Abstract
Background/Aims
This study examines the anecdotal impression that in diabetes eye screening there is a relationship between number of consecutive missed screening appointments and the incidence of referable retinopathy at the next screening appointment that is attended.
Methods
A retrospective observational audit was conducted of data from 62,067 people who were due for annual diabetes eye screening in the North East London Diabetes Eye Screening Programme between January 2010 and January 2017, and who had missed at least one screening appointment within that time.
Results
Missing 5 consecutive screening appointments increased the incidence of referable retinopathy from a programme average of 4% up to 15%. The incidence of referable retinopathy in people missing 10 or more consecutive appointments was ~20%. There was an association between younger age, male gender, type I disease, and being of African ethnicity with increasing number of missed appointments.
Conclusions
There was a strong association between the number of missed appointments and the proportion of patients showing referable retinopathy at the next visit. Approaches to reduce the number of missed appointments may help to reduce the incidence of referable retinopathy. These may be targeted at those showing the greatest non-attendance behaviour in the current study.
Similar content being viewed by others
Introduction
According to the World Health Organization, the prevalence of diabetes is rising; in 1980, there were 108 million known cases and in 2014, 422 million [1]. Diabetic eye disease is one of the leading causes of blindness among working age adults in England and Wales [2], and diabetic retinopathy (DR) is responsible for about 3.5% of cases of sight loss in the UK [3]. Longer diabetes duration, poor glycaemic and blood pressure control and elevated blood lipid levels are strongly associated with DR onset and progression [4].
The UK National Institute of Clinical Excellence (NICE) recommends that diabetic patients aged 12 years old and above, should have their eyes screened at the time of diagnosis and at least annually thereafter for signs of referable retinopathy [5, 6]. Management with panretinal laser photocoagulation (for neovascular changes) [7], and laser [8], steroid [9] or anti-VEGF therapy (for diabetic macular oedema) [10], has been shown to provide better outcomes if implemented earlier, so early detection of treatable retinopathy is vital. Furthermore, detection of progression of retinopathy, even before a referable stage, may allow the opportunity for healthcare providers to advise on management of blood sugar, lipids, hypertension and other modifiable risk factors for retinopathy progression [11].
There are data to suggest that patients who do not attend for diabetes eye screening have poorer HbA1c and blood pressure control and have been diagnosed with diabetes for longer [12], all of which are factors for increased risk of diabetic eye disease [11, 13]. Anecdotally, there is a perception that poor attendance is associated with a greater risk of adverse outcome. There has only been one prior study relating number of consecutive nonattendances in a UK diabetic retinopathy screening service to risk of referable retinopathy [14]. They reported that missing screening for just 2 years among participants who had mild retinopathy at their first screen was associated with increased likelihood of having referable retinopathy or maculopathy when they next attended.
The aim of the current study was to evaluate a large dataset from a multi-ethnic, relatively deprived cohort in North-East London to determine (1) the correlation (if any) between the number of consecutive missed screening appointments and the rate of referable retinopathy and, (2) to examine the characteristics of those at greater risk of nonattendance.
Materials and methods
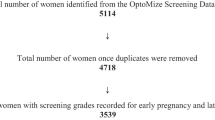
Homerton University hospital provides the Diabetes Eye Screening Service for north-east London. Data on people with diabetes screened for diabetic retinopathy in the North East London Diabetes Eye Screening Programme are stored in a database which is compliant with national standards and which is used to manage all aspects of diabetic eye screening (Optomize, EMIS Health, Cambridge, UK). A retrospective audit was undertaken of data obtained from the eye screening software over a 7-year period from January 2010 to January 2017. NHS Research Ethical approval was not required for this clinical audit. The audit was registered (No. 2166-2545) by the Homerton University Hospital Quality and Risk Department and approved by the Caldicott Guardian. Approval was also obtained from the City University School of Health Sciences Research Ethics Committee. All data were fully anonymised and no patient identifiable data were made available to anyone outside the clinical care team.
