Abstract
Immune checkpoint blockade therapy has become a major weapon in fighting cancer. Antibody drugs, such as anti-PD-1 and anti-PD-L1, demonstrate obvious advantages such as broad applicability across cancer types and durable clinical response when treatment is effective. However, the overall response rates are still unsatisfying, especially for cancers with low mutational burden. Moreover, adverse effects, such as autoimmune symptoms and tumor hyperprogression, present a significant downside in some clinical applications. These challenges reflect the urgent need to fully understand the basic biology of immune checkpoints. In this review, we discuss regulation of immune checkpoint signaling at multiple levels to provide an overview of our current understanding of checkpoint biology. Topics include the regulation of surface expression levels for known immune checkpoint proteins via surface delivery, internalization, recycling, and degradation. Upon reaching the surface, checkpoints engage in both conventional trans and also cis interactions with ligands to induce signaling and regulate immune responses. Novel therapeutic strategies targeting these pathways in addition to classical checkpoint blockade have recently emerged and been tested in preclinical models, providing new avenues for developing next-generation immunotherapies.
Similar content being viewed by others
Introduction
The tumor microenvironment (TME) is infiltrated with many types of innate and adaptive immune cells whose immune surveillance functions are often suppressed by multiple mechanisms in a context-dependent manner.1,2 Signaling suppression and metabolic suppression represent two major causes of immune suppression, and the prior will be discussed here. Signaling suppression is reflected by the ways that tumor cells downregulate the activity of stimulatory immunoreceptors while upregulating the activity of inhibitory immunoreceptors. Using T cells as an example, tumor cells can tune down T cell receptor (TCR)-mediated stimulatory signaling by downregulating surface MHC-I level.3 On the other hand, tumor cells can tune up PD-1-mediated inhibitory signaling by upregulating surface PD-L1 level.4 The concept that blocking the activation of inhibitory immunoreceptors can reinvigorate antitumor function of immune cells has been demonstrated experimentally and translated to treatment of many types of cancer in the clinic.5,6
A number of inhibitory immunoreceptors have been identified and studied in cancer in past decades, including but not limited to PD-1, CTLA-4, LAG3, TIM3, TIGIT and BTLA. They are named as “immune checkpoints” referring to molecules that act as gatekeepers of immune responses. In the evolutionary process, immune checkpoints have co-evolved with stimulatory immunoreceptors and appear as early as in fish.7 These receptors often use mono-tyrosine signaling motifs, such as immunoreceptor tyrosine-based inhibitory motif (ITIM) and immunoreceptor tyrosine-based switch motif (ITSM), to deliver inhibitory signals. As surface molecules, their activity can be easily inhibited by blocking antibodies that prevent ligand-receptor engagement. The most successful immune checkpoint blockade therapy is anti-PD-1/PD-L1 therapy that has been approved to treat a wide variety of cancer types, such as blood, skin, lung, liver, bladder and kidney cancers.6 Immune checkpoint blockade therapy often leads to more durable response than chemo or targeted therapies, perhaps reflecting the memory feature of the immune system. However, as clinical data accumulates worldwide, drawbacks and side effects have begun to be revealed. The major bottleneck of immune checkpoint blockade therapy is its low response rate in most cancers, with a range of 10%–30%.6 For some major cancer types such as colorectal cancer with microsatellite stability, anti-PD-1/PD-L1 therapy shows nearly no effect.8 Mechanisms of non-responsiveness have been extensively studied, and many factors have been found to be relevant, such as tumor mutational burden, PD-L1 expression level, IFN signaling and MHC-I loss.9,10,11,12 However, biomarkers that faithfully predict efficacy are still lacking. Better understanding of checkpoint biology is therefore urgently needed to design next-generation therapies and to improve clinical protocols of current therapies.
In recent years, many biochemical and biophysical studies have revealed sophisticated regulation of checkpoint surface expression. Upon ligand engagement, different checkpoints show distinct signaling mechanisms to suppress antitumor immunity. Here we review these fundamental discoveries and highlight new targeting strategies with potential for clinical translation.
Surface level regulation of immune checkpoints
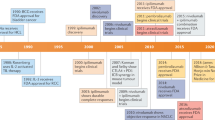
High surface level of checkpoints is a hallmark of TME, but the underlying mechanisms are poorly understood. As membrane proteins, immune checkpoints are expressed in the endoplasmic reticulum (ER) and then delivered to cell surface to exert their inhibitory functions, which involves sequential transportation through Golgi apparatus and secretory vesicle by the protein-sorting system. During surface delivery, glycosylation serves as a quality control to ensure only mature and functional immune checkpoints are delivered to cell surface.13,14 After reaching the cell surface, immune checkpoints are subjected to internalization and recycling, which offer a rapid regulatory pathway to modulate their surface levels.15,16 Ubiquitination-mediated protein degradation is another crucial mechanism to control protein level and immune checkpoints can be ubiquitinated and sorted to proteasome or lysosome for degradation. These cellular processes together determine surface level of immune checkpoints to shape cell signaling (Fig. 1).
a Fut8-mediated core fucosylation pathway is required for PD-1 surface expression. Internalized PD-1 is ubiquitinated by FBXO38 for proteasomal degradation and can also be recycled to surface with the help of TOX in liver cancer microenvironment. b STT3-catalyzed N-glycosylation stabilizes PD-L1 surface expression. P-S195-induced abnormally glycosylation of PD-L1 causes ERAD. Internalized PD-L1 is either sorted to the lysosome by HIP1R for degradation or recycled to the cell surface with the help of CMTM6/4. PD-L1 is ubiquitinated by different E3 ligases (HRD1, Cullin3-SPOP, β-TrCP and STUB1) under different contexts, and deubiquitinated by CNS5. Palmitoylation of PD-L1 by DHHC3 suppresses its mono-ubiquitination and lysosomal degradation. c Mgat1 mediates CTLA-4 N-glycosylation and surface retention. Trafficking of CTLA-4 to the cell surface relies on the TRIM/LAX/Rab8 complex and PLD/ARF1-dependent exocytosis. Rapid CTLA-4 internalization is mediated by AP-2 binding to the unphosphorylated YVKM motif. Internalized CTLA-4 is either degraded in the lysosome or recycled to cell surface by LRBA. CTLA-4 in TGN can also be delivered to the lysosome for degradation through AP-1 binding.
PD-1 regulations
Human PD-1 contains four N-linked glycosylation sites at its extracellular IgV domain: N49, N58 (N54 in mouse PD-1), N74, and N116. The structure of PD-1 shows that the glycan at N58 consists of two N’acetylglucosamines and one fucose.17 Furthermore, whole genome CRISPR screening identified that the core fucosylation pathway directly regulates PD-1 surface level.18 Mass spectrometry analysis showed that all four N-glycosylation sites had core fucose modification. Mutation of N49 or N74 caused dramatic decrease of surface PD-1 level. Genetic ablation of the core fucosyltransferase 8 (Fut8) reduced PD-1 surface level and enhanced T cell activation.18 How glycosylation regulates PD-1 expression level is still unknown. Sugar groups might regulate PD-1 folding and thus affect the quality control process at the ER. Another possible role of glycosylation is the regulation of ligand binding.19 Different microenvironment cues such as hypoxia20 and nutrient stress21 might cause different glycosylation patterns of PD-1, which can in turn affect PD-1 function. More mass spectrometry studies are warranted in the future to understand the “sugar code” of PD-1 and its functional meaning in specific disease contexts.
Internalization of surface PD-1 has been observed by fluorescence imaging22 but it is still unknown whether conventional clathrin-mediated endocytosis is involved in PD-1 internalization. Internalized PD-1 molecules can either recycle back to the cell surface or become ubiquitinated and sorted to proteasome for degradation (Fig. 1a). In liver cancer infiltrating CD8+ T cells, the thymocyte selection-associated high mobility group box protein (Tox), a master transcription factor of T cell exhaustion,23 was shown to exert a nonconventional function of binding with PD-1 in the cytoplasm and facilitating PD-1 recycling.24 Whether Tox also regulates PD-1 recycling in other contexts has not been tested. A specific E3 ubiquitin ligase of PD-1, named F-box protein 38 (FBXO38), has been identified and validated by biochemical and animal experiments. As a part of the Skp, Cullin, F-box containing complex (SCF complex), FBXO38 can mediate K48 polyubiquitination at a conserved lysine site (K233 in human PD-1). Interestingly, polyubiquitinated PD-1 is sorted to the proteasome rather than the lysosome for degradation. This is unusual, as most membrane proteins are internalized and degraded via the lysosome. In the TME, the FBXO38-mediated PD-1 degradation pathway is deficient because of the low transcriptional level of FBXO38. TCR signaling without concomitant CD28 signaling was found to be the cause of FBXO38 downregulation.22 Persistent exposure to tumor antigen and low CD80/86 expression on tumor cells25 therefore could explain the reduced FBXO38 expression in TILs. Furthermore, IL-2, the major growth factor of T cells, can rescue FBXO38 level in tumor-infiltrating T cells via STAT5-mediated transcriptional regulation.22 Notably, FBXO38 expression levels in tumor infiltrating lymphocytes (TILs) are even lower than in naïve T cells. How chronic TCR signaling downregulates FBXO38 transcription is still an open question.
