Abstract
Aims
The purpose of the present study is to determine the overall and disease-related accuracy of clinical and radiological diagnosis when compared to the histology result of the surgical orbital biopsy.
Methods
A retrospective case notes analysis of patients who underwent surgical orbital biopsy during a 12-year period involving more than 100 orbital lesions. The accuracy of clinical and radiological diagnosis was compared with histological diagnosis.
Results
A total of 112 orbital biopsies were carried out in 104 eyes of 101 patients between 2003 and 2015. Correct diagnosis was reached in <50% of cases by both ophthalmologists and radiologists alike. Vascular lesions exhibit characteristic clinical and imaging features that allow for accurate diagnosis and can often be managed conservatively. The greatest challenge, both clinically and on imaging was in differentiating between inflammatory and haematological orbital lesions which represented half of our cases. There was no operative mortality and there were no post-operative complications recorded.
Conclusion
Surgical orbital biopsy is a safe and accurate diagnostic tool for orbital lesions of unknown aetiology and, in our opinion, remains the gold standard.
Similar content being viewed by others
Introduction
Surgical orbital biopsy is often considered essential for the definitive diagnosis of patients with orbital lesions of unknown aetiology. The development and refinement of more sophisticated and accurate imaging and diagnostic methods may challenge the necessity of tissue diagnosis in all cases.
There are two main indications for surgical orbital biopsy. First, there are the patients with an orbital lesion that requires excision either due to visual threat or suspected malignancy, and in this situation the surgical orbital biopsy is simultaneously a diagnostic and therapeutic procedure. Then, there is the group of patients with a disease that can be managed conservatively with medical therapy or observation alone but without a precise diagnosis the clinician is usually reluctant to do so. In this case, the surgical orbital biopsy is merely a diagnostic procedure and it is precisely this group of patients that we should be targeting to improve the accuracy of our non-invasive or minimally invasive diagnostic modalities.
To date, only few studies have been published on the accuracy of clinical or radiological diagnosis of orbital lesions. The purpose of the present study was to determine the overall and disease-related accuracy of clinical and radiological diagnosis when compared to the histology result of the surgical orbital biopsy. Just how accurate the requisite clinical and radiological acumen can be expected to be was evaluated in this 12-year retrospective study involving the biopsy of more than 100 orbital lesions.
Materials and methods
Patient selection
This was a retrospective case notes analysis of patients who underwent surgical orbital biopsy from 2003 to 2015. Patients were identified from the theatre surgical logbook. Data was retrospectively retrieved from patients’ records and included demographic material, presumptive clinical diagnosis, radiological (CT or MRI) reports and histology results. Operative morbidity and mortality were also noted. Patients with previous established histological diagnosis were excluded. Cases with thyroid-related orbitopathy and extraocular extension of uveal melanoma were also excluded.
We considered six major pathological groups: inflammatory, haematological, neoplastic (primary or metastatic; subdivided into benign and malignant), vascular, infective and miscellaneous.
Statistical analysis
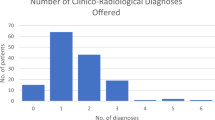
The presumed diagnosis was based on clinical and radiological evaluation, made pre-operatively, and was compared to the gold standard of tissue diagnosis and was categorised as: correct diagnosis (CD), new (incorrect) diagnosis (ND) and inconclusive (ICD). If the presumptive diagnosis, clinical and radiological independently and the histological outcome were in concordance, this was labelled as CD. In contrast, if the histological report differed from the presumptive diagnosis, this was considered as ND. If no presumptive clinical and radiological diagnosis was given, it was considered as no diagnosis and when compared to tissue diagnosis, it was categorised as ND. If a clinician or radiologist included more than one possible diagnosis, this was also considered as no diagnosis and therefore categorised as ND when compared to histology.
Sensitivity is the probability of the clinician, ophthalmologist or radiologist, correctly identifying all positive diagnoses of an orbital lesion (i.e. the proportion of correct clinical positive diagnoses among all histopathologically verified diagnoses of lesions) [1].The positive predictive value (PPV) of the clinical diagnosis is the probability of a clinically based, positive diagnosis of a lesion being correct, expressed as the proportion of histopathologically verified, positive clinical diagnoses among all positive clinical diagnoses [1].The same applies for radiological diagnosis. PPV measures the rate of accuracy [2].
