Abstract
Background
Cancer poses a huge disease burden, which could be reduced by adopting healthy lifestyles mainly composed of healthy diet, body weight, physical activity, limited alcohol consumption, and avoidance of smoking. However, no systematic review has summarised the relations of combined lifestyle factors with cancer morbidity and mortality.
Methods
EMBASE and PubMed were searched up to April 2019. Cohort studies investigating the association of combined lifestyle factors with risks of incident cancer and cancer mortality were selected. Summary hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated using random-effects models. Heterogeneity and publication bias tests were conducted.
Results
The HRs (95% CIs) comparing individuals with the healthiest versus the least healthy lifestyles were 0.71 (0.66–0.76; 16 studies with 1.9 million participants) for incident cancer and 0.48 (0.42–0.54; 30 studies with 1.8 million participants) for cancer mortality. Adopting the healthiest lifestyles was also associated with 17 to 58% lower risks of bladder, breast, colon, endometrial, oesophageal, kidney, liver, lung, rectal, and gastric cancer. The relations were largely consistent and significant among participants with different characteristics in the subgroup analyses.
Conclusions
Adopting healthy lifestyles is associated with substantial risk reduction in cancer morbidity and mortality, and thus should be given priority for cancer prevention.
Similar content being viewed by others
Background
Cancer is the second leading cause of death worldwide and clearly a major growing public health issue. It was estimated that there were 18.1 million incident cancer cases and 9.6 million deaths from cancer in 2018,1 which contributed to 234 million all-age disability-adjusted life-years in 2017 globally.2 Besides, cancer costed 124.6 billion US dollars in the US and 83.2 billion Euros in the European Union annually.3,4 Therefore, prevention of cancer and premature deaths caused by cancer is a matter of vital importance.
Cancer is largely preventable,5 and adopting a healthy lifestyle (including but not limited to avoiding smoking, maintaining a healthy weight, being physically active, avoiding harmful alcohol consumption, and keeping a healthy diet) is a ‘best buy’ strategy for prevention and management of cancer, as well as for other major non-communicable diseases.6,7 However, to the best of our knowledge, there is a lack of randomised controlled trials testing the effects of comprehensive lifestyle interventions on prevention and prognosis of cancer. Thus, evidence from long-term cohort studies is urgently needed for clinical guidelines and public health policy-making. Previous studies have systematically reviewed the associations of individual lifestyle factors with cancer incidence8,9,10,11,12 and cancer mortality,13,14,15,16,17 and a previous systematic review summarised evidence from 12 studies about the association between the adherence to established cancer prevention guidelines for diet and physical activity and cancer outcomes;18 however, no systematic review and meta-analysis is currently available to investigate the combined lifestyle factors with risks of incident cancer and cancer mortality, and whether the association was consistent across participants with different characteristics remained unclear. Hence, we conducted this systematic review and meta-analysis to fill in the gap. In addition, we investigated whether the associations varied across different regions and characteristics of participants.
Methods
Search strategy
The study was conducted according to the Meta-analysis Of Observational Studies in Epidemiology guideline.19 PubMed and EMBASE were searched for studies investigating the relations of combined lifestyle factors with incident cancer and cancer mortality from database inception to April 26, 2019 by Y.-B.Z. and J.C. independently. Since the study was a part of a larger systematic review of the association of combined lifestyle with risk of mortality and major non-communicable diseases (including incident cancer, cardiovascular disease, and diabetes), the search terms included the following Medical Subject Heading terms and related exploded versions as well as keywords: “combined”, “lifestyle”, “mortality”, “cancer”, “cardiovascular disease”, “diabetes”, and “cohort study”. The detailed search strategy was published previously.20 No date and language restrictions were made. To identify additional publications, reference lists of relevant reviews and original studies were further searched.
Inclusion criteria
Y.-B.Z. filtered all the citations, and another group of investigators including J.C., A.C., Y.-G.Z., L.X., J.W., and H.L. also independently performed the study selection. Discrepancies were resolved by discussion, or by conferring with the senior investigator (A.P.). There were only 62 divergences (0.08%) among 82,214 citations, mostly due to the different comprehension of the included lifestyle factors or data format issues.