Indeed, in general the processes governing internalization and concomitant degradation or recycling of PD-1 molecules remain poorly understood. Several interesting questions warrant further investigation such as whether PD-1 internalization is signaling-dependent and which signal determines the fate of internalized PD-1, as to whether it is delivered to the proteasome for degradation or recycled back to the cell surface for future usage. These questions are better understood for PD-L1 in cancer cells, as described in the following section.
PD-L1 regulations
PD-L1 (also named as CD127, B7-H1) also contains four N-glycosylation sites: N35, N192 (N191 in mouse PD-L1), N200 (N199 in mouse PD-L1), and N219 (N218 in mouse PD-L1). These modifications are significant for PD-L1 protein stability. STT3 is an ER-associated N-glycosyltransferase that catalyzes the first step of protein N-glycosylation. In cancer stem-like cells, STT3-dependent N-glycosylation stabilized and upregulated PD-L1 level, which was required for epithelial–mesenchymal transition (EMT)-induced enrichment of PD-L1.26 Conversely, phosphorylation of PD-L1 S195 by AMP-activated protein kinase (AMPK) induced abnormal glycosylation of PD-L1 and blocked its ER to Golgi transportation, resulting in ER-associated degradation (ERAD).27 In the cases of some cancer cells, the glycan modification rendered PD-L1 undetectable by conventional antibodies, which led to misinterpretation of PD-L1 surface level.28 Removal of N-glycosylation led to more faithful detection of PD-L1 surface level.28 This finding reflects the fact that glycosylation patterns of PD-L1 can vary in different cancer cells, which might be due to their different microenvironments,29 and some patterns prevent binding of conventional antibodies.
Surface PD-L1 undergoes constant internalization, followed by recycling or degradation (Fig. 1b). A chaperone protein, CKLF-like MARVEL transmembrane domain containing 6 (CMTM6) that belongs to a family of eight MARVEL domain-containing proteins with previously unknown function, regulates PD-L1 recycling. CMTM6 associates with PD-L1 at both the plasma membrane and endosomes to facilitate recycling and also inhibits ubiquitination and degradation by the lysosome. Tumor cells with CMTM6 deficiency showed reduced PD-L1 recycling and surface level, leading to less suppression of T cell activity.30 CMTM4, an analog of CMTM6, also has a similar function.31 How CMTM6/4 supports PD-L1 recycling remains undefined. Multiple proteins were identified to regulate lysosome degradation of PD-L1. HIP1R carries a lysosome sorting motif, and its binding with PD-L1 targets PD-L1 to the lysosome with the help of the AP complex and ALIX/ESCRT.32 It was suggested that STUB1 E3 ubiquitin ligase can mediate PD-L1 degradation in the lysosome.30,31 Whether STUB1 cooperates with HIP1R is still unknown. According to the work from several groups, the proteasome is also involved in PD-L1 degradation. Cullin 3-SPOP, β-TrCP, and HRD1 E3 ligases were reported to regulate PD-L1 ubiquitination and proteasomal degradation, and they seem to regulate PD-L1 degradation in different contexts. During cell cycling, PD-L1 surface level showed evident fluctuations, peaking in M and early G1 phases and quickly declining in late G1 and S phases. This fluctuation was regulated by the cyclin D-CDK4-SPOP-FZR1 signaling pathway. CDK4 phosphorylated and stabilized SPOP, an adaptor protein in the Cullin 3-based E3 ubiquitin ligase complex, to mediate PD-L1 polyubiquitination and degradation by the proteasome.33 Interestingly, glycosylation can directly affect PD-L1 ubiquitination and degradation through β-TrCP and HRD1. When PD-L1 was not glycosylated, it can be phosphorylated by glycogen synthase kinase 3β (GSK3β) at T180 and S184 and recruit β-TrCP to mediate PD-L1 ubiquitination and degradation.34 On the other hand, S195 phosphorylation caused abnormal glycosylation of PD-L1, which resulted in recruitment of HRD1 to trigger ER-associated degradation.27
There are also sophisticated mechanisms antagonizing PD-L1 ubiquitination and degradation. COP9 signalosome 5 (CSN5) was reported to deubiquitinate PD-L1, thereby inhibiting PD-L1 degradation. NF-κB pathway activated by TNF-α induced CSN5 expression to stabilize PD-L1 expression in cancer cells.35 Palmitoylation of PD-L1 at C272 by DHHC3 blocked mono-ubiquitination of PD-L1 and the subsequent ESCRT-mediated trafficking to multivesicular bodies (MVB), resulting in suppression of PD-L1 lysosomal degradation.36
CTLA-4 regulation
Differing from PD-1 whose primary location is at the plasma membrane, CTLA-4 is mainly localized in intracellular compartments. Upon T cell activation, CTLA-4 translocates to the cell surface to mediate its inhibitory function.37 T cell receptor-interacting molecule (TRIM) is required for CTLA-4 trafficking from the trans Golgi network (TGN) to the cell surface. TRIM knockdown led to retention of CTLA-4 in the TGN.38 A subsequent study showed that a CTLA-4/TRIM/LAX/Rab8 complex was essential for this trafficking pathway.39 Phospholipase D (PLD)- and ADP ribosylation factor-1 (ARF1)-dependent exocytosis was also reported to trigger the trafficking of CTLA-4 to the cell surface.40
Surface CTLA-4 molecules are rapidly internalized to maintain relatively low surface levels (Fig. 1c). The clathrin-associated adaptor complex AP-2 binds to the YVKM motif in the CTLA-4 cytoplasmic domain to mediate internalization, which can be prevented by YVKM phosphorylation41. However, another study showed that YVKM-mediated CTLA-4 internalization was not impaired during T cell activation, thus suggesting that YVKM phosphorylation might not regulate CTLA-4 internalization directly.42 Another clathrin adaptor complex, AP-1, also binds to the YVKM motif, but differs in that it shuttles CTLA-4 from the TGN to lysosomes for degradation.43 Additionally, the internalization rate of CTLA-4 is also regulated by N-glycosylation. Vitamin D3 treatment enhanced N-acetylglucosaminyltransferase I (Mgat1) expression and N-glycan branching, leading to reduced internalization and increased surface level of CTLA-4 in T cells.44 N-glycosylation is also essential for CTLA-4 surface delivery. A T17A polymorphism in the signal peptide led to insufficient glycosylation and lower CTLA-4 surface level.45 TCR signaling was shown to increase hexosamine metabolism and N-glycan-branching pathway, therefore increasing CTLA-4 glycosylation and surface expression.46 Internalized CTLA-4 in endosomes can be recycled back to the cell surface.42 LPS responsive beige-like anchor protein (LRBA) co-localizes with CTLA-4 in recycling endosomes to assist its recycling. LRBA mutation in human patients reduces CTLA-4 levels in regulatory and conventional T cells, which leads to the phenotypes of autoimmunity, lymphoproliferation, and humoral immune deficiency.47
Checkpoint signaling mechanisms
The suppressive functions of immune checkpoints usually depend on ligand-induced signaling. Here we summarize ligand interactions and signaling mechanisms of several well studied immune checkpoints (Fig. 2).
