Abstract
Objectives
To determine the efficacy and safety of combined phacoemulsification and single first-generation iStent implantation over 84 months.
Subjects/Methods
Single-surgeon, single-centre, uncontrolled prospective interventional study in real-world settings. Forty-one patients with open-angle glaucoma on at least one antihypertensive drop underwent phaco-iStent surgery. This cohort was monitored over the subsequent 84 months. The primary outcome measure was intraocular pressure (IOP). Secondary outcome measures were number of glaucoma drops, visual acuity, cup-disc-ratio (CDR), mean deviation (MD) and visual field index (VFI). Thirty-one (76%) patients survived to 48 months and 19 (46%) patients to 84 months.
Results
At 84 months, we demonstrate an absolute mean reduction of 4.87 mmHg (95% CI 1.62–7.64) for IOP and 0.59 (95% CI 0.03–1.16) for number of glaucoma drops. At the final clinic visit, LogMAR VA improved by 0.21 (95% CI 0.08–0.34), with no significant change in CDR, MD and VFI. Attrition was mainly due to death (27%) and further glaucoma surgery (12%). A single patient suffered from postoperative hyphaema, with no sequalae. Patients at high risk for progression to filtration surgery were defined as those on oral acetazolamide for IOP control, or those fulfilling all the following criteria: IOP ≥ 20 mmHg, CDR ≥ 0.7, MD ≤ −4.0 dB, number of drops ≥ 2. This group is to be considered for surgery as the next step in management according to NICE glaucoma guidelines. These patients (n = 14) demonstrated a more marked final IOP reduction of 6.85 mmHg (95% CI 3.97–9.75) vs 1.62 mmHg (95% CI 0.04–3.22) in their low-risk counterparts (n = 27). Reduction in glaucoma drops was 0.86 (95% CI 0.07–1.64) for the high-risk and 0.56 (95% CI 0.06–1.05) for the low-risk cohort. Further glaucoma surgery was required for 4 (29%) high-risk and 1 (0.5%) low-risk patients over the study period.
Conclusions
Our results strongly suggest that the expected outcome of phaco-iStent surgery is a maintained reduction in intraocular pressure and number of glaucoma medications over 7 years. This is combined with a negligible rate of complications, a sustained improvement in central visual acuity, and a reliable maintenance of peripheral visual function.
Similar content being viewed by others
Introduction
Glaucoma is the second most common cause of irreversible blindness worldwide. In open-angle glaucoma, resistance to the outflow of aqueous humour is often the limiting factor in maintaining an optimal intraocular pressure (IOP). Historical treatment modalities have included topical medication in the form of eye drops, laser therapy and glaucoma drainage surgery. The common objective of these operations is the re-channelling of aqueous fluid outside the anterior chamber by bypassing the eyeʼs natural drainage pathways. Eye drops demand meticulous adherence from patients, a difficult feat in the face of ocular surface irritation and discomfort [1]. Selective laser trabeculoplasty (SLT) and argon laser trabeculoplasty (ALT) provide good solutions to the problem of adherence, but are limited in their longevity, and unpredictable in their efficacy [2]. Drainage surgery is the gold standard end-point in the face of progressive optic nerve damage despite conservative treatment. Trabeculectomy and tube surgery have the support of decades of data confirming their pressure lowering effect, but are susceptible to non-negligible complications in the form of inflammation, hypotony, bleb encapsulation, and a lifelong risk of infection [3]. In the postoperative period, frequent drop administration and regular follow-up are key to successful outcomes, a challenging ordeal for patients with limited mobility, dexterity and cognitive impairment [4].
Novel approaches to IOP reduction aim to circumvent the limitations of these treatments, namely adherence, comfort and complications. The advent of micro-invasive glaucoma surgery (MIGS) has inspired a paradigm shift in the surgical approach to glaucoma management. As one of the first and most widely used MIGS devices, the iStent (Glaukos Corporation, Laguna Hills, CA, USA) has been the bellwether of this trend. This 1 mm long, 0.3 mm wide, non-ferromagnetic titanium stent bypasses the trabecular meshwork and cannulates Schlemm’s canal, acting as a conduit between the anterior chamber and distal drainage pathways.
