis.22 All participants provided informed consent and the Peter MacCallum Cancer Centre Human Research Ethics Committee approved the study. A summary of HBOC gene PV frequency in 1997 of these women has been previously published.23
Sequencing and variant calling
Germline DNA was sequenced for all exons and intron boundaries of 11 HBOC genes (Table 1) using a custom HaloPlex Targeted Enrichment Assay (Agilent Technologies) and sequenced as previously described.23,24 Detailed methods are available in Supplementary Materials and Methods.
The variant calling pipeline has been described previously.25 The data were filtered to identify loss of function (LoF) PVs (defined as nonsense or frameshift PVs), or essential splice site and missense PVs that were classified as unequivocally pathogenic in ClinVar.26 All pathogenic variants were validated by Sanger sequencing. A custom algorithm, designed to detect large germline copy-number changes from amplicon-based sequencing data, was used to identify large genomic rearrangements (LGRs) in BRCA1 and BRCA2. LGRs with high confidence calls were validated by multiplex ligation-dependent probe amplification (MLPA).
Feedback of results to participants
The pathogenicity of validated variants was confirmed by a molecular geneticist in a National Association of Testing Authorities (NATA) accredited molecular diagnostic laboratory according to American College of Medical Genetics and Genomics (ACMG) guidelines (class 4 and class 5) (ref.27), and clinical actionability was assessed by clinical geneticists in an FCC according to current national clinical guidelines.28 PVs in ovarian cancer risk genes BRIP1, RAD51C, and RAD51D, and LoF PVs in ATM are currently not deemed actionable according to national management guidelines and therefore these results were not returned to participants. For ATM, only the nonsynonymous variant c.7271T>G (rs28904921, p.Val2424Gly) was defined as high risk and actionable in the Australian context.29
Participants harboring a validated, clinically actionable germline PV were notified by letter of a potentially significant finding and invited to contact the standard Parkville FCC telephone genetic counseling service for further discussion (File S1).30 If no response was received after 2 weeks, the participant was followed up by telephone call. On FCC referral, participants received standard clinical care by specialists through the FCC clinical framework, which included confirmation of the PV in an independent blood sample in a nationally accredited molecular diagnostic laboratory, collection of family history data validated through the local cancer registry, calculation of BRCA1/BRCA2 PV carrier probabilities using the current version of BOADICEA based on a verified family cancer history, and rates of predictive testing in relatives and uptake of risk management strategies.
Results
Cohort characteristics
The 5908 participants who provided a DNA sample were significantly younger than the 42,792 who did not (59.2 years ± 8.7 (SD) vs. 60.2 years ± 7.1 (SD), p < 0.0001, t test). They also self-reported higher rates of having at least one first-degree relative diagnosed with breast or ovarian cancer (21.3% vs. 19.7%, p = 0.0039, Fisher’s exact test [FET]), and a higher FCC attendance rate prior to enrollment in lifepool (1.10% vs. 0.62%, p < 0.0001, FET). A small number of participants (42/5908, 0.71%) were under 40 years of age at DNA collection.
Pathogenic Variant prevalence
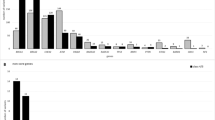
Of the 5908 women screened, 38 (0.64%) were identified with actionable PVs in 4 of the 11 HBOC genes; the majority (72%) within BRCA2 and PALB2 as anticipated with the age of the cohort (Table 1). Six women harbored a BRCA1 PV, and three women the ATM c.7271T>G PV. No PVs were identified in CDH1, PTEN, STK11, or TP53. An additional 29 participants carried PVs in BRIP1, RAD51C, RAD51D, or LoF PVs in ATM but have not been contacted for return of these results at this time (Table 1; Table S1).
Patient characteristics
The 38 women with actionable PVs ranged in age from 24 to 77 years at DNA collection, with an average age of 57 years (Table 2). Only 2 of the 38 PV carriers (LP-08 and LP-09) had a BOADICEA-assessed BRCA PV probability of >20% that, in the cancer-unaffected setting, may have qualified them for publicly funded genetic testing. A third Ashkenazim woman with a BRCA2 PV (LP-20) would also have qualified based on her ethnicity and family history (Table 2; Table 3). Twenty-two of the 38 PV carriers (58%) self-reported a first-degree relative with breast or ovarian cancer, or DCIS, and 6 had an affected second-degree relative only (Table 3).
