Abstract
Repurposing nonantibiotic drugs for antimicrobial therapy presents a viable approach to drug discovery. Development of therapeutic strategies that overcome existing resistance mechanisms is important especially against those bacterial infections in which treatment options are limited, such as against multidrug-resistant Gram-negative bacilli. Herein, we provide in vitro data that suggest the addition of anthelmintic salicylanilides, including oxyclozanide, rafoxanide, and closantel, in colistin therapy to treat multidrug-resistant colistin-susceptible but more importantly colistin-resistant Gram-negative bacilli. As a stand-alone agent, the three salicylanilides suffered from limited outer membrane permeation in Pseudomonas aeruginosa, with oxyclozanide also susceptible to efflux. Synergy was apparent for the combinations against multidrug-resistant clinical isolates of P. aeruginosa, Acinetobacter baumannii, Klebsiella pneumoniae, Escherichia coli, and Enterobacter cloacae. Susceptibility breakpoints for colistin, but also with polymyxin B, were reached upon addition of 1 µg ml−1 of the corresponding salicylanilide against colistin-resistant Gram-negative bacilli. Furthermore, enhanced bacterial killing was observed in all combinations. Our data corroborate the repositioning of the three salicylanilides as adjuvants to counter resistance to the antibiotic of last resort colistin. Our findings are timely and relevant since the global dissemination of plasmid-mediated colistin resistance had been realized.
Similar content being viewed by others
Introduction
The escalating incidence of multidrug-resistant (MDR) bacterial infections imposes a serious threat and significant burden to our current healthcare system [1,2,3]. Infections caused by Gram-negative bacteria are arguably difficult to treat due to their inherent resistance mechanisms that include double protective (outer and inner) membrane barriers and overexpressed efflux systems, aside from chromosomal and plasmid resistance genes that they harbor [4, 5]. The dearth of available options to treat MDR Gram-negative bacterial infections drives the development of novel strategies that overcomes existing resistance mechanisms. One strategy that has proven of therapeutic utility is to combine existing antibiotics with helper molecules called adjuvants. Addition of adjuvants to antibiotics results in an enhanced efficacy for the combination. Adjuvants may play an active role in disarming resistance mechanisms against their antibiotic partner. Combinations of β-lactam antibiotics with β-lactamase inhibitors are examples of such strategy, in which the latter are responsible for preventing the degradation/hydrolysis of the former. Adjuvants may also be of chemical entities that possess latent antibacterial activity albeit inactive or poorly active against a pathogen if used alone. For instance, the use of membrane permeabilizers such as ethylenediamine tetraacetic acid [6] and select bioactive peptides [7,8,9] that are capable of disintegrating bacterial membranes at certain (typically high) concentrations. At therapeutic (low) concentrations, these membrane permeabilizers enhance intracellular accumulation of their partner antibiotic. Notably, there are membrane-active antibiotics with potent antibacterial activity that also possess the ability to permeabilize and disrupt bacterial membranes, including the lipopeptides polymyxin B, colistin (polymyxin E), and daptomycin. Lastly, an adjuvant may be a bioactive molecule that induces genotypic/phenotypic changes in the bacterium that render them more susceptible to an antibiotic(s). This cohort of molecules includes bacterial two-component system inhibitors and antivirulence agents.
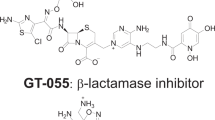
Repurposing nonantibiotic drugs as antibacterial agents and/or adjuvants offers time and cost-effectiveness in comparison to de novo discovery/development. Certainly, the agents approved by the government health agencies such as the United States Food and Drug Administration (FDA) have passed rigorous safety and efficacy evaluations and their pharmacokinetic profiles and liabilities have been well characterized. Therefore, repurposing FDA-approved nonantibiotic drugs for antimicrobial therapy especially against complicated MDR bacterial infections has recently drawn considerable interest [10, 11]. The FDA-approved anthelmintic salicylanilide niclosamide (NIC) had been reported to possess potent activity against Gram-positive bacteria [12, 13]. Our group and others therefore have realized the potential for NIC in antimicrobial therapy. For instance, NIC has been suggested for the treatment of methicillin-resistant Staphylococcus aureus [12], vancomycin-resistant Enterococci [13], and other gut pathogens including Helicobacter pylori [14] and Clostridium difficile [15, 16]. The antibacterial action of NIC, while not fully understood, appears to be through dissipation of the proton motive force that is crucial for bacterial ATP production [14, 17]. NIC displayed poor activity against most Gram-negative bacteria [18, 19] and therefore perceived therapeutic use as an antibacterial agent is limited to only Gram-positive bacteria. However, NIC may be a prospective adjuvant against Gram-negative bacteria, especially those that are MDR. The ability of NIC to quench bacterial quorum sensing and induce phenotypic changes in the Gram-negative bacilli Pseudomonas aeruginosa