Abstract
Background/Objectives
The objective of this study is to compare the long-term outcomes of bilateral and unilateral medial rectus (BMR/UMR) resection for recurrent exotropia after bilateral lateral rectus (BLR) recession.
Subjects/Methods
Retrospective study was performed of 99 patients who underwent BMR resection (BMR group) or UMR resection (UMR group) for recurrent exotropia of 20–30 prism diopters (PD), with a minimum follow-up of 5 years. Surgical outcomes including success rate, exodrift rate, and average effect of MR resection were compared between two groups. The risk factors associated with poor outcomes were evaluated.
Results
At 5 years after surgery, 57% in the BMR group and 62% in the UMR group showed successful outcome. Success and recurrence rates were not significantly different between two groups, whereas the overcorrection rate was significantly higher in the BMR group (35% vs. 15%; p = 0.039). The average effect of MR resection was significantly greater after BMR throughout the whole postoperative period. The average effect of UMR resection was significantly greater in those who had previously undergone a large amount of BLR recession compared with those with a smaller dosage (p = 0.006). By multivariate analysis, a large amount of previous BLR recession and initial overcorrection of >10 PD of esotropia were found to be significant risk factors of overcorrection.
Conclusion
In moderate angles of recurrent exotropia, large UMR resection is a safe and efficient procedure. However, if a large BLR recession was performed previously, surgical dosage for UMR resection should be reduced because of the high risk of long-term overcorrection.
Similar content being viewed by others
Introduction
Recurrence after surgery for intermittent exotropia is relatively common. The recurrence rates vary from 22% to 59%, and up to 30% of patients require more than one surgery to maintain ocular alignment [1,2,3]. The second surgery for recurrent exotropia depends on the previous surgery undertaken [4, 5]. Bilateral medial rectus (BMR) resection is commonly used to treat patients who underwent bilateral lateral rectus (BLR) recession as the primary surgery [5]. Unilateral MR (UMR) resection may be another option for small-to-moderate angles of recurrent exotropia with the advantage of requiring less surgical and anesthesia time, placing only one eye at the risk of possible complications, and preserving the fellow muscle for future use [6,7,8].
To date, there is scarce evidence in the literature determining long-term outcomes of BMR resection and/or UMR resection in recurrent exotropia [7, 9]. Luk et al. [10] and Kim et al. [11] evaluated surgical outcomes of BMR and UMR resection in recurrent exotropia; however, only a small number of patients were included in those studies with short durations of follow-up periods. In our previous study, we compared the two procedures and reported that UMR resection can be a safe and effective procedure in small-to-moderate angles of recurrent exotropia ranging from 14 to 25 prism diopters (PD), but it was relatively a short-term result [12]. In the current study, we compared the long-term surgical outcomes over more than 5 years after BMR and UMR resection for the treatment of moderate angles of recurrent exotropia, and investigated the risk factors associated with poor surgical outcomes after reoperation.
Materials and methods
A retrospective review of medical records was performed on 99 patients who underwent BMR or UMR resection for recurrent exotropia of 20–30 PD between November 2004 and December 2012 at Seoul National University Bundang Hospital by a single experienced surgeon (J-MH). The minimum required follow-up period after reoperation was 5 years. All patients had previously undergone BLR recession for intermittent or constant exotropia by the same surgeon. Patients with paralytic or restrictive strabismus, ocular disease other than strabismus, and systemic disorders such as congenital anomalies or neurologic disorders were excluded. Patients who had moderate to severe amblyopia were also excluded in this study. The study protocol was approved by the Institutional Review Board of Seoul National University Bundang Hospital and adhered to the tenets of the Declaration of Helsinki.
Preoperative ophthalmologic examination
The angle of deviation was measured by prism and alternate cover test at distance (6 m) and near (1/3 m) with refractive correction. Refractive errors were measured by cycloplegic refraction and analyzed as spherical equivalent values. Anisometropia was defined as a spherical equivalent difference of >1.5 diopters (D) between two eyes. Amblyopia was defined as a difference of two lines or more between monocular visual acuities. Lateral incomitance was defined as a change of 5 PD or more in lateral gaze. Sensory status was evaluated using the Randot stereoacuity test (Stereo Optical Company, Inc., Chicago, IL) in cooperative patients. Good stereoacuity was defined as 100 arcsec or better.