Samualson et al. first reported that the addition of a single first-generation iStent to phacoemulsification offers a statistically and clinically significant reduction in IOP with less medication use compared with cataract surgery alone [5]. The outcomes of combined cataract surgery and iStent implantation in real-world settings were first reported in the original Manchester iStent study [6]. Patel et al. showed that at 6 months, the mean IOP was lowered from 21.1 to 16.7 mmHg, while the mean number of drops reduced from 2.3 to 0.6 (p < 0.01). Tan and Au observed the same cohort at 3 years, demonstrating a final mean IOP of 17.1 mmHg on 1.3 drops (p < 0.01) [7]. In this study, we follow these patients for a further 4 years, analysing data on the longest follow-up series for single iStent implantation published to date.
Materials and methods
This study was a single-surgeon, single-centre, uncontrolled prospective interventional case series at Manchester Royal Eye Hospital, UK. Forty-one consecutive cases were selected to undergo unilateral combined cataract surgery and ab-interno single first-generation iStent implantation (phaco-iStent) between January 2010 and June 2011. Inclusion criteria were mild, moderate and severe open-angle glaucoma, current use of at least one antihypertensive drop and visibility of the nasal scleral spur on gonioscopy documented as Shaffer grade 3+. This was to facilitate implantation of iStent within the nasal drainage angle. Exclusion criteria were other forms of glaucoma, history of any angle surgery or cyclodestructive procedure, elevated episcleral venous pressure and peripheral anterior synechiae in the nasal angle. Perimetry was performed using the 24-2 SITA Standard protocol on the Humphrey visual field analyser. Best-corrected visual acuity (BCVA) was recorded in LogMAR units and IOP measurements recorded in millimetres of mercury (mmHg) via Goldmann applanation tonometry.
The surgical procedure has been previously reported [2]. All glaucoma medications including oral acetazolamide were discontinued following surgery. Chloramphenicol qds and dexamethasone 0.1% qds were instilled for 3 weeks postoperatively. A standardised follow-up protocol mandated documentation of BCVA, IOP and number of drops at 1 week, 1 month, 3 months and 6 months. The frequency of subsequent follow-ups and need for recommencement of hypotensive medications were determined by the attending clinician according to IOP and disease progression. IOP and the number and breakdown of topical drops were then recorded every 12 months for a total duration of 7 years. Patients were excluded from data collection following death, further glaucoma surgery, transfer of care to another hospital, discharge to own optometrist or self-discharge. At the final clinic visit, BCVA, IOP, number of drops, cup–disc ratio (CDR), visual field mean deviation (MD), and visual field index (VFI) were recorded.
Informed consent was obtained from all patients after a thorough explanation of the procedure and its risks. All procedures followed the tenets of the Declaration of Helsinki. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research. Statistical analysis was performed using Origin Pro 2018 (OriginLab Corporation, MA). The Kolmogorov–Smirnov test was used to confirm a normal distribution of IOPs at the preoperative and final clinic visits. Paired t-tests were used to compare continuous outcomes over time. The limit of statistical significance was set at p < 0.05.
Given the attrition rate due to patient death, a post hoc paired t-test power calculation was performed utilising the data from surviving patients at the 84-month time point to ensure adequate power in the face of reducing patient numbers. For the surviving sample size of 19, at a one-sided significance level of 0.05, the mean IOP reduction was significant with a power of 86.33%.