have been reported [18]. P. aeruginosa is an opportunistic pathogen that commonly infects cystic fibrosis and immunocompromised patients. Naturally, repurposing NIC as an antivirulence agent against P. aeruginosa cystic fibrosis lung infection had been described [20]. Our group also found utility for NIC as an adjuvant in combination with colistin for the treatment of MDR Gram-negative bacillary infections [19]. We found potent synergism between the two agents against MDR clinical isolates of P. aeruginosa, Acinetobacter baumannii, Klebsiella pneumoniae, Escherichia coli, and Enterobacter cloacae. More importantly, 1 µg ml−1 NIC revived and significantly enhanced colistin’s potency against colistin-resistant Gram-negative bacterial isolates, including strains that harbored the mcr-1 gene plasmid [19]. This is important since colistin is an antibiotic of last resort to treat complicated Gram-negative bacterial infections that are nonresponsive to conventional therapy [21], and global dissemination of plasmid-mediated colistin resistance has been realized [22]. Herein, we explored combinations of colistin and other FDA-approved salicylanilides (Fig. 1), albeit currently for veterinary use only, against MDR Gram-negative bacteria. We found that the salicylanilides oxyclozanide (OXY), rafoxanide (RAF), and closantel (CLO) potently synergized with colistin, but also with polymyxin B, against colistin-susceptible but more importantly colistin-resistant Gram-negative bacilli. The three salicylanilides present options to replace NIC for combination therapy with colistin to treat complicated MDR Gram-negative bacterial infections. Our findings support the repurposing of FDA-approved salicylanilides for antimicrobial therapy especially against recalcitrant MDR pathogens. Furthermore, our results suggest that the salicylanilide scaffold may be of use to generate newer derivatives with better activity and/or safer toxicity profile.
Results and discussion
Oxyclozanide, rafoxanide, and closantel synergized with colistin against wild-type Gram-negative bacilli
In line with our recent discovery that the anthelminthic NIC synergized with the lipopeptide colistin in eradicating pathogenic MDR Gram-negative bacilli [19], we wondered whether the same effect can be observed in other FDA-approved salicylanilides. We evaluated three salicylanilides (Fig. 1) that included OXY, RAF, and CLO. While not used to treat tapeworm infections in humans like NIC, these three agents are prescribed for veterinary usage to treat infections caused by internal parasites such as flukes and roundworms in ruminants and other livestock. We initially assessed the activity of the combination against three wild-type (laboratory-reference) Gram-negative bacilli, including P. aeruginosa PAO1, A. baumannii ATCC 17978, and E. coli ATCC 25922, to observe possible synergistic effects devoid of the possibility that this may be due to resistance mechanisms resulting from accumulated mutations or acquired plasmids that a clinical isolate may harbor. Antibacterial activity was measured by minimum inhibitory concentration (MIC), or the lowest concentration of an agent to prevent visible bacterial growth, while synergism between colistin and salicylanilides was determined by fractional inhibitory concentration (FIC) index. The FIC of antibiotic was calculated by dividing the MIC of antibiotic in the presence of adjuvant by the MIC of antibiotic alone. Likewise, the FIC of adjuvant was calculated by dividing the MIC of adjuvant in the presence of antibiotic by the MIC of adjuvant alone. The FIC index was the summation of both FIC values where an FIC index of 0.5, 0.5 < x < 4, or ≥4 was interpreted as synergistic, additive, or antagonistic, respectively.
OXY, RAF, and CLO displayed poor activities as stand-alone agents against all three wild-type Gram-negative bacilli (Table 1). However, all three salicylanilides potentiated the antibacterial activity of colistin against the three tested wild-type Gram-negative bacilli, with FIC indices ranging from 0.023 to 0.251 values (Table 1). This initial finding suggested the therapeutic potential for the combination of colistin with either OXY, RAF or CLO against Gram-negative bacterial pathogens, similar to what we recently reported [19] for NIC.
Efflux affected oxyclozanide but not rafoxanide and closantel in P. aeruginosa
OXY, RAF, and CLO had been reported [12, 23] to display potent antibacterial effect against Gram-positive bacteria. However salicylanilides have fairly limited activity against Gram-negative bacteria [18, 19]. In view of the available literature data, one may postulate that the inactivity of salicylanilides against Gram-negative bacteria is due to either limited permeation of the outer membrane or extensive intracellular expulsion by efflux systems, or both. We recently reported [19] that NIC was a substrate of efflux systems in P. aeruginosa but not of the MexAB-OprM tripartite efflux pump. This finding (Table 2) was apparent since the MIC of NIC against efflux-deficient P. aeruginosa PAO750 strain (2 µg ml−1) was significantly lower in comparison against wild-type P. aeruginosa PAO1 (512 µg ml−1). Strain PAO750 lacked five clinically-relevant efflux pumps (MexAB-OprM, MexCD-OprJ, MexEF-OprnN, MexJK, and MexXY) and the outer membrane protein OpmH. However, the MIC of NIC was unchanged against PAO200, which only lacked the MexAB-OprM efflux system, relative to PAO1 (Table 2).
