Abstract
Background
Vitamin D deficiency (VDD) affects the health and wellbeing of millions worldwide. In high latitude countries such as the United Kingdom (UK), severe complications disproportionally affect ethnic minority groups.
Objective
To develop a decision-analytic model to estimate the cost effectiveness of population strategies to prevent VDD.
Methods
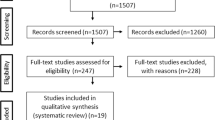
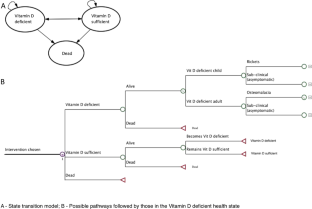
An individual-level simulation model was used to compare: (I) wheat flour fortification; (II) supplementation of at-risk groups; and (III) combined flour fortification and supplementation; with (IV) a ‘no additional intervention’ scenario, reflecting the current Vitamin D policy in the UK. We simulated the whole population over 90 years. Data from national nutrition surveys were used to estimate the risk of deficiency under the alternative scenarios. Costs incurred by the health care sector, the government, local authorities, and the general public were considered. Results were expressed as total cost and effect of each strategy, and as the cost per ‘prevented case of VDD’ and the ‘cost per Quality Adjusted Life Year (QALY)’.
Results
Wheat flour fortification was cost saving as its costs were more than offset by the cost savings from preventing VDD. The combination of supplementation and fortification was cost effective (£9.5 per QALY gained). The model estimated that wheat flour fortification alone would result in 25% fewer cases of VDD, while the combined strategy would reduce the number of cases by a further 8%.
Conclusion
There is a strong economic case for fortifying wheat flour with Vitamin D, alone or in combination with targeted vitamin D3 supplementation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Holick MF. The vitamin D epidemic and its health consequences. J Nutr. 2005;135:2739s–48s. 2005/10/28
Bates B, Lennox A, Prentice A, Bates C, Page P, Nicholson S, et al. National diet and nutrition survey results from years 5 and 6 (combined) of the rolling programme (2012/2013–2013/2014). Public Health Engand and the Food Standards Agency; 2016.
Munns CF, Shaw N, Kiely M, Specker BL, Thacher TD, Ozono K, et al. Global consensus recommendations on prevention and management of nutritional rickets. J Clin Endocrinol Metab. 2016;101:394–415. 2016/01/09
Uday S, Fratzl-Zelman N, Roschger P, Klaushofer K, Chikermane A, Saraff V, et al. Cardiac, bone and growth plate manifestations in hypocalcemic infants: revealing the hidden body of the vitamin D deficiency iceberg. BMC Pediatr. 2018;18:183.
Maiya S, Sullivan I, Allgrove J, Yates R, Malone M, Brain C, et al. Hypocalcaemia and vitamin D deficiency: an important, but preventable, cause of life-threatening infant heart failure. Heart. 2008;94:581–4.
Patel JV, Chackathayil J, Hughes EA, Webster C, Lip GY, Gill PS. Vitamin D deficiency amongst minority ethnic groups in the UK: a cross sectional study. Int J Cardiol. 2013;167:2172–6. 2012/11/13
Uday S, Högler W. Prevention of rickets and osteomalacia in the UK: political action overdue. Arch Dis Child. 2018;103:901–906.
Brown LL, Cohen B, Tabor D, Zappalà G, Maruvada P, Coates PM. The vitamin D paradox in Black Americans: a systems-based approach to investigating clinical practice, research, and public health—expert panel meeting report. BMC Proc. 2018;12:6 https://doi.org/10.1186/s12919-018-0102-4.
Vatanparast H, Nisbet C, Gushulak B. Vitamin D insufficiency and bone mineral status in a population of newcomer children in Canada. Nutrients. 2013;5:1561–72. https://www.ncbi.nlm.nih.gov/pubmed/23673607.
Bärebring L, Schoenmakers I, Glantz A, Hulthén L, Jagner Å, Ellis J, et al. Vitamin D status during pregnancy in a multi-ethnic population-representative Swedish cohort. Nutrients. 2016;8:655.