Included studies should fulfil the following criteria: (1) prospective cohort studies; (2) incident total and site-specific cancer, or cancer mortality as an outcome; (3) using the combination of lifestyle factors as an exposure variable. The lifestyle factors mainly included tobacco smoking, alcohol consumption, physical activity/sedentary behaviour, overweight/obesity, diet, and sleep duration, while some studies also included hot tea consumption, un-piped water consumption, exposure to indoor air pollution, and breastfeeding. Several studies used Life’s Simple 7 (LS7) defined by the American Heart Association as the exposure which additionally included metabolic factors, i.e., blood pressure, blood glucose, and blood lipid levels.21,22 These studies were also included in our main analyses, because the LS7 score could reflect one’s overall lifestyle status. Accordingly, there are three major scores, defined as basic lifestyle score (which gave an equal weight to each behavioural factor, for example, most studies23 assigned one or zero to individuals with or without a certain healthy behaviour), the World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) score24,25 (which included body weight, physical activity, consumption of plant foods, consumption of fast foods and other processed foods high in fat, starches or sugars, consumption of animal foods, consumption of sugar-sweetened drinks, alcohol consumption, and breastfeeding), and the LS7 score21,22 (Supplementary Table 1).
Studies were excluded if they were: (1) other publication types (such as protocols, reviews, cross-sectional studies, case-control studies, and animal experiments) or not peer-reviewed publications (such as meeting abstracts, editorials, and commentaries); (2) focusing on a single lifestyle factor or a combination of only two lifestyle factors (we assumed that lifestyles could not be entirely reflected by two factors); (3) formulation or validation of prediction models; (4) duplicate reporting from the same cohort studies or duplicate publications; (5) studies without necessary or sufficient data. Considering that cancer survivors had substantially different prevalence of risk factors and comorbidity compared with the general population, studies conducted among cancer survivors were not included in the main analysis of combined lifestyle and mortality but were pooled separately. Besides, we did not additionally select studies according to the characteristics of the participants in the main analysis, and cohorts from certain occupational groups or diseased populations were also included. Conference abstracts were not included in our analysis, but for those reporting the relations of combined lifestyle factors with incident cancer or cancer mortality, we searched online and inquired of the authors about whether the full texts had been accepted for publication to avoid missing any potentially eligible studies.
Data extraction and quality assessment
Y.-B.Z. performed data extraction and quality assessment for all studies. Another group of investigators including J.C., A.C., Y.-G.Z., L.X., J.W., and H.L. also independently extracted data and evaluated study quality. Discrepancies were resolved by discussion, or by conferring with the senior investigator (A.P.).
The following data were extracted using standardised extraction form: first author, publication year, title, cohort name, country, study duration and mean/median follow-up duration, sample size, definitions and attainments of outcomes, definitions of included healthy lifestyle factors, and the characteristics of the participants, including sex composition, age (range and mean/median), race/ethnicity, and education level. For articles with unclear information or insufficient data, we contacted the corresponding authors at least two attempts.
We used the Newcastle-Ottawa Scale (NOS) to evaluate the study quality,26 which assessed the selection of the study groups (four items), the comparability of the groups (two items), and the ascertainment of outcome (three items).
Statistical analysis
We used STATA software (Version 14.0, StataCorp, College Station, Texas, USA) to perform all meta-analyses. Hazard ratio (HR) was applied as an effect size for the pooled estimate. Risk ratios (RRs) were used in some studies and were considered as interchangeable with HRs. The odds ratios (ORs) were transformed into RRs using the following formula: RR = OR/[(1 − P0) + (P0 × OR)], where P0 is the incidence of the outcome in the non-exposed group.27 Since different studies constructed varied healthy lifestyle scores (different numbers of factors and different weights for certain factors), we pooled HR comparing the participants in the highest score group with those in the lowest score group, to represent the risk estimate comparing adopting the healthiest with the least healthy lifestyles. Most studies divided participants into three to six groups according to the distributions of the healthy lifestyle scores. Data were synthesised by random-effects models to allow heterogeneity among different studies. The weight of each study was the inverse of the sum of the within-study variance plus variance across studies.28 Forest plots were used to visualise the effect sizes with its 95% confidence intervals (CIs) across studies.