We then wondered if active efflux could be attributed to the inactivity of OXY, RAF, and CLO in P. aeruginosa. Our microbiological assessment on efflux-deficient strains revealed that OXY was slightly affected by efflux (Table 2). This is apparent by the 4-fold MIC difference of OXY against PAO1 (256 µg ml−1) and PAO750 (64 µg ml−1). Similar to NIC, OXY appeared not to be a substrate of the MexAB-OprM efflux system since its MIC was unchanged against PAO200. However, the comparatively smaller MIC change in OXY, with respect to what was observed in NIC, suggested that other factors aside from efflux may be restricting its activity against Gram-negative bacilli. The MICs of both RAF and CLO were also unchanged against both efflux-deficient strains, suggesting their nonsusceptibility to efflux in P. aeruginosa.
Outer membrane impermeability restricted oxyclozanide, rafoxanide, and closantel from eliciting antibacterial effect in P. aeruginosa
We then evaluated the antibacterial activity of the three salicylanilides against P. aeruginosa PAO1 in the presence of 16 µg ml−1 polymyxin B nonapeptide (PMBN), a well-known polymyxin-derived outer membrane permeabilizer [24] that possessed poor antibacterial activity against Gram-negative bacteria. PMBN perturbs the organization and lipid packing of the outer membrane resulting in a leaky barrier where molecules can easily pass through [25]. Subjecting P. aeruginosa to PMBN will disarm the restrictive outer membrane and allow the entry of salicylanilides into the periplasm, upon which potential antibacterial effect may then be elicited. PMBN alone exhibited poor activity (MIC of 128 µg ml−1) against P. aeruginosa PAO1. In the presence of 16 µg ml−1 PMBN, the activity of OXY, RAF, and CLO became apparent (Table 3). A 16-fold, >64-fold and >128-fold difference in MIC of OXY, RAF, and CLO, respectively, were obtained upon disruption of the restrictive outer membrane barrier of P. aeruginosa. These data confirmed that the activity of the three salicylanilides against P. aeruginosa was greatly limited by their poor outer membrane penetration. Outer membrane impermeability of these salicylanilides can be explained by their respective physicochemical property (Fig. 1) and molecular weight (MW). NIC, OXY, RAF, and CLO are comparatively hydrophobic, due to their conjugated aromatic planar rings, with NIC being relatively polar owing to its nitro substituent (Fig. 1). Conversely, it is widely accepted that large (MW > 600 g mol−1) nonpolar molecules are restricted to cross the water-filled cavity of porin channels in the outer membrane, which is typically used by polar compounds to enter the periplasm [4, 26, 27]. Suggestively, NIC (MW = 327.12 g mol−1) and OXY (MW = 401.46 g mol−1) are able to enter the periplasm through porins, with OXY more limited relative to NIC, only then to be expelled out by efflux pumps; hence their inactivity as a stand-alone agent against Gram-negative bacteria. On the other hand, both RAF (MW = 626.01 g mol−1) and CLO (MW = 663.07 g mol−1) are likely too hydrophobic and bulky to traverse through porins to elicit their antibacterial effect. The lipopolysaccharides and exopolysaccharides studded in the outer membrane of Gram-negative bacteria confer a hydrophilic shield therefore effective passive diffusion of hydrophobic salicylanilides is unlikely; and thus their inability to cross the membrane.
Synergy with colistin was retained in colistin-susceptible multidrug-resistant clinical isolates of Gram-negative bacilli
Combinations of colistin with the three salicylanilides were then evaluated against colistin-susceptible MDR Gram-negative bacilli via checkerboard assay. Firstly, the activity of the combinations was evaluated against seven clinical isolates of MDR P. aeruginosa (Fig. 2 and Supplementary information Table 1). OXY, RAF, and CLO displayed limited activity by themselves against all tested colistin-susceptible Gram-negative bacilli (see Supplementary information Table 1–3). The combinations were synergistic against MDR P. aeruginosa isolates except for two (PA259-96918 and PA260-97103), to which were found only additive effects (see Supplementary information Table 1). In order to compare adjuvant potency, we looked at the fold potentiation of colistin in the presence of either 1 µg ml−1 OXY, RAF or CLO. Fold potentiation is the degree of activity enhancement induced by a fixed concentration of the adjuvant, which is calculated by dividing the MIC of colistin alone by the absolute MIC of colistin in the presence of adjuvant. Out of the seven MDR colistin-susceptible P. aeruginosa, synergy of the combinations were most pronounced in PA095 strain (see Supplementary information Table 1). RAF displayed highest synergism with colistin (FIC index of 0.031 < x < 0.033) against PA095. Colistin’s MIC (0.25 µg ml−1) against PA095 strain was reduced to 0.008 µg ml−1 in the presence of 1 µg ml−1 RAF; hence elicited a 32-fold potentiation (Fig. 2). In fact, RAF appeared to be most effective synergizer of colistin in all tested P. aeruginosa clinical isolates (Fig. 2), followed by CLO then OXY.