To be eligible for inclusion, patients were already registered with diabetes in primary care in 2010, were due for annual screening within the 2010–2017 timeframe, and failed to attend for at least one appointment. Data for screened patients were extracted from the Optomize software database as part of an internal audit process using semi-automated data collection algorithms (Structured Query Language, SQL, codes) supplemented by validation processes. The audit extracted information regarding the number of consecutive nonattendances for each patient from the timepoint of their first nonattendance until attendance or the end of the audit period. If there were multiple strings of missed appointments, data relating to the first series of nonattendances within the timeframe were analysed. Additional data extracted included; age, gender, type of diabetes, self-declared ethnicity and outcome of the first attended appointment after the first series of nonattendances. Referable patients included those who had signs of pre-proliferative or proliferative diabetic retinopathy and those with diabetic maculopathy (R2, R3a or M1, according to the diabetic eye screening programme grading system) [15]. Non-referable patients were those with no diabetic retinopathy or maculopathy or with only background retinopathy (R0M0 or R1M0). Patients who had unclear images were recalled into a slit lamp examination clinic and their final grading outcome was determined by the examining optometrist.
Data analysis
All data analysis was conducted in SPSS (version 10, IBM analytics). The raw data were coded and categorised by ethnicity, gender, referable/non-referable, age group, type of diabetes and by number of consecutive nonattendances. Ethnicity was determined by the self-declared response of patients, who selected from 17 categories, according to the ethnicity classification system recommended by the Office for National Statistics [16].
The distribution of continuous data was assessed for normality using the Kolmogorov–Smirnov test. A Pearson’s correlation coefficient was calculated to assess the relationship between age and the number of consecutive missed appointments. The Mann–Whitney U test was used to determine if there was a significant difference in number of consecutive missed appointments between those with a diagnosis of referable and non-referable retinopathy at the next visit, between type I and type II diabetes, and between genders, and the Kruskal–Wallis test was conducted to determine if there was a significant difference in nonattendance between age groups and between ethnic groups. The Chi-Square (χ2) test was used for comparison of proportions.
Results
During the study period, 62,067 patients failed to attend at least one occasion, and thus were eligible for inclusion. Of this cohort, 6078 patients (9.8%) were diagnosed with referable retinopathy at their first visit after the string of nonattendances. The distribution of age of the cohort was not normally distributed (Kolmogorov–Smirnoff test, p = 0.027), with the histogram showing a peak frequency at the age of around 56–60 years, with a second peak at around 70 years (see Fig. 1). The median age of the cohort (at their first visit after their nonattendance) was 57 years (47–68 IQR), 54.5% were male and 45.5% were female. 3106 patients (5.0%) were diagnosed with type I diabetes (median age 34 years, 25–47 IQR), whilst 57497 (92.6%) were diagnosed with type II diabetes (median age 58 years, 48–69 IQR). The age of the individuals with type II diabetes was significantly higher than that of those with type I disease (Mann–Whitney U test, U = 28011869.0, p < 0.001). The remaining individuals were either diagnosed with Maturity Onset Diabetes of the Young (MODY, n = 49, 0.08%), or the type of diabetes was not specified.
The range of consecutive nonattendances varied from 1–34 (median 1, 1–2 IQR). The consecutive nonattendance data were non-normally distributed, being heavily skewed towards the lower numbers (see Fig. 2, solid line).
In Fig. 2, the dotted line represents the proportion of participants with referable retinopathy at the next attended screening appointment as a function of the number of consecutive missed appointments. It is clear from this visual representation that the proportion of patients with referable retinopathy increased as the number of missed screening appointments increased. Missing 5 consecutive screening appointments increased the risk of referable retinopathy being found at the next appointment from a programme average of 4% up to ~15%. Missing 10 or more consecutive appointments was associated with a risk of ~20%. Accordingly, the average length of the string of missed appointments in people with referable retinopathy at the next visit (Median 2, 1–3 IQR) was significantly higher than in those with non-referable retinopathy (Median 1, 1–2 IQR; Mann–Whitney U test, U = 140298746.5, p ≤ 0.001). However, the solid line in Fig. 2 also shows that, as the number of consecutive missed appointments increased, so the number of patients decreased. There were fewer than 100 patients each for the numbers of missed appointments exceeding 13.
