Abstract
Background/Objectives
Although several studies have investigated the association between dietary Glycemic Index (GI), glycemic load (GL) and depression, results are inconsistent. This systematic review and meta-analysis was performed to summarize earlier evidence on the association between dietary GI, GL, and depression.
Subjects/Methods
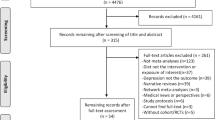
We searched in PubMed/Medline, ISI Web of Knowledge, Scopus, EMBASE, and Google Scholar to identify related articles published until April 2018. Publications that fulfilled the following criteria were included in the current study: (1) publications with participants aged ≥ 18 years; (2) studies that considered GI or GL as the exposure; (3) studies that considered depression as the main outcome or as one of the outcomes; and (4) publications in which odds ratios (ORs) or mean difference were reported as the effect size. Finally, 11 studies, including 6 cross-sectional studies, 2 cohort studies, and 3 clinical trials were considered for inclusion in the systematic review, and 5 cross-sectional studies, 2 cohort studies, and 2 clinical trials (out of 11 studies included in the systematic review) were included in the meta-analysis. The quality of cross-sectional and cohort studies examined by the Newcastle–Ottawa Scale (NOS) and the quality of clinical trials examined using Cochrane Collaboration Risk of Bias tool. We also assessed the quality of evidence with the GRADE system.
Results
Sample sizes of the included cross-sectional studies ranged from 140 to 87,618 participants, and in total 101,389 participants were included in 6 studies. In total, 85,500 participants were included in 2 cohort studies. Sample sizes of the included clinical trials ranged from 40 to 82 participants, and in total 164 participants were included in three studies. Combining seven effect sizes from five cross-sectional studies, no significant association was observed between dietary GI and odds of depression (OR: 1.01; 95% CI: 0.94, 1.08; I2 = 80.2%; n = 5). We also failed to find any significant association between dietary GL and odds of depression (OR: 0.93; 95% CI: 0.84, 1.04; I2 = 42%; n = 5). Combining two effects sizes from two cohort studies, there was a significant positive association between dietary GI and depression (HR: 1.13; 95% CI: 1.02, 1.25; I2 = 86.1%, n = 2). In addition, combining two effect sizes from two clinical trials, we found a significant change in depression score after consumption of a high-GL diet (weighted mean difference (WMD): 0.66; 95% CI: 0.28, 1.04; I2 = 0.0%, n = 2).
Conclusions
Summarizing earlier findings, we found no significant association between either dietary GI or GL and odds of depression in cross-sectional studies. However, a significant positive association was observed between dietary GI and depression in cohort studies. In addition, a significant effect of a high-GL diet consumption on risk of depression was seen in clinical trials.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Steel Z, Marnane C, Iranpour C, Chey T, Tien C, Jackson JW, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. Int J Epidemiol. 2014;43:476–93.
Murray CJ, Lopez AD. The Global Burden of Disease. Cambridge, MA: Harvard Univ. Press; 1996.
Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289:3095–105.
Noorbala AA, Bagheri Yazdi SA, Yasamy MT, Mohammad K. Mental health survey of the adult population in Iran. Br J Psychiatry. 2004;184:70–3.
Mozaffari-Khosravi H, Nabizade L, Yassini-Ardakani SM, Hadinedoushan H, Barzegar K. The effect of 2 different single injections of high dose of vitamin D on improving the depression in depressed patients with vitamin D deficiency: a randomized clinical trial. J Clin Psychopharmacol. 2013;33:378–85.
Dana-Alamdari L, Kheirouri S, Noorazar SG. Serum 25-hydroxyvitamin D in patients with major depressive disorder. Iran J Public Health. 2015;44:690–7.
Sanchez-Villegas A, Verberne L, De Irala J, Ruíz-Canela M, Toledo E, Serra-Majem L, et al. Dietary fat intake and the risk of depression: the SUN Project. PLoS ONE. 2011;6:e16268.
Grenyer BF, Crowe T, Meyer B, Owen AJ, Grigonis-Deane EM, Caputi P, et al. Fish oil supplementation in the treatment of major depression: a randomised double-blind placebo-controlled trial. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:1393–6.
Silvers KM, Woolley CC, Hamilton FC, Watts PM, Watson RA. Randomised double-blind placebo-controlled trial of fish oil in the treatment of depression. Prostaglandins Leukot Essent Fat Acids. 2005;72:211–8.
Kamphuis MH, Geerlings MI, Grobbee DE, Kromhout D. Dietary intake of B(6-9-12) vitamins, serum homocysteine levels and their association with depressive symptoms: the Zutphen Elderly Study. Eur J Clin Nutr. 2008;62:939–45.
Murakami K, Miyake Y, Sasaki S, Tanaka K, Arakawa M. Dietary folate, riboflavin, vitamin B-6, and vitamin B-12 and depressive symptoms in early adolescence: the Ryukyus Child Health Study. Psychosom Med. 2010;72:763–8.
Michels N, Sioen I, Braet C, Eiben G, Hebestreit A, Huybrechts I, et al. Stress, emotional eating behaviour and dietary patterns in children. Appetite. 2012;59:762–9.
Moubarac JC, Cargo M, Receveur O, Daniel M. Psychological distress mediates the association between daytime sleepiness and consumption of sweetened products: cross-sectional findings in a Catholic Middle-Eastern Canadian community. BMJ Open. 2013;3:e002298.
Mwamburi DM, Liebson E, Folstein M, Bungay K, Tucker KL, Qiu WQ. Depression and glycemic intake in the homebound elderly. J Affect Disord. 2011;132:94–8.
Aparicio A, Robles F, Lopez-Sobaler AM, Ortega RM. Dietary glycaemic load and odds of depression in a group of institutionalized elderly people without antidepressant treatment. Eur J Nutr. 2013;52:1059–66.
