Abstract
Although several factors are known to play a role in the development and progression of glaucoma, intraocular pressure (IOP) remains the only modifiable risk factor. Medical and surgical treatments for glaucoma both aim to reduce IOP to minimize disease progression. Tonometry is therefore an essential element of the ophthalmological exam. There are several types of tonometers available currently. These range from well-established instruments that have been in clinical use for decades to new devices, which are the result of recent technological advances. The various instruments have advantages and disadvantages that affect their suitability for a given setting, purpose, and patient population. In this review, we aim to describe the most commonly available tonometers today along with their advantages, disadvantages, and applicability.
Similar content being viewed by others
Introduction
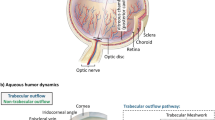
Aqueous humor is produced in the eye by the non-pigmented ciliary epithelium and provides nourishment to the cornea, lens, and the trabecular meshwork [1]. The balance between its production and drainage pressurizes the eye and this is measured as the intraocular pressure (IOP). IOP is a key factor in the development and worsening of glaucoma, a leading cause of irreversible blindness worldwide [2, 3]. IOP reduction has been shown to delay or prevent the onset of glaucoma in individuals with high IOP and is associated with slowing of disease progression in individuals with established glaucoma [4, 5]. Accurate measurement and management of IOP are crucial parameters of glaucoma monitoring and therapy.
Tonometry is an essential component of routine ophthalmological examination. This review aims to discuss the most common types of tonometers available today with their applicability, advantages, and disadvantages.
Applanation tonometry
Applanation tonometry is based on the Imbert–Fick law, according to which, the pressure inside a sphere surrounded by an infinitely thin and flexible membrane can be measured by the force required to flatten a certain area of the membrane [6, 7]. There are several instruments that use an applanating force to flatten an area of the cornea.
Goldmann applanation tonometer
The Goldmann applanation tonometer (GAT) [Haag-Streit, Koeniz, Switzerland and other manufacturers] consists of a biprism mounted on a slit lamp. Fluorescein dye is instilled in the eye to highlight the tear film of the patient. The double prism splits the formed image of the tear film meniscus into a superior and inferior arc. The moment of applanation is ascertained when the arcs are aligned such that their inner margins just touch. GAT uses an applanating force to flatten a constant area of 7.35 mm² (diameter of 3.06 mm). At this selected area, the forces of tear surface tension pulling the tonometer tip toward the eye and the corneal elasticity pushing the tip away are almost equal and opposite. Moreover, at this area, the flattening force(g) multiplied by 10 is equivalent to the IOP (mmHg) [6, 7].
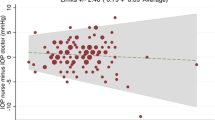
GAT is considered the reference standard for IOP measurement in current clinical practice due to its historical use in most clinical research studies to date and the extensive publications on its validity, reliability, and reproducibility [8, 9]. GAT has relatively low intra and inter-observer variability [10]. In a population-based study including two parts: an inter-observer variation study (n = 40) and an intra-observer variation study (n = 22), subjects had their IOP measured by GAT thrice in a consecutive manner. After a wait of 10 min, the three measurements were obtained again by the same observer in the intra-observer variation study and a different observer in the inter-observer variation study. Median values for the three measurements were calculated for both series of measurements. In the intra-observer variation study, the mean difference was 1.64 (SD 2.07) mmHg between the first measurements and 1.50 (SD 1.96) mmHg between the medians of the three measurements. In the inter-observer variation study, the mean difference was 1.79 (SD 2.41) mmHg between the first measurements and 1.60 (SD 2.15) mmHg between the medians of the three measurements [10]. In another study comprising 420 eyes, Phelps and Phelps reported an inter-observer variability of 3 mmHg or more in 30% of the eyes [11]. Another study including various tonometers found GAT to have the best repeatability followed by non-contact tonometry, ocular blood flow tonography, and Tono-Pen, respectively [12].