Intraoperative procedures
All surgeries were performed under general anesthesia using the same surgical table by a single experienced surgeon (J-MH). BMR resection was performed based on the largest angle of preoperative deviation measured at distance or near, whereas, UMR resection was performed by a uniform surgical dose of 10 mm for patients with 20 PD or more exotropia. A uniform 10 mm of UMR resection was performed for recurrent exotropia of 20–30 PD, as this was considered safe without causing significant limitation of abduction and long-term overcorrection [12]. The surgical dosage is presented in Table 1.
Postoperative measurements
Postoperative angle of deviation at distance in the primary position was noted at 1 month, 6 months, 1 year, 2, 3, and 5 years postoperatively and afterwards. Sensory status was evaluated with the same manner as the preoperative examination. Patients with diplopia associated with consecutive esotropia underwent alternating full-time patching for 1–4 weeks until diplopia resolved. If the esotropia did not resolve with patching in 4 weeks, base-out prism glasses were prescribed until the esotropia resolved [13, 14].
Main outcome measures
Primary outcome measures included the final success rate and the improvement of stereopsis at 5 years after reoperation. The risk factors associated with recurrence and overcorrection were evaluated. Successful surgical outcome was defined as exodeviation <10 PD or esodeviation <5 PD. Exodeviation of 10 PD or more was defined as undercorrection and esodeviation of 5 PD or more was defined as overcorrection. Improved stereopsis was defined as a decrease of more than two octaves after reoperation [15]. Primary outcomes were compared between two groups.
Secondary outcome measures were exodrift rates and the average effect of MR resection. Exodrift rate was defined as the change of alignment toward exodeviation per year after reoperation. A positive value represents exodeviation and negative value represents esodeviation. The average effect of MR resection was calculated by the average deviation corrected per millimeter of MR resection at each postoperative period.
Surgical analysis
Statistical analysis was performed using SPSS for Window version 22.0 (SPSS, Inc., Chicago, IL, USA). The Student’s t-test, Mann–Whitney U-test, χ2- test, and Fisher’s exact test were used to compare the patients’ characteristics and surgical outcomes. Univariate analysis and multivariate logistic regression were performed to identify the factors affecting surgical outcomes including age at onset, gender, age at surgery, preoperative angle of exodeviation before reoperation, amount of previous BLR recession, best-corrected visual acuity, spherical equivalent, anisometropia, dissociated vertical deviation, oblique dysfunction, lateral incomitance, vertical deviation, stereopsis, and initial postoperative alignment at 1 month after reoperation. P-values of <0.05 were considered to be statistically significant.
Results
Ninety-nine patients were included in this study. Twenty-three patients underwent BMR resection and 76 patients underwent UMR resection for recurrent exotropia. The preoperative characteristics were not significantly different between two groups (Table 2). The mean follow-up period after reoperation was 7.2 ± 2.5 years (range, 5.0–11.5 years) in the BMR group and 6.6 ± 1.1 years (range, 5.2–9.9 years) in the UMR group.
Surgical outcomes
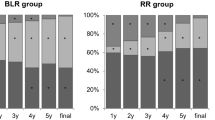
After 5 years of follow-up in the BMR group, 13 (57%) of 23 patients had successful outcome, 2 (9%) had undercorrection, and 8 (35%) had overcorrection. In the UMR group, 47 (62%) of 76 patients had successful outcomes, 18 (24%) had undercorrection, and 11 (15%) had overcorrection (Fig. 1).
Surgical outcomes at postoperative 1 year, 2 years, 3 years, and 5 years in the bilateral medial rectus (BMR) resection group and the unilateral medial rectus (UMR) resection group. After 5 years, the success rate and the undercorrection rate were not significantly different between two groups. However, the overcorrection rate was significantly higher in the BMR group than in the UMR group (35% vs. 15%; p = 0.039). *p < 0.05 by Fisher’s exact test
The undercorrection rate was significantly lower in the BMR group at 2 years after reoperation (p = 0.019; Fisher’s exact test), but did not show any difference at 5 years. One patient (4%) in the BMR group and 16 patients (21%) in the UMR group required a third operation for recurrent exotropia after a mean duration of 3.1 ± 1.1 years from reoperation (p = 0.108).