a PD-L1 and PD-L2 are ligands for PD-1. PD-1 recruits protein tyrosine phosphatase SHP2/SHP1 via phosphorylated ITSM/ITIM, which in turn inhibits both TCR and CD28 signaling. SAP inhibits SHP2 activity to suppress PD-1 signaling. Both PD-1 and CD80 interact with PD-L1 in cis to restrict its trans ligation of PD-1. b CTLA-4 competes with CD28 on binding with CD80/86 binding to inhibit CD28 signaling. The phosphorylated YVKM motif of CTLA-4 recruits SHP2 to inhibit RAS. CTLA-4 also inhibits AKT activity through PP2A. CTLA-4 in Tregs reduces CD80/86 on APCs by trans-endocytosis, which requires KxxKKR motif and PKCη. c TIM3 expresses in both T cells and innate immune cells. Four known ligands have been identified: Ceacam1, Galectin9, HMBG1, and PS. Galectin9 binds to glycosylated IgV domain of TIM3 in T cells. Ceacam1 exhibits both cis and trans interactions. Cis interaction of Ceacam1 with TIM3 is essential for TIM3 surface expression in T cells. In the absence of ligands, Bat3 binds to unphosphorylated Y256/263 in TIM3 cytoplasmic domain and recruits active Lck to deliver stimulatory signal in T cells. Interaction with Galectin9/Ceacam1 leads to phosphorylation of TIM3 Y256/263 and the subsequent abolishment of Bat3 binding, thus converting TIM3 from a stimulatory to an inhibitory molecule. TIM3 in DCs binds with PS and HMBG1 to regulate innate immunity. d LAG3 binds to MHC-II to inhibit CD4-dependent T cell function with its cytoplasmic domain. TME-derived Galectin3, LSECtin and FGL1 bind with LAG3 to inhibit T cell function, which requires the KIEELE motif in the LAG3 cytoplasmic domain. TCR signaling upregulates activity of ADAM10 and ADAM17, which cleave LAG3 at the extracellular domain to abolish its suppression of T cell signaling. e TIGIT and CD226 bind to the same ligands, CD112 and CD155. CD226 is a co-stimulatory receptor whereas TIGIT is a co-inhibitory receptor. TIGIT binds with CD112/CD155 with higher affinity than CD226 and inhibits the PI3K, MAPK and NF-κB pathways by recruiting SHIP1. f BTLA interacts with HVEM both in trans and cis. The cis interaction between BTLA and HVEM inhibits the trans-ligation of HVEM by LIGHT and thus inhibits HVEM stimulatory signaling triggered by LIGHT binding. ITIM and ITSM in BTLA recruit SHP1/SHP2 to inhibit both TCR and CD28 signaling.
PD-1 signaling
PD-1 signaling can be triggered by its engagement with the ligands PD-L1 and PD-L2. Conventionally, PD-L1 or PD-L2 expressed on the surface of antigen presenting cells or tumor cells engages in trans interactions with PD-1 expressed on the surface of T cells to induce inhibitory signaling.48,49,50 Tumor cells can also secrete PD-L1-containing extracellular vesicles, mainly in the form of exosomes, to activate PD-1 pathway. These exosomal PD-L1 molecules primarily suppress T cell activity in the draining lymph node. Melanoma patients who were not responsive to anti-PD-1 therapy showed higher levels of exosomal PD-L1 than responders.51,52 Recent studies show that the PD-1/PD-L1 interaction can also occur in cis. The co-expression and interaction between PD-L1 and PD-1 on APCs prevented the trans-ligation of PD-1, thus decreasing the inhibitory function of T cell PD-1.53 In addition to PD-1, PD-L1 can interact with CD80 in cis,54,55,56 which can disrupt PD-L1/PD-1 and CD80-CTLA-4 interactions but preserve the ability of CD80 to activate CD28 signaling.56,57 Thus, the cis PD-L1-CD80 interaction plays positive roles in antitumor immunity by inhibiting PD-1 and CTLA-4 function.
After ligand engagement, PD-1 becomes phosphorylated to deliver inhibitory function (Fig. 2a). An ITIM and an ITSM are present in its cytoplasmic domain. The phosphorylated ITSM might be more important, as mutation of tyrosine in ITSM but not ITIM, significantly abrogated the inhibitory function of PD-1.58,59,60 Phosphorylated ITSM primarily recruits SHP2 to dephosphorylate key signaling molecules to downmodulate activation level.61,62,63 Although ITIM is usually considered to be dispensable for PD-1 inhibitory function, recent studies suggested that ITIM plays a role in converting SHP2 from inactive to active conformation.64,65 Signaling lymphocytic activation molecule-associated protein (SAP) was shown to block SHP2 interaction with its substrate and thus could inhibit PD-1 signaling.64 Although SHP2 is essential for PD-1 inhibitory signaling in most cases, Shp2-deficient T cells can still acquire dysfunctional features and respond to α-PD-1 treatment in vivo, suggesting an alternative signaling mechanism.62 Several groups reported that SHP1 can also be recruited by phosphorylated PD-1 ITSM.59,66 A recent study applied mass spectrometry to quantitatively illustrate PD-1 signalosome assembly.63 They found that SHP2 was predominantly recruited by PD-1, while SHP1 serves as a reserve to compensate for loss of SHP2 or in the event that SHP2 becomes limited, a likely scenario in chronic/dormant T cells with typically high expression of PD-1.63 Intriguingly, PD-1 still potently inhibited proliferation and cytokine production of primary T cells with Shp1/2 double knockout,67 suggesting an unknown mechanism underlying PD-1 inhibitory function.
It has been shown that PD-1 inhibits both antigen and co-stimulatory signaling.58,60,61,63,66,68 In activated T cells, PD-1 translocates to the immunological synapse and therefore is in close proximity to both TCR and CD28. A biochemical study showed that SHP2 had significant preference for CD28 over TCR.61 Indeed, the downstream PI3K-AKT pathway of CD28 was inhibited by PD-1 in an ITSM-dependent and ITIM-independent manner.58 However, PD-1 signaling was also shown to inhibit phosphorylation of TCR and downstream signaling molecules like ZAP70.60,66 A transcriptional analysis of PD-1-modulated gene expression during early T cell activation showed that PD-1 mainly suppressed genes induced by strong TCR signaling.69 It is likely that SHP2 recruited by phosphorylated PD-1 ITSM prefers CD28 over TCR but can still inhibit TCR signaling. In addition to its inhibitory roles in T cell signaling, SHP2 was also reported to activate TCR signaling by reversing CSK-mediated inhibitory phosphorylation of LCK. Evidence suggest that sequestration of SHP2 by phosphorylated PD-1 prevent SHP2 from stimulating LCK activity, thus contributing to suppression of T cell signaling.70
CTLA-4 signaling
Compared to CD28, CTLA-4 binds to CD80/86 with higher affinity,71 thus inhibiting co-stimulation by ligand competition. In addition, CTLA-4-expressing T cells can reduce CD80/86 expression on APCs by trans-endocytosis, resulting in decreased CD28 signaling.72 For example, regulatory T (Treg) cells with constitutive CTLA-4 expression can mediate CD80/86 downregulation on dendritic cells (DCs) through this trans-endocytosis process, which is required for the suppressive function of Treg cells.73 As mentioned above, a cis-CD80/PD-L1 heterodimer on APCs protects CD80 from CTLA-4-mediated trans-endocytosis.56 Although the cis interaction between PD-L1 and CD80 disrupts inhibitory function of both PD-1 and CTLA-4, tumor cells often have low CD80 expression such that this protective mechanism might not be effective.