There are several limitations associated with GAT. Corneal factors such as corneal thickness and elasticity can be a source of error and affect the accuracy of measurements obtained. Thin corneas can lead to underestimation, whereas thick corneas can lead to overestimation of the IOP [13,14,15]. That said, a population-based study in Singapore found that IOP increased by 0.15 mmHg in right eyes and 0.19 mmHg in left eyes for every 10 μm increase in central corneal thickness (CCT). As the standard deviation of CCT was found to be around 30 μm across all 10-year age groups in the study, it was deduced that a CCT range of 120 μm would include 95% of the study population in each age group. Thus, a variation in GAT-measured IOP of only between 1.8 mmHg and 2.3 mmHg, based on data from right and left eyes respectively, was determined to be attributable to variations in CCT among individuals of equal age [16]. Using similar reasoning, authors of another population-based study in East Asia determined a variation in GAT-measured IOP of between 2.3 mmHg and 3.1 mmHg to be attributable to variations in CCT [17]. Another study used a corneal biomechanical model to evaluate errors in applanation tonometry measurements due to corneal factors. The results showed that variation in corneal biomechanical properties may cause a larger error in IOP measurements as compared with CCT and corneal curvature [18]. Moreover, factors such as corneal irregularities and scarring, inappropriate amounts of fluorescein dye, pressure applied on the eyelids, Valsalva maneuver, breath holding, and high astigmatism can all affect the accuracy of measurements taken with the GAT [7]. The GAT also requires the use of fluorescein dye, topical anesthetics, and a slit-lamp arrangement. It is not portable and requires patients to be seated upright. Therefore, it might not be suitable for certain populations, such as the pediatric, elderly, or those with disabilities [19, 20]. Moreover, it requires a trained person to operate it and it’s calibration needs to be checked monthly [8, 21].
Perkins tonometer
The Perkins tonometer (Clement Clarke, Haag-Streit, UK) uses the same underlying principles as GAT, but is portable and can be used in any position. IOP is similar to GAT [22]. These qualities make it useful in situations where the patient is unable to sit upright or GAT is not possible such as in the operating room or at the patient bedside [8].
Non-contact tonometer
The non-contact tonometer (NCT) [various manufacturers] also called the air-puff tonometer is an applanation tonometer, which uses a column of air to flatten the cornea. The force of the air increases in a steady and linear fashion. The instrument contains a light emitter and a photodetector. The light emitter generates a beam of light that is aimed at the cornea and the reflected light is captured by the detector. The wave form of the reflected light is used to determine when the cornea is applanated. The NCT uses an internal algorithm to convert the force required to flatten the cornea to IOP in mmHg [8, 9].
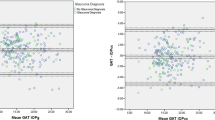
The advantages of the NCT include its non-contact nature, which eliminates the risk of infection and corneal abrasions. It does not require topical anesthesia or instillation of fluorescein dye and can be used by paramedical staff, making it a potential screening tool [23, 24]. Several studies have reported NCT to compare well with GAT [25,26,27]. However, the NCT has shown to overestimate IOP at higher levels and underestimate at lower levels of GAT-measured IOP [12]. In another study, the NCT was found to overestimate IOP as compared with GAT with the difference being greater at higher IOP values [9]. Corneal properties can also affect the measurements. There is a trend toward the readings being more comparable to GAT in thinner corneas whereas higher measurements are obtained in thicker corneas [28]. The NCT has been shown to be more influenced by CCT than GAT, with a reported change in IOP for a 10 μm increase in CCT of 0.46 mmHg as compared with 0.28 mmHg for GAT [29]. A suggested reason behind this observation is greater stiffness of the cornea when deformation occurs at a rapid pace, which is around 8 ms for the NCT [29].
Ocular Response Analyzer
The Ocular Response Analyzer (ORA) [Reichert Technologies, Depew, NY, USA] is a relatively new device that also uses a jet of air as the applanating force for the cornea. It has a sophisticated alignment system, which can apply air pressure to a precise location relative to the apex of the cornea. The force from the air pulse flattens the cornea beyond applanation into a slight indentation. The air pulse stops and the cornea returns back to its original position, passing through a second flat stage. The ORA measures the force at both applanation points, the initial flattening caused by the air pulse and the second point of flattening as the cornea returns to its original shape. It relies on an algorithm to produce two IOP summary measures, a Goldmann-correlated IOP and a corneal compensated IOP (IOPcc) [30,31,32]. The ORA also measures corneal hysteresis and corneal resistance factor [30,31,32,33]. Low corneal hysteresis is associated with progression of glaucoma in some studies [34, 35]. The ORA appears to provide higher IOP measurements as compared with GAT [36, 37] with one study reporting a mean difference of 3.65 ± 3.85 mmHg between IOPcc and GAT [38]. In another study, the ORA was shown to be less repeatable but more reproducible than GAT, whereas the dynamic contour tonometer was reported to be more precise than both ORA and GAT [39]. The ORA is also relatively expensive, limiting its use to more affluent settings.
Pneumatonometer
The pneumatonometer (Model 30, Reichert Technologies, Depew, NY, USA) contains a silicone tip, measuring 5 mm in diameter, at the end of a floating piston. The tip is used to gently indent the cornea with pressure from a controlled flow of air. The pressure forcing the tip ahead, when the tip and cornea are both flat and an equilibrium is achieved, is used to provide an IOP measurement [7, 40].
