Abstract
There has been an increase in the range of non-insulin anti-hyperglycaemic agents used to treat type 2 diabetes. With the globally rising rates of type 2 diabetes and complications such as diabetic retinopathy, it is important for ophthalmologists to be aware of these new agents and their impacts on diabetic retinopathy and diabetic macular oedema. We conducted a review of the literature to determine if there were any beneficial or harmful effects of the currently used anti-hyperglycaemic agents on diabetic retinopathy or diabetic macular oedema. Our review of the current literature found that apart from thiazolidinediones, anti-hyperglycaemic agents have been reported to have beneficial or neutral effects on diabetic eye complications. Thiazolidinediones (pioglitazone is the only one currently available) have been linked to incident or worsening diabetic macular oedema, although the rate is believed to be low. Glucagon-like peptide 1 (GLP1) agonists (incretins) in general are beneficial except semaglutide which is associated with increased rates of diabetic retinopathy complications. These results have implications for selection of anti-hyperglycaemic agents for patients with diabetic retinopathy or macular oedema. Further studies need to be conducted to identify if reported beneficial effects are independent of the impact of glycaemic control. Early worsening of retinopathy with tight glycaemic control should also be noted in interpretation of future studies.
摘要
目前用于治疗2型糖尿病的非胰岛素降糖药物的种类不断在增加。2型糖尿病与其并发症如糖尿病视网膜病 (DR) 的患病率在全球范围内升高, 因此眼科医生们知道这些新药物以及它们对DR和糖尿病性黄斑水肿 (DME) 发生与发展的影响十分重要。我们对现有降糖药物对于DR或DME的文献进行了分析与回顾。对现有的文献回顾发现, 除了噻唑烷二酮类, 其他降糖类药物对糖尿病眼部并发症的影响有益或中立。噻唑烷二酮类药物 (目前仅售吡格列酮) 与糖尿病性黄斑水肿的发生与恶化有关, 但发生率低。胰高血糖素样肽1 (GLP1) 激动剂 (肠促胰岛素类药物) 通常是有益的, 但是索马鲁肽与DR发生率的增加有关。这些结果提示对于并发DR与DME如何选择降糖药物。今后需要研究对DR及DME治疗有益的降糖药物的作用是否与血糖控制相关。血糖在严格控制达标下, 早期视网膜病变恶化也应成为今后的研究方向。
Similar content being viewed by others
Introduction
Pharmacotherapy for the management of diabetes mellitus has had enormous impact on glycaemic control and prevention of progression to complications of diabetes. Insulin was the first anti-diabetic pharmacotherapy developed from bovine extracts by Banting and Best in 1922 [1]. Since then, oral anti-hyperglycaemic agents have been developed for the management of type 2 diabetes (T2D), the first of which were the sulfonylureas discovered in the 1940s including tolbutamide, chlorpropamide and acetohexamide [2]. Though the effects of biguanides such as metformin were discovered in the 1920s, they were only available for use in 1959, and were not approved by the US Food and Drug Administration until 1994 due to increased incidence of lactic acidosis.
Over the last two decades, several new classes of anti-hyperglycaemic agents have become available. These include incretins (glucagon-like peptide-1 receptor agonists), dipeptidyl peptidase 4 (DPP4) inhibitors, sodium-glucose cotransporter-2 (SGLT-2) inhibitors, thiazolidinediones and alpha-glucosidase inhibitors. These agents may be used as monotherapy or in combination with more established agents and insulin. Diabetic retinopathy (DR) remains a major cause of blindness and visual morbidity and unlike most other causes, is a systemic condition requiring multidisciplinary approach in its management. This review will summarise the new anti-hyperglycaemic agents, their mechanisms of action, indications and contraindications, and any direct effects on DR independent of glycaemic control.
Methods
We conducted a Medline and PubMed search of published studies involving anti-hyperglycaemic agents and diabetic retinopathy from 1980 to Dec 2018. The search strategy terms were “diabetic retinopathy”, “macular oedema”, “glucagon-like peptide 1”, “dipeptidyl-peptidase IV inhibitors”, “sodium-glucose transporter 2”, “glucoside hydrolase inhibitors OR acarbose”, “thiazolidinediones”, “sulfonylurea compounds”, “metformin OR biguanides”. We identified 173 abstracts for review and retrieved 58 articles (Table 1). Full articles were retrieved if the abstract provided either clinical or laboratory data on the effects of anti-hyperglyacemic agents on retinopathy. We grouped articles by type, i.e., experimental research, population-based studies, review articles and case reports. Information about the mechanism of action, indications and contraindications of the oral hyperglycaemic agents was obtained from the MIMS medical database. The FDA database was cross-referenced to provide additional information.