Fold potentiation of colistin (COL) by the addition of either 1 µg ml−1 oxyclozanide (OXY), rafoxanide (RAF) or closantel (CLO) against wild-type and colistin-susceptible multidrug-resistant clinical isolates of P. aeruginosa. Note that combinations of three salicylanilides with COL yielded only additive effects against P. aeruginosa PA259-96918 and PA260-97103. Higher concentrations of salicylanilides resulted in higher fold potentiation of COL. (see Supplementary information Table 1 for MIC and FIC values)
We then evaluated the combinations against other colistin-susceptible clinical isolates of Gram-negative bacilli, including A. baumannii (4), K. pneumoniae (1), E. coli (1), and E. cloacae (1). Synergy was observed in all combinations of colistin with the three salicylanilides against all tested MDR A. baumannii strains (see Supplementary information Table 2). Similar to observations in P. aeruginosa, RAF appeared to synergize with colistin the most followed by CLO then OXY (Fig. 3 and Supplementary information Table 2). For instance, a 32-fold MIC potentiation was observed for colistin in the presence of 1 µg ml−1 RAF against A. baumannii AB027 strain (Fig. 3). Conversely, 16-fold and 8-fold MIC potentiation were found upon addition of 1 µg ml−1 CLO and OXY, respectively, to colistin against the same strain. OXY, RAF, and CLO also synergized with colistin against the three colistin-susceptible MDR Enterobacteriaceae (Fig. 3 and Supplementary information Table 3). For instance, 1 µg ml−1 of either OXY, RAF or CLO potentiated colistin’s activity by 16-fold against K. pneumoniae 116381 (Fig. 3). Indeed, all three salicylanilides enhanced colistin’s antibacterial effect towards colistin-susceptible Gram-negative bacilli.
Fold potentiation of colistin (COL) by the addition of either 1 µg ml−1 oxyclozanide (OXY), rafoxanide (RAF) or closantel (CLO) against wild-type and colistin-susceptible multidrug-resistant clinical isolates of A. baumannii and Enterobacteriaceae. Note that all combinations of salicylanilides with COL yielded synergistic effects against all tested strains shown above. Higher concentrations of salicylanilides resulted to higher fold potentiation of COL. (see Supplementary information Tables 2 & 3 for MIC and FIC values)
MIC of colistin in the presence of either oxyclozanide, rafoxanide or closantel was reduced below susceptibility breakpoint against colistin-resistant Gram-negative bacilli
Therapeutic potential for combinations of colistin and the three salicylanilides were further assessed against MDR colistin-resistant Gram-negative bacilli, including P. aeruginosa (3), A. baumannii (1), K. pneumoniae (2), E. coli (2), and E. cloacae (2) clinical isolates. Notably, the two MDR colistin-resistant E. coli in the panel harbor the mcr-1 resistance gene [28]. According to the Clinical and Laboratory Standards Institute (CLSI), the susceptibility breakpoint for colistin against P. aeruginosa and A. baumannii is an MIC of ≤2 µg ml−1 [29]. Bacterial strains that yield an MIC value for a drug above the susceptibility breakpoint are considered to be resistant to such a drug. There is currently no established breakpoint for colistin against Enterobacteriaceae, therefore we cautiously used established values on other Gram-negative bacilli such as P. aeruginosa for interpretation. To this note, all our tested colistin-resistant Gram-negative bacilli possessed an MIC of ≥4 µg ml−1 for colistin (Table 4). The three salicylanilides alone displayed poor activity (Table 4) against all tested colistin-resistant Gram-negative bacilli.
Combinations of colistin with either OXY, RAF or CLO were synergistic against almost all tested MDR colistin-resistant Gram-negative bacilli (Table 4), even against the two mcr-1 gene-positive E. coli strains. The combination of CLO with colistin yielded additive effects only against P. aeruginosa 114228. The absolute MIC of colistin in the presence of 1 µg ml−1 salicylanilides was then compared to assess the relative potencies of the combinations (Table 4). Susceptibility breakpoint for colistin was reached in most clinical isolates, with few exceptions (Table 4). For instance, 1 µg ml−1 of OXY and CLO was not able to reduce the MIC of colistin against P. aeruginosa 114228. Neither 1 µg ml−1 of RAF nor CLO lowered colistin’s MIC below susceptibility breakpoint against both E. cloacae 118564 and 121187 strains. However, significant colistin potentiation was observed in almost all strains. For example, the MIC of colistin was reduced from 1024 µg ml−1 to 0.125, 0.25, and 0.25 µg ml−1 upon addition of 1 µg ml−1 OXY, RAF, and CLO, respectively, against P. aeruginosa 101243 (Table 4). Therefore, up to 8192-fold potentiation was achieved by the addition of 1 µg ml−1 of salicylanilide to colistin (Fig. 4). Similarly, the MIC of colistin was reduced from 16 µg ml−1 to 0.5, 0.5, and 2 µg ml−1 in the presence of 1 µg ml−1 OXY, RAF, and CLO, respectively, against the mcr-1 gene-positive E. coli 94474 (Table 4). In general (Fig. 4), OXY and RAF appeared to potentiate colistin superior to CLO. Strong synergism was also observed in combinations of polymyxin B and either OXY, RAF or CLO against MDR colistin-resistant Gram-negative bacilli (see Supplementary information Table 4), in which OXY and RAF showed superior effects relative to CLO. These surprising and astonishing findings are timely and significant since global colistin resistance dissemination have been recently realized. These data strongly suggest the addition of either OXY, RAF or CLO to colistin monotherapy against MDR and especially colistin-resistant Gram-negative bacilli. Optimization of derivatives to match the pharmacokinetics of colistin or polymyxin B is desirable. Evaluation in in vivo infection models with the optimized analogs prior to clinical development of these combinations would be necessary.