The pneumatonometer is portable, easy to use, and has minimal contact with the cornea. This makes it a useful tool for screening purposes. However, the tip can be difficult to disinfect [7] and anesthetic is required. Calibration is essential to acquire reliable readings [8]. As compared with GAT, a study found it to underestimate IOP at lower values and overestimate it at higher values [12]. The measurements were also affected by variation in CCT with a reported change in IOP of 0.38 mmHg for a 10 μm increase in CCT as compared with 0.28 mmHg for GAT, 0.31 mmHg for Tono-Pen, and 0.46 mmHg for NCT [29]. This study used a pneumatonometer, which had disposable tips and a probe that was mounted on a slit-lamp.
Tono-Pen
The Tono-Pen (Reichert Technologies, Depew, NY, USA) is a portable, hand-held tonometer that combines applanation and indentation to determine IOP. The Tono-Pen consists of a small plunger connected to a strain gauge that projects from the applanating surface. The plunger faces increasing resistance from the eye as the tonometer touches the cornea. At the point of applanation, this force is shared by the plunger and the footplate. This causes a momentary decrease in the rising force. The force at this point is used to determine the IOP in mmHg based on empirical studies as the area of applanation is known [7].
The Tono-Pen is an electronic hand-held device, which is lightweight, portable, and easy to use. It can be used in any position and does not require special training. It takes multiple readings and displays the average and provides an estimate of the accuracy of the reading based on the standard deviation of the measures. As it only requires a small contact area, it can be used to measure IOP in patients with irregular corneas [32]. Similarly, it has been shown to provide reliable measurements in eyes with therapeutic contact lenses with no significant difference in the measured IOP with and without a lens. Therapeutic contact lenses may be indicated for an array of reasons and their repeated removal may disrupt epithelial healing of the cornea. Therefore, the Tono-Pen may be useful for situations where measurement of IOP without removal of the lens is preferred [41]. Despite its various advantages, the Tono-Pen has several limitations. As compared with GAT, it can over or underestimate the IOP [42, 43]. Geyer et al. reported the Tono-Pen to overestimate IOP as compared with GAT [44]. In a study by Salvetat et al., a nonsignificant trend was observed towards Tono-Pen underestimating IOP at lower GAT values (<24 mmHg) and overestimating it at higher GAT values (>24 mmHg) [42]. On the other hand, some studies have reported the Tono-Pen to overestimate GAT-measured IOP at lower values and underestimate it at higher values [45, 46]. CCT can also influence Tono-Pen readings [42, 47], with one study reporting a mean change of 0.74 mmHg in the obtained IOP for a 10 μm increase in CCT [42].
Indentation tonometry
Indentation tonometry is based on the principle that a force or weight will cause more indentation in a soft object as compared with a hard object [7].
Schiotz tonometer
The Schiotz tonometer (various manufacturers) is based on the principle of indentation. It became the most widely used tonometer worldwide for the bulk of the 20th century until GAT took over during its last quarter. It consists of a plunger that floats in a barrel. The barrel has a curved footplate attached to its bottom. The weight of the plunger can be altered from 5 to 15 g in order to indent the cornea. The amount of indentation is indirectly proportional to the IOP [7].
The Schiotz tonometer is cumbersome as the patient needs to assume a supine position, but it is affordable and robust. It has no complicated electronics. Therefore, it is suitable for screening especially in low resource and remote settings [48]. On the other hand, a study comprising 1280 eyes found Schiotz obtained measurements to be lower than GAT-measured values in 84% of the eyes. Moreover, 19% of the eyes demonstrated an IOP difference of 5 mmHg or greater between the two instruments [49]. It also has a risk of corneal abrasion if the patient is unable to stay still and can displace aqueous humor resulting in lower IOP with serial attempts at measurement [7]. Scleral rigidity can also influence the IOP measurements [50].
Rebound tonometry
Rebound tonometers use a magnetized probe that is propelled toward the cornea. The device measures the deceleration of the probe when it contacts the cornea to provide an IOP measurement [7].
Icare tonometer
The Icare tonometer (Icare Finland Oy, Vantaa, Finland) is a contact rebound tonometer. It consists of an assembly of two coaxial coils, which propel the probe toward the cornea. As the magnetized probe bounces back, variation in the motion parameters are detected by a sensor to calculate the IOP [51]. The Icare has shown good agreement with the GAT with a small, nonsignificant mean difference (0.64 mmHg) between the two [52]. It has also been reported to estimate IOP within ±3 mmHg of GAT in 74.1% of the eyes in a study [53]. However, in some studies it underestimated GAT measurements at high IOP values [54, 55]. Other studies have found it to overestimate GAT-measured IOP [19, 56, 57]. The Icare is influenced by CCT where it obtains higher IOP than GAT in thicker corneas [58].