Results
Relationship with retinopathy
Glucagon-like peptide 1 (GLP-1) agonists
GLP-1 agonists belong to a class of medications called incretins. Incretins are metabolic hormones secreted by intestinal cells in response to nutrient intake that stimulates pancreatic β-cell insulin production and impairs glucagon secretion, slows gastric emptying to reduce glucose absorption, and reduces appetite [3]. Their advantages over older oral anti-hyperglycaemic agents include lower risk of hypoglycaemia, moderate weight loss and the optional convenience of once-weekly dosing [4].
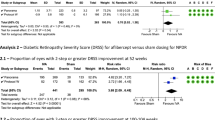
These agents have had mixed associations with DR (Table 2). An interventional case study reported complete regression of DME and improved visual acuity from 20/80 to 20/63 after 1 month of exenatide use [5]. However, another report noted dramatic deterioration in DR from background retinopathy to bilateral PDR and DME with reductions in glycated haemoglobin (HbA1c) from 11.9 to 4.8% after 4 months of exenatide treatment [6]. A retrospective analysis of 165 patients treated with exenatide for 10 months found it was associated with transient worsening of DR (with 30% of patients developing or worsening retinopathy with significant improvements in glycaemic control), but in 80% of these DR improved with continued treatment [7, 8]. Adverse findings on retinopathy were seen in a randomised control trial of 3297 patients looking at the effects of the GLP-1 agonist semaglutide on cardiovascular outcomes (SUSTAIN 6) [9]. This trial found DR complications occurred in 50 patients (3.0%) taking semaglutide compared with 29 (1.8%) in the placebo group (HR 1.76; 95% CI 1.11–2.78; p = 0.02). These reported deteriorations may, however, be related to early worsening of DR with rapid improvement of HbA1c [10], imbalance in baseline DR or short follow-up [11]. Hence further studies are needed to confirm the effects of GLP-1 agonists on retinopathy [12], in particular, if this is a group effect or related to semaglutide alone. A recent network meta-analysis found GLP-1 agonists appear to reduce the incidence and progression of nephropathy and to have no specific effect on retinopathy—with the notable exception of semaglutide, which may negatively impact the retina [13].
Experimental research has suggested potential protective effects of GLP-1 agonists on the diabetic retina through improved blood retina barrier (BRB) function and reduced neuronal apoptosis [14]. Intravitreal administration of an Exendin-4-analogue in rats is suggested to protect the retina by reducing glutamate levels through upregulating GLP-1 receptors and glutamate-aspartate transporter (GLAST) [15]. Furthermore, Exendin-4, a long-acting GLP-1 agonist, showed neuroprotective effects in early experimental DR by decreasing placental growth factor and intercellular adhesion molecule-1 expression and maintaining integrity of the BRB [16]. Systemic administration of liraglutide prevented retinal neurodegeneration via reduction of extracellular glutamate and increased pro-survival signalling pathways. Similar neuroprotective effects were seen using lixisenatide and exenatide independent of glucose reduction, thus suggesting GLP-1 receptor activation itself had retinal neuroprotective effects [17]. In summary, there is clinical and experimental evidence that GLP-1 agonists, with the exception of semaglutide, is likely beneficial for DR. It remains unclear if the adverse DR effects of semaglutide are related to early worsening or other factors, or represents a possible toxic effect on the retina.
DPP4 inhibitors
DPP4 is an enzyme responsible for the rapid degradation of GLP-1. Consequently, DPP4-inhibitors have been developed to delay the breakdown of incretins, thus prolonging their action. Advantages of DPP4-inhibitors over GLP-1 agonists include oral administration rather than injection, as well as avoiding the side effects of nausea associated with GLP-1 agonist use [3].
Experimental research on DPP4-inhibitors has indicated protective effects on DR (Table 2). This is suggested to occur in sitagliptin use by preventing nitrosative stress, inflammation and apoptosis in retinal cells, and preventing increase in BRB permeability [18, 19]. Vildagliptin has demonstrated beneficial metabolic effects by inhibiting body weight increase in addition to its anti-hyperglycaemic, anti-inflammatory and anti-thrombogenic effects in the retinas of obese T2D rats [20]. A retrospective chart review showed DPP4 inhibitors may reduce rates of DR progression [21] However, use of DPP4 inhibitors <12 months may be associated with early worsening of DR [22].
SGLT-2 inhibitors
SGLT-2 inhibitors are a new class of anti-hyperglycaemic medication that cause reversible, competitive inhibition of the SGLT-2 in the renal proximal tubule, resulting in urinary glucose excretion. Its advantages include acting independently of insulin, weight-lowering and non-association with risk of hypoglycaemia, while offering similar HbA1c control as DPP4-inhibitors, thiazolidinediones and sulfonylureas when added to metformin [23, 24].
Experimental research in spontaneously diabetic Torii fatty rats demonstrated that control of hyperglycaemia by a SGLT-2 inhibitor ipragliflozin slowed progression of diabetic microvascular complications of nephropathy, neuropathy and retinopathy (Table 2). This was demonstrated for retinopathy, slower progression of cataract formation and reduced changes on electroretinography [25]. The effects of SGLT-2 inhibitors on DR in humans have not been well studied. A case report found marked regression of DME after 16 weeks of ipragliflozin [26]. Unfortunately, none of the recent large clinical trials looking at the cardiovascular safety of SGLT-2 inhibitors included development or progression of DR as an outcome. Further studies in this area are warranted.