Upon T cell activation, CTLA-4 translocates to the cell surface and clusters into the immune synapse.74,75 The tyrosine in the YVKM motif of CTLA-4 can be phosphorylated by Src family kinases or other kinases, such as Jak2 and Rlk76,77,78 (Fig. 2b). Tyrosine phosphorylation prevents the interaction between CTLA-4 with AP-2, therefore maintaining CTLA-4 on the cell surface to deliver inhibitory signaling.41 On the other hand, the YVKM motif might also recruit SHP2 to repress T cell activation.79 In addition, although the direct recruitment of PP2A by CTLA-4 is still under debate,75,80 the inhibition of AKT activity by CTLA-4 is PP2A-dependent.58 In Treg cells, PKCη was recruited to the immune synapse by CTLA-4. CTLA-4/PKCη further recruited GIT2-αPIX-PAK complex, which facilitated Treg-APC interaction and was required for contact-dependent suppression by Treg cells.81 In addition to cytoplasmic tail-mediated inhibition of the T cell response, CTLA-4 is also thought to inhibit T cell signaling in extrinsic manners. For example, CTLA-4 reduces CD80/86 expression on APCs by either trans-endocytosis as mentioned above or by inducing tumor growth factor β (TGFβ) that in turn downregulates CD80/86.82 CTLA-4 also induces indoleamine 2,3-dioxygenase (IDO) expression in DCs via ligation of CD80/86, resulting in tryptophan depletion and T cell suppression.83
TIM3 signaling
Four ligands have been reported for TIM3, namely C-type lectin galectin9 (Galectin9), carcinoembryonic antigen cell adhesion molecule 1 (Ceacam1), high-mobility group box 1 (HMGB1), and a non-protein ligand phosphatidylserine (PS) (Fig. 2c). Galectin9 is a soluble protein with two carbohydrate recognition domains. The binding of Galectin9 to TIM3 required glycosylated IgV domain of TIM3.84 Ceacam1 binds to TIM3 both in cis and trans. The co-expression and cis interaction with Ceacam1 were essential for TIM3 glycosylation and surface expression, while trans interaction mediated inhibition of effector T cell function.85 The other two ligands mainly regulate innate immune response. HMGB1 is a non-histone chromatin-associated protein that can be secreted to the TME. HMGB1 bound to TIM3 on tumor-associated DCs to suppress the recruitment of released nucleic acid from dying tumor cells to the endosome of DC, thus inhibiting nucleic acid-induced innate immune response.86 Furthermore, TIM3 acts on efferocytosis-recognized apoptotic cells via direct PS binding to regulate efferocytosis in DCs. TIM3 antibody inhibited engulfment of apoptotic cells by CD8+ DC, thereby reducing antigen cross-presentation.87,88
TIM3 signaling remains controversial, as different groups have reported opposite effects of TIM3 in T cell effector function. In an murine acute lymphocytic choriomeningitis virus (LCMV) infection model, TIM3 expression promoted short-lived effector T cell development, accompanied with enhanced AKT/mTOR signaling.89 Another work showed that TIM3 interacted with multiple proximal TCR signaling molecules in the immune synapse, with TIM3 blockade enhancing stable synapse formation between TIM3high CD8 T cells and target cells.90 TIM3 contains five conserved tyrosine residues in its cytoplasmic domain, among which Y265 (Y256 in mouse) and Y272 (Y263 in mouse) can be phosphorylated by Src family kinases91 or interleukin-2-inducible T cell kinase (ITK).92 Upon phosphorylation, these tyrosine residues can recruit p85 to promote NFAT activation.91 Bat3 acts as an inhibitor of TIM3-induced cell death and exhaustion in Th1 cells. Upon binding to unphosphorylated TIM3 cytoplasmic domain, Bat3 specifically recruits the catalytically active form of Lck to promote TCR signaling. TIM3 binding with antibody or ligand causes dissociation of Bat3, likely through the phosphorylation of Y265 and Y272, and reverses the inhibitory effects of Bat3 on TIM3 function.85,93 It is therefore possible that while TIM3 itself might act as an inhibitory receptor, its association with Bat3 converts it to stimulatory in some contexts.
LAG3 signaling
LAG3 is identified as a ligand of MHC-II with higher affinity than CD494,95 and thus might inhibit CD4+ T cell activation by preventing CD4-MHC-II interaction. However, other studies showed that the inhibitory function of LAG3 is independent of CD4 competition but rather dependent on its cytoplasmic domain to deliver inhibitory signaling.96,97 Nevertheless, the inhibitory function of LAG3 in CD8+ T cells does not involve MHC-II, suggesting that other ligands might exist for LAG3. Indeed, LSECtin and Gelectin-3 bind to LAG3 and suppress T cell function in the TME98,99 (Fig. 2d). LAG3 is a glycoprotein with four potential N-linked glycosylation sites in the extracellular domain.94,100 Considering both LSECtin and Gelectin-3 are carbohydrate-binding proteins, their LAG3 binding may be dependent on the glycosylation of LAG3. Recently, fibrinogen-like protein 1 (FGL1) was identified as a new ligand for LAG3. Normally, FGL1 is released into blood at low levels from the liver. However, upregulated FGL1 is detected in several human cancers. Blocking the interaction between FGL1 and LAG3 can enhance the antitumor function of T cells.101 It is interesting to point out that LAG3 is also expressed in Tregs to inhibit proliferation and function.102 Meanwhile, ligation of MHC-II on APCs by Treg-expressed LAG3 also suppresses APCs function.103,104 Therefore, the roles of LAG3 are complex and using LAG3 blockade for cancer immunotherapy needs to be carefully studied to provide clinical benefits.
Knowledge on the signal transduction of LAG3 is still limited. Crosslinking of CD3 and LAG3 inhibited T cell proliferation and cytokine production, which may be caused by impairing proximal TCR signaling as a reduction of calcium influx was also observed.105 The cytoplasmic domain of LAG3 contains three conserved regions in both human and mouse, a serine phosphorylation site, KIEELE motif, and multiple EP repeats. The KIEELE sequence is essential for the inhibitory function of LAG3 in CD4+ T cells.96 LAG3 function can be antagonized by TCR signaling through two transmembrane metalloproteases (A Disintegrin And Metalloproteinase domain-containing protein 10 and 17 (ADAM10 and ADAM17)) that can cleave LAG3. TCR signaling upregulates the cleavage activity of ADAM10 and ADAM17 by distinct mechanisms, which in turns allows efficient T cell proliferation and function.106
TIGIT signaling
CD155 (PVR) and CD112 (PVRL2) are two ligands for TIGIT, with CD155 having a higher affinity than CD122.107 Trans ligation of TIGIT not only delivers inhibitory signals in T and natural killer (NK) cells via TIGIT signaling,108,109 but also suppresses T cell function by enhancing IL-10 production of DCs via reverse CD155 signaling.107 CD226, a co-stimulatory receptor, shares the same ligands with TIGIT.110 However, the affinity of TIGIT to its ligands is higher than CD226, and therefore TIGIT can suppress CD226-mediated co-stimulation via ligand competition.111 Interestingly, TIGIT can also directly bind to CD226 in cis to disrupt its homodimer formation and co-stimulatory function.112
The signal transduction of TIGIT is mainly studied in NK cells. TIGIT cytoplasmic domain contains an ITIM motif and an immunoglobulin tail tyrosine (ITT)-like motif (Fig. 2e). Different studies show that tyrosine phosphorylation in either ITIM motif or ITT-like motif is essential for inhibitory function of TIGIT in human NK cells.108,113,114 However, in murine NK cells these two motifs seem to be redundant.115 The ITT-like domain is reported to recruit SHIP1 through two adaptor proteins Grb2 and β-arrestin2. The Grb2-recruited SHIP1 predominantly inhibits PI3K and MAPK signaling,113 while β-arrestin2-recruited SHIP1 mainly impairs TRAF6 to abolish NF-κB activation.114 However, downstream signals of ITIM motif in TIGIT are still unclear.
BTLA signaling
BTLA and CD160 share the same ligand, herpesvirus entry mediator (HVEM), to suppress T cell function.116,117,118 However, HVEM itself delivers co-stimulatory signal when engaged with TNF superfamily member LIGHT or BTLA/CD160.119,120,121 BTLA/CD160 and LIGHT bind to different sites of HVEM with BTLA/CD160 interacting with the cysteine-rich domain 1 (CRD1) region. CRD1 truncation of HVEM however does not affect LIGHT binding.117,122 Interestingly, soluble LIGHT enhances BTLA/HVEM interaction, while membrane-associated LIGHT purportedly displaces BTLA due to its higher affinity for HVEM.123 Cis interaction occurs when BTLA and HVEM are co-expressed, which prevents HVEM from being activated by trans ligation.124
BTLA contains ITIM and ITSM motifs as well as a Grb2 recognition motif in its cytoplasmic domain.116 Both tyrosine residues in ITIM and ITSM can be phosphorylated and recruit SHP1/SHP2 to inhibit T cell function after ligation116,117,125 (Fig. 2f). Further comparison between BTLA and PD-1 signaling showed that in opposition to PD-1 which recruits the weaker phosphatase SHP2, BTLA prefers to recruit the more potent phosphatase SHP1, to more effectively inhibit both TCR and CD28 signaling.63,126 In addition, BTLA on T follicular helper (Tfh) cells recruits SHP1 to the immune synapse when engaged with HVEM expressed on B cell surface, which inhibits TCR signaling and restrains CD40L to inhibit B cell proliferation.127
Therapeutic strategies targeting immune checkpoint expression
Immune checkpoint blockade therapy using antibodies to block receptor-ligand interactions has gained ground and been approved for clinical use. However, the overall response rate for these blockade antibodies is still low.5,6,10 Given that the inhibitory function of immune checkpoints is critically regulated by their surface expression and signal transduction, targeting these pathways can provide novel strategies for immunotherapy (Table 1).
