Abstract
Purpose:
To evaluate anatomic and functional outcomes of patients treated with pars plana vitrectomy (PPV) with scleral buckling versus PPV with inferior retinectomy for treatment of cases of primary rhegmatogenous retinal detachment (RRD) associated with proliferative vitreoretinopathy (PVR) and inferior retinal breaks.
Methods:
Retrospective, comparative, interventional, single-center study. Fifty-one eyes of fifty-one patients with primary RRD associated with inferior breaks and PVR grade C1 or more were reviewed over 3 years. Twenty-one eyes underwent PPV with encircling band 360° and thirty eyes underwent PPV with primary inferior retinectomy. The primary outcome was final anatomic success. Secondary outcomes included change in visual acuity, primary anatomical success, the mean number of operations, and incidence of postoperative complications.
Results:
Primary anatomical success of 85.7% was achieved in buckle group compared to 83.3% in retinectomy group (p = 0.82). Mean duration of follow-up and mean number of operations was 9.8 ± 2.26 and 9.97 ± 2.44 months; 1.24 ± 0.62 and 1.3 ± 0.75 in buckle group and retinectomy group, respectively, achieving final anatomical success of 95.2% for the buckle group and 90% for the retinectomy group with no statistical significant difference (p = 0.49). Although visual acuity (logMAR) was better in the buckle group in the 1st month, it became nearly equal thereafter during the follow-up period (p = 0.5).
Conclusion:
Similar anatomical and functional outcomes were achieved by combining PPV with scleral buckle or inferior retinectomy for treatment of primary RRD with PVR and inferior breaks.
Similar content being viewed by others
Introduction
Scleral buckling (SB) and pars plana vitrectomy (PPV) are used either alone or in combination for treatment of rhegmatogenous retinal detachment (RRD) [1]. Many factors are employed in the choice of the surgical approach; one of them is the position of retinal breaks. Inferior breaks are usually a surgical challenge so that surgeons might combine a PPV with SB to produce an inferior indent that supports the inferior retina and overcomes retinal contraction [2].
Proliferative vitreoretinopathy (PVR) is a sort of vitreoretinal wound healing response to a retinal break. A cascade of intraocular inflammation is initiated by the breakdown of the blood–retinal barrier, leading to cellular proliferation, and extracellular matrix remodeling. Pro-inflammatory and fibrotic agents (cells, cytokines, and growth factors) are released in the vitreous cavity and the subretinal fluid that leads to epiretinal, intra-retinal, and subretinal fibrosis, causing recurrence of retinal detachment (RD) [3].
PPV with surgical removal of epiretinal and subretinal proliferation is the only line of treatment in eyes with PVR. Different combinations of relaxing retinectomy and scleral buckle are used in case of retinal shortening due to intraretinal fibrosis [4]. Both scleral buckle and retinectomy were studied separately as a primary treatment for cases with inferior PVR and both achieved good anatomical results [5,6,7,8]. Choosing which technique is still controversial. So, in our study, we compared results of combining PPV with scleral buckling versus PPV with relaxing retinectomy as a primary treatment for patients with RRD associated with PVR and inferior breaks.
Methods
Fifty-one eyes of fifty-one patients with primary RRD were retrospectively enrolled in our study. We included patients with inferior breaks (identified as being within 4 to 8 o’clock meridian) and PVR grade C according to The Retina Society Terminology Committee revised classification [9]. All patients were recruited from Cairo University Hospitals and operated between January 2014 and June 2017. The study adhered to Tenets of Declaration of Helsinki and was approved by the ethical board of Cairo University.
We excluded cases of recurrent retinal detachment, macular pathology (macular hole, retinoschisis, choroidal neovascularization), giant retinal tear, penetrating trauma, ruptured globe, intraocular foreign body, thin staphylomatous sclera, retinopathy of prematurity, persistent fetal vasculature, proliferative diabetic retinopathy, cytomegalovirus retinitis, acute retinal necrosis, endophthalmitis, hereditary arthro-ophthalmopathy and <6 months of follow-up.
Baseline evaluation
Complete ocular examination was done including best available visual acuity (with logMARs conversion), intraocular pressure (IOP) using Goldmann applanation tonometry and anterior segment biomicroscopy. The retinal detachment was evaluated using slit lamp biomicroscopy using (Super Field lens; VOLK, Mentor, Ohio, USA) and indirect ophthalmoscopy determining extent and configuration of the detachment, macula status, number and position of the breaks and grade of PVR.