The overcorrection rate was significantly higher in the BMR group compared with the UMR group at 5 years after reoperation (p = 0.039). At the final follow-up examination after 6.8 ± 1.6 years from reoperation, persistent overcorrection was found in 6 patients (26%) of the BMR group with a mean esodeviation of 9.8 ± 4.4 PD (range, 5–16 PD) and in 9 patients (12%) of the UMR group with a mean esodeviation of 10.7 ± 3.8 PD (range, 6–16 PD). However, all patients maintained fusion and good ocular alignment with prismatic correction. One patient (4%) in the BMR group required a third operation for consecutive esotropia of 30 PD at 1.5 years after reoperation. At the final follow-up examination, seven (9%) patients in the UMR group had lateral incomitance. However, no significant limitation was observed during abduction and no patient reported diplopia on lateral gaze. Possible complications, such as abduction limitation or lateral incomitance, were not significant in both groups at the last follow-up examination.
Stereopsis
Good stereopsis of 100 arcsec or better was found in 78% (18/23) of the BMR group and 86% (65/76) of the UMR group at the last follow-up examination. Improved stereopsis of more than 2 octaves after reoperation was observed in 39% (9/23) of the BMR group and in 34% (26/76) of the UMR group. The incidence of improved stereopsis were not significantly different between two groups (p = 0.703; Fisher’s exact test).
Postoperative exodrift rate
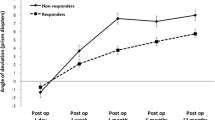
The exodrift rate was most rapid in the first year after reoperation in both groups, which was significantly greater in the BMR group (10.5 ± 7.8 PD/year vs. 5.5 ± 6.5 PD/year; p < 0.001; Mann–Whitney U-test). The exodrift rate significantly decreased after 1 year up to 2 years (3.7 ± 6.1 PD/year vs. 3.3 ± 6.0 PD/year; p = 0.726) in both groups and remained nearly constant after 2 years (0.9 ± 1.2 PD/year vs. 0.5 ± 1.3 PD/year; p = 0.088) (Fig. 2).
Longitudinal changes of postoperative mean angle of deviation at distance in the bilateral medial rectus (BMR) resection group and the unilateral medial rectus (UMR) resection group. The greatest exodrift rate was observed in the first year after reoperation in both groups, which was significantly greater in the BMR group than in the UMR group (10.5 ± 7.8 prism diopters (PD)/year vs. 5.5 ± 6.5 PD/year; p < 0.001). *p < 0.05 by Mann–Whitney U-test
Average effect of MR resection
At 5 years after reoperation, the average effect of MR resection was 2.5 ± 0.9 PD/mm in the BMR group and 1.9 ± 1.1 PD/mm in the UMR group. The average effect of MR resection was significantly greater in the BMR group (p = 0.016; Mann–Whitney U-test).
Analysis of the risk factors for poor surgical outcomes
By multivariate analysis, a large amount of previous BLR recession (p = 0.039) and initial postoperative alignment of >10 PD of esotropia (p = 0.002) were found to be significant risk factors of overcorrection. Age at onset, gender, age at surgery, preoperative deviation before reoperation, best-corrected visual acuity, spherical equivalent, anisometropia, dissociated vertical deviation, oblique dysfunction, lateral incomitance, vertical deviation, and stereopsis were not significantly associated with poor surgical outcome.
Subgroup analysis was performed according to the initial postoperative alignment at 1 month after reoperation. The 5-year success rate was highest in the group with an initial overcorrection of 10 PD esotropia or less. Undercorrection rate was highest in the group with initial orthotropia or exotropia (p < 0.001; Linear-by-linear association). Overcorrection rate was highest in the group with initial overcorrection of >10 PD (p < 0.001) (Supplementary Table 1).
Regarding the amount of previous BLR recession, overcorrection was observed in 41% (7/17) of patients who previously underwent a large BLR recession of 10 mm and 15% (12/82) of patients who underwent a smaller dosage of BLR recession, which was significantly higher in patients who had underwent a large BLR recession previously (p = 0.019; Fisher’s exact test). In particular, when UMR resection was performed as the second operation, the average effect of MR resection was significantly greater in those who had underwent a large BLR recession of 10 mm than those who underwent a smaller dosage (2.7 ± 1.1 PD/mm vs. 1.7 ± 1.0 PD/mm; p = 0.006; Mann–Whitney U-test) (Table 3). The average effect of BMR resection did not differ according to the amount of previous LR surgery, which was similar to the effect of UMR resection after a large BLR recession (p = 0.813).