Many pioneering studies have explored the possibility of targeting checkpoint glycosylation and ubiquitination/degradation pathways. These experiments were performed in different systems and here we list them together to highlight the translational potential of this new approach: (1) Targeting checkpoint glycosylation. Proper glycosylation is required for stable surface expression of checkpoint. Treating T cells with fucosylation inhibitor 2-fluoro-L-fucose (2F-Fuc), reduces the fucosylation and surface level of PD-1. 2F-Fuc-treated cytotoxic T lymphocytes (CTLs) show enhanced antitumor immunity during adoptive cell transfer (ACT) therapy.18 PD-L1 glycosylation is regulated by AMPK and EMT. Metformin, a widely used drug for type 2 diabetes, activates AMPK to induce abnormal glycosylation and degradation of PD-L1. Etoposide, a chemotherapy medication used to treat various cancers, inhibits EMT-induced PD-L1 glycosylation to destabilize surface PD-L1. Downregulation of surface PD-L1 in tumor cells by metformin and etoposide enhances the efficacy of anti-CTLA-4 and anti-TIM therapies.26,27 PD-L1 glycosylation is also regulated by EGFR signaling. Gefitinib, an EGFR inhibitor that is used as a treatment in many cancers, also inhibits PD-L1 glycosylation and in turn promotes GSK3β-mediated ubiquitination and degradation, which results in the enhancement of efficacy of anti-PD-1 therapy.34 (2) Targeting checkpoint ubiquitination/degradation. Promoting degradation of checkpoints appears to be an interesting direction. IL-2, an FDA-approved drug for metastatic melanoma and renal cancer, upregulates FBXO38-mediated PD-1 ubiquitination/degradation. This likely represents one of the several working mechanisms of IL-2 in treating cancer.22 A rationally-designed peptide PD-LYSO, containing a PD-L1-binding sequence and a lysosomal-sorting signal sequence from HIP1R, can target PD-L1 for lysosomal degradation.32 Curcumin inhibits deubiquitination activity of CSN5 to destabilize PD-L1 and benefits anti-CTLA-4 therapy.35 As mentioned above, PD-L1 palmitoylation can suppress mono-ubiquitination and degradation to stabilize surface expression. 2-bromopalmitate inhibits PD-L1 palmitoylation to reduce PD-L1 surface level and in turn promotes antitumor immunity in the murine MC38 tumor model.36 On the other hand, upregulating PD-L1 surface level has also been shown to be beneficial under certain circumstances. The CDK4/6 inhibitor palbociclib inhibits cyclin D-CDK4-SPOP-FZR1 pathway-mediated PD-L1 ubiquitination and degradation, which increases PD-L1 level and sensitizes CT26-implanted tumor to anti-PD-1 therapy.33 Lastly, CTLA-4 blockade antibodies used for cancer immunotherapy often induce severe immunotherapy-related adverse effects (irAEs).128,129 A recent study showed irAE-prone CTLA-4 blocking antibodies induced lysosomal degradation of CTLA-4, while non-irAE-prone antibodies allowed CTLA-4 recycling in an LBRA-dependent manner. Increasing pH sensitivity of irAE-prone anti-CTLA-4 antibodies can prevent antibody-triggered lysosomal degradation of CTLA-4 and attenuates irAE.130
Perspective
Inhibitory functions of immune checkpoints are tightly regulated by surface expression level, receptor-ligand interactions, and intracellular signal transduction. Current immune checkpoint blockade therapies are designed to target the receptor-ligand interaction. In addition to this successful approach, recent studies have shown that modulating surface expression and intracellular signaling might represent other exciting avenues to reinvigorate antitumor immunity. Despite much exciting progress made in the field, several topics remain to be addressed by future research to pave the way for next-generation immunotherapies: (1) Post-translational modifications (PTMs) of immune checkpoints. Current studies highlight the importance of glycosylation, lipid modification, and ubiquitination in checkpoint function. However, our understanding of checkpoint PTMs is still very limited. Advanced mass spectrometry techniques will be needed to systematically investigate checkpoint modifications. (2) Turn-over processes of immune checkpoints. As membrane proteins, surface expression levels of immune checkpoints are controlled by several cell biology processes, including surface delivery, internalization, recycling and degradation. These processes are poorly understood thus far and identifying the key regulatory proteins involved is therefore warranted. (3) Intracellular signaling mechanisms of immune checkpoints. Most checkpoints require tyrosine phosphorylation to activate inhibitory signaling, but the phosphorylation processes are not well studied. Moreover, effector molecules recruited upon checkpoint phosphorylation are also not well characterized. Indeed, it appears that different checkpoints prefer distinct effector molecules to execute their functions. For example, PD-1 primarily recruits SHP2 while BTLA primarily recruits SHP1. The underlying significance of these distinct specificities is unclear. Whether SHP2 and SHP1 play distinct roles in immune suppression is also not fully understood. More experiments therefore need to be performed in the future to fill in these gaps. (4) Context-dependent biology of immune checkpoints. Recent findings strongly suggest that immune checkpoints are subject to specific regulatory mechanisms and exhibit distinct functions in different immune and cancer cell contexts. The tumor microenvironment is packed with various cell types in addition to cancer cells, including T cells, B cells, macrophages, neutrophils, DCs, myeloid-derived suppressor cells, NK cells and cancer-associated fibroblasts. It will be of great interest to both basic and translational researchers to have a more complete picture of checkpoint biology of these different cell types within the TME. For example, the roles of PD-1 in effector, regulatory and memory T cells are complex and multifactorial. Indeed, PD-1 blockade can cause Treg overaction and lead to immune suppression instead of immune reinvigoration, as reflected by the hyperprogressive disease observed in some melanoma patients receiving PD-1 blockade therapy.131
In summary, immunotherapies based on checkpoint biology represent a bright future for the treatment of cancer. Expanding our understanding of immune checkpoint biology will improve the efficacy of current checkpoint blockade therapies and also inform the generation of novel immunotherapy approaches for translation into the clinic.
References
Thorsson, V. et al. The immune landscape of cancer. Immunity 48, 812–830 (2018).
Binnewies, M. et al. Understanding the tumor immune microenvironment (TIME) for effective therapy. Nat. Med. 24, 541–550 (2018).
McGranahan, N. et al. Allele-specific HLA loss and immune escape in lung cancer evolution. Cell 171, 1259–1271 (2017).
Iwai, Y. et al. Involvement of PD-L1 on tumor cells in the escape from host immune system and tumor immunotherapy by PD-L1 blockade. Proc. Natl. Acad. Sci. USA 99, 12293–12297 (2002).
Borghaei, H. et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N. Engl. J. Med. 373, 1627–1639 (2015).
Ribas, A. & Wolchok, J. D. Cancer immunotherapy using checkpoint blockade. Science 359, 1350–1355 (2018).
Bernard, D. et al. Costimulatory receptors in jawed vertebrates: conserved CD28, odd CTLA4 and multiple BTLAs. Dev. Comp. Immunol. 31, 255–271 (2007).
Le, D. T. et al. PD-1 blockade in tumors with mismatch-repair deficiency. N. Engl. J. Med. 372, 2509–2520 (2015).
Samstein, R. M. et al. Tumor mutational load predicts survival after immunotherapy across multiple cancer types. Nat. Genet. 51, 202–206 (2019).
Topalian, S. L. et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N. Engl. J. Med. 366, 2443–2454 (2012).
Gao, J. et al. Loss of IFN-gamma pathway genes in tumor cells as a mechanism of resistance to anti-CTLA-4 therapy. Cell 167, 397–404 (2016).
Sade-Feldman, M. et al. Resistance to checkpoint blockade therapy through inactivation of antigen presentation. Nat. Commun. 8, 1136 (2017).
Mellman, I. & Nelson, W. J. Coordinated protein sorting, targeting and distribution in polarized cells. Nat. Rev. Mol. Cell Biol. 9, 833–845 (2008).
