Abstract
Introduction
In the UK, colorectal cancer is the fourth most common cancer and the second most common cause of cancer death. Surgery is the primary modality of treatment, but it is not without complications. Post-operative complications have been linked to preoperative of weight loss and loss of lean tissue, and also to obesity. Given sex differences in body composition, an examination of body composition and post-operative complications may provide valuable information. Therefore, the aim was to examine the relationship between male/female body composition and post-operative complications in patients with operable colorectal cancer.
Methods
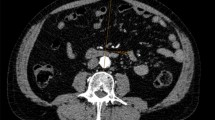
Patients (n = 741) undergoing operation for colorectal cancer were examined. Preoperative CT scans were used to define the muscle mass and quality, visceral obesity, and subcutaneous adiposity. Post-operative complications, in particular, surgical site infection (SSI) and wound infection (WI) were considered as outcome measures.
Results
Male patients with greater subcutaneous adiposity had higher risk of SSI and WI (p < 0.01 and p ≤ 0.001, respectively). On multivariate analysis, Post-operative Glasgow Prognostic Score (poGPS) on Day 4 (OR 2.11, 95% CI 1.53–2.92, P = 0.001) laparoscopic surgery (OR 0.50, 95% CI 0.26–0.98, P = 0.044), and subcutaneous adiposity (OR 2.71, 95% CI 1.26–5.82, P = 0.011) remained significantly independently associated with overall SSI. Subcutaneous adiposity remained significantly independently associated with WI (OR 3.93, 95% CI 1.33–11.57, P = 0.013). In female patients, however, no significant association was found between any body composition measure and complications.
Conclusion
This study showed that increased subcutaneous and visceral adiposity were associated with infective complications in male, but not female patients, after colorectal cancer surgery. Therefore, it is important that sex be taken into account when evaluating the potential impact of body composition on post-operative outcomes in patients undergoing surgery for colorectal cancer.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
OECD. Obesity Update 2017. 2017. https://www.oecd.org/els/health-systems/Obesity-Update-2017.pdf.
Reichman DE, Greenberg JA. Reducing surgical site infections: a review. Rev Obstet Gynecol. 2009;2(4):212–21.
Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol. 1992;13(10):606–8.
Badia JM, Casey AL, Petrosillo N, Hudson PM, Mitchell SA, Crosby C. Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. J Hosp Infect. 2017;96(1):1–15. https://doi.org/10.1016/j.jhin.2017.03.004.
Watt DG, Ramanathan ML, McSorley ST, Walley K, Park JH, Horgan PG, et al. Clinicopathological determinants of an elevated systemic inflammatory response following elective potentially curative resection for colorectal cancer. Ann Surg Oncol. 2017;24(9):2588–94. https://doi.org/10.1245/s10434-017-5987-z.
Moghaddam AA, Woodward M, Huxley R. Obesity and risk of colorectal cancer: a meta-analysis of 31 studies with 70,000 events. Cancer Epidemiol Biomark Prev. 2007;16(12):2533–2547. https://doi.org/10.1158/1055-9965.EPI-07-0708.
Almasaudi A, McSorley S, Edwards C, McMillan D. The relationship between body mass index and short term postoperative outcomes in patients undergoing potentially curative surgery for colorectal cancer: a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2018;121:68–73.
Malietzis G, Aziz O, Bagnall NM, Johns N, Fearon KC, Jenkins JT. The role of body composition evaluation by computerized tomography in determining colorectal cancer treatment outcomes: a systematic review. Eur J Surg Oncol. 2015;41(2):186–196. https://doi.org/10.1016/j.ejso.2014.10.056.
Shachar SS, Williams GR, Muss HB, Nishijima TF. Prognostic value of sarcopenia in adults with solid tumours: a meta-analysis and systematic review. Eur J Cancer. 2016;57:58–67. https://doi.org/10.1016/j.ejca.2015.12.030.
Rickles AS, Iannuzzi JC, Mironov O, Deeb A-P, Sharma A, Fleming FJ, et al. Visceral obesity and colorectal cancer: are we missing the boat with BMI? J Gastrointest Surg. 2013;17(1):133–43. https://doi.org/10.1007/s11605-012-2045-9.