Alpha-glucosidase inhibitors
Alpha-glucosidase inhibitors such as acarbose inhibit alpha-glucosidase enzymes in the proximal small intestine to prolong carbohydrate digestion time and thus reduce glucose absorption. They are, however, associated with unsociable gastrointestinal side effects in 20% of patients, which may limit their usage [27].
Creutzfeldt reviewed 18 animal studies examining effects of acarbose on long-term diabetic complications [28]. With regards to retinopathy, acarbose treatment was successful in reducing or preventing diabetic changes in the retina and lens, due to improvements in glycaemic control. This occurred through prevention of basement membrane thickening in retinal capillaries, decreased retinal blood flow rates, reduced aldose reductase activity by over 50% and increasing lenticular protein and glutathione levels (helping to prevent cataract formation). Yang et al. affirmed the reduction in basement membrane thickening and reduced retinopathy development in Zucker Diabetic Fatty rats, but attributed the effect to reduction of hyperglycaemia [29].
Thiazolidinediones
Thiazolidinediones (TZD) are peroxisome proliferator-activated receptor agonists that alter transcription of genes regulating glucose and lipid metabolism and reduce insulin resistance in adipose tissue, muscle and liver [30]. They have been equivocally linked with increased risk of developing or worsening DME, potentially by increasing endothelial cell permeability and increasing systemic VEGF levels [31] (Table 2). Experimental research has noted mechanisms by which TZDs may protect retinal vasculature. Pioglitazone normalised insulin signalling by reducing TNF-alpha and suppressor-of-cytokine-signalling-3 (SOCS3) levels, restored insulin-growth-factor-binding-protein-3 (IGFBP-3) levels and elicited dilatation of retinal arterioles [32,33,34]. Rosiglitazone attenuated diabetes-induced apoptosis in retinal neurons [35], but did not inhibit basement membrane thickening or block increases in VEGF in ocular fluid [36]. TZDs may also attenuate pathological retinal microvessel formation by modulating TNF-alpha production [37] and inhibit retinal leukostasis and leakage in rats [38].
A 2005 case study first reported development of reversible DME with vision loss in a patient taking rosiglitazone [39]. This was followed by Ryan et al. who carried out a non-controlled, non-randomised, retrospective chart review of 30 T2D patients using a TZD and with CSME and lower limb peripheral oedema that had increased since starting TZDs [31]. DME slowly resolved following cessation of TZD and many required laser therapy, hence the study concluded with the impression that fluid retention associated with TZD use could aggravate DME in susceptible patients.
Since then, similar findings have been observed in a cohort study of 996 new cases of DME from the Diabetes Case Identification Database in which TZD users were more likely to develop DME, even after adjusting for age, glycaemic control and insulin use [40]. The largest and most recent study was a retrospective cohort study of 103,368 patients using The Health Improvement Network database which found an increased risk of DME in TZD users at 1 year (OR 2.3) that persisted at 10-year follow-up [41]. However, limitations of the study including under-ascertainment of early-onset DME and not controlling for confounding factors mean clear conclusions from these findings are somewhat indeterminate [42]. Concerns have also been raised from drug safety reviews, as a 2008 review of TZD safety profiles found DME was a common side effect [43]. A 2012 review of adverse drug reactions in the US FDA Adverse Event Reporting system found significantly more frequent reports of MI, fractures and DME associated with TZD compared with other anti-hyperglycaemic agents, and rosiglitazone use was associated with DME (ROR 3.88) [44].
Other studies have examined the effects of TZDs on retinopathy, with possible adverse results. A longitudinal medical record review found 59% relative risk reduction in progression to PDR over 3 years and lower rates of visual acuity loss with rosiglitazone [45]. A community-based study of 1304 patients on rosiglitazone vs 5385 control patients found rosiglitazone use was associated with increased rates of laser treatment and vitrectomy after a median 3.6 years follow-up [46]. Finally, a 16-week prospective randomised control study of 50 patients assigned to rosiglitazone, pioglitazone or control found TZD use was associated with decreased mediators of endothelial dysfunction, reduced markers of inflammation but increased markers of angiogenic activity, which could be of concern in PDR [47].
In contrast, smaller population-based studies have demonstrated no association between TZD and DME. Studies using OCT measurement have revealed no evidence of fluid retention in the macula and no difference in central retinal thickness [48,49,50]. Moreover, the ACCORD Eye study observed no association between TZD exposure and DME but could not exclude modest protective or harmful associations [51]. A 2013 literature review of drugs associated with DME concluded no definite association could be drawn between its incidence and TZD use [52], and that at-risk individuals, such as those with a history of DME and subgroup of nephropathy and/or congestive heart failure needed further study.