Haghighatdoost F, Azadbakht L, Keshteli AH, Feinle-Bisset C, Daghaghzadeh H, Afshar H, et al. Glycemic index, glycemic load, and common psychological disorders. Am J Clin Nutr. 2016;103:201–9.
Murakami K, Miyake Y, Sasaki S, Tanaka K, Yokoyama T, Ohya Y, et al. Dietary glycemic index and load and the risk of postpartum depression in Japan: the Osaka Maternal and Child Health Study. J Affect Disord. 2008;110:174–9.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Guyatt GH, Oxman AD, Vist GE, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Chin J Evid Based Med. 2009;9:8–11.
Jacka FN, Pasco JA, Mykletun A, Williams LJ, Nicholson GC, Kotowicz MA, et al. Diet quality in bipolar disorder in a population-based sample of women. J Affect Disord. 2011;129:332–7.
Gangwisch JE, Hale L, Garcia L, Malaspina D, Opler MG, Payne ME, et al. High glycemic index diet as a risk factor for depression: analyses from the Women’s Health Initiative. Am J Clin Nutr. 2015;102:454–63.
Gopinath B, Flood VM, Burlutksy G, Louie JC, Mitchell P. Association between carbohydrate nutrition and prevalence of depressive symptoms in older adults. Br J Nutr. 2016;116:2109–14.
Minobe N, Murakami K, Kobayashi S, Suga H, Sasaki S. Higher dietary glycemic index, but not glycemic load, is associated with a lower prevalence of depressive symptoms in a cross-sectional study of young and middle-aged Japanese women. Eur J Nutr. 2017. https://doi.org/10.1007/s00394-017-1502-3.
Sanchez-Villegas A, Zazpe I, Santiago S, Perez-Cornago A, Martinez-Gonzalez MA, Lahortiga-Ramos F, et al. Added sugars and sugar-sweetened beverage consumption, dietary carbohydrate index and depression risk in the Seguimiento Universidad de Navarra (SUN) Project. Br J Nutr. 2018;119:211–221.
Cheatham RA, Roberts SB, Das SK, Gilhooly CH, Golden JK, Hyatt R, et al. Long-term effects of provided low and high glycemic load low energy diets on mood and cognition. Physiol Behav. 2009;98:374–9.
Breymeyer KL, Lampe JW, McGregor BA, Neuhouser ML. Subjective mood and energy levels of healthy weight and overweight/obese healthy adults on high-and low-glycemic load experimental diets. Appetite. 2016;107:253–9.
Ma Y, Olendzki BC, Merriam PA, Chiriboga DE, Culver AL, Li W, et al. A randomized clinical trial comparing low-glycemic index versus ADA dietary education among individuals with type 2 diabetes. Nutrition. 2008;24:45–56.
Wada T, Ishine M, Sakagami T, Kita T, Okumiya K, Mizuno K, et al. Depression, activities of daily living, and quality of life of community-dwelling elderly in three Asian countries: Indonesia, Vietnam, and Japan. Arch Gerontol Geriatr. 2005;41:271–80.
Khosravi M, Sotoudeh G, Majdzadeh R, Nejati S, Darabi S, Raisi F, et al. Healthy and unhealthy dietary patterns are related to depression: a case-control study. Psychiatry Investig. 2015;12:434–42.
Hosseinzadeh M, Vafa M, Esmaillzadeh A, Feizi A, Majdzadeh R, Afshar H, et al. Empirically derived dietary patterns in relation to psychological disorders. Public Health Nutr. 2016;19:204–17.
Nouwen A, Winkley K, Twisk J, Lloyd CE, Peyrot M, Ismail K, et al. Type 2 diabetes mellitus as a risk factor for the onset of depression: a systematic review and meta-analysis. Diabetologia. 2010;53:2480–6.
Yu D, Zhang X, Shu X-O, Cai H, Li H, Ding D, et al. Dietary glycemic index, glycemic load, and refined carbohydrates are associated with risk of stroke: a prospective cohort study in urban Chinese women. Am J Clin Nutr. 2016;104:1345–51.
Rumsfeld JS, Ho PM. Depression and cardiovascular disease a call for recognition. Circulation. 2005;111:250–3.
Acknowledgements
The project was financially supported by a joint collaboration of Endocrinology and Metabolism Molecular-Cellular Sciences Institute, Tehran University of Medical Sciences, and School of Nutritional Sciences and Dietetics, Tehran University of Medical Sciences, Tehran, Iran.
Author contributions:
ASM and PS contributed to the conception, design, search, statistical analyses, data interpretation, and manuscript drafting. BL contributed to the conception, design, and data interpretation. AE contributed to the conception, design, statistical analyses, data interpretation, and manuscript drafting. AE supervised the study. All authors approved the final manuscript prior to submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Salari-Moghaddam, A., Saneei, P., Larijani, B. et al. Glycemic index, glycemic load, and depression: a systematic review and meta-analysis. Eur J Clin Nutr 73, 356–365 (2019). https://doi.org/10.1038/s41430-018-0258-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-018-0258-z
This article is cited by
-
The association between dietary insulin index and load with mental health
BMC Psychology (2022)
-
Higher dietary glycemic load is inversely associated with stress prevalence among Iranian adults
BMC Neuroscience (2022)
-
Associations of overall and specific carbohydrate intake with anxiety status evolution in the prospective NutriNet-Santé population-based cohort
Scientific Reports (2022)
-
Association of sugar intake from different sources with incident depression in the prospective cohort of UK Biobank participants
European Journal of Nutrition (2022)
-
Artificial neural network application for identifying risk of depression in high school students: a cross-sectional study
BMC Psychiatry (2021)