Xu, C. & Ng, D. T. Glycosylation-directed quality control of protein folding. Nat. Rev. Mol. Cell Biol. 16, 742–752 (2015).
Katzmann, D. J., Odorizzi, G. & Emr, S. D. Receptor downregulation and multivesicular-body sorting. Nat. Rev. Mol. Cell Biol. 3, 893–905 (2002).
Grant, B. D. & Donaldson, J. G. Pathways and mechanisms of endocytic recycling. Nat. Rev. Mol. Cell Biol. 10, 597–608 (2009).
Tan, S. et al. An unexpected N-terminal loop in PD-1 dominates binding by nivolumab. Nat. Commun. 8, 14369 (2017).
Okada, M. et al. Blockage of core fucosylation reduces cell-surface expression of PD-1 and promotes anti-tumor immune responses of T cells. Cell Rep. 20, 1017–1028 (2017).
Li, C. W. et al. Eradication of triple-negative breast cancer cells by targeting glycosylated PD-L1. Cancer Cell 33, 187–201 (2018).
Guillaumond, F. et al. Strengthened glycolysis under hypoxia supports tumor symbiosis and hexosamine biosynthesis in pancreatic adenocarcinoma. Proc. Natl. Acad. Sci. USA 110, 3919–3924 (2013).
Huber, A. L. et al. p58(IPK)-mediated attenuation of the proapoptotic PERK-CHOP pathway allows malignant progression upon low glucose. Mol. Cell 49, 1049–1059 (2013).
Meng, X. et al. FBXO38 mediates PD-1 ubiquitination and regulates anti-tumour immunity of T cells. Nature 564, 130–135 (2018).
Bordon, Y. TOX for tired T cells. Nat. Rev. Immunol. 19, 476 (2019).
Wang, X. et al. TOX promotes the exhaustion of antitumor CD8(+) T cells by preventing PD1 degradation in hepatocellular carcinoma. J. Hepatol. 71, 731–741 (2019).
Florcken, A. et al. Immunomodulatory molecules in renal cell cancer: CD80 and CD86 are expressed on tumor cells. Int J. Clin. Exp. Pathol. 10, 1443–1454 (2017).
Hsu, J. M. et al. STT3-dependent PD-L1 accumulation on cancer stem cells promotes immune evasion. Nat. Commun. 9, 1908 (2018).
Cha, J. H. et al. Metformin promotes antitumor immunity via endoplasmic-reticulum-associated degradation of PD-L1. Mol. Cell 71, 606–620 (2018).
Lee, H. H. et al. Removal of N-Linked glycosylation enhances PD-L1 detection and predicts anti-PD-1/PD-L1 therapeutic efficacy. Cancer Cell 36, 169–178 (2019).
Peixoto, A., Relvas-Santos, M., Azevedo, R., Santos, L. L. & Ferreira, J. A. Protein glycosylation and tumor microenvironment alterations driving cancer hallmarks. Front Oncol. 9, 380 (2019).
Burr, M. L. et al. CMTM6 maintains the expression of PD-L1 and regulates anti-tumour immunity. Nature 549, 101–105 (2017).
Mezzadra, R. et al. Identification of CMTM6 and CMTM4 as PD-L1 protein regulators. Nature 549, 106–110 (2017).
Wang, H. et al. HIP1R targets PD-L1 to lysosomal degradation to alter T cell-mediated cytotoxicity. Nat. Chem. Biol. 15, 42–50 (2019).
Zhang, J. et al. Cyclin D-CDK4 kinase destabilizes PD-L1 via cullin 3-SPOP to control cancer immune surveillance. Nature 553, 91–95 (2018).
Li, C. W. et al. Glycosylation and stabilization of programmed death ligand-1 suppresses T-cell activity. Nat. Commun. 7, 12632 (2016).
Lim, S. O. et al. Deubiquitination and stabilization of PD-L1 by CSN5. Cancer Cell 30, 925–939 (2016).
Yao, H. et al. Inhibiting PD-L1 palmitoylation enhances T-cell immune responses against tumours. Nat. Biomed. Eng. 3, 306–317 (2019).
Linsley, P. S. et al. Intracellular trafficking of CTLA-4 and focal localization towards sites of TCR engagement. Immunity 4, 535–543 (1996).
Valk, E. et al. T cell receptor-interacting molecule acts as a chaperone to modulate surface expression of the CTLA-4 coreceptor. Immunity 25, 807–821 (2006).
Banton, M. C., Inder, K. L., Valk, E., Rudd, C. E. & Schneider, H. Rab8 binding to immune cell-specific adaptor LAX facilitates formation of trans-Golgi network-proximal CTLA-4 vesicles for surface expression. Mol. Cell Biol. 34, 1486–1499 (2014).
Mead, K. I. et al. Exocytosis of CTLA-4 is dependent on phospholipase D and ADP ribosylation factor-1 and stimulated during activation of regulatory T cells. J. Immunol. 174, 4803–4811 (2005).
Shiratori, T. et al. Tyrosine phosphorylation controls internalization of CTLA-4 by regulating its interaction with clathrin-associated adaptor complex AP-2. Immunity 6, 583–589 (1997).
Qureshi, O. S. et al. Constitutive clathrin-mediated endocytosis of CTLA-4 persists during T cell activation. J. Biol. Chem. 287, 9429–9440 (2012).
Schneider, H. et al. Cytolytic T lymphocyte-associated antigen-4 and the TCR zeta/CD3 complex, but not CD28, interact with clathrin adaptor complexes AP-1 and AP-2. J. Immunol. 163, 1868–1879 (1999).
Mkhikian, H. et al. Genetics and the environment converge to dysregulate N-glycosylation in multiple sclerosis. Nat. Commun. 2, 334 (2011).
Anjos, S., Nguyen, A., Ounissi-Benkalha, H., Tessier, M. C. & Polychronakos, C. A common autoimmunity predisposing signal peptide variant of the cytotoxic T-lymphocyte antigen 4 results in inefficient glycosylation of the susceptibility allele. J. Biol. Chem. 277, 46478–46486 (2002).
Lau, K. S. et al. Complex N-glycan number and degree of branching cooperate to regulate cell proliferation and differentiation. Cell 129, 123–134 (2007).
Lo, B. et al. Patients with LRBA deficiency show CTLA4 loss and immune dysregulation responsive to abatacept therapy. Science 349, 436–440 (2015).
Curiel, T. J. et al. Blockade of B7-H1 improves myeloid dendritic cell-mediated antitumor immunity. Nat. Med. 9, 562–567 (2003).
Keir, M. E., Butte, M. J., Freeman, G. J. & Sharpe, A. H. PD-1 and its ligands in tolerance and immunity. Annu. Rev. Immunol. 26, 677–704 (2008).
Lin, H. et al. Host expression of PD-L1 determines efficacy of PD-L1 pathway blockade-mediated tumor regression. J. Clin. Invest. 128, 805–815 (2018).
Chen, G. et al. Exosomal PD-L1 contributes to immunosuppression and is associated with anti-PD-1 response. Nature 560, 382–386 (2018).
Poggio, M. et al. Suppression of exosomal PD-L1 induces systemic anti-tumor immunity and memory. Cell 177, 414–427 (2019).
Zhao, Y. et al. Antigen-presenting cell-intrinsic PD-1 neutralizes PD-L1 in cis to attenuate PD-1 signaling in T cells. Cell Rep. 24, 379–390 (2018).
Butte, M. J., Keir, M. E., Phamduy, T. B., Sharpe, A. H. & Freeman, G. J. Programmed death-1 ligand 1 interacts specifically with the B7-1 costimulatory molecule to inhibit T cell responses. Immunity 27, 111–122 (2007).
Chaudhri, A. et al. PD-L1 binds to B7-1 only In Cis on the same cell surface. Cancer Immunol. Res. 6, 921–929 (2018).
Zhao, Y. et al. PD-L1:CD80 Cis-heterodimer triggers the co-stimulatory receptor CD28 while repressing the inhibitory PD-1 and CTLA-4 pathways. Immunity 51, 1059–1073 (2019).
Sugiura, D. et al. Restriction of PD-1 function by cis-PD-L1/CD80 interactions is required for optimal T cell responses. Science 364, 558–566 (2019).
Parry, R. V. et al. CTLA-4 and PD-1 receptors inhibit T-cell activation by distinct mechanisms. Mol. Cell Biol. 25, 9543–9553 (2005).