Formal ethics committee approval was not required for this study; however, full regard was paid to the tenets of the declaration of Helsinki
Results
A total of 112 orbital biopsies were carried out in 104 eyes of 101 patients between August 2003 and April 2015. Of these, 63 of the cases were in the right eye, and 49 were in the left eye. The mean age was 52.7 years, with a range of 0–93 years. There were 49 male patients and 55 female patients.
A total of eight patients had repeat biopsy. The indications for this were inconclusive histology; [2] normal orbital tissue; [2] recurrence; [2] one patient re-presented 3 years later with similar symptoms but in the other eye and one patient with deterioration of symptoms despite maximal therapy and also re-presented with symptoms in the other eye.
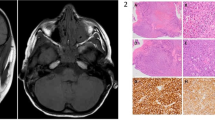
In our cohort of 112 orbital biopsies, the number and percentage of lesions in each category were as follows: inflammatory 35 (31.2%) cases, haematological 21 (18.8%) cases, primary neoplastic 15 (13.4%) cases, benign primary neoplastic 8 (7.1%) cases, malignant primary neoplastic 7 (6.3%) cases, secondary neoplastic 4 (3.6%) cases, vascular 9 (8.0%) cases and miscellaneous 28 (25.0%) cases (Table 1). Half of the cases, 50%, were either inflammatory or haematological orbital lesions.
Clinical diagnosis
Ophthalmologists offered CD in 40 (35.7%) cases (Table 2a). The sensitivity and PPV of clinical diagnosis was 17.1 and 28.6% for inflammatory lesions, 57.1 and 86.0% for haematological lesions, 33.1 and 55.6% for primary neoplastic lesions overall, 50 and 66.7% for benign primary neoplastic lesions, 14.3 and 33.3% for malignant primary neoplastic lesions, 100 and 100% for secondary neoplastic lesions, 55.6 and 83.3% for vascular lesions and 28.6 and 42.1% for miscellaneous lesions, respectively (Table 2b).
Radiological diagnosis
In our cohort, the imaging report was in concordance with the histology results in 34 (30.4%) cases (Table 3a). The sensitivity and PPV of radiological diagnosis was 14.3 and 22.7% for inflammatory lesions, 38.1 and 72.7% for haematological lesions, 33.3 and 71.4% for primary neoplastic lesions overall, 37.5 and 75.0% for benign neoplastic lesions, 28.6 and 66.7% for malignant neoplastic lesions, 100 and 100% for secondary neoplastic lesions, 44.4 and 80.0% for vascular lesions and 28.5 and 42.1% for miscellaneous lesions, respectively (Table 3b).
Complications
There was no operative mortality and there were no post-operative complications recorded. There were five cases of significant intra-operative haemorrhage but haemostasis was achieved in all of them with no other consequences. In four cases the lesion involved the supra-orbital nerve which was sacrificed to allow complete excision. In one patient the surgery had to be cancelled due to difficult intubation but was done later with higher anaesthetic support. Three patients had a histology report that was inconclusive, of which two had repeat biopsy and in the third case it was decided there was no indication for repeat biopsy based on imaging and resolution of symptoms. Of the cases where the histology was reported as ‘normal orbital tissue’, two had a repeat biopsy based on clinical and radiological suspicions, one was reported as healthy lacrimal tissue. The remaining cases were assumed to be more likely herniated orbital fat.
Discussion
Our retrospective case series describes the clinical diagnostic capabilities and imaging reporting of our centre, with the PPV depending almost exclusively on the skills and knowledge of the clinician. With improved diagnostic modalities, many benign lesions such as capillary haemangioma, lymphangioma, optic nerve glioma, optic nerve sheath meningioma, asymptomatic orbital cavernous haemangioma and others are no longer subjected to immediate surgery but are managed by observation, medical therapy or other methods. As Shields et al. concluded on a survey of 1264 patients with orbital tumours and simulating lesions, knowledge of the incidence, clinical and radiological features of various orbital lesions should allow the clinician to arrive at a fairly accurate diagnosis in most cases [3].