Discussion
Our study provides important information on performing UMR/BMR resection to treat recurrent exotropia of 20–30 PD after BLR recession. The overcorrection rate was significantly higher after BMR resection compared with UMR resection even after 5 years from reoperation. Long-term results suggest that a large UMR resection is a relatively safe procedure to treat patients with moderate angles of recurrent exotropia, although recurrence may increase with time. However, if a large BLR recession was performed as the first surgery, long-term overcorrection was frequent even after UMR resection.
Success rates have been reported to be 80–95% at 6 months, and 72.7% and 82% at 2 years after UMR resection for recurrent exotropia [5,6,7,8, 16]. Our previous study had shown that UMR resection was an effective procedure in patients with small to moderate angles of recurrent exotropia [12]. The success rates were 54% in the BMR group and 80% in the UMR group after a mean follow-up of 22 months [12]. In this study, the 5-year success rates were 57% in the BMR group and 62% in the UMR group. The relatively low success rate in our study may be mainly due to the long follow-up period and difference in preoperative alignments, and definition of success might also have affected the results.
The exotropic drift after surgery for intermittent exotropia has been reported by many authors. Scott et al. [17] reported that exodrift stabilized in the first 6 weeks after surgery and Hahm et al. [18] noted that exotropic drift was more pronounced during 2 years after surgery. Our study was in close agreement with the previous reports. In both BMR and UMR groups, the greatest amount of exodrift was observed in the first year after reoperation and the exodrift rates stabilized after 2 years postoperatively. One thing to note is that the exodrift rate was significantly greater in the BMR group during the first year after surgery (p < 0.001). The greater exodrift in the first year after BMR resection may be explained by the larger initial overcorrection after BMR resection. Ruttum et al. [19] and Yam et al. [20] found that a large initial overcorrection was associated with a large postoperative exodrift. However, our results show that the effect of initial overcorrection on the rate of exodrift was not significant after 1 year.
In the BMR group, the overcorrection rate was higher at 5 years after surgery and the average effect of MR resection was significantly greater than the UMR group throughout the whole postoperative period. Suh et al. [21] analyzed the difference in the effects between BMR resection and UMR resection for recurrent exotropia. The average effects were 4.1 PD/mm in the BMR group and 4.2 PD/mm in the UMR group at postoperative 1 month, and no significant difference was noted between the two groups [21]. Our study showed different results as the average effects of MR resection were 2.5 ± 0.9 PD/mm in the BMR group and 1.9 ± 1.1 PD/mm in the UMR group at 5 years after reoperation, which was significantly greater in the BMR group (p = 0.016) resulting in a high rate of long-term overcorrection. Therefore, when planning BMR resection for the treatment of recurrent exotropia, one may consider reducing the surgical dosage from the original table.
Various factors have been reported to affect surgical outcomes such as age at surgery, preoperative angle of deviation, lateral incomitance, divergence excess type, amblyopia, anisometropia, and sensory status [22,23,24,25,26,27]. In our study, none of these factors were found to be relevant. On the other hand, patients who previously underwent 10 mm of BLR recession had a greater chance of developing overcorrection after UMR resection as well as BMR resection. In the UMR group, 29% (4/14) of those who underwent a previous BLR recession of 10 mm had persistent overcorrection at the final follow-up examination. Conversely, those who underwent a smaller dosage of BLR recession were relatively safe from overcorrection after UMR resection. The reason is unclear, but after a large BLR recession, the tonus of the lateral rectus muscle may decrease, and as a result, the large amount of antagonist muscle resection may lead to a significant effect. Another possible cause is a structural change in the rectus pulleys. Although shifting horizontal extraocular muscle insertions by 4–7 mm is known to have little effect on pulley positions [28], a large MR resection after 10 mm LR recession may affect the orbital pulley as well as the global pulley, leading to pulley shift. Thus, the amount of previous LR recession should be considered before planning the surgical procedure for UMR resection in recurrent exotropia.