Four women (11% of all PV carriers) had been referred to an FCC prior to DNA collection due to family history but only one (LP-04) had been offered predictive testing because a PV had been identified in her mother, who developed ovarian cancer at 42 years of age. The PV status of LP-04 was not disclosed to the study at the time of recruitment. An additional three participants were in the process of HBOC gene testing (due to the detection of a PV in an affected relative) contemporaneously with the notification from lifepool of a potentially significant genetic finding (Table 2).
In the interval between DNA collection and receiving the notification letter from lifepool, four of the PV positive women were diagnosed with cancer (Table 2). One woman (LP-08) developed ovarian cancer aged 56, and a BRCA1 PV was identified as part of her treatment-focused testing. None of the other three women were referred to the FCC for genetic testing as part of clinical care.
Acceptability of return of results
Thirty-five of the 38 women (92%) who received a notification letter contacted the telephone genetic counseling service a median of 7 days after receipt (range of 1–49 days) (Table 2). Thirty-four of the 35 who contacted the service (89% of total) accepted referral to their local FCC and 33 (87%) underwent confirmatory genetic testing and standard clinical care and follow up. The participants who did not follow through with a counseling appointment or genetic testing (LP-01 and LP-31) cited reasons of old age and a recent cancer diagnosis, respectively.
Uptake of risk reduction strategies and cascade testing
Of the 16 women over 40 years of age with a BRCA1- or BRCA2-related high risk of ovarian cancer who were cancer-free, attended the FCC, and were unaware of their PV status at recruitment, surgical risk management information is available for 13 individuals. Of these 13, 6 (index cases) (46%) and one PV-positive relative underwent bilateral risk-reducing salpingo-oophorectomy as a result of their BRCA PV being identified by the study (Table 3). No pathological abnormalities were detected. Two woman declined surgery due to old age, and currently no woman has chosen bilateral risk-reducing mastectomy.
Family members of 19 of the identified index cases have requested cascade genetic testing, with 63 relatives attending the FCC for predictive testing (3.3 relatives per index case), of which 32 (51%) tested positive (Table 3). Despite the shorter time during which these families have known their PV status, this cascade testing rate compares favorably with our current local uptake of 3.1 relatives per index case.
Discussion
Enthusiasm among health-care providers for the implementation of population-based HBOC gene testing is growing in tandem with increasing community knowledge of HBOC testing, particularly through key celebrity informants.31 Future implementation of this model requires evidence of its social and clinical implications as well as the development of a cost-effective, equitable framework to inform policy decisions. It has been suggested that BRCA1/2 genetic testing should be offered to all women living in the United States at age 30 before PV carriers are likely to develop cancer.32 While favorable health and economic dividends of population genetic testing of HBOC genes has only been established in studies of founder populations where the frequency of PVs is high (~3% in Ashkenazi Jewish populations), the rapidly reducing costs of gene panel testing should ensure that even at a 0.5–1% carrier frequency, population genetic testing should be cost-effective relative to a family history–based approach.11 The economic benefits of population genetic testing will only be realized if women engage with risk mitigation strategies in the absence of a strong cancer family history. Furthermore, because the known HBOC genes account for less than half of the high-risk breast and ovarian cancer families, the proportion of the population with actionable PVs has capacity to increase at little incremental cost as new HBOC genes are discovered and elevated to a clinically actionable level.33 Indeed, the US and European guideline recommendations include considering RRSO for women aged 45–50 years who harbor RAD51C, RAD51D, or BRIP1 pathogenic PVs.34,35
This study, focused on a conservative panel of high-risk genes, provides real-life data from the most comprehensive, pragmatic model of HBOC testing of a predominantly western European population to date. The results indicate the prevalence of high-risk PVs in cancer-free Australian women is 0.64% and may be in excess of 1%, when a future evidenced-based framework for the integration of moderate-risk gene PVs into clinical care is established.33 As the lifepool cohort is only a surrogate for the general cancer-free population, this frequency will not precisely reflect the population. Firstly, as participants were in the large majority recruited through a population-screening program, the median age was above the expected breast cancer diagnosis age for BRCA1 and BRCA2 carriers (59.2 years versus 44 and 48 years of age, respectively).2 This resulted in three women with PVs developing cancers that were potentially avoidable, had genetic testing been offered at a younger age. It is anticipated that a higher PV frequency would be achieved if unaffected women were offered testing at a younger age (20–30 years), as the proportion of PV-positive unaffected women reduces with age.36 Secondly, not unexpectedly, women with a family history may have a greater incentive to take part in such a study as demonstrated by the finding that four women with PVs had already been assessed by a FCC and three women had been offered predictive testing concomitant with the study results. Indeed, the cohort of cancer-free women who agreed to donate their DNA was significantly younger and had more first-degree relatives affected by breast and/or ovarian cancer than those who did not donate. Two women under the age of 40 were identified as PV carriers. These two women were part of the <5% of the cohort that was recruited by women already in lifepool, or due to study publicity.