Thus, while TZD has not been proven to have a causal relationship with DME, evidence suggests there is likely an association and caution is advised in prescribing its use in those with greater risk of developing DME.
Sulfonylureas
Sulfonylureas are insulin secretagogues that bind to sulfonylurea receptors in pancreatic β-cells, leading to closing of KATP channels and subsequent insulin release [53].
There was a paucity of recent articles on the effects of sulfonylureas on retinopathy. A comparative study of gliclazide vs. glibenclamide in 25 non-insulin-dependent diabetic patients found that gliclazide might be more effective in improving DR or preventing its progression [54] (Table 2). A long-term comparative clinical trial of gliclazide with 159 patients with early or no retinopathy supported the finding that gliclazide appeared to have additional protective properties compared with other sulfonylurea drugs [55]. However, a prospective double-blinded controlled 2-year study comparing gliclazide versus placebo in insulin-treated and gliclazide versus glibenclamide in non-insulin-treated diabetic subjects did not support any action of gliclazide on diabetic microangiopathy independent of its hypoglycaemic actions [56].
Biguanides
Metformin has demonstrated cardioprotective effects independent of glycaemic control [57]. It produces anti-inflammatory and anti-angiogenic effects by increasing levels of thrombospondin-1 which decreases concentrations and activity of plasminogen activator inhibitor-1 and subsequently increases fibrinolytic activity. As inflammation and angiogenesis are implicated in the progression of retinopathy, metformin may have protective effects against retinopathy, though its effects separate to glycaemic control has yet to be investigated [57]. Retrospective chart reviews suggest metformin may have protective effects on DR [58, 59].
Discussion
This review of anti-hyperglycaemic medications used in T2D focuses on newer agents and specifically examines their relationship with diabetic eye complications. There were few well-conducted prospective studies looking at the relationship between anti-hyperglycaemic agents and the progression or regression of DR. It is difficult to determine whether the effect on DR or DME is mediated through improvement in glycaemic control or by direct impact of these anti-hyperglycaemic agents on retinal vasculature. This is also confounded by the possibility of early worsening of DR with rapid lowering of glucose levels on introduction of these medications, before the beneficial effects of improved glycaemic control on microvascular complications become manifested [9, 10, 60]. Most of the evidence consisted of small case studies or experimental studies commenting on benefit or harm associated with medication use. Furthermore, there was a significant paucity of information on the relationship between the older agents (biguanides and sulfonylureas) and retinopathy, with most research from the 1980s. There were also few population-based studies carried out on alpha-glucosidase inhibitors, DPP4-inhibitors and SGLT-2 inhibitors, likely due to DPP4-inhibitors and SGLT-2 inhibitors being recently introduced medications, and the decline in use of alpha-glucosidase inhibitors.
Newer agents such as DPP4-inhibitors, GLP-1 agonists and SGLT-2 inhibitors have been increasingly utilised in combination with established treatment such as metformin due to their relative safety and separate mechanism of actions. The GLP-1 agonists are also notable as the only non-oral anti-hyperglycaemic agents for T2D and have the option of once-weekly dosage via subcutaneous injections.
The undesirable side effects of alpha-glucosidase inhibitors have contributed to their unpopularity, with 25–45% discontinuing use due to side effects [61]. However, a multinational observational study of 15,661 patients of which 92.6% were of Asian background (predominantly from China, South Korea, and India) found that acarbose was effective regardless of presence of cardiovascular comorbidities or diabetic complications, had 84.9% of patients who reported ‘good’ or ‘very good’ tolerability of the drug, and only 3.13% of patients reported adverse events, mainly gastrointestinal [62]. A meta-analysis of 46 studies has also suggested that acarbose may be more efficacious with an Eastern diet compared with a Western diet, raising the possibility for its greater use amongst Asian populations [63]. This may be relevant given the increasing prevalence of DR and DME in Asian populations.
The beneficial effect of tight glycaemic control in reducing risk of microvascular diabetic complications has been established since the UKPDS, particularly with retinopathy, and has since been affirmed by other studies [64]. In addition, the Steno-2 study showed intensive therapy significantly reduced risk of retinopathy by about 60% in T2D patients with microalbuminuria, supporting an aim of tight glucose control [65]. It should be highlighted that evidence of benefit is stronger in younger patients at early stages of disease, whereas effects of tight blood sugar control are weaker once complications have manifested, and hence this should be initiated as early as possible [66].
TZD have repeatedly been associated with increased risk of DME, but further studies must be conducted to determine the nature of the relationship. The reported incidence is rare, at around 1.5–2.6% of patients on TZD [31]. In most cases, cessation of TZD was followed by improvement of the DME although most patients required laser therapy as well. The cardiovascular safety concerns raised regarding TZDs have also led to the decline in their use, in addition to other concerns of increased fracture risk and lower limb oedema.