Surgical procedure
Surgeries were performed by multiple surgeons with the same technique. Phacoemulsification with 3-piece IOL implantation was done in all phakic patients in both groups. PPV was done using 23-gauge system (Constellation system. Alcon, Fort Worth, TX) removing the posterior hyaloid with the aid of triamcinolone. All the epiretinal and subretinal membranes were meticulously dissected and peeled off from the surface of the retina starting from the posterior membranes and extending up anteriorly. Perfluorocarbon is used to flatten the retina. Failure of retinal flattening indicates the presence of intrinsic retinal shortening that cannot be released and requires further intervention either scleral buckle or retinectomy which was chosen according to the surgeon preference. 360° vitreous base shaving with scleral depression was done.
In 21 eyes (Buckle group), 360° encircling silicone band no. 40 (Labtician Ophthalmics Inc, Ontario, Canada) was applied. The band was inserted at the beginning of surgery through four scleral tunnels that were created at the equator of the globe, one at each quadrant, using a crescent knife 2 mm (Mani, Utsunomiya, Japan), secured by Watzke sleeve.
In 30 eyes (Retinectomy group), a relaxing circumferential inferior retinectomy was extended as many clock hours as necessary to relieve all tractions and the anterior retinal shortening. Retinectomy was done using high-speed vitreous cutter after the application of full-thickness retinal cautery. Peripheral non-functioning retina was removed with vitreous cutter to prevent neovascularization and re-proliferation.
ILM peeling was done in all patients to prevent epimacular membrane formation using brilliant blue G stain (ILM-blue, DORC, Zuidland, Netherland). In both groups, laser photocoagulation in three confluent rows was done to all breaks, edge of retinectomy and 360°. Further photocoagulation of the bare area of the choroid in cases of retinectomy was done. Silicone oil (5000 centistokes) was used as tamponading agent (DORC, Zuidland, Netherland) in all cases. No antiproliferative agents were used.
Post PPV evaluation
Full ophthalmological examination was done on day 1, week 1, months 1, 3, and 6 post PPV and included: best-corrected visual acuity (BCVA) by refraction; slit lamp examination, anterior segment biomicroscopy, intraocular pressure using Goldmann applanation tonometry, dilated fundus examination with binocular indirect slit-lamp biomicroscopy. Silicone oil was removed at 3 months.
If retinal redetachment was found during follow-up, a reoperation was scheduled as early as possible to prevent any involvement of the macular area, during which a retinectomy was done to relieve the traction and remove the reproliferation and allow retinal reattachment.
Outcome measurement
Primary outcome measure was final anatomical success, defined as stable complete retinal reattachment without internal tamponade at 6 months post vitrectomy. Secondary outcomes included assessment of primary anatomical success defined as retinal attachment after single operation, mean number of operation required for complete retinal reattachment, best-corrected visual acuity (BCVA), IOP changes, and intraoperative and postoperative complications. Correlation of recurrence of retinal detachment was evaluated in relation to preoperative characteristics.
Statistical analysis
Statistical analysis was done using SPSS computer software package, version 15.0, 2006, Echosoft Corporation, USA. Qualitative data were expressed as frequencies and percentages. Quantitative data were expressed as mean ± standard deviation (SD) for parametric data and median ± interquartile range (IQR) for non-parametric data. Differences between groups were assessed through independent t-test for parametric data and Mann–Whitney U-test for non-parametric data. All tests were two-tailed and considered significant at p < 0.05.
Results
Of the 51 patients identified with inferior breaks and PVR grade C, 66.7% of buckle group and 43.3% of the retinectomy group were males. Mean age was 39.3 ± 11.81 years in buckle group and 44 ± 11.44 years in the retinectomy group. Duration of detachment was 4.6 ± 1.1 weeks in both groups. Regarding the lens status, 62% of buckle group were phakic compared to 60% of the retinectomy group. The baseline characteristics of both groups are summarized in Table 1. Baseline characteristics of the two groups were homogeneous with no significant statistical difference between groups in terms of age, gender, PVR stage, initial BCVA and macular status.