Lifepool participants are a highly motivated population who consented to participate in a research study, and were informed that there was a small chance of being contacted if any genetic findings were detected that may impact their health. This recruitment method differs from true genetic population testing in that the participants did not directly consent to HBOC gene testing. The response rate of direct HBOC population genetic testing may differ.
Only 3 of the 38 PV carriers (7.9%) may have been considered for clinical testing under local testing criteria for cancer-free individuals, as 2 had a BOADICEA score >20% and 1 was of Ashkenazi Jewish heritage. If the BOADICEA score threshold was lowered to >10%, as is recommended in UK and US guidelines,34,37 no additional PV carriers would have been eligible for clinical testing. There is insufficient pedigree data from the carrier families to determine if the absence of family history reflects a genuine lower penetrance of HBOC gene PV pathogenic variant identified in this context or is simply due to a family structure that is not conducive for accurate family history assessment.
For the first time, our study directly confirms in a cancer-free non-Jewish cohort that the large majority of high-risk HBOC gene carriers would not meet eligibility criteria for genetic testing based on their existing family history. In addition, by integrating this study directly with standard FCC clinical care, we can demonstrate that within these families of both BRCA1/2 PV carriers and PALB2 PV carriers, predictive testing occurs at the same rate as seen in families in whom the PV is identified in cancer-affected individuals with strong family histories. Through predictive testing within families, the number of women benefiting from the original test doubled while the average age was significantly younger than the index women.
Notification of a PV-positive status in the absence of a family history of cancer represents a novel challenge for this model of care. All women with actionable PV pathogenic variant were sent a notification letter together with an invitation to contact a FCC telephone genetic counseling service for further information about the research findings, and support. The large majority of participants utilized this service within a median of 7 days from receiving the notification letter. The inclusion of telephone genetic counseling facilitated participants’ understanding of their family-specific genetic information, provided emotional support, and enabled them to be connected with their preferred clinical service. Overall, the response has been very positive for this approach. All except two of the participants who contacted the telephone genetic service proceeded to formal clinical genetic testing and confirmation of their PV status, and the two women who did not proceed themselves did inform other family members. While this study did not address issues including the psychological impact of genetic testing, satisfaction with the notification process, or data on quality of life, these are important areas that will need to be addressed in future studies.
Based on the short response time and high uptake of referral to an FCC, this study provides reassurance of the acceptability of population genetic testing when linked to specialist familial cancer services. This is not unexpected because FCCs are increasingly contacted by women requesting and self-funding genetic testing, even in the context of a low familial risk.31 Easily accessible and affordable clinical guidance on how to interpret and contextualize the information is required to reduce adverse outcomes and unrealistic expectations.30
An important concern regarding population-based testing is how to deal with VUS.38 In this study, in keeping with suggested policy,32 only actionable, PV in high-risk HBOC genes were returned, and no negative test results or VUS were reported back to patients. The clinical utility of a negative test result was therefore not addressed, but it is anticipated that this will be lower in the population setting than in the familial cancer setting.
In conclusion, this study provides the most comprehensive data on population-based HBOC screening in cancer-free women of western European descent where actionable results are communicated back to the participants through the standard clinical care pathway. Our preliminary data provide reassurance of the clinical benefit of population-based genetic testing even in women without a strong family history, although conclusive evidence for surgical prevention rates being similar to those with strong family history requires further research confirmation. We demonstrate a relatively high prevalence of HBOC gene PV pathogenic variant compared with previous estimates, and that most of these PV carriers (92%) would not have been diagnosed through the current clinical HBOC referral pathways. Our study shows that population-based genetic testing is well accepted, despite the absence of any personal or family history of cancer.
References
Metcalfe KA, Lubinski J, Gronwald J, et al. The risk of breast cancer in BRCA1 and BRCA2 mutation carriers without a first-degree relative with breast cancer. Clin Genet. 2018;93:1063–1068.