Fold potentiation of colistin (COL) by the addition of either 1 µg ml−1 oxyclozanide (OXY), rafoxanide (RAF) or closantel (CLO) against colistin-resistant multidrug-resistant clinical isolates of P. aeruginosa, A. baumannii, and Enterobacteriaceae. Note that the combination of CLO with COL yielded only additive effects against P. aeruginosa 114228. Higher concentrations of salicylanilides resulted to higher fold potentiation of COL. (see Table 4 for MIC and FIC values)
Addition of oxyclozanide, rafoxanide, and closantel to colistin monotherapy resulted in enhanced bacterial killing
While our checkerboard assay data confirmed that OXY, RAF, and CLO synergized with colistin in vitro, similar to our recent report [19] for NIC, we questioned whether the synergistic combinations can also be confirmed via time-kill kinetics assay. Synergy for this assay denoted to a significantly greater bacterial eradication induced by the combination relative to monotherapy of either components. We previously demonstrated that combinations of colistin (2 µg ml−1) and NIC (1 or 4 µg ml−1) resulted to augmented bacterial killing in colistin-susceptible but more importantly colistin-resistant Gram-negative bacilli, including P. aeruginosa, A. baumannii, K. pneumoniae, E. coli, and E. cloacae [19]. While we extrapolated that similar time-kill kinetics can be observed for OXY, RAF, and CLO, since the three salicylanilides possessed similar chemical structure to NIC, we decided to confirm our hypothesis by performing the time-kill kinetic assay against E. coli 94474. We stressed that this E. coli strain possessed the mcr-1 gene responsible for plasmid-mediated colistin resistance [28], and therefore data reflected in this assay were relevant. Salicylanilide concentration of 1 µg ml−1 was used as the lower adjuvant concentration, since our checkerboard data suggested that this is the optimal concentration for the combination, while 4 µg ml−1 concentration was used as a higher concentration limit. Colistin concentration was chosen to be at the CLSI interpretative susceptibility breakpoint value (2 µg ml−1).
Combinations of colistin with OXY, RAF, or CLO at either 1 or 4 µg ml−1 displayed enhanced bacterial killing (Fig. 5), and therefore synergism. Neither colistin (2 µg ml−1) nor salicylanilides (4 µg ml−1) alone were able to prevent bacterial growth. It appeared that RAF elicited relatively greater effect on colistin’s bactericidal activity than OXY and CLO (Fig. 5). The combination of colistin at higher RAF concentration (4 µg ml−1) achieved complete bacterial eradication after 8 h, as the colony forming units (CFU) of E. coli 94474 was below the detection limit. Complete bacterial eradication was also obtained for the combination of colistin at lower RAF concentration (1 µg ml−1) after 24 h. Similarly, addition of higher concentration CLO (4 µg ml−1) to colistin (2 µg ml−1) resulted to complete eradication after 8 h. However, the combination of colistin with lower CLO concentration (1 µg ml−1) did not exhibit similar potency as CFU of E. coli 94474 were still observed. On a similar report [30], enhanced bacterial killing was demonstrated for the combination of CLO and polymyxin B against colistin-susceptible and colistin-resistant A. baumannii. The combination of colistin (2 µg ml−1) with higher concentration OXY (4 µg ml−1) lowered CFU of E. coli 94474 below the detection limit after 24 h. Similar to CLO, the lower OXY concentration (1 µg ml−1) did not fully eradicate the pathogen. While further time-kill kinetic studies against other Gram-negative bacilli will be assessed for future work, we believe that the data shown in this study are indicative of the potent synergism between colistin and the three salicylanilides. In fact, the time-kill kinetic curves for combinations of colistin with either OXY, RAF or CLO were similar to what we reported for NIC against the same MDR colistin-resistant E. coli 94474 clinical isolate.
Combinations of colistin with either oxyclozanide, rafoxanide or closantel possessed therapeutic potential but with limitations
Our data reported herein revealed the synergistic combination of colistin with either OXY, RAF or CLO against colistin-susceptible but more importantly colistin-resistant Gram-negative bacilli. Most importantly, the three salicylanilides reduced the MIC of colistin against colistin-resistant pathogens below the CLSI susceptibility breakpoint therefore resensitizing them to the antibiotic. Furthermore, enhanced bacterial killing was observed for all the combinations against an E. coli strain harboring the mcr-1 colistin resistance gene plasmid. The degree of adjuvant potency between the three salicylanilides appeared to be RAF > OXY ≥ CLO for combinations against both colistin-susceptible and colistin-resistant Gram-negative bacilli. In perspective to our recently reported data [19], NIC displayed adjuvant potency similar to RAF. The molecular dynamics resulting to synergism between colistin and the three salicylanilides is most likely similar to what we have reported for colistin and NIC. Since our data revealed that OXY, RAF, and CLO suffered from limited outer membrane penetration (with OXY also susceptible to active efflux), we believe that colistin potentiated the three salicylanilides by permeabilizing and perturbing the outer membrane that effectively enhanced their intracellular accumulation. Conversely, the three salicylanilides, owing to very similar chemical structures to NIC, may elicit similar genetic/phenotypic responses in the bacterium that result in an enhanced susceptibility to colistin (may likely be responsible for colistin potentiation in colistin-resistant strains). While the latter is reported for NIC [18], further genetic investigation with RAF, OXY, and CLO is needed for future work to confirm this hypothesis. The synergistic combination of colistin and the three salicylanilides certainly warrant further investigation.