Results
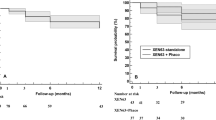
The mean age of participants was 76.1 years old (range 41–98) with a male-to-female ratio of 1.4:1. The aetiology of the glaucomatous process was primary open angle in 28 patient (68%), normal tension in 4 (10%), pseudoexfoliative in 4 (10%), angle recession in 2 (5%), mixed mechanism (open angle following previous peripheral iridotomy) in 2 (5%), and ocular hypertension in 1 (2%). Nine patients (22%) had previous SLT or ALT and two (4.9%) had peripheral iridotomies resulting in Shaffer grade 3 angle opening. At the time of enrolment, the mean duration since glaucoma diagnosis was 6.1 ± 3.2 years. At 48 months, 31 (76%) patients were still enrolled. The longest follow-up period was 7 years (84 months), with 19 (46%) patients surviving to this time point. Attrition was due to death in 11 (27%), further glaucoma surgery in 5 (12%), transfer of care to another hospital in 2 (5%), discharge to community optometrist in 2 (5%), and self-discharge in 2 (5%) patients.
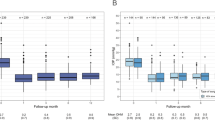
The mean preoperative parameters were as follows; IOP 21.3 ± 4.96 mmHg, number of topical drops 2.17 ± 0.95, BCVA 0.50 ± 0.29, CDR 0.67 ± 0.24, visual field MD −9.46 ± 7.78 and VFI 78 ± 21%. Six patients were on oral acetazolamide. The complication rate of iStent insertion was 2.4%, with a singular patient developing postoperative hyphaema that resolved without sequelae within 1 week. The variation of IOP and number of hypotensive drops over the study period are demonstrated in Fig. 1. Acetazolamide was discontinued for all six patients and was not required in any patient thereafter. IOP reduction was modest in the first postoperative month, dropping from 21.3 ± 4.96 mmHg on 2.17 ± 0.95 drops to 19.82 ± 5.86 mmHg on 0.21 ± 0.52 drops (p < 0.01). This reduction peaked at 6 months, with IOP averaging 16.05 ± 3.43 mmHg on 0.55 ± 0.90 drops (p < 0.01). This marked IOP reduction was steadily maintained at 24 months, encouraged by the gradual reintroduction of 1.02 ± 1.15 drops (p < 0.01). By the 84th month, IOP control remained remarkably tight amongst survivors at 16.42 ± 3.27 mmHg (p < 0.01), while the average number of drops increased to 1.58 ± 1.17 (p < 0.01). At this time point, the absolute reduction in mean IOP and drops for survivors were 4.63 mmHg (95% CI 1.62–7.64) and 0.79 (95% CI 0.16–1.42), respectively (p < 0.01).
Given the high attrition rate at 7 years, predominantly due to death and further surgery, it is elucidating to compare baseline parameters with final recorded values at the last clinic visit for each patient. These results are demonstrated in Fig. 2. The reduction in IOP is accompanied by stability in optic nerve function parameters. BCVA improved from 0.49 to 0.34 (p < 0.01), an expected outcome following uncomplicated phacoemulsification and IOL implantation. CDR increased from 0.67 ± 0.24 to 0.72 ± 0.24 (p < 0.01), and the VFI reduced from 81.8 ± 18% to 77 ± 23% (p < 0.05). MD declined from −8.46 to −9.00, although this was statistically non-significant (p = 0.39). For the five patients (12.2%) requiring further intervention, the average time to surgery was 4.4 years. The study design did not mandate retinal nerve fibre layer analysis and was thus not uniformly performed on this cohort pre and postoperatively.
Figure 3 illustrates the daily drop requirement as a percentage of the total cohort of 41 patients. Preoperatively, there were no drop-free patients, a result of the study exclusion criteria. Six of these patients were additionally taking oral acetazolamide as a temporising measure. Postoperatively, 63% were drop-free at 12 months (n = 41), 34% at 36 months (n = 36) and 21% at 84 months (n = 19). Only 27% of patients were controlled on ≤1 drop prior to iStent implantation. Postoperatively, this value increased to 83% at 12 months, 63% at 36 months and 47% at 84 months.
In the 7 years leading up to phaco-iStent surgery, the mean number of clinic visits per annum was 2.5 ± 0.34 (range 2–3). This number rose to 4.83 in the first postoperative year, a figure which reflects the protocolised follow-up regime at 1 week, 1 month, 3 months and 6 months. In the subsequent years, the number of clinic visits steadily declined, achieving a steady range between 1.44 and 1.65 from years 4 to 7. These results are demonstrated graphically in Fig. 4.