Kuchenbaecker KB, Hopper JL, Barnes DR, et al. Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA. 2017;317:2402–2416.
Domchek SM, Friebel TM, Singer CF, et al. Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA. 2010;304:967–975.
Antoniou AC, Hardy R, Walker L, et al. Predicting the likelihood of carrying a BRCA1 or BRCA2 mutation: validation of BOADICEA, BRCAPRO, IBIS, Myriad and the Manchester scoring system using data from UK genetics clinics. J Med Genet. 2008;45:425–431.
Antoniou AC, Cunningham AP, Peto J, et al. The BOADICEA model of genetic susceptibility to breast and ovarian cancers: updates and extensions. Br J Cancer. 2008;98:1457–1466.
Antoniou AC, Pharoah PP, Smith P, Easton DF. The BOADICEA model of genetic susceptibility to breast and ovarian cancer. Br J Cancer. 2004;91:1580–1590.
Kurian AW, Griffith KA, Hamilton AS, et al. Genetic testing and counseling among patients with newly diagnosed breast cancer. JAMA. 2017;317:531–534.
Alsop K, Fereday S, Meldrum C, et al. BRCA mutation frequency and patterns of treatment response in BRCA mutation-positive women with ovarian cancer: a report from the Australian Ovarian Cancer Study Group. J Clin Oncol. 2012;30:2654–2663.
Manchanda R, Legood R, Burnell M, et al. Cost-effectiveness of population screening for BRCA mutations in Ashkenazi Jewish women compared with family history-based testing. J Natl Cancer Inst. 2015;107:380.
Foulkes WD, Knoppers BM, Turnbull C. Population genetic testing for cancer susceptibility: founder mutations to genomes. Nat Rev Clin Oncol. 2016;13:41–54.
Manchanda R, Patel S, Gordeev VS. et al. Cost-effectiveness of population-Based BRCA1, BRCA2, RAD51C, RAD51D, BRIP1, PALB2 mutation testing in unselected general population women. J Natl Cancer Inst. 2018;110:714–725.
Khoury MJ, McCabe LL, McCabe ER. Population screening in the age of genomic medicine. N Engl J Med. 2003;348:50–58.
Richards CS, Ward PA, Roa BB, et al. Screening for 185delAG in the Ashkenazim. Am J Hum Genet. 1997;60:1085–1098.
Struewing JP, Hartge P, Wacholder S, et al. The risk of cancer associated with specific mutations of BRCA1 and BRCA2 among Ashkenazi Jews. N Engl J Med. 1997;336:1401–1408.
Gabai-Kapara E, Lahad A, Kaufman B, et al. Population-based screening for breast and ovarian cancer risk due to BRCA1 and BRCA2. Proc Natl Acad Sci USA 2014;111:14205–14210.
Gronwald J, Huzarski T, Byrski T, et al. Direct-to-patient BRCA1 testing: the Twoj Styl experience. Breast Cancer Res Treat. 2006;100:239–245.
Manchanda R, Loggenberg K, Sanderson S, et al. Population testing for cancer predisposing BRCA1/BRCA2 mutations in the Ashkenazi-Jewish community: a randomized controlled trial. J Natl Cancer Inst. 2015;107:379.
McClain MR, Palomaki GE, Nathanson KL, Haddow JE. Adjusting the estimated proportion of breast cancer cases associated with BRCA1 and BRCA2 mutations: public health implications. Genet Med. 2005;7:28–33.
Song H, Cicek MS, Dicks E, et al. The contribution of deleterious germline mutations in BRCA1, BRCA2 and the mismatch repair genes to ovarian cancer in the population. Hum Mol Genet. 2014;23:4703–4709.
Jervis S, Song H, Lee A, et al. A risk prediction algorithm for ovarian cancer incorporating BRCA1, BRCA2, common alleles and other familial effects. J Med Genet. 2015;52:465–475.
BreastScreen Victoria. Annual report 2016–2017. Melbourne, Australia: BreastScreen Victoria; 2017.
Li N, Thompson ER, Rowley SM, et al. Reevaluation of RINT1 as a breast cancer predisposition gene. Breast Cancer Res Treat. 2016;159:385–392.
Thompson ER, Rowley SM, Li N, et al. Panel testing for familial breast cancer: calibrating the tension between research and clinical care. J Clin Oncol. 2016;34:1455–1459.
Thompson ER, Gorringe KL, Rowley SM, et al. Prevalence of PALB2 mutations in Australian familial breast cancer cases and controls. Breast Cancer Res. 2015;17:111.