Anatomical outcome
Primary anatomical success of 84.3% (43 eyes) was achieved in our study. After the primary surgery, 14.3% (3 eyes) showed recurrence in buckle group compared to 16.7% (5 eyes) in the retinectomy group (p = 0.82). Mean number of procedures to achieve complete retinal attachment and mean duration of follow-up were 1.24 ± 0.62 and 1.3 ± 0.75 (p = 0 .87); 9.8 ± 2.26 and 9.97 ± 2.44 months, in buckle group and retinectomy group, respectively. Silicone oil was removed at 3 months and final anatomical success was achieved in 92.2% (47 eyes). Final anatomical success was 95.2% for the buckle group and 90% for the retinectomy group with no statistical significant difference (p = 0.49). Recurrence occurred in 4.8% (1 eye) in buckle group due to severe intrinsic retinal shortening and in 10% (3 eyes) in the retinectomy group due to proliferation from the site of the retinectomy in these cases (Table 2).
Secondary outcomes
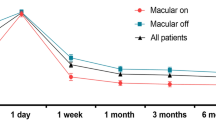
Functional outcome
Visual acuity was significantly better at 1st month in the buckle group with mean BCVA (logMAR) of 0.7 ± 0.41 (equivalent to 20/100 Snellen’s acuity) compared to 0.92 ± 0.42 in retinectomy group (equivalent to 20/160 Snellen’s acuity) (p = 0.036). However, this difference disappeared throughout the remaining follow-up period with final mean BCVA of 0.67 ± 0.37 in buckle group (equivalent to 20/90 Snellen’s acuity) and 0.68 ± 0.61 in retinectomy group (equivalent to 20/100 Snellen’s acuity) (p = 0.5).
Complications
IOP was significantly higher in buckle group during the whole follow-up period with mean of 18.28 ± 2.79 mmHg in buckle group and 15.8 ± 3.87 mmHg in retinectomy group (p = 0.005). However, 7 eyes (33.3%) of buckle group required to be kept on anti-glaucoma medication compared to 8 eyes (26.7%) of retinectomy group and this difference was not statistically significant (p = 0.607).
In the buckle group, buckle-related complications such as scleral perforation, anterior segment ischemia, diplopia, extrusion, or infection did not occur. None of the eyes of retinectomy group developed postoperative hypotony.
Factors correlated with recurrence
Using multiple linear regression to analyze the correlation of surgical technique to recurrence of RD considering preoperative characteristics including age, duration of RD, preoperative vision and lens status, macula status, extent of retinal detachment, only duration of RD was the significant predictor with R square of 0.597 and p value 0.001.
Discussion
Rhegmatogenous retinal detachment complicated with inferior breaks and PVR remains a challenging situation for vitreoretinal surgeons. In order to achieve a successful retinal reattachment, three important factors should be considered: a proper vitrectomy with removal of all proliferative membranes to relief any traction, alteration of intraocular currents by endotamponade (silicone oil) or external tamponade (Scleral buckle), and chorioretinal adhesion either by cryopexy or endophotocoagulation [10]. PPV with silicone oil tamponade is the standard surgical procedure for these cases. The main concern is that silicone oil does not tamponade the inferior quadrant completely. Therefore, PPV could be combined with scleral buckling (SB) to add external tamponading effect and elevate the lower retinal edge or a relaxing inferior retinectomy as described by Machemer 1981 to eliminate inferior traction [11].
PPV with scleral buckle was studied for treatment of inferior retinal breaks and PVR. In a pilot study of 10 eyes with RRD with inferior breaks with PVR ≥ CP2 that underwent PPV, silicone oil and segmental scleral buckle, the primary anatomical success rate was 90% [5]. Similarly, Alexander et al. achieved successful attachment of 95% in 60 eyes having RD with inferior breaks using vitrectomy, gas, and segmental buckle [6]. Although adding scleral buckle achieves satisfactory results, it carries risk of complication such as scleral perforation, choroidal hemorrhage, refractive changes, anterior segment ischemia, infection, buckle erosion, and diplopia [12,13,14,15,16,17].
On the other hand, relaxing retinectomy was studied as a method to relieve the traction and achieve retinal attachment. Sheng et al. retrospectively showed that after complete vitrectomy the residual traction can be treated with retinectomy as a primary procedure which achieved a good anatomical result (87.5%) [7]. Similarly, Tan et al. showed that primary retinectomy without SB had good anatomical results (77.2%) for severe PVR [8]. Both studies showed similar anatomical results to our study (83.3%) but they were not comparative studies as ours.