The older version of the Icare cannot be used in an inclined position. A newer version, the Icare PRO allows inclination, which enables it to be used on patients lying supine. The Icare PRO has shown good agreement with GAT with a study reporting a small mean difference of −0.38 mmHg [59]. Another study showed that the difference in IOP measurements between the Icare PRO and the GAT was not affected by CCT, age, axial length, or spherical equivalent [20]. Another reported that the Icare PRO overestimated IOP at lower GAT values and underestimated it at higher GAT values [60].
The Icare is a hand-held, lightweight, and portable device. The measurement does not cause patient discomfort with no need for anesthesia or fluorescein dye. These attributes make it suitable for screening purposes. The Icare measurements have shown to not be affected if the probe does not precisely touch the central corneal apex [61]. Disposable probes are required and cost about one US dollar each.
The Icare HOME is a newer version of the device that can be used by patients to perform self-tonometry. About 75% of patients were able to obtain measurements on their own eyes with the device in one study [62]. However, it seems to overestimate measurements as compared with GAT [63] and IOP can differ from GAT by a substantial amount in some patients [62].
Dynamic contour tonometry
The Pascal dynamic contour tonometer (DCT) [SMT Swiss Microtechnology AG, Port, Switzerland] uses the Pascal principle to calculate IOP. According to the Pascal principle, the change in pressure is transmitted undiminished in all parts of a fluid contained in an enclosed space [64]. The DCT consists of a tiny piezoelectric sensor installed in its tip. The tip also contains a contour, which, when applied to the cornea, causes the shape of the cornea to conform to the preferred contour. The IOP is then measured by the sensor transcorneally [65]. The instrument also generates a score ranging from 1 (optimum) to 5 (not acceptable) to represent the quality of the IOP measurements obtained. A score of 1 or 2 is thought to be reliable for clinical practice [32].
The DCT has shown to be more repeatable and reproducible than GAT or ORA [66]. IOP measured by the DCT is reported to be higher than that obtained by the GAT with their difference being greatest at low CCT [67]. Similarly, poor agreement with the GAT has been reported for both very thin and very thick corneas [68], which may indicate that DCT measurements are less influenced by corneal factors as compared with the GAT [69, 70]. It therefore may be useful after keratoplasty and refractive surgery as it is less affected by variations in corneal properties following such procedures [70, 71]. A study has shown DCT to agree well with intracameral IOP (Lin’s concordance coefficient = 0.9763), however, it significantly underestimated the reference IOP at higher values. There was no statistically significant effect of corneal curvature, astigmatism, axial length, and age on the difference between DCT and intracameral IOP. Although CCT was found to have a statistically significant effect on their difference, it was not deemed to be clinically pertinent [72].
The disadvantages of DCT include its nature as a contact tonometer, lack of wide use at present, and the need for trained staff and patient cooperation for accurate measurements [73].
Corvis ST
The Corvis ST (Oculus, Wetzlar, Germany) is a novel device, which comprises an air-jet indentation system and ultra-high-speed Scheimpflug technology, to monitor the corneal deformation response. It provides in vivo characterization of corneal biomechanical properties in two dimensions. The Scheimpflug camera has a blue light LED with a horizontal coverage of 8.5 mm. It monitors the corneal response to the air puff by taking >4300 frames per second [74]. A study including healthy eyes reported the device to have good repeatability and reproducibility for measurement of IOP and dynamic corneal response [75]. Another study including both glaucoma patients and healthy controls reported the obtained IOP to be 1.3 mmHg lower, on average, as compared with GAT [76]. Advantages of this device include its non-contact nature and in vivo monitoring of corneal properties. The disadvantages include its cost, lack of wide use at present, need for trained staff, and the table mount setup.
Conclusion
Accurate and precise measurement of IOP is an important component of glaucoma management. There are numerous types of tonometers available today. The GAT has the advantage of its long history of use, reliability, and reproducibility. Furthermore, almost all clinical trials in glaucoma have relied on GAT as the gold standard. Non-contact devices such as the NCT, ORA, and Corvis ST have the advantage of reduced risk for infections and corneal abrasions. Tonometers that are portable and do not require anesthetic or specialized training for use such as the Icare can be useful for screening purposes, as well as in the clinic. Devices that allow use in the supine position such as the Tono-Pen and Perkins are helpful in cases where patients cannot sit upright. Devices that produce rapid deformation of the cornea such as the NCT may be more influenced by corneal properties. Newer devices, such as the ORA and DCT, are proposed to be less influenced by corneal properties, however, they are not widely used at present. In summary, different types of tonometers vary in terms of their portability, positioning, agreement with the GAT, influence of corneal properties, and the need for trained operators and patient cooperation. These factors should be taken into consideration when selecting the appropriate instrument to be used for a specific purpose, setting and patient population.