Li N, Rowley SM, Goode DL, et al. Mutations in RECQL are not associated with breast cancer risk in an Australian population. Nature Genetics. Published Online September 17, 2018. https://doi.org/10.1038/s41588-018-0206-9.
Landrum MJ, Lee JM, Riley GR, et al. ClinVar: public archive of relationships among sequence variation and human phenotype. Nucleic Acids Res. 2014;42:D980–985.
Richards S, Aziz N, Bale S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–424.
EviQ. eviQ cancer treatments online. https://www.eviq.org.au/cancer-genetics. Accessed 2018.
Goldgar DE, Healey S, Dowty JG, et al. Rare variants in the ATM gene and risk of breast cancer. Breast Cancer Res. 2011;13:R73.
Forrest LE, Young M-A. Clinically significant germline mutations in cancer-causing genes identified through research studies should be offered to research participants by genetic counselors. J Clin Oncol. 2016;34:898–901.
James PA, Mitchell G, Bogwitz M, et al. The Angelina Jolie effect. Med J Aust. 2013;199:646.
King M-C, Levy-Lahad E, Lahad A. Population-based screening for BRCA1 and BRCA2: 2014 Lasker Award. JAMA. 2014;312:1091–1092.
Muranen TA, Greco D, Blomqvist C, et al. Genetic modifiers of CHEK2*1100delC-associated breast cancer risk. Genet Med. 2017;19:599–603.
National Comprehensive Cancer Network. Clinical practice guidelines in oncology: genetic/familial high-risk assessment: breast and ovarian. 2017. Version 1.2018. https://www.nccn.org/professionals/physician_gls/pdf/genetics_screening.pdf. Accessed 30 April 2018.
Paluch-Shimon S, Cardoso F, Sessa C, et al. Prevention and screening in BRCA mutation carriers and other breast/ovarian hereditary cancer syndromes: ESMO clinical practice guidelines for cancer prevention and screening. Ann Oncol. 2016;27 Suppl 5 :v103–v110.
Evans DG, Woodward E, Harkness EF, et al. Penetrance estimates for BRCA1, BRCA2 (also applied to Lynch syndrome) based on presymptomatic testing: a new unbiased method to assess risk? J Med Genet. 2018;55:442–448.
National Institute for Health and Care Excellence. Familial breast cancer: classification, care and managing breast cancer and related risks in people with a family history of breast cancer. Clinical guideline CG164. 2013. https://www.nice.org.uk/guidance/cg164. Accessed 30 April 2018.
Yurgelun MB, Hiller E, Garber JE. Population-wide screening for germline BRCA1 and BRCA2 mutations: too much of a good thing? J Clin Oncol. 2015;33:3092–3095.
Acknowledgements
The authors would like to thank S. Hughes, R. Huynh, and H. Saunders for processing DNA samples, and R. Lupat and J. Li for bioinformatics analysis. This work was supported by the National Breast Cancer Foundation (IF-15-004, I.G.C., P.A.J., L.D.); Cancer Australia (APP1107870); the National Health and Medical Research Council of Australia (APP1126679, I.G.C., A.H.T., M-A.Y., P.J.; APP1092856, I.G.C., P.A.J.); and the Victorian Cancer Agency (P.A.J.). The funders had no role in the design and execution of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare no conflicts of interest.
Additional information
Joint Senior Authors: Paul A. James, Alison H. Trainer, and Ian G. Campbell.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Rowley, S.M., Mascarenhas, L., Devereux, L. et al. Population-based genetic testing of asymptomatic women for breast and ovarian cancer susceptibility. Genet Med 21, 913–922 (2019). https://doi.org/10.1038/s41436-018-0277-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-018-0277-0
Keywords
This article is cited by
-
My Research Results: a program to facilitate return of clinically actionable genomic research findings
European Journal of Human Genetics (2022)
-
Do current family history-based genetic testing guidelines contribute to breast cancer health inequities?
npj Breast Cancer (2022)
-
Interest in genetic testing and risk-reducing behavioral changes: results from a community health assessment in New York City
Journal of Community Genetics (2022)
-
Genotype-first approach to the detection of hereditary breast and ovarian cancer risk, and effects of risk disclosure to biobank participants
European Journal of Human Genetics (2021)
-
A functionally impaired missense variant identified in French Canadian families implicates FANCI as a candidate ovarian cancer-predisposing gene
Genome Medicine (2021)