In our study, we compared PPV with scleral buckle and PPV with retinectomy evaluating anatomical and functional results. Primary success rate was more in scleral buckle group (85.7%) than in retinectomy group (83.3%) but the difference was not statistically significant (p = 0.82). Also, the final anatomical success was more for the buckle group (95.2%) than the retinectomy group (90%) with no statistical significant difference (p = 0.49). Similar to our results but in recurrent cases, Mancino et al. showed that successful attachment for cases with recurrent RD after vitrectomy using inferior retinectomy was higher in cases with previous buckle than cases with previous vitrectomy [18].
In our study, we used standard silicone oil of 5000-centistokes viscosity. Several previous studies were done in order to assess the effectiveness of using standard SO [19,20,21] and heavy silicone oil Oxane Hd® and Densiron 68® for the treatment of complicated RD [22,23,24,25,26] and they had almost equal results. Auriol et al. showed that using heavy silicone oil for treatment of complicated RD with inferior retinectomy achieved total anatomical success of 92.5% at the last follow-up visit that was similar to the previous results reported by standard silicone oil [27].
On evaluating factors affecting recurrence in this study, it was only correlated with the duration of detachment (p = 0.001) rather than surgical technique, age, preoperative vision, or the lens status. Other studies showed that postoperative PVR and recurrence were associated with PVR grade at time of presentation of RD, preoperative vitreous hemorrhage, the presence of choroidal detachment preoperatively, excessive cryotherapy, and repeated surgical procedures [28].
The mean postoperative IOP was significantly higher in buckle group throughout the whole follow-up period. Although hypotony is reported as a devastating complication of retinectomy with an incidence ranging from 11 to 39% [11] none of the eyes in retinectomy group developed hypotony. This could be related to photocoagulation of the bare area of the choroid during PPV to eliminate this fluid absorptive surface responsible for postoperative hypotony.
The current study has few limitations. We had a relatively small sample size, being retrospective and non-randomized. Further research is needed to evaluate and compare different techniques in the management of this specific group of patients and to highlight the causes of recurrence.
In conclusion, rhegmatogenous retinal detachment complicated with inferior breaks and PVR remains a challenging situation for vitreoretinal surgeons. Our study showed similar anatomical and functional outcomes achieved by combining PPV with scleral buckle or inferior retinectomy.
Summary
What was known before
-
Retinal detachment with inferior breaks and PVR is still a surgical challenge. Pars plana vitrectomy with scleral buckle or with retinectomy was studied as a treatment option.
What this study adds
-
Similar anatomical and functional outcome with PPV combined with scleral buckle or retinectomy.
References
Falkner-Radler CI, Graf A, Binder S. Vitrectomy combined with endolaser or an encircling scleral buckle in primary retinal detachment surgery: a pilot study. Acta Ophthalmol. 2015;93:464–9.
Ghoraba HH, Zaky AG, Ellakwa AF. Long-term follow-up of vitrectomy, with or without 360 degrees encircling buckle, for rhegmatogenous retinal detachment due to inferior retinal breaks. Clin Ophthalmol. 2016;10:1145–51.
Leiderman YI, Miller JW. Proliferative vitreoretinopathy: pathobiology and therapeutic targets. Semin Ophthalmol. 2009;24:62–9.
Veckeneer M, Maaijwee K, Charteris DG, van Meurs JC. Deferred laser photocoagulation of relaxing retinotomies under silicone oil tamponade to reduce recurrent macular detachment in severe proliferative vitreoretinopathy. Graefes Arch Clin Exp Ophthalmol. 2014;252:1539–44.
Boscia F, Furino C, Recchimurzo N, Besozzi G, Sborgia G, Sborgia C. Oxane HD vs silicone oil and scleral buckle in retinal detachment with proliferative vitreoretinopathy and inferior retinal breaks. Graefes Arch Clin Exp Ophthalmol. 2008;246:943–8.
Alexander P, Ang A, Poulson A, Snead MP. Scleral buckling combined with vitrectomy for the management of rhegmatogenous retinal detachment associated with inferior retinal breaks. Eye. 2008;22:200–3.
Sheng Y, Sun W, Mo B, Yu YJ, Gu YS, Liu W. Non-buckled vitrectomy for retinal detachment with inferior breaks and proliferative vitreoretinophathy. Int J Ophthalmol. 2012;5:591–5.
Tan HS, Mura M, Oberstein SY, de Smet MD. Primary retinectomy in proliferative vitreoretinopathy. Am J Ophthalmol. 2010;149:447–52.
Hilton G, Machemer R, Michels R, Okun E, Schepens C, Schwartz A. The classification of retinal detachment with proliferative vitreoretinopathy. Ophthalmology. 1983;90:121–5.