Yip C, Dinkel C, Mahajan A, Siddique M, Cook G, Goh V. Imaging body composition in cancer patients: visceral obesity, sarcopenia and sarcopenic obesity may impact on clinical outcome. Insights Imaging. 2015;6(4):489–497.
Majek O, Gondos A, Jansen L, Emrich K, Holleczek B, Katalinic A, et al. Sex differences in colorectal cancer survival: population-based analysis of 164,996 colorectal cancer patients in Germany. PLoS ONE. 2013;8(7):e68077 https://doi.org/10.1371/journal.pone.0068077.
Richards C, Roxburgh C, MacMillan M, Isswiasi S, Robertson E, Guthrie G, et al. The relationships between body composition and the systemic inflammatory response in patients with primary operable colorectal cancer. PLoS ONE. 2012;7(8):e41883.
Doyle S, Bennett A, Donohoe C, Mongan A, Howard J, Lithander F, et al. Establishing computed tomography–defined visceral fat area thresholds for use in obesity-related cancer research. Nutr Res. 2013;33(3):171–179.
Ebadi M, Martin L, Ghosh S, Field C, Lehner R, Baracos V, et al. Subcutaneous adiposity is an independent predictor of mortality in cancer patients. Br J Cancer. 2017;117(1):148–155.
Caan B, Meyerhardt J, Kroenke C, Alexeeff S, Xiao J, Weltzien E, et al. Explaining the Obesity Paradox: the association between body composition and colorectal cancer survival (C-SCANS Study). Cancer Epidemiol Biomark & Prev. 2017;26(7):1008–1015
Martin L, Birdsell L, MacDonald N, Reiman T, Clandinin M, McCargar L, et al. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol. 2013;31(12):1539–1547.
Langelotz C, Mueller-Rau C, Terziyski S, Rau B, Krannich A, Gastmeier P, et al. Gender-specific differences in surgical site infections: an analysis of 438,050 surgical procedures from the German National Nosocomial Infections Surveillance System. Viszeralmedizin. 2014;30(2):114–7. https://doi.org/10.1159/000362100.
Fuente-Martín E, Argente-Arizón P, Ros P, Argente J, Chowen JA. Sex differences in adipose tissue: It is not only a question of quantity and distribution. Adipocyte. 2013;2(3):128–34. https://doi.org/10.4161/adip.24075.
Nakanishi R, Oki E, Sasaki S, Hirose K, Jogo T, Edahiro K, et al. Sarcopenia is an independent predictor of complications after colorectal cancer surgery. Surg Today. 2017;48(2):151–157.
Lieffers J, Bathe O, Fassbender K, Winget M, Baracos V. Sarcopenia is associated with postoperative infection and delayed recovery from colorectal cancer resection surgery. Br J Cancer. 2012;107(6):931–936.
Kabon B, Nagele A, Reddy D, Eagon C, Fleshman J, Sessler D, et al. Obesity decreases perioperative tissue oxygenation. Anesthesiology. 2004;100(2):274–280.
Sen C. Wound healing essentials: let there be oxygen. Wound Repair Regen. 2009;17(1):1–18.
Acknowledgements
The authors acknowledge Douglas H Black for his assistance. Sources of Support (scholarship): King AbdulAziz university. Clinical nutrition department, Jeddah, Saudi Arabia. Clinical Trial Registry number: not applicable.
Author information
Authors and Affiliations
Contributions
ASA, DCM, and CE designed research; ASA, RDD, STM, and PGH collect the data; ASA and DCM analyzed data and interpretation; ASA wrote the paper; DCM and CE manuscript editing; and ASA, CE, and DCM had responsibility for final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Almasaudi, A.S., Dolan, R.D., McSorley, S.T. et al. Relationship between computed tomography-derived body composition, sex, and post-operative complications in patients with colorectal cancer. Eur J Clin Nutr 73, 1450–1457 (2019). https://doi.org/10.1038/s41430-019-0414-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-019-0414-0
This article is cited by
-
High visceral adipose tissue area is independently associated with early allograft dysfunction in liver transplantation recipients: a propensity score analysis
Insights into Imaging (2022)
-
The association of body composition parameters and adverse events in women receiving chemotherapy for early breast cancer
Breast Cancer Research and Treatment (2020)