Abstract
Background/Objectives
Malignant pleural mesothelioma (MPM) is an incurable cancer and optimizing daily physical activity and quality of life are key goals of patient management. Little is known about the prevalence of pre-sarcopenia and malnutrition in MPM or their associations with patient outcomes. This study aimed to determine the prevalence of pre-sarcopenia and malnutrition in MPM and investigate if activity levels and quality of life differed according to body composition and nutritional status.
Subjects/Methods
Patients with a diagnosis of MPM were recruited. Pre-sarcopenia was defined as low appendicular skeletal muscle mass (≤ 7.26 kg/m2 for men and ≤ 5.45 kg/m2 for women), measured by dual energy X-ray absorptiometry. Malnutrition was defined as a rating of B or C on the Patient-Generated Subjective Global Assessment. Outcome measures included objective activity levels (Actigraph GT3X) and health-related quality of life (HRQoL; Functional Assessment of Cancer Therapy General).
Results
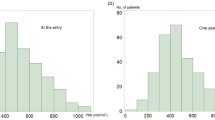
Sixty-one people participated (79% male, median age 69 [IQR 62–74] years and median BMI 25.8 [IQR 24.3–28.4] kg/m2). Fifty-four percent were pre-sarcopenic and 38% were malnourished. Percent of time spent in light activity/day was lower in participants with pre-sarcopenia compared with non-sarcopenic participants (median 25.4 [IQR 19.8–32.1]% vs. 32.3 [27.1–35.6]%; p = 0.008). Participants with malnutrition had poorer HRQoL than well-nourished participants (mean 69.0 (16.3) vs. 84.4 (13.3); p < 0.001).
Conclusion
Participants with MPM had high rates of pre-sarcopenia and malnutrition. Pre-sarcopenia was associated with poorer activity levels, whilst malnutrition was associated with poorer quality of life. Interventions that aim to address reduced muscle mass and weight loss, should be tested in MPM to assess their impact on patient outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Kao SCH, Rei G, Lee K, Vardy J, Clarke S, van Zandwijk N. Malignant mesothelioma. Intern Med J. 2010;40:742–50.
Brims FJ, Meniawy TM, Duffus I, de Fonseka D, Segal A, Creaney J, et al. A novel clinical prediction model for prognosis in malignant pleural mesothelioma using decision tree analysis. J Thorac Oncol. 2016;11:573–82. https://doi.org/10.1016/j.jtho.2015.12.108.
Finn RS, Brims FJ, Gandhi A, Olsen N, Musk AW, Maskell NA, et al. Postmortem findings of malignant pleural mesothelioma: a two-center study of 318 patients. Chest. 2012;142:1267–73. https://doi.org/10.1378/chest.11-3204.
Vogelzang NJ, Rusthoven JJ, Symanowski J, Denham C, Kaukel E, Ruffie P, et al. Phase III study of pemetrexed in combination with cisplatin versus cisplatin alone in patients with malignant pleural mesothelioma. J Clin Oncol. 2003;21:2636–44. https://doi.org/10.1200/jco.2003.11.136.
Scherpereel A, Wallyn F, Albelda SM, Munck C. Novel therapies for malignant pleural mesothelioma. Lancet Oncol. 2018;19:e161–e72. https://doi.org/10.1016/s1470-2045(18)30100-1.
Carneiro IP, Mazurak VC, Prado CM. Clinical implications of sarcopenic obesity in cancer. Curr Oncol Rep. 2016;18:62. https://doi.org/10.1007/s11912-016-0546-5.
Ramos Chaves M, Boleo-Tome C, Monteiro-Grillo I, Camilo M, Ravasco P. The diversity of nutritional status in cancer: new insights. Oncologist. 2010;15:523–30. https://doi.org/10.1634/theoncologist.2009-0283.
Gioulbasanis I, Martin L, Baracos VE, Thezenas S, Koinis F, Senesse P. Nutritional assessment in overweight and obese patients with metastatic cancer: does it make sense? Ann Oncol. 2015;26:217–21. https://doi.org/10.1093/annonc/mdu501.
Nipp RD, Fuchs G, El-Jawahri A, Mario J, Troschel FM, Greer JA, et al. Sarcopenia is associated with quality of life and depression in patients with advanced cancer. Oncologist. 2017. https://doi.org/10.1634/theoncologist.2017-0255.
Bye A, Sjoblom B, Wentzel-Larsen T, Gronberg BH, Baracos VE, Hjermstad MJ, et al. Muscle mass and association to quality of life in non-small cell lung cancer patients. J Cachex- Sarcopenia Muscle. 2017;8:759–67. https://doi.org/10.1002/jcsm.12206.
Polanski J, Jankowska-Polanska B, Uchmanowicz I, Chabowski M, Janczak D, Mazur G, et al. Malnutrition and quality of life in patients with non-small-cell lung cancer. Adv Exp Med Biol. 2017;1021:15–26. https://doi.org/10.1007/5584_2017_23.