References
Levin LA, Nilsson SFE, Ver Hoeve J, Wu S, Kaufman PL, Alm A. Adler’s physiology of the eye: expert consult. London: Elsevier Health Sciences; 2011.
Tham Y-C, Li X, Wong TY, Quigley HA, Aung T, Cheng C-Y. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–90.
Sommer A, Tielsch JM, Katz J, Quigley HA, Gottsch JD, Javitt J, et al. Relationship between intraocular pressure and primary open angle glaucoma among white and black Americans. The Baltimore Eye Survey. Arch Ophthalmol. 1991;109:1090–5.
Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol Chic Ill 1960. 2002;120:701–13.
Leske MC, Heijl A, Hyman L, Bengtsson B, Komaroff E. Factors for progression and glaucoma treatment: the Early Manifest Glaucoma Trial. Curr Opin Ophthalmol. 2004;15:102–6.
Goldmann H, Schmidt T. [Applanation tonometry]. Ophthalmol J Int Ophtalmol Int J Ophthalmol Z Augenheilkd. 1957;134:221–42.
Stamper RL. A history of intraocular pressure and its measurement. Optom Vis Sci. 2011;88:E16–28.
Kass MA. Standardizing the measurement of intraocular pressure for clinical research. Guidelines from the Eye Care Technology Forum. Ophthalmology. 1996;103:183–5.
Farhood QK. Comparative evaluation of intraocular pressure with an air-puff tonometer versus a Goldmann applanation tonometer. Clin Ophthalmol Auckl Nz. 2013;7:23–7.
Dielemans I, Vingerling JR, Hofman A, Grobbee DE, de Jong PT. Reliability of intraocular pressure measurement with the Goldmann applanation tonometer in epidemiological studies. Graefes Arch Clin Exp Ophthalmol Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1994;232:141–4.
Phelps CD, Phelps GK. Measurement of intraocular pressure: a study of its reproducibility. Albrecht Von Graefes Arch Für Klin Exp Ophthalmol. 1976;198:39–43.
Tonnu P-A, Ho T, Sharma K, White E, Bunce C, Garway-Heath D. A comparison of four methods of tonometry: method agreement and interobserver variability. Br J Ophthalmol. 2005;89:847–50.
Herndon LW, Choudhri SA, Cox T, Damji KF, Shields MB, Allingham RR. Central corneal thickness in normal, glaucomatous, and ocular hypertensive eyes. Arch Ophthalmol Chic Ill 1960. 1997;115:1137–41.
Ehlers N, Bramsen T, Sperling S. Applanation tonometry and central corneal thickness. Acta Ophthalmol (Copenh). 1975;53:34–43.
Shah S, Chatterjee A, Mathai M, Kelly SP, Kwartz J, Henson D, et al. Relationship between corneal thickness and measured intraocular pressure in a general ophthalmology clinic1. Ophthalmology. 1999;106:2154–60.
Foster PJ, Machin D, Wong T-Y, Ng T-P, Kirwan JF, Johnson GJ, et al. Determinants of intraocular pressure and its association with glaucomatous optic neuropathy in Chinese Singaporeans: the Tanjong Pagar Study. Invest Ophthalmol Vis Sci. 2003;44:3885–91.
Foster PJ, Baasanhu J, Alsbirk PH, Munkhbayar D, Uranchimeg D, Johnson GJ. Central corneal thickness and intraocular pressure in a Mongolian population. Ophthalmology. 1998;105:969–73.
Liu J, Roberts CJ. Influence of corneal biomechanical properties on intraocular pressure measurement: quantitative analysis. J Cataract Refract Surg. 2005;31:146–55.
Poostchi A, Mitchell R, Nicholas S, Purdie G, Wells A. The iCare rebound tonometer: comparisons with Goldmann tonometry, and influence of central corneal thickness. Clin Exp Ophthalmol. 2009;37:687–91.
Kim KN, Jeoung JW, Park KH, Yang MK, Kim DM. Comparison of the new rebound tonometer with Goldmann applanation tonometer in a clinical setting. Acta Ophthalmol (Copenh). 2013;91:e392–396.