In the year leading up to cataract surgery, the number of clinic visits was artificially raised due to the extra consultation required for the proposed surgery. Similarly, this number was elevated following surgery due to the protocolised mandatory visits in the first 12 months. Exclusion of these data yields a preoperative average of 2.4 ± 0.27 and a postoperative average of 1.71 ± 0.32.
Discussion
Our data strongly suggest that in the real-world setting, the expected outcome of phaco-iStent surgery is one of negligible complications, with sustained improvement in central visual acuity and reliable maintenance of peripheral visual function over 7 years.
A by-product of patient selection from a tertiary ophthalmology centre was the inclusion of 14 cases (34%) which were high risk for eventual glaucoma filtration surgery. We define this high-risk cohort as patients satisfying all the following conditions; IOP ≥ 20 mmHg, CDR ≥ 0.7, MD ≤ −4.0 dB, and number of drops ≥2. In addition, patients on oral acetazolamide, which could not tolerate other topical treatment modalities were included in this definition. According to NICE guidance (2017) clinicians within the UK are to consider surgery with antimetabolite augmentation for patients at risk of progression “after trying drugs from two therapeutic classes”. Indeed, in this group of patients, 50% had already undergone laser trabeculoplasty, and in the absence of adequate IOP control, would be considered for glaucoma drainage surgery in the era before the advent of MIGS. Table 1 illustrates clinical outcomes at the final clinic visit taking into account the risk for progression to surgery. It is interesting to note that the higher preoperative IOP in the high-risk subgroup (24.71 vs 19.51 mmHg) is counteracted by a significantly higher absolute IOP reduction in this cohort (6.85 vs 1.62 mmHg). Thus, the final average IOP is comparable in the two cohorts, despite the disparity in glaucoma severity at the time of enrolment.
Arriola-Villalobos et al. reported the long-term outcomes of phaco-iStent in a cohort of 19 patients with mild-to-moderate open-angle glaucoma, with 13 patients completing 5 years of follow-up [8]. Mean IOP reduction at the final visit was 3.16 mmHg (19.42 preoperative vs 16.26 final), with mean drop reduction of 0.48 (1.32 preoperative vs 0.84 final). We report a higher magnitude IOP and drop reduction of 4.87 mmHg (21.29 preoperative vs 16.42 at 84 months) and 0.59 (2.17 preoperative vs 1.58 at 84 months), respectively. Larger randomised controlled trials (RCTs) by Craven et al. and Fea et al. both demonstrated a more modest IOP reduction of 1.5 mmHg at 12 months [9, 10]. This less sizeable IOP reduction correlates with lower preoperative IOPs, measuring 18.6 ± 3.4 for Craven et al. and 17.8 ± 2.7 mmHg for Fea et al. Indeed, in our low-risk cohort defined above, we observe a preoperative IOP of 19.51, and an 84-month IOP of 18.14 mmHg closely mimicking these RCT findings, with a singular patient progressing to further surgery. Our results suggest that the IOP findings of these RCTs at 12 months are sustainable for up to 7 years. In addition, the magnitude of IOP reduction positively correlates with the magnitude of the preoperative IOP. These observations may pave the way for further exploration of the role of MIGS as one step of the treatment pathway for non-mild glaucoma.
Eleven (27%) of the 41 patients enrolled in this study passed away during the 7-year follow-up period. According to the Office for National Statistics, the average lifespan in the UK is 80.96 years, while the average age of our patients was 76.15 years at the time of surgery. In the group of patients that died during this study, the mean age at enrolment was 82.9, with an average survival of 5.18 years, yielding an average lifespan of 88.09. At enrolment, 4 (36%) of these 11 were classified as high risk and none were drop-free. The average preoperative IOP was 20 mmHg on 2.27 drops with BCVA 0.6, CDR 0.6 and MD −8.205 dB. At the time of death, the average IOP was 17.73 on 1.36 drops, with BCVA 0.48, CDR 0.63 and MD −8.87 dB. Five (45%) of these patients were drop-free at the time of death. None required further glaucoma surgery.