Other reviews have looked at the relationship between anti-hyperglycaemic medications and nephropathy as another diabetic microvascular complication. In contrast to retinopathy, there are greater restrictions on selection of anti-hyperglycaemic agents in diabetic nephropathy dependent on severity of impaired renal function. Albuminuria alone does not contraindicate use of anti-hyperglycaemic agents, but guidelines suggest contraindication of metformin at GFR <30 ml/min, acarbose <25 ml/min, DPP4 inhibitors <50 ml/min (except for Linagliptin which is safe even for dialysis patients), exenatide <30 ml/min, liraglutide <60 ml/min and sulfonylureas <30 ml/min [65]. This, however, is more likely due to the risk of lactic acidosis in the case of metformin and mechanisms of drug clearance leading to unpredictable pharmacodynamics, rather than specific effects of the agents on renal function itself. Nonetheless, there is still little data on reduction in microalbuminuria with specific anti-hyperglycaemic drugs.
In summary, we reviewed the literature on anti-hyperglycaemic agents and found that apart from thiazolidinediones and one of the GLP-1 agonists, semaglutine, anti-hyperglycaemics have been reported to have beneficial or neutral effects on diabetic eye complications. Thiazolidinediones, of which the only one used in the United Kingdom is pioglitazone, have been linked to incident or worsening DME, although the rate is believed to be low. A detailed medication history may uncover use of this potentially reversible cause of DME. In addition, in the future with large cardiovascular studies mandated for all new anti-hyperglycaemic agents, it may be worthwhile to include the effects on progression of retinopathy as another endpoint to provide further information about the relationship between these agents and development or progression of retinopathy. The phenomenon of early worsening of retinopathy with tight glycaemic control should also be noted in further studies on the effects of anti-hyperglycaemic agents on retinopathy.
References
White JR. A brief history of the development of diabetes medications. Diabetes Spectr. 2014;27:82–6.
Quianzon CC, Cheikh IE. History of current non-insulin medications for diabetes mellitus. J Community Hosp Intern Med Perspect. 2012;2. https://doi.org/10.3402/jchimp.v3402i3403.19081.
Drucker DJ, Nauck MA. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet. 2006;368:1696–705.
Grossman SS. Pathophysiological and pharmacological rationale for the use of exenatide once weekly in patients with type 2 diabetes. Adv Ther. 2014;31:247–63.
Sarao V, Veritti D, Lanzetta P. Regression of diabetic macular edema after subcutaneous exenatide. Acta Diabeta. 2014;51:505–8.
Brooks AM, Lissett CA. A dramatic deterioration in diabetic retinopathy with improvement in glycated haemoglobin (HbA(1c)) on exenatide treatment. Diabet Med. 2009;26:190.
Varadhan L, Humphreys T, Hariman C, Walker AB, Varughese GI. GLP-1 agonist treatment: implications for diabetic retinopathy screening. Diabetes Res Clin Pr. 2011;94:e68–71.
Varadhan L, Humphreys T, Walker AB, Varughese GI. The impact of improved glycaemic control with GLP-1 receptor agonist therapy on diabetic retinopathy. Diabetes Res Clin Pr. 2014;103:e37–9.
Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jódar E, Leiter LA, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375:1834–44.
DCCT DCaCTRG. Early worsening of diabetic retinopathy in the diabetes control and complications trial. Arch Ophthal. 1998;116:874–86.
Simo R, Hernandez C. GLP-1R as a target for the treatment of diabetic retinopathy: friend or foe? Diabetes. 2017;66:1453–60.
Coon SA, Crannage EF, Kerwin LC, Guyton JE. Semaglutide once-weekly: improved efficacy with a new safety warning. Expert Rev Clin Pharm. 2018;11:1061–72.
Dicembrini I, Nreu B, Scatena A, Andreozzi F, Sesti G, Mannucci E, et al. Microvascular effects of glucagon-like peptide-1 receptor agonists in type 2 diabetes: a meta-analysis of randomized controlled trials. Acta Diabetol. 2017;54:933–41.
Pang B, Zhou H, Kuang H. The potential benefits of glucagon-like peptide-1 receptor agonists for diabetic retinopathy. Peptides. 2018;100:123–6.
Zhang Y, Zhang J, Wang Q, Lei X, Chu Q, Xu GT, et al. Intravitreal injection of exendin-4 analogue protects retinal cells in early diabetic rats. Invest Ophthalmol Vis Sci. 2011;52:278–85.
Fan Y, Liu K, Wang Q, Ruan Y, Ye W, Zhang Y. Exendin-4 alleviates retinal vascular leakage by protecting the blood–retinal barrier and reducing retinal vascular permeability in diabetic Goto-Kakizaki rats. Exp Eye Res. 2014;127:104–16.
Hernandez C, Bogdanov P, Corraliza L, Garcia-Ramirez M, Sola-Adell C, Arranz JA, et al. Topical administration of GLP-1 receptor agonists prevents retinal neurodegeneration in experimental diabetes. Diabetes. 2016;65:172–87.