CD was reached in <50% of cases by both ophthalmologists and radiologists alike. What was more surprising was that no differential diagnosis was offered in 39 (34.8%) and 44 (39.3%) of cases by ophthalmologists and radiologists respectively. Clinicians most often took a detailed history and performed a comprehensive ocular examination, correctly concluding that there was an orbital lesion requiring imaging but without offering a more specific diagnosis. This confirms a well known phenomenon where physicians nowadays rely less and less on their clinical acumen and more on modern diagnostic modalities. Radiologists also produced detailed reports of the imaging findings using suggestive language such as ‘fat stranding’, ‘encapsulated’, ‘intraconal’ or ‘moulding’ but without offering any conclusive diagnosis. Further, in imaging reports there was often a long list of possible diagnoses highlighting how difficult it can be to differentiate between certain pathologies, more specifically between inflammatory and haematological lesions [4].
Interestingly, both ophthalmologists and radiologists were more accurate in their diagnosis of benign neoplasia than malignant neoplasia. Again, features of malignancy such as “bony destruction” were reported but often lacking a firm diagnosis. Where a firm diagnosis was given, there was a reasonably high PPV, particularly for radiologists in the benign primary neoplasia subgroup.
Ophthalmologists and radiologists alike demonstrated their highest diagnostic sensitivity rate with vascular and secondary neoplastic lesions, 55.6 and 100%, respectively of clinical diagnoses and 44.0 and 100%, respectively of radiological diagnoses, as may be expected. In all secondary neoplastic cases a primary site was known, while there were three further cases with a known extraocular malignancy whose orbital lesion turned out not to be metastatic in nature. Vascular lesions exhibit characteristic clinical and imaging features that allow for accurate diagnosis and can often be managed conservatively [4,5,6,7,8].
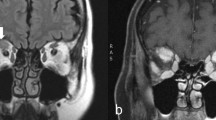
The greatest challenge, both clinically and on imaging, was in differentiating between inflammatory and haematological orbital lesions which represented half of our cases (50%). Management of inflammatory orbital disease is often with systemic corticosteroids allowing clinical response to guide further management. In contrast, haematological lesions such as lymphoma require tissue confirmation and classification before embarking on more specific and aggressive treatment. We observed that ophthalmologists and radiologists often narrowed down their diagnoses to ‘lymphoma or inflammatory lesion’ but could not further differentiate between the two. This counted as incorrect diagnosis, as multiple diagnoses were offered, and therefore contributed to the low sensitivity and predictive value for these types of lesions. Studies in the use of advanced MRI techniques, such as proton magnetic resonance spectroscopy and diffusion-weighted imaging, show promising potential in the ability of differentiating between these overlapping entities [9,10,11,12]. To further complicate matters, inflammatory orbital lesions are a heterogeneous group with several entities and several diagnostic hypotheses present under the cover of this broad spectrum. Differentiating between sarcoid and idiopathic orbital inflammatory disease is difficult and specific diagnosis most often can only be reached after surgical orbital biopsy.
Ben Simon et al. established and subsequently published a set of guidelines for the interpretation of orbital imaging by MRI and CT. They assessed their predictive value on 131 patients with biopsy-proven orbital tumours [4]. They concluded that certain imaging features showed significant differential ability but none had a high enough sensitivity to distinguish between malignant, benign and inflammatory lesions [4]. Our study indirectly supports this conclusion. Nevertheless, there are new studies constantly being published highlighting the value and accuracy of MRI in differentiating between benign and malignant orbital tumours, especially in adults [13, 14].
Our study has several of the usual limitations associated with an unmasked retrospective study. Also, the study assesses only excised lesions with the assumption that the conservatively managed lesions are benign and non-sight threatening, which could potentially increase the ‘true’ sensitivity rate and PPV.
In conclusion, surgical orbital biopsy is a safe and accurate diagnostic tool for orbital lesions of unknown aetiology and, in our opinion, remains the gold standard.
Summary
What was known before
Non-invasive imaging for orbital lesions has improved significantly in recent years. There is a lack of research showing levels of concordance between radiological, clinical diagnosis and histological diagnosis from orbital biopsy.