Early postoperative overcorrection of more than 10 PD is known to be a predictive factor of successful outcomes after exotropia surgery [29, 30]. However, in our study, the desirable amount of initial overcorrection was 10 PD or less after BMR/UMR resection for recurrent exotropia. These results may be due to the differences in surgical methods [31] or the difference in exodrift rates between the first operation and reoperation[9].
This study has several limitations. First, because of its retrospective nature, surgical indications and treatment options were not randomized. In addition, as the minimum required follow-up period was relatively long ( ≥5 years after reoperation), selection bias might have occurred. As patients with favorable outcome tend to be lost during follow-up, long-term success rates might be underestimated. Second, in the UMR group, a maximum amount of 10 mm UMR resection was performed on patients with different amount of preoperative deviations ranging from 20 to 30 PD. Despite several limitations, our results are based on a large number of patients with a longer follow-up period compared with the previous studies [6,7,8, 11, 12, 16].
In conclusion, BMR resection was associated with a high risk of long-term overcorrection. A large UMR resection of 10 mm is safe and efficient for moderate angles of recurrent exotropia after BLR recession. However, if a large BLR recession was performed as the first surgery to treat intermittent exotropia, the surgical dosage for UMR resection should be reduced because of the high risk of long-term overcorrection.
Summary
What was known before
Bilateral medial rectus resection for recurrent exotropia is associated with a high risk of overcorrection.
What this study adds
Patients who previously underwent 10 mm of bilateral lateral rectus recession had a greater chance of developing overcorrection after unilateral medial rectus resection as well as bilateral medial rectus resection for recurrent exotropia.
References
Pratt-Johnson J, Barow J, Tillson G. Early surgery in intermittent exotropia. Am J Ophthalmol. 1977;84:689–94.
Kim M, Cho S. Long-term surgical results of intermittent exotropia. J Korean Ophthalmol Soc. 1994;35:1321–6.
Hardesty HH, Boynton JR, Keenan JP. Treatment of intermittent exotropia. Arch Ophthalmol. 1978;96:268–74.
Yazdian Z, Ghiassi G. Re-recession of the lateral rectus muscles in patients with recurrent exotropia. J Am Assoc Pediatr Ophthalmol Strabismus. 2006;10:164–7.
Olitsky SE, Kelley CJ, Lee H, Nelson LB. Unilateral rectus resection in the treatment of undercorrected or recurrent strabismus. J Pediatr Ophthalmol Strabismus. 2001;38:349–53.
Kim SC, Kim MM. The efficacy of unilateral rectus resection in the reoperation of strabismus. J Korean Ophthalmol Soc. 2003;44:904–10.
Mims J 3rd. Outcome of 5 mm resection of one medial rectus extraocular muscle for recurrent exotropia. Binocul Vision Strabismus Q. 2003;18:143.
Chae SH, Chun BY, Kwon JY. The effect of unilateral medial rectus muscle resection in patients with recurrent exotropia. Korean J Ophthalmol. 2008;22:174–7.
Kim EY, Kim HK, Lee SY, Lee YC. Comparison of postoperative exodrift after first unilateral and second contralateral lateral rectus recession in recurrent exotropia. Korean J Ophthalmol. 2016;30:48–52.
Luk AS, Yam JC, Lau HH, Yip WW, Young AL. Surgical outcome of medial rectus resection in recurrent exotropia: a novel surgical formula. J Ophthalmol. 2015;2015:758463.
Kim SJ, Choi DG. The clinical analysis after reoperation for recurrent intermittent exotropia. J Korean Ophthalmol Soc. 2007;48:321–7.
Yang HK, Hwang J-M. Bilateral vs unilateral medial rectus resection for recurrent exotropia after bilateral lateral rectus recession. Am J Ophthalmol. 2009;148:459–65. e451.
Lee EK, Hwang J-M. Prismatic correction of consecutive esotropia in children after a unilateral recession and resection procedure. Ophthalmology. 2013;120:504–11.
Lee EK, Yang HK, Hwang J-M. Long-term outcome of prismatic correction in children with consecutive esotropia after bilateral lateral rectus recession. Br J Ophthalmol. 2015;99:342–5.