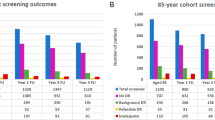
When considered by type of diabetes, the number of missed appointments was significantly higher for type I (median 2, range 1–34, 1–3 IQR), than for type II disease (median 1, range 1–34, 1–2 IQR; Mann–Whitney U test, U = 77843106.0, p ≤ 0.001). The graphical representation of the percentage referable retinopathy against number of consecutive missed appointments (Fig. 3) also shows that a higher proportion of type I patients was referable for a given number of missed appointments (for example, after two missed appointments ~10% of patients with type II diabetes had referable retinopathy, compared to 20% of those with type I diabetes).
The number of patients ascribed to each number of consecutive missed appointments by disease type (solid line type II, dashed line type I), and the percentage of patients who were referable at their next appointment as a function of the total number of consecutive missed appointments (closed circles type II, open circles type I) are shown.
With respect to demographic factors, there was a significant difference in the number of consecutive missed appointments between genders, with males having a higher average number of consecutive missed appointments (Median 1, 1–2 IQR) than females (Median 1, 1–2 IQR); Mann–Whitney U test, U = 469124134.0, p ≤ 0.001). Also, a significantly higher proportion of males were referable at their next appointment (10.7%) than females (8.7%; Chi-squared test; Χ2 (2) = 67.829, p ≤ 0.001).
There was a small but significant negative correlation between age and the number of missed appointments (Pearson’s r = −0.065, p ≤ 0.001). When patients were grouped by age (see Table 1), there was a statistically significant difference in the number of nonattendances per age group, (Kruskal–Wallis H test; χ2 (8) = 398.76, p ≤ 0.001). The 22–31 year old group had the highest number of nonattendances (median 2, 1–3 IQR), whilst the older adults ≥92years had the lowest tendency to fail to attend (median 1, 1–2 IQR). When type I and type II diabetes are considered separately, the significant correlation between age and number of missed appointments remains for type II (Pearson’s r = −0.049, p ≤ 0.001), but not type I disease (p = 0.103).
The distribution of the population between ethnic groups can be seen in Table 2. There was a statistically significant difference in the median number of nonattendances between ethnic groups (Kruskal–Wallis H test; χ2 (16) = 581.521, p ≤ 0.001). The highest number of nonattendances was recorded for the ‘White & Black African - mixed’, ‘Any other Black Background’, ‘African’, ‘White and Black Caribbean-mixed’, and ‘Any Other White’ (all median 2, 1–3 IQR). However, the median number of consecutive nonattendances ranged between 1 and 2 for all ethnic groups.
Discussion
This retrospective observational study indicated that failure to attend multiple consecutive screening appointments is associated with an increased risk of referable retinopathy being diagnosed at the next screening appointment. There was evidence that demographic factors such as age, gender and ethnicity have a significant effect upon risk of multiple failures to attend appointments.
Within the North East London Diabetes Eye Screening Service, if patients miss their appointment, they are offered another appointment automatically. Patients are offered further appointments at increasing intervals (from one month upwards) until they miss a third appointment, when there will be a gap of about six months before the cycle of appointment invitations starts over (after each missed appointment, a letter of invitation is sent to encourage the patient to call for a new appointment). In this study, patients who had failed to attend 10 consecutive appointments were nearly 3 times more likely to have referable retinopathy at their next appointment than individuals who had only missed one appointment.