Chemnitz, J. M., Parry, R. V., Nichols, K. E., June, C. H. & Riley, J. L. SHP-1 and SHP-2 associate with immunoreceptor tyrosine-based switch motif of programmed death 1 upon primary human T cell stimulation, but only receptor ligation prevents T cell activation. J. Immunol. 173, 945–954 (2004).
Yokosuka, T. et al. Programmed cell death 1 forms negative costimulatory microclusters that directly inhibit T cell receptor signaling by recruiting phosphatase SHP2. J. Exp. Med. 209, 1201–1217 (2012).
Hui, E. et al. T cell costimulatory receptor CD28 is a primary target for PD-1-mediated inhibition. Science 355, 1428–1433 (2017).
Rota, G. et al. Shp-2 is dispensable for establishing T cell exhaustion and for PD-1 signaling in vivo. Cell Rep. 23, 39–49 (2018).
Celis-Gutierrez, J. et al. Quantitative interactomics in primary T cells provides a rationale for concomitant PD-1 and BTLA coinhibitor blockade in cancer immunotherapy. Cell Rep. 27, 3315–3330 (2019).
Peled, M. et al. Affinity purification mass spectrometry analysis of PD-1 uncovers SAP as a new checkpoint inhibitor. Proc. Natl. Acad. Sci. USA 115, E468–E477 (2018).
Marasco, M. et al. Molecular mechanism of SHP2 activation by PD-1 stimulation. Sci. Adv. 6, eaay4458 (2020).
Sheppard, K. A. et al. PD-1 inhibits T-cell receptor induced phosphorylation of the ZAP70/CD3zeta signalosome and downstream signaling to PKCtheta. FEBS Lett. 574, 37–41 (2004).
Xu, X. et al. PD-1 and BTLA regulate T cell signaling differentially and only partially through SHP1 and SHP2. J. Cell Biol. https://doi.org/10.1083/jcb.202002049 (in press).
Wang, B. et al. Combination cancer immunotherapy targeting PD-1 and GITR can rescue CD8(+) T cell dysfunction and maintain memory phenotype. Sci. Immunol. 3, https://doi.org/10.1126/sciimmunol.aat7061 (2018).
Shimizu, K. et al. PD-1 imposes qualitative control of cellular transcriptomes in response to T cell activation. Mol. Cell 77, 937–950 (2020).
Bardhan, K. et al. PD-1 inhibits the TCR signaling cascade by sequestering SHP-2 phosphatase, preventing its translocation to lipid rafts and facilitating Csk-mediated inhibitory phosphorylation of Lck. J. Immunol. 196 (1 Suppl), 128.15 (2016).
vanderMerwe, P. A., Bodian, D. L., Daenke, S., Linsley, P. & Davis, S. J. CD80 (B7-1) binds both CD28 and CTLA-4 with a low affinity and very fast kinetics. J. Exp. Med. 185, 393–403 (1997).
Qureshi, O. S. et al. Trans-endocytosis of CD80 and CD86: a molecular basis for the cell-extrinsic function of CTLA-4. Science 332, 600–603 (2011).
Wing, K. et al. CTLA-4 control over Foxp3(+) regulatory T cell function. Science 322, 271–275 (2008).
Egen, J. G. & Allison, J. P. Cytotoxic T lymphocyte antigen-4 accumulation in the immunological synapse is regulated by TCR signal strength. Immunity 16, 23–35 (2002).
Yokosuka, T. et al. Spatiotemporal basis of CTLA-4 costimulatory molecule-mediated negative regulation of T cell activation. Immunity 33, 326–339 (2010).
Schneider, H., Schwartzberg, P. L. & Rudd, C. E. Resting lymphocyte kinase (Rlk/Txk) phosphorylates the YVKM motif and regulates PI3-kinase binding to T-cell antigen CTLA-4. Biochem. Biophys. Res. Commun. 252, 14–19 (1998).
Chuang, E. et al. Regulation of cytotoxic T lymphocyte-associated molecule-4 by Src kinases. J. Immunol. 162, 1270–1277 (1999).
Chikuma, S., Murakami, M., Tanaka, K. & Uede, T. Janus kinase 2 is associated with a box 1-like motif and phosphorylates a critical tyrosine residue in the cytoplasmic region of cytotoxic T lymphocyte associated molecule-4. J. Cell Biochem. 78, 241–250 (2000).
Marengere, L. E. et al. Regulation of T cell receptor signaling by tyrosine phosphatase SYP association with CTLA-4. Science 272, 1170–1173 (1996).
Chuang, E. et al. The CD28 and CTLA-4 receptors associate with the serine/threonine phosphatase PP2A. Immunity 13, 313–322 (2000).
Kong, K. F. et al. Protein kinase C-eta controls CTLA-4-mediated regulatory T cell function. Nat. Immunol. 15, 465–472 (2014).
Chen, W., Jin, W. & Wahl, S. M. Engagement of cytotoxic T lymphocyte-associated antigen 4 (CTLA-4) induces transforming growth factor beta (TGF-beta) production by murine CD4(+) T cells. J. Exp. Med. 188, 1849–1857 (1998).
Mellor, A. L. et al. Specific subsets of murine dendritic cells acquire potent T cell regulatory functions following CTLA4-mediated induction of indoleamine 2,3 dioxygenase. Int. Immunol. 16, 1391–1401 (2004).
Sabatos, C. A. et al. Interaction of Tim-3 and Tim-3 ligand regulates T helper type 1 responses and induction of peripheral tolerance. Nat. Immunol. 4, 1102–1110 (2003).
Huang, Y. H. et al. CEACAM1 regulates TIM-3-mediated tolerance and exhaustion. Nature 517, 386–390 (2015).
Chiba, S. et al. Tumor-infiltrating DCs suppress nucleic acid-mediated innate immune responses through interactions between the receptor TIM-3 and the alarmin HMGB1. Nat. Immunol. 13, 832–842 (2012).
Nakayama, M. et al. Tim-3 mediates phagocytosis of apoptotic cells and cross-presentation. Blood 113, 3821–3830 (2009).
DeKruyff, R. H. et al. T cell/transmembrane, Ig, and mucin-3 allelic variants differentially recognize phosphatidylserine and mediate phagocytosis of apoptotic cells. J. Immunol. 184, 1918–1930 (2010).
Avery, L., Filderman, J., Szymczak-Workman, A. L. & Kane, L. P. Tim-3 co-stimulation promotes short-lived effector T cells, restricts memory precursors, and is dispensable for T cell exhaustion. Proc. Natl. Acad. Sci. USA 115, 2455–2460 (2018).
Clayton, K. L. et al. T cell Ig and mucin domain-containing protein 3 is recruited to the immune synapse, disrupts stable synapse formation, and associates with receptor phosphatases. J. Immunol. 192, 782–791 (2014).
Lee, J. et al. Phosphotyrosine-dependent coupling of Tim-3 to T-cell receptor signaling pathways. Mol. Cell Biol. 31, 3963–3974 (2011).
van de Weyer, P. S. et al. A highly conserved tyrosine of Tim-3 is phosphorylated upon stimulation by its ligand galectin-9. Biochem. Biophys. Res. Commun. 351, 571–576 (2006).
Rangachari, M. et al. Bat3 promotes T cell responses and autoimmunity by repressing Tim-3-mediated cell death and exhaustion. Nat. Med. 18, 1394–1400 (2012).
Baixeras, E. et al. Characterization of the lymphocyte activation gene 3-encoded protein. A new ligand for human leukocyte antigen class II antigens. J. Exp. Med. 176, 327–337 (1992).
Huard, B., Prigent, P., Tournier, M., Bruniquel, D. & Triebel, F. CD4/major histocompatibility complex class II interaction analyzed with CD4- and lymphocyte activation gene-3 (LAG-3)-Ig fusion proteins. Eur. J. Immunol. 25, 2718–2721 (1995).
Workman, C. J., Dugger, K. J. & Vignali, D. A. Cutting edge: molecular analysis of the negative regulatory function of lymphocyte activation gene-3. J. Immunol. 169, 5392–5395 (2002).
Maruhashi, T. et al. LAG-3 inhibits the activation of CD4(+) T cells that recognize stable pMHCII through its conformation-dependent recognition of pMHCII. Nat. Immunol. 19, 1415–1426 (2018).