Adams WE, Leske DA, Hatt SR, Holmes JM. Defining real change in measures of stereoacuity. Ophthalmology. 2009;116:281–5.
Park DG, Kim WJ, Kim MM. The effect of unilateral medial rectus resection for recurrent intermittent exotropia. J Korean Ophthalmol Soc. 2014;55:1681–6.
Scott WE, Keech R, Mash AJ. The postoperative results and stability of exodeviations. Arch Ophthalmol. 1981;99:1814–8.
Hahm KH, Shin MC, Sohn MA. The change in deviation angle with time course after surgical correction of intermittent exotropia. J Korean Ophthalmol Soc. 2002;43:2214–9.
Ruttum MS. Initial versus subsequent postoperative motor alignment in intermittent exotropia. J Am Assoc Pediatr Ophthalmol Strabismus. 1997;1:88–91.
Yam J, Chong GS, Wu PK, Wong US, Chan CW, Ko ST. Predictive factors affecting the short term and long term exodrift in patients with intermittent exotropia after bilateral rectus muscle recession and its effect on surgical outcome. Biomed Res Int. 2014;2014:82093.
Suh Y-W, Seo I, Cho YA, Kim S-H. Analysis of the effects of medial rectus muscle resection for recurrent exotropia. Korean J Ophthalmol. 2011;25:341–3.
Richard JM, Parks MM. Intermittent exotropia: surgical results in different age groups. Ophthalmology. 1983;90:1172–7.
Abbasoglu OE, Sener EC, Sanac AS. Factors influencing the successful outcome and response in strabismus surgery. Eye. 1996;10:315.
Beneish R, Flanders M. The role of stereopsis and early postoperative alignment in long-term surgical results of intermittent exotropia. Can J Ophthalmol. 1994;29:119–24.
Jang JH, Park JM, Lee SJ. Factors predisposing to consecutive esotropia after surgery to correct intermittent exotropia. Graefe Arch Clin Exp Ophthalmol. 2012;250:1485–90.
Pineles SL, Ela-Dalman N, Zvansky AG, Yu F, Rosenbaum AL. Long-term results of the surgical management of intermittent exotropia. J Am Assoc Pediatr Ophthalmol Strabismus. 2010;14:298–304.
Kim HJ, Choi DG. Consecutive esotropia after surgery for intermittent exotropia: the clinical course and factors associated with the onset. Br J Ophthalmol. 2014;98:871–5.
Clark RA, Demer JL. Magnetic resonance imaging of the effects of horizontal rectus extraocular muscle surgery on pulley and globe positions and stability. Invest Ophthalmol Vis Sci. 2006;47:188–94.
Oh J, Hwang J. Survival analysis of 365 patients with exotropia after surgery. Eye. 2006;20:1268.
Stoller SH, Simon JW, Lininger LL. Bilateral lateral rectus recession for exotropia: a survival analysis. J Pediatr Ophthalmol Strabismus. 1994;31:89–92.
Jeoung JW, Lee MJ, Hwang J-M. Bilateral lateral rectus recession versus unilateral recess-resect procedure for exotropia with a dominant eye. Am J Ophthalmol. 2006;141:683–8.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP) (Number 2017R1A2B4011450).
Financial disclosures
No financial disclosures
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Ethics approval was provided by the Institutional Review Board of Seoul National University Bundang Hospital. All aspects of the research protocol were in compliance with the Declarations of Helsinki.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The author(s) have no proprietary or commercial interest in any materials discussed in this paper.
Supplementary information
Rights and permissions
About this article
Cite this article
Sung, J.Y., Yang, H.K. & Hwang, JM. Long-term surgical outcomes of bilateral vs. unilateral medial rectus resection for recurrent exotropia. Eye 33, 1119–1125 (2019). https://doi.org/10.1038/s41433-019-0379-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-019-0379-1
This article is cited by
-
Clinical factors affecting the rate of exodrift after surgery in patients with basic intermittent exotropia
Scientific Reports (2021)
-
Long term surgical outcomes of unilateral recession-resection versus bilateral lateral rectus recession in basic-type intermittent exotropia in children
Scientific Reports (2021)
-
Risk factors associated with poor outcome after medial rectus resection for recurrent intermittent exotropia
Graefe's Archive for Clinical and Experimental Ophthalmology (2020)