Sandhu SS, Chattopadhyay S, Birch MK, Ray-Chaudhuri N. Frequency of goldmann applanation tonometer calibration error checks. J Glaucoma. 2005;14:215–8.
Arora R, Bellamy H, Austin M. Applanation tonometry: a comparison of the Perkins handheld and Goldmann slit lamp-mounted methods. Clin Ophthalmol Auckl Nz. 2014;8:605–10.
Shields MB. The non-contact tonometer. Its value and limitations. Surv Ophthalmol. 1980;24:211–9.
Yilmaz I, Altan C, Aygit ED, Alagoz C, Baz O, Ahmet S, et al. Comparison of three methods of tonometry in normal subjects: Goldmann applanation tonometer, non-contact airpuff tonometer, and Tono-Pen XL. Clin Ophthalmol Auckl Nz. 2014;8:1069–74.
Parker VA, Herrtage J, Sarkies NJ. Clinical comparison of the Keeler Pulsair 3000 with Goldmann applanation tonometry. Br J Ophthalmol. 2001;85:1303–4.
Jorge J, Díaz-Rey JA, González-Méijome JM, Almeida JB, Parafita MA. Clinical performance of the Reichert AT550: a new non-contact tonometer. Ophthalmic Physiol Opt J Br Coll Ophthalmic Opt Optom. 2002;22:560–4.
Jorge J, González-Méijome JM, Díaz-Rey JA, Almeida JB, Ribeiro P, Parafita MA. Clinical performance of non-contact tonometry by Reichert AT550 in glaucomatous patients. Ophthalmic Physiol Opt J Br Coll Ophthalmic Opt Optom. 2003;23:503–6.
Domke N, Hager A, Wiegand W. [Intraocular pressure and corneal thickness. A comparison between non-contact tonometry and applanation tonometry]. Ophthalmol Z Dtsch Ophthalmol Ges. 2006;103:583–7.
Tonnu P-A, Ho T, Newson T, El Sheikh A, Sharma K, White E, et al. The influence of central corneal thickness and age on intraocular pressure measured by pneumotonometry, non-contact tonometry, the Tono-Pen XL, and Goldmann applanation tonometry. Br J Ophthalmol. 2005;89:851–4.
Kaushik S, Pandav SS. Ocular response analyzer. J Curr Glaucoma Pract. 2012;6:17–9.
Sullivan-Mee M, Billingsley SC, Patel AD, Halverson KD, Alldredge BR, Qualls C. Ocular response analyzer in subjects with and without glaucoma. Optom Vis Sci Publ Am Acad Optom. 2008;85:463–70.
De Moraes CGV, Prata TS, Liebmann J, Ritch R. Modalities of tonometry and their accuracy with respect to corneal thickness and irregularities. J Optom. 2008;1:43–9.
Luce DA. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J Cataract Refract Surg. 2005;31:156–62.
De Moraes CVG, Hill V, Tello C, Liebmann JM, Ritch R. Lower corneal hysteresis is associated with more rapid glaucomatous visual field progression. J Glaucoma. 2012;21:209–13.
Medeiros FA, Freitas D, Lisboa R, Kuang T-M, Zangwill LM, Weinreb RN. Corneal hysteresis as a risk factor for glaucoma progression: a prospective longitudinal study. Ophthalmology. 2013;120:1533–40.
Martinez-de-la-Casa JM, Garcia-Feijoo J, Fernandez-Vidal A, Mendez-Hernandez C, Garcia-Sanchez J. Ocular response analyzer versus Goldmann applanation tonometry for intraocular pressure measurements. Invest Ophthalmol Vis Sci. 2006;47:4410–4.
Kynigopoulos M, Schlote T, Kotecha A, Tzamalis A, Pajic B, Haefliger I. Repeatability of intraocular pressure and corneal biomechanical properties measurements by the ocular response analyser. Klin Mon Augenheilkd. 2008;225:357–60.
Hager A, Annette H, Loge K, Kristina L, Schroeder B, Bernd S, et al. Effect of central corneal thickness and corneal hysteresis on tonometry as measured by dynamic contour tonometry, ocular response analyzer, and Goldmann tonometry in glaucomatous eyes. J Glaucoma. 2008;17:361–5.
Kotecha A, White E, Schlottmann PG, Garway-Heath DF. Intraocular pressure measurement precision with the Goldmann applanation, dynamic contour, and ocular response analyzer tonometers. Ophthalmology. 2010;117:730–7.
Lim T-C, Chattopadhyay S, Acharya UR. A survey and comparative study on the instruments for glaucoma detection. Med Eng Phys. 2012;34:129–39.