Takayama K, Atagi S, Imamura F, Tanaka H, Minato K, Harada T, et al. Quality of life and survival survey of cancer cachexia in advanced non-small cell lung cancer patients-Japan nutrition and QOL survey in patients with advanced non-small cell lung cancer study. Support Care Cancer. 2016. https://doi.org/10.1007/s00520-016-3156-8.
Wallengren O, Lundholm K, Bosaeus I. Diagnostic criteria of cancer cachexia: relation to quality of life, exercise capacity and survival in unselected palliative care patients. Support Care Cancer. 2013;21:1569–77. https://doi.org/10.1007/s00520-012-1697-z.
Thoresen L, Frykholm G, Lydersen S, Ulveland H, Baracos V, Birdsell L, et al. The association of nutritional assessment criteria with health-related quality of life in patients with advanced colorectal carcinoma. Eur J Cancer Care (Engl). 2012;21:505–16. https://doi.org/10.1111/j.1365-2354.2012.01327.x.
Sanchez-Lara K, Turcott JG, Juarez E, Guevara P, Nunez-Valencia C, Onate-Ocana LF, et al. Association of nutrition parameters including bioelectrical impedance and systemic inflammatory response with quality of life and prognosis in patients with advanced non-small-cell lung cancer: a prospective study. Nutr Cancer. 2012;64:526–34. https://doi.org/10.1080/01635581.2012.668744.
Persson C, Glimelius B. The relevance of weight loss for survival and quality of life in patients with advanced gastrointestinal cancer treated with palliative chemotherapy. Anticancer Res. 2002;22(6b):3661–8.
Fearon K, Arends J, Baracos V. Understanding the mechanisms and treatment options in cancer cachexia. Nat Rev Clin Oncol. 2013;10:90–9. https://doi.org/10.1038/nrclinonc.2012.209.
Hutton JL, Martin L, Field CJ, Wismer WV, Bruera ED, Watanabe SM, et al. Dietary patterns in patients with advanced cancer: implications for anorexia-cachexia therapy. Am J Clin Nutr. 2006;84:1163–70.
Srdic D, Plestina S, Sverko-Peternac A, Nikolac N, Simundic AM, Samarzija M. Cancer cachexia, sarcopenia and biochemical markers in patients with advanced non-small cell lung cancer-chemotherapy toxicity and prognostic value. Support Care Cancer. 2016;24:4495–502. https://doi.org/10.1007/s00520-016-3287-y.
Kim EY, Kim YS, Seo JY, Park I, Ahn HK, Jeong YM, et al. The relationship between sarcopenia and systemic inflammatory response for cancer cachexia in small cell lung cancer. PLoS ONE. 2016;11:e0161125. https://doi.org/10.1371/journal.pone.0161125.
Amano K, Maeda I, Morita T, Baba M, Miura T, Hama T, et al. C-reactive protein, symptoms and activity of daily living in patients with advanced cancer receiving palliative care. J Cachexia Sarcopenia Muscle. 2017. https://doi.org/10.1002/jcsm.12184.
Batista ML Jr., Olivan M, Alcantara PS, Sandoval R, Peres SB, Neves RX, et al. Adipose tissue-derived factors as potential biomarkers in cachectic cancer patients. Cytokine. 2013;61:532–9. https://doi.org/10.1016/j.cyto.2012.10.023.
Diakowska D, Krzystek-Korpacka M, Markocka-Maczka K, Diakowski W, Matusiewicz M, Grabowski K. Circulating leptin and inflammatory response in esophageal cancer, esophageal cancer-related cachexia-anorexia syndrome (CAS) and non-malignant CAS of the alimentary tract. Cytokine. 2010;51:132–7. https://doi.org/10.1016/j.cyto.2010.05.006.
Lerner L, Hayes TG, Tao N, Krieger B, Feng B, Wu Z, et al. Plasma growth differentiation factor 15 is associated with weight loss and mortality in cancer patients. J Cachex- Sarcopenia Muscle. 2015;6:317–24. https://doi.org/10.1002/jcsm.12033.
Musk AW, Dolin PJ, Armstrong BK, Ford JM, de Klerk NH, Hobbs MS. The incidence of malignant mesothelioma in Australia, 1947–1980. Med J Aust. 1989;150:242–3, 246.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–55.
World Health Organisation. Waist circumference and waist-hip ratio: reports of a WHO expert consultation, Geneva, 8–11 December 2008: World Health Organisation; 2011.
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147:755–63.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412–23. https://doi.org/10.1093/ageing/afq034.
Ottery FD. Definition of standardized nutritional assessment and interventional pathways in oncology. Nutrition. 1996;12(1 Suppl):S15–9.
Freedson PS, Melanson E, Sirard J. Calibration of the computer science and applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30:777–81.
Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167:875–81. https://doi.org/10.1093/aje/kwm390.
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11:570–9.