I2 statistic (ranging from 0 to 100%) was used to assess heterogeneity across studies, with a small value indicating less heterogeneity.28 Prespecified stratified analyses were performed according to the study characteristics (such as geographical region, economic level, mean/median follow-up duration, and different combinations of lifestyle factors) and population characteristics (age group, sex, race and ethnicity, and education level). To explore the sources of heterogeneity and possible effect modifications, we also tested between-group p-values by meta-regression.28
The fail-safe N statistic, Begg and Mazumdar rank correlation test, and Egger’s test were used to assess publication bias. If significant publication bias was indicated, we used the Duval and Tweedie’s trim and fill method to generate an “unbiased” estimate by adding the hypothesised studies to make the funnel plot symmetrical.28
Results
Literature search and study characteristics
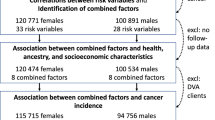
Based on the search strategy, 82,214 unique citations were identified, and 82,108 articles were excluded after screening for the titles and abstracts according to the inclusion/exclusion criteria. Through manual inspections of the full text, 25 studies were further excluded (the list of those publications is shown in the Supplementary Table 2). Finally, 21 studies (five studies were only used for stratified analyses) were included for meta-analyses of incident total cancer, 35 studies were included for meta-analyses of incident site-specific cancer, and 38 studies were included for meta-analyses of cancer mortality (five studies were only used for subgroup analyses and three studies were conducted in cancer survivors). Figure 1 shows the detailed study selection procedure.
The characteristics of the included studies on incident total cancer are shown in the Supplementary Table 3. Among 16 studies used for the main analysis, there were nine, three, and four studies from America, Asia, and Europe. Fourteen studies were from high-income countries. There were three and two studies being only conducted in women and men, respectively, and 11 studies reported results in men and women together (among which, seven studies also conducted subgroup analyses according to sex). The mean age at baseline ranged from less than 42.0–72.0 years old (median = 54.5, interquartile range [IQR] = 11.6). The sample size ranged from 635 to 476 396. The average follow-up duration ranged from 5.5 to over 22.2 years (median = 11.5, IQR = 4.3). The NOS scores of these studies were all equal to or greater than six (Supplementary Table 4), indicating that most studies were of high-quality.
Thirty-five studies investigated the association of combined lifestyle factors with incident site-specific cancer, including colorectal cancer (17 studies), breast cancer (16 studies), lung (8 studies), colon cancer (8 studies), prostate cancer (6 studies), rectal cancer (6 studies), ovarian cancer (6 studies), endometrial cancer (5 studies), and gastric cancer (5 studies). Several studies also investigated other cancers but with limited sample sizes (Supplementary Table 5).
The characteristics of the included studies on cancer mortality are shown in the Supplementary Table 6. Thirty studies were included in the main analysis. There were fourteen, seven, eight, and one studies from America, Asia, Europe, and Oceania, among which 27 studies were from high-income countries or regions. Three studies and two studies were conducted only in women and men, respectively (one study included in the main analysis pooled the Health Professional Follow-Up Study and the Nurses’ Health Study together and did not perform stratified analysis by sex, while another study only included participants from the Nurses’ Health Study and was additionally included in the stratified analysis by sex), and among the other 25 studies, 12 studies reported results in women and men separately. The mean baseline age ranged from 43.1 to 76.5 years old (median = 55.4, IQR = 11.1). The sample size ranged from 1,062 to 476,396. The average follow-up duration ranged from 4.0 to 33.9 years. The NOS scores of these studies were equal to or greater than five (Supplementary Table 4), indicating that most studies were of moderate- to high-quality.
Association of combined lifestyle factors with risk of incident cancers
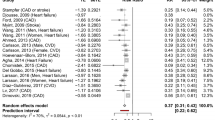
Sixteen studies (1,890,237 participants and over 170,777 cases) reported results comparing participants with the healthiest lifestyles with those with the least healthy lifestyles for incident total cancer, and the pooled HR (95% CI) was 0.71 (0.66–0.76; I2 = 79.2%; Fig. 2).
CI confidence interval; CRPD Clinical Practice Research Datalink; HR hazard ratio; NA not available. The forest plot shows the HRs comparing individuals with the healthiest lifestyles (in the highest score group) with those with the least healthy lifestyles (in the lowest score group) for incident cancer. The number of participants and incident cases were shown in the figure. Each dot represents the HR for each original article, with the location of the circle representing both the direction and magnitude of the effect size, and the HR is bounded by a CI. The rhombs represent the pooled HRs. aOdds ratio was reported in the study and was transformed into relative risk, which was then used in the pooled analysis.