Machemer R. The importance of fluid absorption, traction, intraocular currents and chorioretinal scars in the therapy of rhegmatogenous retinal detachments. Am J Ophthalmol. 1984;98:681–93.
Machemer R, McCuen BW 2nd, de Juan E Jr. Relaxing retinotomies and retinectomies. Am J Ophthalmol. 1986;102:7–12.
Goel R, Crewdson J, Chignell AH. Astigmatism following retinal detachment surgery. Br J Ophthalmol. 1983;67:327–9.
Arruga A. Motility disturbances induced by operations for retinal detachment. Mod Probl Ophthalmol. 1977;18:408–14.
Fison PN, Chignell AH. Diplopia after retinal detachment surgery. Br J Ophthalmol. 1987;71:521–5.
Flindall RJ, Norton EW, Curtin VT, GassJD. Reduction of extrusion and infection following episcleral silicone implants and cryopexy in retinal detachment surgery. Am J Ophthalmol. 1971;71:835–7.
Kwartz J, Charles S, McCormack P, Jackson A, Lavin M. Anterior segment ischaemia following segmental scleral buckling. Br J Ophthalmol. 1994;78:409–10.
Ryan SJ, Goldberg MF. Anterior segment ischemia following scleral buckling in sickle cell hemoglobinopathy. Am J Ophthalmol. 1971;72:35–50.
Mancino R, Aiello F, Ciuffoletti E, Di Carlo E, Cerulli A, Nucci C. Inferior retinotomy and silicone oil tamponade for recurrent inferior retinal detachment and grade C PVR in eyes previously treated with pars plana vitrectomy or scleral buckle. BMC Ophthalmol. 2015;15:173.
Gonvers M. Temporary use of silicone oil in the treatment of special cases of retinal detachment. Ophthalmologica. 1983;187:202–9.
Lucke KH, Foerster MH, Laqua H. Long-term results of vitrectomy and silicone oil in 500 cases of complicated retinal detachments. Am J Ophthalmol. 1987;104:624–33.
McCuen BW, Landers MB, Machemer R. The use of silicone oil following failed vitrectomy for retinal detachment. Ophthalmology. 1985;92:1029–34.
Wong D, Van Meurs JC, Stappler T, Groenewald C, Pearce IA, McGalliard JN, et al. A pilot study on the use of a perfluorohexyloctane/silicone oil solution as a heavier than water internal tamponade. Br J Ophthalmol. 2005;89:662–5.
Wolf S, Schon V, Meier P, Wiedemann P. Siliconeoil-RMN3 mixture (Heavy silicone oil) as internal tamponade for complicated retinal detachment. Retina. 2003;23:335–42.
Sandner D, Engelmann K. First experiences with high density silicone oil (Densiron) as intraocular tamponade in complex retinal detachment. Graefes Arch Clin Exp Ophthalmol. 2006;244:609–19.
Sandner D, Herbrig E, Engelmann K. High-silicone oil (Densiron) as a primary intraocular tamponade: 12-month followup. Graefes Arch Clin Exp Ophthalmol. 2007;245:1097–105.
Pagot-Mathis V, Benouaich X, Mathis A, Rico-Lates I. DumoulinA Tamponnement interne par huile de silicone loured (Oxane Hd®) dans les décollements de rétine complexes. J Fr Ophtalmol. 2006;29:137–45.
Auriol S, Pagot-Mathis V, Mahieu L, Lemoine C, Mathis A. Efficacy and safety of heavy silicone oil Densiron 68®in the treatment of complicated retinal detachment with large inferior retinectomy. Graefes Arch Clin Exp Ophthalmol. 2008;246:1383–9.
Kon CH, Asaria RH, Occleston NL, Khaw PT, Aylward GW. Risk factors for proliferative vitreoretinopathy after primary vitrectomy: a prospective study. Br J Ophthalmol. 2000;84:506–11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Abu Eleinen, K.G., Mohalhal, A.A., Ghalwash, D.A. et al. Vitrectomy with scleral buckling versus with inferior retinectomy in treating primary rhegmatogenous retinal detachment with PVR and inferior breaks. Eye 32, 1839–1844 (2018). https://doi.org/10.1038/s41433-018-0194-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-018-0194-0
This article is cited by
-
Results of different strategies to manage complicated retinal re-detachment
Graefe's Archive for Clinical and Experimental Ophthalmology (2021)