What this study adds
Orbital biopsy remains the gold standard for diagnosis of orbital lesions.
References
Har-Shai Y, Hai N, Taran A, Mayblum S, Barak A, Tzur E, Schafer I, David R, David E, Linn S. Sensitivity and positive predictive values of presurgical clinical diagnosis of excised benign and malignant skin tumours: a prospective study of 835 lesions in 778 patients. Plas Reconstr Surg. 2001;108:1982–9.
Coutinho FG, Pancas R, Magalhaes E, Bernardo EJ, Eugenio L, Antunes JM. Diagnostic value of surgical lung biopsy: comparison with clinical and radiological diagnosis. Eur J Cardiothorac Surg. 2008;33:781–5.
Shields AJ, Shields LC, Scartozzi R. Survey of 1264 patients with orbital tumours and simulating lesions. The 2002 Montgomery Lecture, Part 1. Ophthalmology. 2004;111:997–1008.
Ben Simon JG, Annunziata CC, Fink J, Villablanca P, McCann DJ, Goldberg AR. Rethinking orbital imaging. Establishing guidelines for interpreting orbital imaging studies and evaluating their predictive value in patients with orbital tumours. Ophthalmology. 2005;112:2196–207.
Poon SC, Sze G, Johnson HM. Orbital lesions: differentiating vascular and nonvascular aetiologic factors. Am J Radiol. 2008;190:956–65.
Bilaniuk TL. Orbital vascular lesions. Radiol Clin North Am. 1999;37:169–83.
Detorakis E, Drakonaki E, Kymionis G, Pallikaris I, Tsilimbaris M. Clinical and imaging findings in multifocal orbital vascular lesions: a case series. Sem Ophthalmol. 2009;24:241–4.
Vohra S, Escott E, Stevens D, Branstetter B. Categorization and characterisation of the orbital apex. Neuroradiol . 2011;53:89–107.
Roshdy N, Shahin M, Kishk H, Ghanem AA, El-Khoury S, Mousa A, Elsalekh I. MRI in diagnosis of orbital masses. Cur Eye Res. 2010;35:986–91.
Lee GA, Johnson CM, Policeni AB, Smoker RKW. Imaging of neuro-ophthalmic and orbital disease – a review. Clin Exp Ophthalmol. 2009;37:30–53.
Kapur R, Sepadhari AR, Mafee MF, Putterman AM, Aakalu V, Wendel LJA, Setabutr. P. MR imaging of orbital inflammatory syndrome, orbital cellulitis, and orbital lymphoid lesions: the role of diffusion-weighted imaging. Am J Neuroradiol. 2009;30:64–70.
Cytryn SA, Putterman MA, Schneck LG, Beckman E, Valvassori GE. Predictability of magnetic resonance imaging in differentiation of orbital lymphoma from orbital inflammatory syndrome. Ophthalmic Plast Reconstr Surg. 1997;13:129–34.
Xian J, Zhang Z, Wang Z, Li J, Yang B, Man F, Chang Q, Zhang Y. Value of MR imaging in the differentiation of benign and malignant orbital tumours in adults. Eur Radiol. 2012;20:1692–702.
Razek A, Elkhamary S, Mousa A. Differentiation between benign and malignant orbital tumours at 3-T diffusion MR-imaging. Neuroradiol . 2011;53:517–22.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Koukkoulli, A., Pilling, J.D., Patatas, K. et al. How accurate is the clinical and radiological evaluation of orbital lesions in comparison to surgical orbital biopsy?. Eye 32, 1329–1333 (2018). https://doi.org/10.1038/s41433-018-0078-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-018-0078-3
This article is cited by
-
Multi-disciplinary team meetings with specialist radiologists may improve pre-operative clinico-radiological diagnostic accuracy in patients requiring orbital biopsy and offer reciprocal educational opportunities
Eye (2022)
-
Intravoxel incoherent motion (IVIM) 3 T MRI for orbital lesion characterization
European Radiology (2021)
-
Orbital Rosai-Dorfman disease initially diagnosed as IgG4-related disease: a case report
Acta Neuropathologica Communications (2020)