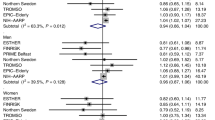
The results were consistent in most stratified analyses (Fig. 3). However, the association was not statistically significant among individuals from non-high-income countries, although the between-group p-value was not statistically significant. Besides, it seemed that the association of combined lifestyle factors with incident cancer was attenuated when the lifestyle score did not include tobacco smoking (HRs [95% CI] comparing individuals with the healthiest lifestyles with those with the least healthy lifestyles were 0.69 [0.62–0.76] and 0.83 [0.80–0.86] when the lifestyle score included or did not include tobacco smoking as a component).
AICR American Institute for Cancer Research; CI confidence interval; HR hazard ratio; NA not available; WCRF World Cancer Research Fund. The forest plot shows HRs comparing individuals with the healthiest lifestyles (in the highest score group) with those with the least healthy lifestyles (in the lowest score group). Each dot represents the HR, with the location of the circle representing both the direction and magnitude of the effect size, and the HR is bounded by a CI. Foraker et al.44 did not report the number of incident cancer cases. aSince a number of studies conducted subgroup analyses or sensitivity analyses, the total number of studies in these stratified analyses exceeded the number of studies included in main analysis.
Begg and Mazumdar rank correlation test and Egger’s regression indicated the results might suffer from potential publication bias (Supplementary Table 7). However, the funnel plots seemed symmetrical (Supplementary Fig. 1), and the classic fail-safe N statistics indicated small possibility of publication bias.
Association of combined lifestyle factors with risk of site-specific cancers
Figure 4 showed the association of combined lifestyle factors with the risk of multiple site-specific cancers. Compared with participants with the least healthy lifestyles, those with the healthiest lifestyles were associated with 17–58% lower risks of cancer in different sites (i.e., cancer of bladder, breast, colon, colorectum, endometrium, oesophagus, kidney, liver, lung, rectum, and stomach). A positive association with skin cancer was reported (HR 1.25; 95% CI 1.08–1.46), but there were only two studies (Supplementary Fig. 2).
CI confidence interval; HR hazard ratio. The forest plot shows the HRs comparing individuals with the healthiest lifestyles (in the highest score group) with those with the least healthy lifestyles (in the lowest score group) for the risks of site-specific cancers. Each dot represents the HR, with the location of the circle representing both the direction and magnitude of the effect size, and the HR is bounded by a CI.
Association of combined lifestyle factors with cancer mortality
Thirty studies (1,822,712 participants and 78,126 deaths) reported results comparing participants with the healthiest lifestyles with those with the least healthy lifestyles for cancer mortality, and the pooled HR (95% CI) was 0.48 (0.42–0.54 I2 = 85.9%; Fig. 5).
CI confidence interval; CVD cardiovascular disease; HR hazard ratio. The forest plot shows the HRs comparing individuals with the healthiest lifestyles (in the highest score group) with those with the least healthy lifestyles (in the lowest score group) for cancer mortality. Each dot represents the HR for each original article, with the location of the circle representing both the direction and magnitude of the effect size, and the HR is bounded by a CI. The rhombs represent the pooled HRs. aEguchi et al.45 reported results in well-educated and poor-educated groups respectively.
The results were consistent in most stratified analyses (Fig. 3). However, the associations were not statistically significant among individuals from non-high-income countries, although the between-group p-value was not statistically significant. When evaluating different scoring systems with cancer mortality, the HRs (95% CIs) were 0.43 (0.37–0.51) for the basic lifestyle score (23 studies), 0.70 (0.59–0.84) for the WCRF/AICR score (four studies), and 0.75 (0.42–1.34) for the LS7 score (two studies). Besides, when considering all scores, the HR (95% CI) was 0.74 (0.69–0.79) when the score did not include tobacco smoking and it was 0.45 (0.37–0.55) when tobacco smoking was included in the score. Furthermore, the association seemed weaker among cancer survivors, and the HR (95% CI) was 0.70 (0.57–0.86; three studies with 6 146 patients; Supplementary Fig. 3).
Egger’s regression indicated the results might suffer from potential publication bias (Supplementary Table 7). However, the funnel plots seemed symmetrical (Supplementary Fig. 4), and the classic fail-safe N statistics along with Begg and Mazumdar rank correlation test indicated small possibility of publication bias.