Goncalves A, Leal E, Paiva A, Teixeira Lemos E, Teixeira F, Ribeiro CF, et al. Protective effects of the dipeptidyl peptidase IV inhibitor sitagliptin in the blood-retinal barrier in a type 2 diabetes animal model. Diabetes Obes Metab. 2012;14:454–63.
Goncalves A, Marques C, Leal E, Ribeiro CF, Reis F, Ambrosio AF, et al. Dipeptidyl peptidase-IV inhibition prevents blood-retinal barrier breakdown, inflammation and neuronal cell death in the retina of type 1 diabetic rats. Biochem Biophys Acta. 2014;1842:1454–63.
Maeda S, Yamagishi S, Matsui T, Nakashima S, Ojima A, Maeda S, et al. Beneficial effects of vildagliptin on retinal injury in obese type 2 diabetic rats. Ophthalmic Res. 2013;50:221–6.
Chung YR, Park SW, Kim JW, Kim JH, Lee L. Protective effects of dipeptidyl peptidase-4 inhibitors on progression of diabetic retinopathy in patients with type 2 diabetes. Retina. 2016;36:2357–63.
Kim NH, Choi J, Kim NH, Choi KM, Baik SH, Lee J, et al. Dipeptidyl peptidase-4 inhibitor use and risk of diabetic retinopathy: a population-based study. Diabetes Metab. 2018;44:361–7.
Goring S, Hawkins N, Wygant G, Roudaut M, Townsend R, Wood I, et al. Dapagliflozin compared with other oral anti‐diabetes treatments when added to metformin monotherapy: a systematic review and network meta‐analysis. Diabetes Obes Metab. 2014;16:433–42.
Bailey CJ, Gross JL, Pieters A, Bastien A, List JF. Effect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with metformin: a randomised, double-blind, placebo-controlled trial. Lancet. 2010;375:2223–33.
Takakura S, Toyoshi T, Hayashizaki Y, Takasu T. Effect of ipragliflozin, an SGLT2 inhibitor, on progression of diabetic microvascular complications in spontaneously diabetic Torii fatty rats. Life Scis. 2016;147:125–31.
Yoshizumi H, Ejima T, Nagao T, Wakisaka M. Recovery from diabetic macular edema in a diabetic patient after minimal dose of a sodium glucose co-transporter 2 inhibitor. Am J Case Rep. 2018;19:462–6.
Cheng AYY, Fantus IG. Oral antihyperglycemic therapy for type 2 diabetes mellitus. CMAJ. 2005;172:213–26.
Creutzfeldt W. Effects of the alpha-glucosidase inhibitor acarbose on the development of long-term complications in diabetic animals: pathophysiological and therapeutic implications. Diabetes Metab Res Rev. 1999;15:289–96.
Yang YS, Danis RP, Peterson RG, Dolan PL, Wu YQ. Acarbose partially inhibits microvascular retinopathy in the Zucker Diabetic Fatty rat (ZDF/Gmi-fa). J Ocul Pharm Ther. 2000;16:471–9.
Hauner H. The mode of action of thiazolidinediones. Diabetes Metab Res Rev. 2002;18(S2):S10–5.
Ryan EH Jr, Han DP, Ramsay RC, Cantrill HL, Bennett SR, Dev S, et al. Diabetic macular edema associated with glitazone use. Retina. 2006;26:562–70.
Jiang Y, Thakran S, Bheemreddy R, Ye EA, He H, Walker RJ, et al. Pioglitazone normalizes insulin signaling in the diabetic rat retina through reduction in tumor necrosis factor alpha and suppressor of cytokine signaling 3. J Biol Chem. 2014;289:26395–405.
Thakran S, Zhang Q, Morales-Tirado V, Steinle JJ. Pioglitazone restores IGFBP-3 levels through DNA PK in retinal endothelial cells cultured in hyperglycemic conditions. Invest Ophthalmol Vis Sci. 2015;56:177–84.
Omae T, Nagaoka T, Tanano I, Yoshida A. Pioglitazone, a peroxisome proliferator–activated receptor-γ agonist, induces dilation of isolated porcine retinal arterioles: role of nitric oxide and potassium. Channels Invest Opthalmol Vis Sci. 2011;52:6749–56.
Li P, Xu X, Zheng Z, Zhu B, Shi Y, Liu K. Protective effects of rosiglitazone on retinal neuronal damage in diabetic rats. Curr Eye Res. 2011;36:673–9.
Bosco AA, Lerario AC, Santos RF, Wajchenberg BL. Effect of thalidomide and rosiglitazone on the prevention of diabetic retinopathy in streptozotocin-induced diabetic rats. [Erratum appears in Diabetologia. 2004;47:963]. Diabetologia. 2003;46:1669–75.