King et al. found that the survivorship of glaucoma patients over 20 years is directly correlated with their age at diagnosis [11]. Mean age at diagnosis was 73.7 in their deceased group versus 63.2 years for survivors. The mean age of death was 84 years. Interestingly, only 23.5% of the deceased patients required trabeculectomy, nearly half as much as the 47.5% of survivors. In their multicentre analysis, Kirwan et al. reported the mean age of patients undergoing trabeculectomy surgery in the United Kingdom as 69.2 ± 10.7 [12]. While it appears that patients selected for trabeculectomy are generally younger than our cohort, 34% of our patients were classified as high risk for progression to trabeculectomy. The mean IOP at the final clinic visit was 17.86 for our high-risk and 17.92 for our low-risk cohorts. While it may be argued that the higher risk category of patients require more aggressive IOP lowering, the stability of all central and peripheral visual parameters over 84 months strongly suggests that MIGS can be a suitable surgical option for these patients.
The average number of clinic visits per year prior to surgery was 2.4, in contrast to 1.7 in the postoperative years. We believe this is the first time such a reduction of glaucoma monitoring need has been demonstrated. This is a noteworthy reduction and confers an enhanced quality of life (QoL) to patients and cost savings to the healthcare system. Further analysis reliant upon subjective QoL improvement questionnaires may further aid in establishing the incremental cost effectiveness ratio for this intervention. Formal QoL assessment has traditionally been lacking in studies of MIGS. Our results provide the basis for an indirect inference of QoL improvement. In summary, we found a sizeable reduction in topical and oral medications, clinic visits and an obviation of the need for glaucoma surgery, a challenging feat in such elderly patients.
The complication rate for our cohort was negligibly small, suggesting a good long-term safety profile for this procedure. This finding is corroborated by larger randomised control trials in which the complication rates of phaco-iStent were comparable to phacoemulsification surgery alone [5].
Study limitations
As a cohort study of MIGS intervention in the real-world setting, this study followed the first 41 patients to undergo phaco-iStent surgery under the principal investigator. A natural result of this patient selection process is heterogeneity in patient demographics and disease severity. While this limits the scope of detailed conclusions that may be drawn for specific patient populations, it does provide valuable insight into the natural history of disease progression following this intervention in the real world.
Beyond the first 12 months of mandatory follow-up, the frequency of clinic attendance was influenced by the judgement of the attending clinician and the capability of attendance of the patients. This reality imposed a variable gap in data collection over the course of 7 years, despite our best efforts to extract clinical data at annual intervals.
The attrition rate was high, predominantly due to mortality, a phenomenon that was expected given the advanced age of the patients at the study outset. This fact has implications for all glaucoma interventions and will be consequential in cost-analysis calculations that take into account the longevity of derived benefit from a given procedure. Six patients were lost to follow-up as a result of a change in living location, discharge back to their own optometrist or self-discharge.
We acknowledge our classification of “high risk for filtration surgery” can be debatable. However, we believe our criteria reflects real life clinical practice in the face of current NICE guidance in the UK. We feel this allows an insight into the pre-intervention severity of disease in our cohort, and the results suggest the possibility that phaco-iStent can delay the need for filtration surgery in suitable patients.
While phaco-iStent efficacy and safety have been demonstrated at 7 years, the main obstacle to routine use is that of cost effectiveness. The relatively high cost of these MIGS devices is a barrier to entry in a variety of healthcare models, and must pass the health economics litmus test if it is to become routinely funded.
Summary
What was known before
-
The iStent has been demonstrated to successfully reduce IOP up to 5 years after implantation.
-
The long-term effects of iStent on a mixed cohort of low- and high-risk glaucoma patients in the real world has not been extensively studied.