Discussion
In this systematic review and meta-analysis of prospective cohort studies, the combination of multiple healthy lifestyle factors was associated with a substantial risk reduction in incident cancer and cancer mortality. Adopting the healthiest lifestyle was associated with a 29 and 52% lower risk of incident cancer and cancer mortality compared with having the least healthy lifestyle. The associations remained largely consistent in the stratified analyses by different characteristics of studies and participants. Besides, adopting healthy lifestyles was associated with lower risks of several site-specific cancers, including bladder, breast, colon, colorectal, endometrial, oesophageal, kidney, liver, lung, rectal, and gastric cancer.
Although no meta-analysis has summarised the associations of combined lifestyle factors with cancer morbidity and mortality, the associations with each individual healthy lifestyle factor have been well established. For example, meta-analyses have shown a dose-response association between alcohol consumption and cancer risk: drinking 50 and 100 g of ethanol per day were associated with 22 and 91% higher risks of incident cancer compared with abstainers,8 and heavy drinkers were associated with a 31% higher risk of cancer mortality compared with non-drinkers.14 Body weight was also associated with several site-specific cancers: each five-unit increase in body mass index was associated with 5–50% higher risks of postmenopausal breast, colon and rectal, endometrial, oesophageal, gallbladder, kidney, liver, ovarian, pancreas, stomach cardia, and thyroid cancer, along with meningioma and multiple myeloma.10 In addition, men and women with obesity had 6 and 10% higher risks of cancer mortality compared with their normal-weight counterparts.17 For physical activity and diet, individuals in the highest group had 9%-42 and 10% lower risks of cancer,11,12 and 20 and 22% lower risks of cancer mortality,13,16 respectively, compared with those in the lowest group. Finally, tobacco smoking is the most important risk factor for cancer morbidity and mortality. Compared with never smokers, the risk of incident cancer in current smokers increased by several folds for some cancers, such as lung, laryngeal, pharyngeal, upper digestive tract, and oral cancer,9 furthermore, smokers had substantially increased risks for both smoking-related cancers and other cancers.15 Our stratified analyses showed that the associations were much stronger when smoking was included in the lifestyle scores, indicating the importance of not smoking for cancer prevention. However, 12 studies which did not include smoking in the lifestyle scores all adjusted for smoking status in the multivariate models, and the associations were still statistically significant, which indicated that other lifestyle factors except smoking were also important for cancer prevention. Taken together, encouraging the population to adopt overall healthy lifestyles is necessary for the comprehensive prevention of cancer morbidity and mortality.
On the basis of the current evidence, the World Health Organization,29 the American Cancer Society,30 the WCRF and AICR,7 and some other organisations31 have recommended general population and cancer survivors to adopt healthy lifestyles to prevent cancer and improve prognosis. Since no randomised controlled trials have provided evidence for the effects of multiple lifestyle interventions on cancer prevention and prognosis, our systematic review and meta-analysis of prospective cohort studies provided the highest-quality evidence to support these recommendations. Furthermore, our stratified analyses by different lifestyle scoring systems provided additional evidence for revisions of the current recommendations in the future. We found that the association of the WCRF/AICR score or the LS7 score with cancer mortality was weaker than the association of basic lifestyle score with cancer mortality. This is probably because avoiding smoking was not included in the WCRF/AICR recommendation or scoring system, although the WCRF/AICR acknowledged that avoiding any form of tobacco and other exposure to tobacco was the foremost means of reducing cancer risk. In addition, the weaker association with the LS7 score suggested that more emphases should be given to the upstream lifestyle factors (such as avoiding smoking, maintaining a healthy weight, being physically active, avoiding harmful alcohol consumption, and keeping a healthy diet), in addition to the intermediate metabolic changes, for the prevention of premature deaths from cancer. However, the results should also be interpreted cautiously given that the results for different score systems came from different studies with varied population characteristics, and no study has directly compared the relations of the three scoring methods with cancer mortality in the same population.
Our meta-analysis also found that adopting the healthiest lifestyles was associated with a 30% lower risk of cancer mortality among cancer survivors. However, there were only three studies on this topic. One study was conducted among 837 women with invasive breast cancer,32 one study among 2017 women with cancer,33 and the other study was conducted among 3292 patients with colorectal cancer.34 The mean follow-up durations were all less than 10 years, and thus more studies with longer follow-ups are still needed to investigate the relations of combined lifestyle factors with quality of life, cancer recurrence, and survival among cancer patients. Nonetheless, the limited evidence still indicated that lifestyle changes towards healthy behaviours should be recommended for patients with cancer.