Higuchi A, Ohashi K, Shibata R, Sono-Romanelli S, Walsh K, Ouchi N. Thiazolidinediones reduce pathological neovascularization in ischemic retina via an adiponectin-dependent mechanism. Arterioscler Thromb Vasc Biol. 2010;30:46–53.
Muranaka K, Yanagi Y, Tamaki Y, Usui T, Kubota N, Iriyama A, et al. Effects of peroxisome proliferator-activated receptor gamma and its ligand on blood-retinal barrier in a streptozotocin-induced diabetic model. Invest Ophthalmol Vis Sci. 2006;47:4547–52.
Colucciello M. Vision loss due to macular edema induced by rosiglitazone treatment of diabetes mellitus. Arch Ophthalmol. 2005;123:1273–5.
Fong DS, Contreras R. Glitazone use associated with diabetic macular edema. Am J Ophthalmol. 2009;147:583–6.e1.
Idris I, Warren G, Donnelly R. Association between thiazolidinedione treatment and risk of macular edema among patients with type 2 diabetes. Arch Intern Med. 2012;172:1005–11.
Singh S, Segal JB. Thiazolidinediones and macular edema: comment on “Association between thiazolidinedione treatment and risk of macular edema among patients with type 2 diabetes”. Arch Intern Med. 2012;172:1011–3.
Rizos CV, Elisaf MS, Mikhailidis DP, Liberopoulos EN. How safe is the use of thiazolidinediones in clinical practice? Expert Opin Drug Saf. 2009;8:15–32.
Motola D, Piccinni C, Biagi C, Raschi E, Marra A, Marchesini G, et al. Cardiovascular, ocular and bone adverse reactions associated with thiazolidinediones: a disproportionality analysis of the US FDA adverse event reporting system database. Drug Saf. 2012;35:315–23.
Shen LQ, Child A, Weber GM, Folkman J, Aiello LP. Rosiglitazone and delayed onset of proliferative diabetic retinopathy. Arch Ophthalmol. 2008;126:793–9.
Shani M, Feldman L, Kaiserman I, Dresner J, Baevsky T, Vinker S. Is rosiglitazone use associated with an increase in intensive eye treatment in diabetic patients? A community based study. Eur J Gen Pr. 2011;17:205–9.
Vijay SK, Mishra M, Kumar H, Tripathi K. Effect of pioglitazone and rosiglitazone on mediators of endothelial dysfunction, markers of angiogenesis and inflammatory cytokines in type-2 diabetes. Acta Diabetol. 2009;46:27–33.
Tarbett AK, VanRoekel RC, Howard RS, Vigersky RA. The use of optical coherence tomography to determine the effect of thiazolidinediones on retinal thickness in patients with type 2 diabetes. J Diabetes Sci Technol. 2011;5:945–51.
Azar S, El-Mollayess GM, Al Shaar L, Salti HI, Bashshur ZF. Impact of thiazolidinediones on macular thickness and volume in diabetic eyes. Can J Ophthalmol. 2013;48:312–6.
Tatti P, Arrigoni F, Longobardi A, Costanza F, Di Blasi P, Merante D. Retrospective analysis of rosiglitazone and macular oedema in patients with type 2 diabetes mellitus. Clin Drug Invest. 2008;28:327–32.
Ambrosius WT, Danis RP, Goff DC Jr., Greven CM, Gerstein HC, Cohen RM, et al. Lack of association between thiazolidinediones and macular edema in type 2 diabetes: the ACCORD eye substudy. Arch Ophthalmol. 2010;128:312–8.
Makri OE, Georgalas I, Georgakopoulos CD. Drug-induced macular edema. Drugs. 2013;73:789–802.
Ashcroft FM. Mechanisms of the glycaemic effects of sulfonylureas. Horm Metab Res. 1996;28:456–63.
Minami N, Ikeda Y, Abe M. Preventive and therapeutic effects of gliclazide on diabetic retinopathy: comparison with glibenclamide treatment. Tohoku J Exp Med. 1983;141(Suppl):707–11.
Akanuma Y, Kosaka K, Kanazawa Y, Kasuga M, Fukuda M, Aoki S. Long-term comparison of oral hypoglycemic agents in diabetic retinopathy. Gliclazide vs. other sulfonylureas. Diabetes Res Clin Pr. 1988;5:81–90.
Jerums G, Murray RM, Seeman E, Cooper ME, Edgley S, Marwick K, et al. Lack of effect of gliclazide on early diabetic nephropathy and retinopathy: a two-year controlled study. Diabetes Res Clin Pr. 1987;3:71–80.
Silva PS, Cavallerano JD, Sun JK, Aiello LM, Aiello LP. Effect of systemic medications on onset and progression of diabetic retinopathy. Nat Rev Endocrinol. 2010;6:494–508.
Li Y, Ryu C, Munie M, Noorulla S, Rana S, Edwards P, et al. Association of metformin treatment with reduced severity of diabetic retinopathy in type 2 diabetic patients. J Diabetes Res. 2018;2018:2801450.