Ware JE Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
LeBlanc TW, Samsa GP, Wolf SP, Locke SC, Cella DF, Abernethy AP. Validation and real-world assessment of the Functional Assessment of Anorexia-Cachexia Therapy (FAACT) scale in patients with advanced non-small cell lung cancer and the cancer anorexia-cachexia syndrome (CACS). Support Care Cancer. 2015. https://doi.org/10.1007/s00520-015-2606-z.
Cella D. The Functional Assessment of Cancer Therapy-Anemia (FACT-An) Scale: a new tool for the assessment of outcomes in cancer anemia and fatigue. Semin Hematol. 1997;34(3Suppl 2):13–9.
Blauwhoff-Buskermolen S, Ruijgrok C, Ostelo RW, de Vet HC, Verheul HM, de van der Schueren MA, et al. The assessment of anorexia in patients with cancer: cut-off values for the FAACT-A/CS and the VAS for appetite. Support Care Cancer. 2016;24:661–6. https://doi.org/10.1007/s00520-015-2826-2.
Van Belle S, Paridaens R, Evers G, Kerger J, Bron D, Foubert J, et al. Comparison of proposed diagnostic criteria with FACT-F and VAS for cancer-related fatigue: proposal for use as a screening tool. Support Care Cancer. 2005;13:246–54. https://doi.org/10.1007/s00520-004-0734-y.
Arends J, Baracos V, Bertz H, Bozzetti F, Calder PC, Deutz NEP, et al. ESPEN expert group recommendations for action against cancer-related malnutrition. Clin Nutr. 2017;36:1187–96. https://doi.org/10.1016/j.clnu.2017.06.017.
Volpato S, Bianchi L, Cherubini A, Landi F, Maggio M, Savino E, et al. Prevalence and clinical correlates of sarcopenia in community-dwelling older people: application of the EWGSOP definition and diagnostic algorithm. J Gerontol A Biol Sci Med Sci. 2014;69:438–46. https://doi.org/10.1093/gerona/glt149.
Bauer J, Ash S, Davidson W, Hill J, Brown B, Isenring E, et al. Evidence based practice guidelines for the nutritional management of cancer cachexia. Nutr & Diet. 2006;63:S5–S32. https://doi.org/10.1111/j.1747-0080.2006.00099.x.
Ryan AM, Power DG, Daly L, Cushen SJ, Ni Bhuachalla E, Prado CM. Cancer-associated malnutrition, cachexia and sarcopenia: the skeleton in the hospital closet 40 years later. Proc Nutr Soc. 2016;75:199–211. https://doi.org/10.1017/s002966511500419x.
Li R, Wu J, Ma M, Pei J, Song Y, Zhang X, et al. Comparison of PG-SGA, SGA and body-composition measurement in detecting malnutrition among newly diagnosed lung cancer patients in stage IIIB/IV and benign conditions. Med Oncol. 2011;28:689–96. https://doi.org/10.1007/s12032-010-9534-z.
Lippitz BE. Cytokine patterns in patients with cancer: a systematic review. Lancet Oncol. 2013;14:e218–28. https://doi.org/10.1016/s1470-2045(12)70582-x.
Arnold DT, Hooper CE, Morley A, White P, Lyburn ID, Searle J, et al. The effect of chemotherapy on health-related quality of life in mesothelioma: results from the SWAMP trial. Br J Cancer. 2015;112:1183–9. https://doi.org/10.1038/bjc.2015.77.
de van der Schueren MAE, Laviano A, Blanchard H, Jourdan M, Arends J, Baracos VE. Systematic review and meta-analysis of the evidence for oral nutritional intervention on nutritional and clinical outcomes during chemo(radio)therapy: current evidence and guidance for design of future trials. Ann Oncol. 2018;29:1141–53. https://doi.org/10.1093/annonc/mdy114.
Hopkinson JB. Psychosocial impact of cancer cachexia. J Cachex- Sarcopenia Muscle. 2014;5:89–94. https://doi.org/10.1007/s13539-014-0142-1.
Acknowledgements
EJ was supported by an Australian Lung Foundation/Edith Cowan University PhD Scholarship and Australian Government Research Training Program Scholarship. CJPM was supported by a Cancer Council Western Australia Postdoctoral Fellowship.
Author information
Authors and Affiliations
Contributions
EJ, YCGL, RUN, PLW, JC, and CJPM contributed to the conception of the design of the study. EJ, BN, HMC, and DBF collected the data. EJ, JM, AKN, and LS contributed to data analysis. All authors contributed to the article and have approved the submission of the article for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Jeffery, E., Lee, Y.C.G., Newton, R.U. et al. Body composition and nutritional status in malignant pleural mesothelioma: implications for activity levels and quality of life. Eur J Clin Nutr 73, 1412–1421 (2019). https://doi.org/10.1038/s41430-019-0418-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-019-0418-9
This article is cited by
-
Changes in body composition in patients with malignant pleural mesothelioma and the relationship with activity levels and dietary intake
European Journal of Clinical Nutrition (2022)
-
Voluntary exercise in mesothelioma: effects on tumour growth and treatment response in a murine model
BMC Research Notes (2020)