The only prior published study relating number of consecutive nonattendances in a UK diabetic retinopathy screening service to risk of referable retinopathy had a smaller patient database of 6556 participants based in south-east London [14]. Their patient demographic varied from this study in that most of their participants were of white ethnic origin followed by Caribbean then African, and the greatest proportion of participants were in the age group 65–74 years. In contrast, after ‘White British’ (21.6%), patients who identified as ‘Bangladeshi’ formed the largest part of the current cohort (17.7%), and the majority of participants fell within a younger 52–61 (27.3%) age-group. Despite these population differences, the relationship between increased risk of referable retinopathy and number of consecutive missed appointments was clear in both studies.
This strong relationship between increasing number of consecutive missed appointments and the chance of referable retinopathy being diagnosed at the next visit may be, in part, because these patients are also missing other healthcare appointments. In one study, diabetic patients showing nonattendance behaviour with their dietician were also more likely to miss appointments with other care givers [17]. It may also reflect a generally lower level of compliance to lifestyle advice in people with a tendency to miss appointments, and the missed opportunity to provide lifestyle advice before retinopathy has reached the referable stage. The findings of this study are in accordance with a report that, amongst other factors, poorer glycaemic control was more frequent in those who had infrequent attendance at clinic [18].
The individuals with type I diabetes in this study comprised ~5% of the study sample. This proportion was slightly lower than expected as type I diabetes constitutes ~8% of cases of diabetes in the wider UK population [19]. This is almost certainly due to the marked ethnic heterogeneity in the population, many people originating from communities with a high prevalence of type 2, but a lower prevalence of type 1 than is found in the white north European population [20].
Within the study sample, people with type I diabetes showed a significantly greater number of consecutive missed appointments than those with type II disease. This could reflect a higher level of health complications and co-morbidities associated with type I disease [21], meaning that a subset of patients with this condition will have numerous other medical appointments and health complications to manage. The patients with type I disease were also significantly younger than those with type II disease. Therefore, another possible explanation for the significantly higher number of missed appointments in this cohort was that the younger patients may find greater difficulty in getting time off work, or time away from their mandatory daily activities. This finding is consistent with published data suggesting that 57% of people with type I diabetes, as opposed to 41% of people with type II, fail to attend at least eight of the nine basic annual health checks which are recommended for people with diabetes [22], and that 20% of people with type I vs. 40% of people with type II diabetes are meeting treatment targets to reduce risk of complications [22]. For all numbers of consecutive missed appointments, people with type I diabetes were more likely to be referable at the next visit. This reflects the fact that the global prevalence of diabetic retinopathy is much higher in type I than type II disease (77% vs. 25% [4],).
In the current study, there was a small but significant trend for males to have a higher number of missed appointments. In contrast, Forster et al. [14]. found that missing screening appointments was not associated with gender [14]. Another audit of diabetes eye screening offered to 21,797 patients in Oxfordshire, indicated that uptake was actually higher for men (83.2%) than for women (81.5%) [23]. This contrasting finding suggests that the tendency for men to be less compliant may not be consistent across populations. As age increased in the current cohort, the number of consecutive nonattendances decreased. Patients between ages 22–31 years were most likely to fail to attend, whilst the elderly aged ≥92 years had the lowest tendency to fail to attend. Other studies have also reported that younger patients are more likely to have nonattendance behaviour [12, 14, 23]. When the distribution of age in the cohort of patients missing at least one appointment was considered, the peak frequency was at around 56 years, with a second smaller peak at around 70 years. It is possible that the first peak reflects the increased problems associated with finding time to attend appointments for those in the working age category, whilst the second peak may be reflective of co-morbidities which begin to become more prevalent in this age group [21], making attendance of appointments more challenging. Within this study, patients of black and African ethnicities showed a small but statistically significantly greater number of consecutive nonattendances than patients of other ethnicities. Studies in other aspects of healthcare have also indicated that non-Caucasian ethnicity may be a risk factor for nonattendance of appointments [24]. Others have reported that certain psychosocial variables may also play a role in nonattendance, such as lower risk perception related to diabetes [17]. This could form the basis of future studies in this area.