An apparent advantage for further pursuing these combinations for treatment against Gram-negative bacterial infections is that all components, including the three salicylanilides, are FDA-approved drugs and that their pharmacological profile is well characterized. Certainly, repurposing existing nonantibiotic drugs for antibiotic therapy offer a low sk and cost approach relative to de novo drug discovery/development. However, toxicity and poor plasma concentration/bioavailability limits these combinations for systemic applications. Colistin, among other polymyxins, is known to be nephrotoxic and neurotoxic and thus regarded as drugs of last resort for MDR Gram-negative bacterial infections nonresponsive to conventional antibiotic treatment. Therefore, partner agents that significantly lower the required dose of colistin to eradicate the pathogen are needed, especially now that plasmid-mediated colistin resistance had globally disseminated. We disclosed herein that OXY, RAF, and CLO certainly are able to reduce the needed colistin concentration to eradicate colistin-susceptible but more importantly colistin-resistant Gram-negative bacilli. However, the three salicylanilides have been described to induce moderate cytotoxicity. The CC50, or the concentration to reduce cell viability to 50%, for OXY, RAF, and CLO was reported to be 8, 16, and 16 µg ml−1, respectively, against human kidney HEK 293 T/17 cells [16]. Similar CC50 values were found for the three salicylanilides against human liver HepG2 cells [16]. However, it should be noted that NIC displayed much greater cytotoxic effects towards human kidney HEK293T/17 and human liver HepG2 cells with CC50 values of 0.25 µg ml−1 for both [16]. Aside from possible cytotoxicity concerns, the three salicylanilides have limited systemic availability. Plasma concentrations obtained following oral administration of OXY (15 mg kg−1), RAF (7.5 mg kg−1), and CLO (7.5 mg kg−1) to sheep (n = 5) were reported [31] to be 19.0 ± 2.3 µg ml−1, 23.0 ± 2.4 µg ml−1, and 48.0 ± 4.6 µg ml−1, respectively. However, all the three salicylanilides were found to be extensively (>99%) bound to plasma proteins that greatly limit their ability to elicit therapeutic effect [31]. To circumvent these problems, we foresee colistin in combination with either of the three salicylanilides being developed for topical applications to treat complicated bacterial infections. Indeed, there is an urgent need to develop therapeutic strategies that overcome bacterial resistance especially against those antibiotics of last resort such as colistin. Our findings positioned the combination of colistin with salicylanilides as a potential strategy that may address the issue of antimicrobial resistance in Gram-negative bacilli. Furthermore, repurposing FDA-approved nonantibiotic drugs as adjuvants to existing antibiotics may hold key for future treatment of MDR bacterial infections. While drug repurposing strategy has its own merits, scientific ingenuity should not only be bound to commercially-available salicylanildes like NIC, OXY, RAF, and CLO. New derivatives may be generated from the salicylanilide scaffold with improved pharmacokinetic properties and reduced toxicity. Our findings position the combination of colistin with salicylanilides as a potential strategy that may address the issue of antimicrobial resistance in Gram-negative bacilli.
Materials and methods
General
Antibiotics and salicylanilides in this study were obtained from commercial sources. Bacterial strains in this study were acquired from either the American Type Culture Collection (ATCC) or the Canadian Ward Surveillance (CANWARD) study [32]. Bacterial isolates from CANWARD were isolated from clinical specimens collected from patients suffering a presumed infectious diseases admitted in a participating medical center across Canada. Two MDR colistin-resistant E. coli strains in this study have been described to harbor the plasmid-mediated colistin resistance gene mcr-1 [28]. Efflux-deficient P. aeruginosa PAO200 lacked the MexAB-OprM efflux system while PAO750 lacked five clinically-relevant pumps (MexAB-OprM, MexCD-OprJ, MexEF-OprN, MexJK, and MexXY) and the outer membrane protein OpmH. Prior to conducting experiments, bacterial isolates were grown overnight in lysogeny/luria broth (LB) on an incubator shaker at 37 °C.