Maleskic S, Kusturica J, Gusic E, Rakanovic-Todic M, Secic D, Burnazovic-Ristic L, et al. Metformin use associated with protective effects for ocular complications in patients with type 2 diabetes—observational study. Acta Med Acad. 2017;46:116–23.
Dahl-Jørgensen K, Brinchmann-Hansen O, Hanssen K, Sandvik L, Aagenaes O. Rapid tightening of blood glucose control leads to transient deterioration of retinopathy in insulin dependent diabetes mellitus: the Oslo study. Br Med J (Clin ResEd). 1985;290:811–5.
Lillioja S. Diabetes: assessment, therapeutics and management. Liverpool: Diabetes Centre Liverpool Health Service; 2016. p. 34.
Zhang W, Kim D, Philip E, Miyan Z, Barykina I, Schmidt B, et al. A multinational, observational study to investigate the efficacy, safety and tolerability of acarbose as add-on or monotherapy in a range of patients: the GlucoVIP study. Clin Drug Invest. 2013;33:263–74.
Zhu Q, Tong Y, Wu T, Li J, Tong N. Comparison of the hypoglycemic effect of acarbose monotherapy in patients with type 2 diabetes mellitus consuming an Eastern or Western diet: a systematic meta-analysis. Clin Ther. 2013;35:880–99.
Hemmingsen B, Lund SS, Gluud C, Vaag A, Almdal T, Hemmingsen C, et al. Intensive glycaemic control for patients with type 2 diabetes: systematic review with meta-analysis and trial sequential analysis of randomised clinical trials. BMJ. 2011;343:d6898.
Tschöpe D, Hanefeld M, Meier JJ, Gitt AK, Halle M, Bramlage P, et al. The role of co-morbidity in the selection of antidiabetic pharmacotherapy in type-2 diabetes. Cardiovasc Diabetol. 2013;12:1.
Scheen A, Charbonnel B. Effects of glucose-lowering agents on vascular outcomes in type 2 diabetes: a critical reappraisal. Diabetes Metab. 2014;40:176–85.
Dietrich N, Kolibabka M, Busch S, Bugert P, Kaiser U, Lin J, et al. The DPP4 inhibitor linagliptin protects from experimental diabetic retinopathy. PloS One. 2016;11:e0167853.
Chakrabarti S, Varghese Cherian P, Sima AAF. The effect of acarbose on diabetes- and age-related basement membrane thickening in retinal capillaries of the BBW-rat. Diabetes Res Clin Pr. 1993;20:123–8.
Takagi C, King GL, Clermont AC, Cummins DR, Takagi H, Bursell S-E. Reversal of abnormal retinal hemodynamics in diabetic rats by acarbose, an α-glucosidase inhibitor. Curr Eye Res. 1995;14:741–9.
Cohen-Melamed E, Nyska A, Pollack A, Madar Z. Aldose reductase (EC 1.1.1.21) activity and reduced-glutathione content in lenses of diabetic sand rats (Psammomys obesus) fed with acarbose. Br J Nutr. 2007;74:607–15.
Nyssen V, Hautenauven F, Lekeu Hinostroza JP, Guagnini AP. Diabetic edematous maculopathy associated with rosiglitazone treatment: report of a case. Bull Soc Belg Ophthalmol. 2009;313:39–44.
Oshitari T, Asaumi N, Watanabe M, Kumagai K, Mitamura Y. Severe macular edema induced by pioglitazone in a patient with diabetic retinopathy: a case study. Vasc Health Risk Manag. 2008;4:1137–40.
Liazos E, Broadbent DM, Beare N, Kumar N. Spontaneous resolution of diabetic macular oedema after discontinuation of thiazolidenediones. Diabet Med. 2008;25:860–2.
Cusi K, Consoli A, Defronzo RA. Metabolic effects of metformin on glucose and lactate metabolism in noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab. 1996;81:4059–67.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Saw, M., Wong, V.W., Ho, IV. et al. New anti-hyperglycaemic agents for type 2 diabetes and their effects on diabetic retinopathy. Eye 33, 1842–1851 (2019). https://doi.org/10.1038/s41433-019-0494-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-019-0494-z
This article is cited by
-
Effects of newer-generation anti-diabetics on diabetic retinopathy: a critical review
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Incretins and microvascular complications of diabetes: neuropathy, nephropathy, retinopathy and microangiopathy
Diabetologia (2023)
-
Management of Hyperglycemia in Older Adults with Type 2 Diabetes
Drugs & Aging (2022)
-
Comment on “New anti-hyperglycaemic agents for type 2 diabetes and their effects on diabetic retinopathy”
Eye (2021)
-
Subpopulation Differences in the Cardiovascular Efficacy of Long-Acting Glucagon-Like Peptide 1 Receptor Agonists in Type 2 Diabetes Mellitus: A Systematic Review and Meta-analysis
Diabetes Therapy (2020)