Scibilia GD, Ehlers WH, Donshik PC. The effects of therapeutic contact lenses on intraocular pressure measurement. J Publ Contact Lens Assoc Ophthalmol Inc. 1996;22:262–5.
Salvetat ML, Zeppieri M, Tosoni C, Brusini P. Comparisons between Pascal dynamic contour tonometry, the TonoPen, and Goldmann applanation tonometry in patients with glaucoma. Acta Ophthalmol Scand. 2007;85:272–9.
Mollan SP, Wolffsohn JS, Nessim M, Laiquzzaman M, Sivakumar S, Hartley S, et al. Accuracy of Goldmann, ocular response analyser, Pascal and TonoPen XL tonometry in keratoconic and normal eyes. Br J Ophthalmol. 2008;92:1661–5.
Geyer O, Mayron Y, Loewenstein A, Neudorfer M, Rothkoff L, Lazar M. Tono-Pen tonometry in normal and in post-keratoplasty eyes. Br J Ophthalmol. 1992;76:538–40.
Kao SF, Lichter PR, Bergstrom TJ, Rowe S, Musch DC. Clinical comparison of the Oculab Tono-Pen to the Goldmann applanation tonometer. Ophthalmology. 1987;94:1541–4.
Frenkel RE, Hong YJ, Shin DH. Comparison of the Tono-Pen to the Goldmann applanation tonometer. Arch Ophthalmol Chic Ill 1960. 1988;106:750–3.
Dohadwala AA, Munger R, Damji KF. Positive correlation between Tono-Pen intraocular pressure and central corneal thickness. Ophthalmology. 1998;105:1849–54.
Cordero I. Understanding and caring for a Schiotz tonometer. Community Eye Health. 2014;27:57.
The incidence of Schiøtz-applanation disparity. Arch Ophthalmol Chic Ill 1960. 1967;77:305–8.
Patel H, Gilmartin B, Cubbidge RP, Logan NS. In vivo measurement of regional variation in anterior scleral resistance to Schiotz indentation. Ophthalmic Physiol Opt J Br Coll Ophthalmic Opt Optom. 2011;31:437–43.
Ademola-Popoola D, ODI A, Akande T. Comparison of IOP readings using rebound I CARE tonometer and Perkins applanation tonometer in an African population. J West Afr Coll Surg. 2014;4:17–30.
van der Jagt LH, Jansonius NM. Three portable tonometers, the TGDc-01, the ICARE and the Tonopen XL, compared with each other and with Goldmann applanation tonometry. Ophthalmic Physiol Opt J Br Coll Ophthalmic Opt Optom. 2005;25:429–35.
Brusini P, Salvetat ML, Zeppieri M, Tosoni C, Parisi L. Comparison of ICare tonometer with Goldmann applanation tonometer in glaucoma patients. J Glaucoma. 2006;15:213–7.
Gao F, Liu X, Zhao Q, Pan Y. Comparison of the iCare rebound tonometer and the Goldmann applanation tonometer. Exp Ther Med. 2017;13:1912–6.
Sinha G, Gupta S, Temkar S, Pandey V, Sihota R, Dada T. IOP agreement between I-Care TA01 rebound tonometer and the Goldmann applanation tonometer in eyes with and without glaucoma. Int Ophthalmol. 2015;35:89–93.
Fernandes P, Diaz-Rey JA, Queiros A, Gonzalez-Meijome JM, Jorge J. Comparison of the ICareR rebound tonometer with the Goldmann tonometer in a normal population. Ophthalmic Physiol Opt. 2005;25:436–40.
Martinez-de-la-Casa JM, Garcia-Feijoo J, Castillo A, Garcia-Sanchez J. Reproducibility and clinical evaluation of rebound tonometry. Invest Ophthalmol Vis Sci. 2005;46:4578–80.
Nakamura M, Darhad U, Tatsumi Y, Fujioka M, Kusuhara A, Maeda H, et al. Agreement of rebound tonometer in measuring intraocular pressure with three types of applanation tonometers. Am J Ophthalmol. 2006;142:332–4.
Güler M, Bilak Ş, Bilgin B, Şimşek A, Çapkin M, Hakim Reyhan A. Comparison of intraocular pressure measurements obtained by Icare PRO Rebound Tonometer, Tomey FT-1000 Noncontact Tonometer, and Goldmann Applanation Tonometer in healthy subjects. J Glaucoma. 2015;24:613–8.
Tamçelik N, Atalay E, Cicik E, Özkök A. Comparability of Icare Pro Rebound Tonometer with Goldmann Applanation and Noncontact Tonometer in a wide range of intraocular pressure and central corneal thickness. Ophthalmic Res. 2015;54:18–25.