Ramnemark A, Norberg M, Pettersson-Kymmer U, Eliasson M. Adequate vitamin D levels in a Swedish population living above latitude 63 N: the 2009 Northern Sweden MONICA study. Int J Circumpolar Health. 2015;74:27963.
Andersson Å, Björk A, Kristiansson P, Johansson G. Vitamin D intake and status in immigrant and native Swedish women: a study at a primary health care centre located at 60 N in Sweden. Food Nutr Res. 2013;57:20089.
Glerup H, Rytter L, Mortensen L, Nathan E. Vitamin D deficiency among immigrant children in Denmark. Eur J Pediatr. 2004;163:272–3.
O’Callaghan KM, Kiely ME. Ethnic disparities in the dietary requirement for vitamin D during pregnancy: considerations for nutrition policy and research. Proc Nutr Soc. 2018;77:164–73.
Spiro A, Buttriss JL. Vitamin D: an overview of vitamin D status and intake in Europe. Nutr Bull. 2014;39:322–50. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4288313/.
(SACN) SAC on N. Vitamin D and Health. Public Health England; 2016. https://www.gov.uk/government/groups/scientific-advisory-committee-on-nutrition.
Uday S, Kongjonaj A, Aguiar M, Tulchinsky T, Högler W. Variations in infant and childhood vitamin D supplementation programmes across Europe and factors influencing adherence. Endocr Connect. 2017;6:667–75. https://www.ncbi.nlm.nih.gov/pubmed/28924002.
Bates B, Lennox A, Prentice A, Bates C, Page P, Nicholson S, et al. National diet and nutrition survey results from years 1, 2, 3 and 4 (combined) of the rolling programme (2008/2009 –2011/2012). Public Health Engand and Food Standards Agency; 2014.
Basatemur E, Sutcliffe A. Incidence of hypocalcemic seizures due to vitamin D deficiency in children in the United Kingdom and Ireland. J Clin Endocrinol Metab. 2014;100:E91–5.
Julies P, Lynn RM, Pall K, Leoni M, Calder A, Mughal Z, et al. I16 Nutritional rickets presenting to secondary care in children (16 years)—a UK surveillance study. Arch Dis Child. 2018;103(Suppl 1):A202 LP–A203. http://adc.bmj.com/content/103/Suppl_1/A202.3.abstract.
Cashman KD, Dowling KG, Skrabakova Z, Gonzalez-Gross M, Valtuena J, De Henauw S, et al. Vitamin D deficiency in Europe: pandemic? Am J Clin Nutr. 2016;103:1033–44. 2016/02/13
Darling AL, Hart KH, Macdonald HM, Horton K, Kang’Ombe AR, Berry JL, et al. Vitamin D deficiency in UK South Asian Women of childbearing age: a comparative longitudinal investigation with UK Caucasian women. Osteoporos Int. 2013;24:477–88.
Martin CA, Gowda U, Renzaho AMN. The prevalence of vitamin D deficiency among dark-skinned populations according to their stage of migration and region of birth: a meta-analysis. Nutrition. 2016;32:21–32.
van der Meer IM, Middelkoop BJC, Boeke AJP, Lips P. Prevalence of vitamin D deficiency among Turkish, Moroccan, Indian and sub-Sahara African populations in Europe and their countries of origin: an overview. Osteoporos Int. 2011;22:1009–21. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3046351/.
Ginde AA, Liu MC, Camargo CA. Demographic differences and trends of vitamin D insufficiency in the US population, 1988–2004. Arch Intern Med. 2009;169:626–32. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3447083/.
Aguiar M, Andronis L, Pallan M, Högler W, Frew E. Preventing vitamin D deficiency (VDD): a systematic review of economic evaluations. Eur J Public Health. 2017;27:292–301. 2017/02/17
Barton P, Bryan S, Robinson S. Modelling in the economic evaluation of health care: selecting the appropriate approach. J Health Serv Res Policy. 2004;9:110–8.