Antimicrobial susceptibility assay
Antibacterial activity of the tested agents in vitro was evaluated by microbroth dilution susceptibility testing according to the CLSI guidelines [29]. Overnight grown bacterial cultures were diluted in saline to achieve a 0.5 McFarland turbidity. Subsequently, the diluted bacterial culture was then further diluted 1:50 in Mueller-Hinton broth (MHB) for inoculation to a final concentration of approximately 5 × 105 CFU/ml. Experiments were performed on 96-well plates where the tested agents were 2-fold serially diluted in MHB and incubated with equal volumes of bacterial inoculum at 37 °C for 18 h. MIC values for tested agents were determined as the lowest concentration to inhibit visible bacterial growth in the form of turbidity, which was confirmed via EMax Plus microplate reader (Molecular Devices, USA) at 590 nm wavelength. Wells with or without bacterial cells were used as positive or negative controls, respectively.
Checkerboard assay
Experiments were performed on 96-well plates as previously described [7, 33]. The antibiotic of interest was 2-fold serially diluted along the x-axis, while the salicylanilide was 2-fold serially diluted along the y-axis to create a matrix where each well consisted of a combination of both agents at different concentrations. Overnight grown bacterial cultures were then diluted in saline to 0.5 McFarland turbidity, subsequently followed by 1:50 further dilution in MHB and inoculation on each well to achieve a final concentration of approximately 5 × 105 CFU ml−1. Wells consisting of MHB with or without bacterial cells were used as positive or negative controls, respectively. The 96-well plates were then incubated at 37 °C for 18 h and examined for visible turbidity, which was confirmed using an EMax Plus microplate reader (Molecular Devices, USA) at 590 nm wavelength. FIC of the antibiotic was calculated by dividing the MIC of antibiotic in the presence of salicylanilide by the MIC of antibiotic alone. Similarly, FIC of salicylanilide was calculated by dividing the MIC of salicylanilide in the presence of antibiotic by the MIC of salicylanilide alone. The FIC index was the summation of both FIC values. An FIC index of ≤0.5, 0.5 < x < 4, or ≥4 was interpreted as synergistic, additive, or antagonistic, respectively.
Time-kill kinetics assay
The kinetics of bacterial killing was evaluated as previously described [34] with minor modifications. Overnight grown bacterial culture was diluted in saline to 0.5 McFarland turbidity followed by further 1:50 dilution in LB broth. The cell culture was incubated at 37 °C with either colistin, salicylanilide or combinations thereof at desired concentrations, to result in sets of culture tubes per designated time intervals. Then, a 100 µl aliquot was obtained from each tubes at specified time interval and plated on LB agar plates following serial dilution in phosphate-buffered saline (pH 7.2). Bacterial colonies were counted from the plates after incubation for 18 h at 37 °C.
References
Klemm EJ, Wong VK, Dougan G. Emergence of dominant multidrug-resistant bacterial clades: lessons from history and whole-genome sequencing. Proc Natl Acad Sci USA. 2018;115:12872–7.
Schwartz KL, Morris SK. Travel and the spread of drug-resistant bacteria. Curr Infect Dis Rep. 2018;20:29.
Guitor AK, Wright GD. Antimicrobial resistance and respiratory infections. Chest. 2018;154:1202–12.
Domalaon R, Idowu T, Zhanel GG, Schweizer F. Antibiotic hybrids: the next generation of agents and adjuvants against Gram-negative pathogens? Clin Microbiol Rev. 2018;31:pii:e00077–17.
Koulenti D et al. Infections by multidrug-resistant Gram-negative bacteria: what’s new in our arsenal and what’s in the pipeline? Int J Antimicrob Agents. 2018;53:211–224. https://doi.org/10.1016/j.ijantimicag.2018.10.011
Liu Z, et al. In vitro and in vivo activity of EDTA and antibacterial agents against the biofilm of mucoid Pseudomonas aeruginosa. Infection. 2017;45:23–31.
Domalaon R et al. Dilipid ultrashort cationic lipopeptides as adjuvants for chloramphenicol and other conventional antibiotics against Gram-negative bacteria. Amino Acids. 2018;51:383–393. https://doi.org/10.1007/s00726-018-2673-9
Domalaon R, Zhanel GG, Schweizer F. Short antimicrobial peptides and peptide scaffolds as promising antibacterial agents. Curr Top Med Chem. 2016;16:1217–30.
Domalaon R et al. Short proline-rich lipopeptide potentiates minocycline and rifampin against multidrug- and extensively drug-resistant Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2018;62:pii:e02374-17.
Das S, Dasgupta A, Chopra S. Drug repurposing: a new front in the war against Staphylococcus aureus. Future Microbiol. 2016;11:1091–9.
Hennessy E, Adams C, Reen FJ, O’Gara F. Is there potential for repurposing statins as novel antimicrobials? Antimicrob Agents Chemother. 2016;60:5111–21.
Rajamuthiah R, et al. Repurposing salicylanilide anthelmintic drugs to combat drug resistant Staphylococcus aureus. PLoS ONE. 2015;10:e0124595.
Mohammad H, AbdelKhalek A, Abutaleb NS, Seleem MN. Repurposing niclosamide for intestinal decolonization of vancomycin-resistant Enterococci. Int J Antimicrob Agents. 2018;51:897–904.