This evidence suggests that any strategies which can be used to increase uptake of screening appointments may help to reduce risk of onset of referable retinopathy. There is substantial evidence that advice on lifestyle interventions such as reduction of body mass index and dietary changes may help to avert the risk of referable retinopathy [4]. Attendance to appointments provides an opportunity to proffer this advice. Approaches have been considered to help to increase uptake in some services. Contacting individuals by telephone and discussing causes for missed appointments may help understanding of the process of screening and the insidious effects of diabetes. Many screening services now send out automated appointments according to software databases. A reminder closer to the appointment date (for example SMS test messaging) may help to increase uptake [25]. Sending patients pre-booked appointments rather than an invitation to book an appointment may also help uptake [26]. Allowing patients to alter appointments online may, in future, also make the programme more accessible.
As discussed above, people with diabetes are expected to attend at least nine basic annual health checks, in addition to any additional appointments required when complications develop [22]. Another way to improve attendance may be to attempt to reduce the patient burden by consolidating screening tests into one visit. Patients of working age in particular may find it easier to schedule a reduced number of hospital visits.
This study from the third largest diabetes eye screening programme in England provides clarity on the association between non-attendance for screening and adverse clinical outcomes. The strength of this manuscript is that it analyses a large data set to demonstrate this point. The findings also suggest that interventions could be focused on those most likely to fail to attend such as; younger patients, people with type I disease, males and people of African origin. This may be useful as a benchmark for what to expect when rolling out a DR screening service, and for anticipating which patients might not attend. Limitations are that it was restricted to north-east London and thus the findings might not reflect national trends. Duration and type of diabetes, smoking, diet and other risk factors were not considered. Further research could involve looking at which boroughs were most vulnerable to referable retinopathy or most likely not to attend. This may offer some insight into the effect of socioeconomic status on attendance behaviour.
Summary
What was known before
-
A previous study indicated that, in a patient database in South East London, missing diabetes eye screening appointments was associated with an increased risk of referable retinopathy at the next appointment. The current study included a larger patient cohort with a different ethnicity and age demographic to determine whether this finding was generalisable.
What this study adds
-
This retrospective observational study indicated that failure to attend multiple consecutive screening appointments is associated with an increased risk of referable retinopathy being diagnosed at the next screening appointment. Despite the differences between this cohort and the previously published study, the association was consistent. The findings also suggested that interventions to improve attendance could be focused on those most likely to fail to attend such as; younger patients, people with type I disease, males and people of African origin.
References
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442.
Liew G, Michaelides M, Bunce CA. comparison of the causes of blindness certifications in England and Wales in working age adults (16–64 years), 1999–2000 with 2009–2010. BMJ Open. 2014;4:e004015.
Access Economics. Future sight loss UK (1): the economic impact of partial sight and blindness in the UK adult population. Report prepared for RNIB by Access Economics Pty Limited. Canberra, Australia: Access Economics; 2009. https://www.rnib.org.uk/sites/default/files/FSUK_Report.pdf.
Yau JWY, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Beck T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–64.
NICE. Management of Type 2 diabetes - retinopathy screening and early management. London: NICE; 2002.
NICE. Type 1 diabetes: diagnosis and management of type 1 diabetes in adults. London: NICE; 2004.
Early Treatment Diabetic Retinopathy Study Research Group. Early photocoagulation for diabetic retinopathy. ETDRS Report Number 9. Ophthalmology. 1991;98:766–85.
Photocoagulation for diabetic macular edema. Early treatment diabetic retinopathy study report number 1. Early treatment diabetic retinopathy study research group. Arch Ophthalmol. 1985;103:1796–806.
DRCR Network. A randomized trial comparing intravitreal triamcinolone acetonide and focal/grid photocoagulation for diabetic macular edema. Ophthalmology. 2008;115:1447–9.
Wykoff CC. Impact of intravitreal pharmacotherapies including antivascular endothelial growth factor and corticosteroid agents on diabetic retinopathy. Curr Opin Ophthalmol. 2017;28:213–8.
Kai S, Sarngal S, Ganjoo S. To study the prevalence of diabetic retinopathy in diabetes mellitus patients and its correlation with various associated risk factors. J Evolution Med Dent Sci. 2015;4:16341–6.