Davis S, Stevenson M, Tappenden P, Wailoo AJ. NICE DSU Technical Support Document 15: Cost-effectiveness modelling using patient-level simulation. School of Health and Related Research (ScHARR), The University of Sheffield. 2014.
(NICE) NI for H and CE. Developing NICE guidelines: the manual [Internet]. 3rd ed. Process and methods [PMG20]. 2014. https://www.nice.org.uk/process/pmg20/chapter/incorporating-economic-evaluation.
Siebert U, Alagoz O, Bayoumi AM, Jahn B, Owens DK, Cohen DJ, et al. State-transition modeling: a report of the ISPOR-SMDM modeling good research practices task force-3. Value Health. 2012;15:812–20.
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated health economic evaluation reporting standards (CHEERS) statement. Cost Eff Resour Alloc. 2013;11:6.
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–30.
Statistics O for N. Census. UK: Data Services Census Support.
Allen RE, Dangour AD, Tedstone AE, Chalabi Z. Does fortification of staple foods improve vitamin D intakes and status of groups at risk of deficiency? A United Kingdom modeling study. Am J Clin Nutr. 2015;102:338–44.
Research NS, Laboratory MRCEW, London UC, School M. National Diet and Nutrition Survey Years 1–6, 2008/09-2013/14 [Internet]. UK Data Services; 2017. https://doi.org/10.5255/UKDA-SN-6533-7.
Allen RE. Would fortification of more foods with vitamin D improve vitamin D intakes and status of groups at risk of deficiency in the UK? London School of Hygiene & Tropical Medicine; 2013.
Limited T FreeD: Vitamin D supplementation in Lewisham; 2014. http://www.therapyaudit.com/media/2015/05/lewisham-casestudy.pdf.
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012. https://doi.org/10.1002/14651858.CD007146.pub3.
Aguiar M. Decision analytic modelling of the prevention of vitamin D deficiency in England and Wales. Birmingham, UK: University of Birmingham; 2018. http://etheses.bham.ac.uk/8120/.
Food Standards Agency (FSA). Improving folate intakes of women of reproductive age and preventing neural tube defects: practical issues [Internet]. 2007. http://tna.europarchive.org/20120419000433/http://www.food.gov.uk/multimedia/pdfs/fsa070604.pdf.
NABIM. Statistics [Internet]; 2014. http://www.nabim.org.uk/statistics.
Roy S, Sherman A, Monari-Sparks MJ, Schweiker O, Hunter K. Correction of low vitamin d improves fatigue: effect of correction of low vitamin D in fatigue study (EViDiF Study). North Am J Med Sci. 2014;6:396–402. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4158648/.
Santos AS, Guerra-Junior AA, Godman B, Morton A, Ruas CM. Cost-effectiveness thresholds: methods for setting and examples from around the world. Exp Rev Pharm Outcomes Res. 2018;18:277–88.
Jentink J, van de Vrie-Hoekstra NW, de Jong-van den Berg LT, Postma MJ. Economic evaluation of folic acid food fortification in The Netherlands. Eur J Public Heal. 2008;18:270–4.
Bentley TGK, Weinstein MC, Willett WC, Kuntz KM. A cost-effectiveness analysis of folic acid fortification policy in the United States. Public Health Nutr. 2009;12:455–67.
Grosse SD, Berry RJ, Tilford JM, Kucik JE, Waitzman NJ. Retrospective assessment of cost savings from prevention. Am J Prev Med. 2016;50:S74–80.
Basatemur E, Hunter R, Horsfall L, Sutcliffe A, Rait G. Costs of vitamin D testing and prescribing among children in primary care. Eur J Pediatr. 2017;176:1405–9. http://www.ncbi.nlm.nih.gov/pubmed/28803270.
Poole CD, Smith J, Davies JS. Cost-effectiveness and budget impact of Empirical vitamin D therapy on unintentional falls in older adults in the UK. BMJ Open. 2015;5:e007910.
Del Valle HB, Yaktine AL, Taylor CL, Ross AC. Dietary reference intakes for calcium and vitamin D. Washington (DC), US: National Academies Press; 2011.