Xu, F. et al. LSECtin expressed on melanoma cells promotes tumor progression by inhibiting antitumor T-cell responses. Cancer Res. 74, 3418–3428 (2014).
Kouo, T. et al. Galectin-3 shapes antitumor immune responses by suppressing CD8+ T cells via LAG-3 and inhibiting expansion of plasmacytoid dendritic cells. Cancer Immunol. Res. 3, 412–423 (2015).
Andrews, L. P., Marciscano, A. E., Drake, C. G. & Vignali, D. A. LAG3 (CD223) as a cancer immunotherapy target. Immunol. Rev. 276, 80–96 (2017).
Wang, J. et al. Fibrinogen-like protein 1 is a major immune inhibitory ligand of LAG-3. Cell 176, 334–347 (2019).
Zhang, Q. et al. LAG3 limits regulatory T cell proliferation and function in autoimmune diabetes. Sci. Immunol. 2, https://doi.org/10.1126/sciimmunol.aah4569 (2017).
Liang, B. et al. Regulatory T cells inhibit dendritic cells by lymphocyte activation gene-3 engagement of MHC class II. J. Immunol. 180, 5916–5926 (2008).
Bauche, D. et al. LAG3(+) regulatory T cells restrain interleukin-23-producing CX3CR1(+) Gut-resident macrophages during group 3 innate lymphoid cell-driven colitis. Immunity 49, 342–352 (2018).
Hannier, S., Tournier, M., Bismuth, G. & Triebel, F. CD3/TCR complex-associated lymphocyte activation gene-3 molecules inhibit CD3/TCR signaling. J. Immunol. 161, 4058–4065 (1998).
Li, N. et al. Metalloproteases regulate T-cell proliferation and effector function via LAG-3. EMBO J. 26, 494–504 (2007).
Yu, X. et al. The surface protein TIGIT suppresses T cell activation by promoting the generation of mature immunoregulatory dendritic cells. Nat. Immunol. 10, 48–57 (2009).
Stanietsky, N. et al. The interaction of TIGIT with PVR and PVRL2 inhibits human NK cell cytotoxicity. Proc. Natl. Acad. Sci. USA 106, 17858–17863 (2009).
Joller, N. et al. Cutting edge: TIGIT has T cell-intrinsic inhibitory functions. J. Immunol. 186, 1338–1342 (2011).
Bottino, C. et al. Identification of PVR (CD155) and nectin-2 (CD112) as cell surface ligands for the human DNAM-1 (CD226) activating molecule. J. Exp. Med. 198, 557–567 (2003).
Levin, S. D. et al. Vstm3 is a member of the CD28 family and an important modulator of T-cell function. Eur. J. Immunol. 41, 902–915 (2011).
Johnston, R. J. et al. The immunoreceptor TIGIT regulates antitumor and antiviral CD8(+) T cell effector function. Cancer Cell 26, 923–937 (2014).
Liu, S. et al. Recruitment of Grb2 and SHIP1 by the ITT-like motif of TIGIT suppresses granule polarization and cytotoxicity of NK cells. Cell Death Differ. 20, 456–464 (2013).
Li, M. et al. T-cell immunoglobulin and ITIM domain (TIGIT) receptor/poliovirus receptor (PVR) ligand engagement suppresses interferon-gamma production of natural killer cells via beta-arrestin 2-mediated negative signaling. J. Biol. Chem. 289, 17647–17657 (2014).
Stanietsky, N. et al. Mouse TIGIT inhibits NK-cell cytotoxicity upon interaction with PVR. Eur. J. Immunol. 43, 2138–2150 (2013).
Watanabe, N. et al. BTLA is a lymphocyte inhibitory receptor with similarities to CTLA-4 and PD-1. Nat. Immunol. 4, 670–679 (2003).
Sedy, J. R. et al. B and T lymphocyte attenuator regulates T cell activation through interaction with herpesvirus entry mediator. Nat. Immunol. 6, 90–98 (2005).
Cai, G. et al. CD160 inhibits activation of human CD4+ T cells through interaction with herpesvirus entry mediator. Nat. Immunol. 9, 176–185 (2008).
Marsters, S. A. et al. Herpesvirus entry mediator, a member of the tumor necrosis factor receptor (TNFR) family, interacts with members of the TNFR-associated factor family and activates the transcription factors NF-kappaB and AP-1. J. Biol. Chem. 272, 14029–14032 (1997).
Tamada, K. et al. Modulation of T-cell-mediated immunity in tumor and graft-versus-host disease models through the LIGHT co-stimulatory pathway. Nat. Med. 6, 283–289 (2000).
Cheung, T. C. et al. Unconventional ligand activation of herpesvirus entry mediator signals cell survival. Proc. Natl. Acad. Sci. USA 106, 6244–6249 (2009).
Compaan, D. M. et al. Attenuating lymphocyte activity — The crystal structure of the BTLA-HVEM complex. J. Biol. Chem. 280, 39553–39561 (2005).
Cheung, T. C. et al. Evolutionarily divergent herpesviruses modulate T cell activation by targeting the herpesvirus entry mediator cosignaling pathway. Proc. Natl. Acad. Sci. USA 102, 13218–13223 (2005).
Cheung, T. C. et al. T cell intrinsic heterodimeric complexes between HVEM and BTLA determine receptivity to the surrounding microenvironment. J. Immunol. 183, 7286–7296 (2009).
Gavrieli, M., Watanabe, N., Loftin, S. K., Murphy, T. L. & Murphy, K. M. Characterization of phosphotyrosine binding motifs in the cytoplasmic domain of B and T lymphocyte attenuator required for association with protein tyrosine phosphatases SHP-1 and SHP-2. Biochem. Biophys. Res. Commun. 312, 1236–1243 (2003).
Xu, X. et al. BTLA and PD-1 employ distinct phosphatases to differentially repress T cell signaling. bioRxiv https://doi.org/10.1101/669812 (2019).
Mintz, M. A. et al. The HVEM-BTLA axis restrains T cell help to germinal center B cells and functions as a cell-extrinsic suppressor in lymphomagenesis. Immunity 51, 310–323 (2019).
Postow, M. A., Sidlow, R. & Hellmann, M. D. Immune-related adverse events associated with immune checkpoint blockade. N. Engl. J. Med. 378, 158–168 (2018).
Bertrand, A., Kostine, M., Barnetche, T., Truchetet, M. E. & Schaeverbeke, T. Immune related adverse events associated with anti-CTLA-4 antibodies: systematic review and meta-analysis. BMC Med. 13, 211 (2015).
Zhang, Y. et al. Hijacking antibody-induced CTLA-4 lysosomal degradation for safer and more effective cancer immunotherapy. Cell Res. 29, 609–627 (2019).
Kamada, T. et al. PD-1(+) regulatory T cells amplified by PD-1 blockade promote hyperprogression of cancer. Proc. Natl. Acad. Sci. USA 116, 9999–10008 (2019).
Acknowledgements
We thank Preston Dennett, Enfu Hui, Weiping Zou, Teri Elkins and Binlu Huang for critical reading and revision of the manuscript. C.X. is funded by CAS grants (Strategic Priority Research Program XDB29000000, Facility based Open Research Program QYZDB-SSW-SMC048), NSFC grants (31530022, 31861133009), STSMC 16JC1404800, the Ten Thousand Talent Program “National Program for Support of Topnotch Young Professionals” of China, and Fountain-Valley Life Sciences Fund of University of Chinese Academy of Sciences Education Foundation.
Author information
Authors and Affiliations
Contributions
X.H. and C.X. wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
He, X., Xu, C. Immune checkpoint signaling and cancer immunotherapy. Cell Res 30, 660–669 (2020). https://doi.org/10.1038/s41422-020-0343-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41422-020-0343-4
This article is cited by
-
The enhanced antitumor activity of bispecific antibody targeting PD-1/PD-L1 signaling
Cell Communication and Signaling (2024)
-
Identifying a survival-associated cell type based on multi-level transcriptome analysis in idiopathic pulmonary fibrosis
Respiratory Research (2024)
-
Therapeutic and immunomodulatory potentials of mesenchymal stromal/stem cells and immune checkpoints related molecules
Biomarker Research (2024)
-
Identification of breast cancer subgroups and immune characterization based on glutamine metabolism-related genes
BMC Medical Genomics (2024)
-
Immune evasion in cell-based immunotherapy: unraveling challenges and novel strategies
Journal of Biomedical Science (2024)