Beasley IG, Laughton DS, Coldrick BJ, Drew TE, Sallah M, Davies LN. Does rebound tonometry probe misalignment modify intraocular pressure measurements in human eyes? J Ophthalmol. 2013;2013:791084.
Mudie LI, LaBarre S, Varadaraj V, Karakus S, Onnela J, Munoz B, et al. The Icare HOME (TA022) Study: performance of an intraocular pressure measuring device for self-tonometry by glaucoma patients. Ophthalmology. 2016;123:1675–84.
Takagi D, Sawada A, Yamamoto T. Evaluation of a new rebound self-tonometer, Icare HOME: comparison with Goldmann Applanation Tonometer. J Glaucoma. 2017;26:613–8.
Pascal’s law - Oxford reference [Internet]. [Cited 2017 Sep 26]. Available from: http://www.oxfordreference.com/oso/viewauthority/10.1093$002foi$002fauthority.20110803100308954
Punjabi OS, Kniestedt C, Stamper RL, Lin SC. Dynamic contour tonometry: principle and use. Clin Exp Ophthalmol. 2006;34:837–40.
Wang AS, Alencar LM, Weinreb RN, Tafreshi A, Deokule S, Vizzeri G, et al. Repeatability and reproducibility of Goldmann applanation, dynamic contour, and ocular response analyzer tonometry. J Glaucoma. 2013;22:127–32.
Francis BA, Hsieh A, Lai M-Y, Chopra V, Pena F, Azen S, et al. Effects of corneal thickness, corneal curvature, and intraocular pressure level on Goldmann applanation tonometry and dynamic contour tonometry. Ophthalmology. 2007;114:20–6.
Milla E, Duch S, Buchacra O, Masuet C. Poor agreement between Goldmann and Pascal tonometry in eyes with extreme pachymetry. Eye Lond Engl. 2009;23:536–42.
Erickson DH, Goodwin D, Rollins M, Belaustegui A, Anderson C. Comparison of dynamic contour tonometry and Goldmann applanation tonometry and their relationship to corneal properties, refractive error, and ocular pulse amplitude. Optom St Louis MO. 2009;80:169–74.
Siganos DS, Papastergiou GI, Moedas C. Assessment of the Pascal dynamic contour tonometer in monitoring intraocular pressure in unoperated eyes and eyes after LASIK. J Cataract Refract Surg. 2004;30:746–51.
Papastergiou GI, Kozobolis V, Siganos DS. Effect of recipient corneal pathology on Pascal tonometer and Goldmann tonometer readings in eyes after penetrating keratoplasty. Eur J Ophthalmol. 2010;20:29–34.
Boehm AG, Weber A, Pillunat LE, Koch R, Spoerl E. Dynamic contour tonometry in comparison to intracameral IOP measurements. Invest Ophthalmol Vis Sci. 2008;49:2472–7.
Bochmann F, Kaufmann C, Thiel MA. Dynamic contour tonometry versus Goldmann applanation tonometry: challenging the gold standard. Expert Rev Ophthalmol. 2010;5:743–9.
Ambrósio R Jr, Ramos I, Luz A, Faria FC, Steinmueller A, Krug M, et al. Dynamic ultra high speed Scheimpflug imaging for assessing corneal biomechanical properties. Rev Bras Oftalmol. 2013;72:99–102.
Lopes BT, Roberts CJ, Elsheikh A, Vinciguerra R, Vinciguerra P, Reisdorf S, et al. Repeatability and reproducibility of intraocular pressure and dynamic corneal response parameters assessed by the Corvis ST. J Ophthalmol. 2017;2017:8515742.
Hong J, Xu J, Wei A, Deng SX, Cui X, Yu X, et al. A new tonometer—the Corvis ST tonometer: clinical comparison with noncontact and Goldmann applanation tonometers. Invest Ophthalmol Vis Sci. 2013;54:659–65.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Aziz, K., Friedman, D.S. Tonometers—which one should I use?. Eye 32, 931–937 (2018). https://doi.org/10.1038/s41433-018-0040-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-018-0040-4
This article is cited by
-
Corneal biomechanics and diagnostics: a review
International Ophthalmology (2024)
-
The short-term effects of intranasal steroids on intraocular pressure in pediatric population
International Ophthalmology (2022)
-
Correlation between corneal thickness, keratometry, age, and differential pressure difference in healthy eyes
Scientific Reports (2021)
-
Effect of trabeculectomy and Ahmed glaucoma valve implantation surgery on corneal biomechanical changes
International Ophthalmology (2020)