Zhang R, Li B, Gao X, Tian R, Pan Y, Jiang Y, et al. Serum 25-hydroxyvitamin D and the risk of cardiovascular disease: dose-response meta-analysis of prospective studies. Am J Clin Nutr. 2017;105:810–9. https://academic.oup.com/ajcn/article/105/4/810-819/4569717.
Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. https://doi.org/10.1136/bmj.i6583. Accessed 18 Apr 2019.
(IOM) Institute of Medicine. Dietary reference intakes for calcium and vitamin D. Washington (DC), US: National Academies Press; 2011.
Lindsay A, Benoist B, Dary O, Hurrell R, WHO/FAO. Guidelines on food fortification with micronutrients. Geneva: World Health Organization and Food and Agriculture Organization of the United Nations; 2006.
WHO/FAO. Evaluating the public health significance of micronutrient malnutrition. In: Guidelines on food fortification with micronutrients. Geneva: World Health Organization and Food and Agriculture Organization of the United Nations; 2006. p. 39–92.
Urrutia-Pereira M, Solé D. Vitamin D deficiency in pregnancy and its impact on the fetus, the newborn and in childhood. Rev Paul Pediatr. 2015;33:104–13.
Holick MF. The influence of vitamin D on bone health across the life cycle. J Nutr. 2005;135:2726S–2727S. https://academic.oup.com/jn/article/135/11/2726S/4669897.
Darnton-Hill I, Webb P, Harvey PWJ, Hunt JM, Dalmiya N, Chopra M, et al. Micronutrient deficiencies and gender: social and economic costs. Am J Clin Nutr. 2005;81:1198S–1205S. https://doi.org/10.1093/ajcn/81.5.1198.
Bivins R. “The English Disease” or “Asian Rickets”? Medical responses to postcolonial immigration. Bull Hist Med. 2007;81:533.
Horton S. The economics of food fortification. J Nutr. 2006;136:1068–71. https://doi.org/10.1093/jn/136.4.1068.
Filby A, Wood H, Jenks M, Taylor M, Burley V, Barbier M, et al. Examining the cost-effectiveness of moving the healthy start vitamin programme from a targeted to a universal offering: cost-effectiveness systematic review [Internet]. NICE, editor. Vol. July; 2015. https://www.nice.org.uk/Media/Default/About/what-we-do/NICE-guidance/NICE-guidelines/healthy-start-cost-effectiveness-review.pdf.
Acknowledgements
Dr. Sue Horton, School of Public Health and Health Systems, University of Waterloo, for initial advice on the economics of food fortification. Dr. Helena Pachón, Rollins School of Public Health, Emory University, for the insights on the practicalities of wheat flour fortification. The team at the Center for Health Economics Research and Evaluation, University Technology Sydney, particularly Dr. Phillip Haywood, as well as Dr. Kim Dalziel, Center for Health Policy, University of Melbourne, for the methodological advice. Smita Hanciles and Gwenda Scott from Lewisham Local Authority, UK, as well as Eleanor McGee from Birmingham Local Authority, UK, for the insights on supplementation alternatives and data access.
Funding
This research was funded by the College of Medical and Dental Sciences of the University of Birmingham, through an internal PhD studentship grant.
Author information
Authors and Affiliations
Contributions
All authors contributed to designing the research. MA conducted the research and analysed data supervised by LA, MP, WH and EF. All authors contributed substantially to writing the paper, while MA and EF had primary responsibility for final content. All authors have read and approved the final paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Aguiar, M., Andronis, L., Pallan, M. et al. The economic case for prevention of population vitamin D deficiency: a modelling study using data from England and Wales. Eur J Clin Nutr 74, 825–833 (2020). https://doi.org/10.1038/s41430-019-0486-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-019-0486-x
This article is cited by
-
The evident and the hidden factors of vitamin D status in older people during COVID-19 pandemic
Nutrire (2021)
-
Prevalence of vitamin D deficiency and its associated risk factors among rural population of the northern part of the Persian Gulf
BMC Endocrine Disorders (2021)
-
Serum 25-hydroxyvitamin D is negatively associated with severe periodontitis: a cross-sectional study
BMC Oral Health (2021)