Tharmalingam N, Port J, Castillo D, Mylonakis E. Repurposing the anthelmintic drug niclosamide to combat Helicobacter pylori. Sci Rep. 2018;8:3701.
Tam J, et al. Host-targeted niclosamide inhibits C. difficile virulence and prevents disease in mice without disrupting the gut microbiota. Nat Commun. 2018;9:5233.
Gooyit M, Janda KD. Reprofiled anthelmintics abate hypervirulent stationary-phase Clostridium difficile. Sci Rep. 2016;6:33642.
Chen W, Mook RAJ, Premont RT, Wang J. Niclosamide: beyond an antihelminthic drug. Cell Signal. 2018;41:89–96.
Imperi F, et al. New life for an old drug: the anthelmintic drug niclosamide inhibits Pseudomonas aeruginosa quorum sensing. Antimicrob Agents Chemother. 2013;57:996–1005.
Domalaon R, De Silva PM, Kumar A, Zhanel GG, Schweizer F. The anthelmintic drug niclosamide synergizes with colistin and reverses colistin resistance in Gram-negative bacilli. Antimicrob Agents Chemother. In press, manuscript accepted (AAC02574-18R1). 2019;63:pii:02574-18.
Costabile G, et al. Toward repositioning niclosamide for antivirulence therapy of Pseudomonas aeruginosa lung infections: development of inhalable formulations through nanosuspension technology. Mol Pharm. 2015;12:2604–17.
Bergen PJ, et al. Polymyxin combinations: pharmacokinetics and pharmacodynamics for rationale use. Pharmacotherapy. 2015;35:34–42.
Liu YY, et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect Dis. 2016;16:161–8.
Rajamuthiah R, et al. Whole animal automated platform for drug discovery against multi-drug resistant Staphylococcus aureus. PLoS ONE. 2014;9:e89189.
Domalaon R, Berry L, Tays Q, Zhanel GG, Schweizer F. Development of dilipid polymyxins: investigation on the effect of hydrophobicity through its fatty acyl component. Bioorg Chem. 2018;80:639–48.
Sahalan AZ, Dixon RA. Role of the cell envelope in the antibacterial activities of polymyxin B and polymyxin B nonapeptide against Escherichia coli. Int J Antimicrob Agents. 2008;31:224–7.
Pages J-M, James CE, Winterhalter M. The porin and the permeating antibiotic: a selective diffusion barrier in Gram-negative bacteria. Nat Rev Microbiol. 2008;6:893–903.
Chevalier S, et al. Structure, function and regulation of Pseudomonas aeruginosa porins. FEMS Microbiol Rev. 2017;41:698–722.
Walkty A, et al. Frequency of MCR-1-mediated colistin resistance among Escherichia coli clinical isolates obtained from patients in Canadian hospitals (CANWARD 2008–2015). CMAJ Open. 2016;4:E641–E645.
The Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing CLSI supplement M100S. 26th ed. Wayne, PA: Clinical and Laboratory Standards Institute; 2016.
Tran TB, et al. Anthelmintic closantel enhances bacterial killing of polymyxin B against multidrug-resistant Acinetobacter baumannii. J Antibiot. 2016;69:415–21.
Mohammed-Ali NA, Bogan JA. The pharmacodynamics of the flukicidal salicylanilides, rafoxanide, closantel and oxyclosanide. J Vet Pharmacol Ther. 1987;10:127–33.
Zhanel GG, et al. Antimicrobial susceptibility of 22746 pathogens from Canadian hospitals: results of the CANWARD 2007–11 study. J Antimicrob Chemother. 2013;68(Suppl 1):7–22.
Domalaon R, Yang X, Lyu Y, Zhanel GG, Schweizer F. Polymyxin B3-tobramycin hybrids with Pseudomonas aeruginosa-selective antibacterial activity and strong potentiation of rifampicin, minocycline, and vancomycin. ACS Infect Dis. 2017;3:941–54.
Lyu Y, et al. Amphiphilic tobramycin-lysine conjugates sensitize multidrug resistant Gram-negative bacteria to rifampicin and minocycline. J Med Chem. 2017;60:3684–702.
Acknowledgements
This work was supported by the Natural Sciences and Engineering Research Council of Canada NSERC-DG (2018-06047) and the University of Manitoba. We thank Dr. Ayush Kumar (University of Manitoba) for generously providing access to efflux-deficient P. aeruginosa strains PAO200 and PAO750.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Domalaon, R., Okunnu, O., Zhanel, G.G. et al. Synergistic combinations of anthelmintic salicylanilides oxyclozanide, rafoxanide, and closantel with colistin eradicates multidrug-resistant colistin-resistant Gram-negative bacilli. J Antibiot 72, 605–616 (2019). https://doi.org/10.1038/s41429-019-0186-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41429-019-0186-8
This article is cited by
-
Prospects of Using Pharmacologically Active Compounds for the Creation of Antimycobacterial Drugs
Pharmaceutical Chemistry Journal (2022)
-
Natural Inhibitors of Quorum-Sensing Factors: a Novel Strategy to Control Pathogenic Bacteria
Revista Brasileira de Farmacognosia (2020)