What this study adds
-
First published report of real-world outcomes of phaco-iStent surgery at 7 years.
-
Mean IOP reduction was 4.87 mmHg and mean glaucoma drop reduction was 0.59 at 7 years.
-
Patients at risk for progression to filtration surgery demonstrated a more marked IOP reduction. Only 29% of these patients required further glaucoma surgery at 7 years.
References
Rossi GC, Pasinetti GM, Scudeller L, Bianchi PE. Ocular surface disease and glaucoma: how to evaluate impact on quality of life. J Ocul Pharmacol Ther. 2013;29:390–4.
Juzych MS, Chopra V, Banitt MR, Hughes BA, Kim C, Goulas MT, et al. Comparison of long-term outcomes of selective laser trabeculoplasty versus argon laser trabeculoplasty in open angle glaucoma. Ophthalmology. 2004;111:1853–9.
Gedde SJ, Herndon LW, Brandt JD, Budenz DL, Feuer WJ, Schiffman JC. Postoperative complications in the Tube Versus Trabeculectomy (TVT) study during five years of follow-up. Am J Ophthalmol. 2012;153:804–14.
Murdoch I. Post-operative management of trabeculectomy in the first three months. Community Eye Health. 2012;25:73–5.
Samuelson TW, Katz LJ, Wells JM, Duh YJ, Giamporcaro JE. Randomized evaluation of the trabecular micro-bypass stent with phacoemulsification in patients with glaucoma and cataract. Ophthalmology. 2010;118:459–67.
Patel I, de Klerk TA, Au L. Manchester iStent study: early results from a prospective UK case series. Clin Exp Ophthalmol. 2013;41:648.
Tan SZ, Au L. Manchester iStent study: 3-year results and cost analysis. Eye. 2016;30:1365–70.
Arriola-Villalobos P, Martínez-de-la-Casa JM, Díaz-Valle D, Fernández-Pérez C, García-Sánchez J, García-Feijoó J. Combined iStent trabecular micro-bypass stent implantation and phacoemulsification for coexistent open-angle glaucoma and cataract: a long-term study. Br J Ophthalmol. 2012;96:645–9.
Craven ER, Katz LJ, Wells JM, Giamporcaro JE. Cataract surgery with trabecular micro-bypass stent implantation in patients with mild-to-moderate open-angle glaucoma and cataract: two-year follow-up. J Cataract Refract Surg. 2012;38:1339–45.
Fea AM, Belda JI, Rękas M, Jünemann A, Chang L, Pablo L, et al. Prospective unmasked randomized evaluation of the iStent inject® versus two ocular hypotensive agents in patients with primary open-angle glaucoma. Clin Ophthalmol. 2014;8:875–82.
King C, Sherwin C, Ratnarajan G, Salmon JF. Twenty-year outcomes in patients with newly diagnosed glaucoma: mortality and visual function. Br J Ophthalmol. 2018;0:1–4.
Kirwan JF, Lockwood AJ, Shah P, Macleod A, Broadway DC, King AJ, et al. Trabeculectomy in the 21st century: a multicenter analysis. Ophthalmology. 2013;120:2532–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ziaei, H., Au, L. Manchester iStent study: long-term 7-year outcomes. Eye 35, 2277–2282 (2021). https://doi.org/10.1038/s41433-020-01255-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01255-6
This article is cited by
-
Five-year outcomes of ab interno Xen 45 gel stent implantation
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Biomaterials for Glaucoma Surgery
Current Ophthalmology Reports (2023)
-
Efficacy and Safety of Pairing iStent Inject Trabecular Micro-Bypass and iAccess Precision Blade Goniotomy in Patients with Open-Angle Glaucoma
Ophthalmology and Therapy (2023)
-
„Minimally invasive glaucoma surgery“ – Kammerwinkelbasierte Verfahren im Vergleich
Die Ophthalmologie (2023)
-
Five-Year Outcomes of Single Trabecular Microbypass Stent (iStent®) Implantation with Phacoemulsification in Korean Patients
Ophthalmology and Therapy (2023)