Leese GP, Boyle P, Feng Z, Emslie-Smith A, Ellis JD. Screening uptake in a well-established diabetic retinopathy screening program: the role of geographical access and deprivation. Diabetes Care. 2008;31:2131–5.
Warwick AN, Brooks AP, Osmond C, Krishnan R. Prevalence of referable, sight-threatening retinopathy in type 1 diabetes and its relationship to diabetes duration and systemic risk factors. Eye (Lond). 2017;31:333–41.
Forster AS, Forbes A, Dodhia H, Connor C, Du Chemin AD, Sivaprasad S, et al. Non-attendance at diabetic eye screening and risk of sight-threatening diabetic retinopathy: a population-based cohort study. Diabetologia. 2013;56:2187–93.
Public Health England. National pathway standards for the NHS diabetic eye screening (DES) programme. London, United Kingdom: Public Health England; 2014
Office for national statistics; Ethnic Group https://www.ons.gov.uk/methodology/classificationsandstandards/measuringequality/ethnicgroupnationalidentityandreligion#ethnic-group.
Spikmans FJM, Brug J, Doven MMB, Kruizenga HM. Van Bokhorst-van der Schueren MAE. Why do diabetic patients not attend appointments with their dietitian? J Hum Nutr Diet. 2003;16:151–8.
Khan H, Lasker SS, Chowdhury TA. Exploring reasons for very poor glycaemic control in patients with Type 2 diabetes. Prim Care Diabetes. 2011;5:251–5.
NHS Digital. National Diabetes Audit 2017/18: Report 1: care processes and treatment targets. London, United Kingdom: NHS Digital; 2018.
Health and Social Care Information Centre. Health survey for England 2004, health of ethnic minorities and ethnic-specific obesity cufoffs for diabetes risk: cross-sectional study of 490,288 UK Biobank Participants. Diabetes Care. 2006;37:2500–7.
NHS Digital. National diabetes audit report 2A: complications and mortality royal college of physicians sentinel stroke national audit programme (SSNAP). National clinical audit annual results portfolio March 2015–April 2016. London, United Kingdom: NHS Digital; 2017.
NHS Digital. National diabetes audit care processes and treatment targets 2017–18 short report. London, United Kingdom: NHS Digital; 2018.
Moreton RBR, Stratton IM, Lipinski H, Scanlon PH. Factors determining uptake of diabetic retinopathy screening in Oxfordshire. Diabet Med. 2017;34:993–9.
Kempny A, Diller GP, Dimopoulos K, Alonso-Gonzalez R, Uebing A, Li W, et al. Determinants of outpatient clinic attendance amongst adults with congenital heart disease and outcome. Int J Cardiol. 2016;203:245–50.
Boksmati N, Butler-Henderson K, Anderson K, Sahama T. The effectiveness of SMS reminders on appointment attendance: a meta-analysis. J Med Syst. 2016;40:90.
Lewis K. Improving patient compliance with diabetic retinopathy screening and treatment. Community Eye Health 2015;28:68–69.
Acknowledgements
This study was carried out as part of an MSc research project under the auspices of City, University of London. There was no external funding for the research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Virk, R., Binns, A.M., Chambers, R. et al. How is the risk of being diagnosed with referable diabetic retinopathy affected by failure to attend diabetes eye screening appointments?. Eye 35, 477–483 (2021). https://doi.org/10.1038/s41433-020-0877-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-0877-1
This article is cited by
-
Racial, Ethnic, and Socioeconomic Disparities Drive Appointment No-Show in Patients with Chronic Eye Disease
Journal of Racial and Ethnic Health Disparities (2023)
-
Attendance in a national screening program for diabetic retinopathy: a population-based study of 205,970 patients
Acta Diabetologica (2022)
-
Comment on: How is the risk of being diagnosed with referable diabetic retinopathy affected by failure to attend diabetes eye screening appointments?
Eye (2021)