We also evaluated the associations between combined lifestyles and risk of site-specific cancers. The meta-analysis found varying degrees of associations for different cancers, which may in part because of limited studies in certain cancers that precluded us from making a reliable conclusion. More importantly, the results also indicated that different cancers may have different aetiologies and some were more prone to lifestyle factors.29 However, it should be noted that some risk factors were not included in the lifestyle score when considering site-specific cancers, e.g., second-hand smoking and air pollution in scores for lung cancer, endogenous and exogenous oestrogen exposure history in scores for breast cancer. Intriguingly, two studies35,36 found individuals with the healthiest lifestyles were associated with a higher risk of skin cancer compared with those with the least healthy lifestyles. However, these two studies did not consider the sun/ultraviolet exposures on the individual level and behaviours related to the degree of sun exposure, which may confound the results, as shown in the illusive positive relation of physical activity with melanoma.37
The pooled estimates were stronger for the association between lifestyle factors with cancer mortality than that with incident cancer, which was also observed in original studies simultaneously reporting these two outcomes.36,38,39,40 Although the exact reasons are unknown, it is possible that lifestyle factors might have affected more aggressive cancers. In our analyses of different cancer types, we also found that the associations were stronger with more aggressive cancers (such as colorectum cancer, stomach cancer, and liver cancer) than less aggressive cancers (such as prostate cancer, thyroid cancer, lymphoma, and ovary cancer). In addition, participants with healthier lifestyles were more likely to adhere to screening guidelines, get diagnosed earlier, and have access to better treatment, which would be related to better prognosis and reduced risk of mortality.
Our stratified analyses showed that the relations of combined lifestyle factors with cancer morbidity and mortality were largely consistent among individuals from different socioeconomic backgrounds (such as different age groups, sexes, geographic regions, economic levels, races and ethnicities, and education levels). Hence, each country and region should formulate policies tailored to the preference of local population and the reality of local public health practice, in order to accelerate the progressions of achieving Sustainable Development Goal target 3.4.41 Notably, although most studies adjusted some of these socioeconomic factors, residual confounding in the original studies was still possible given that few studies fully adjusted for all of them.
Our study is the first systematic review and meta-analysis to quantitatively summarise the relations of combined lifestyle factors with cancer morbidity and mortality. We followed the standard procedures of the Meta-analysis Of Observational Studies in Epidemiology guideline and included 81 studies in the meta-analysis. We were able to perform various stratified analyses because of a sufficient number of included studies, and the results were largely consistent, indicating the universal importance of adopting healthy lifestyles. We were also able to identify knowledge gaps and future directions via the meta-analysis approach, and the findings of the meta-analysis are also important for establishment of public policy and clinical guidelines. Besides, the results were unlikely to be influenced by publication bias. However, several limitations should also be acknowledged. First, most studies were from high-income countries. More evidence from other countries is needed since lifestyle factors could be greatly varied across countries/regions.42,43 Second, different studies were conducted in populations from different socioeconomic backgrounds, and the combinations or definitions of healthy lifestyle factors varied across studies, which might generate potential heterogeneity. Hence, we only pooled the estimates comparing participants in the highest versus the lowest score group by random-effects model. Third, there is a lack of studies for several site-specific cancers, and evidence for lifestyle modifications in cancer survivors is also limited. Thus, the results should be interpreted cautiously, and more studies are needed.
In conclusion, adopting healthy lifestyles is associated with substantially lower risks of cancer morbidity and mortality. Given that the proportion of individuals having the healthiest lifestyles is low in many countries, creating an environment for better facilitating behaviour modifications should be a public health priority worldwide. More studies are still needed for site-specific cancers, and more evidence among cancer survivors and from populations in low- and middle-income countries is warranted.
References
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A. & Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68, 394–424 (2018).
Kyu, H. H., Abate, D., Abate, K. H., Abay, S. M., Abbafati, C., Abbasi, N. et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392, 1859–1922 (2018).
Jönsson, B., Hofmarcher, T., Lindgren, P. & Wilking, N. The cost and burden of cancer in the European Union 1995–2014. Eur. J. Cancer 66, 162–170 (2016).
Mariotto, A. B., Yabroff, K. R., Shao, Y., Feuer, E. J. & Brown, M. L. Projections of the cost of cancer care in the United States: 2010-2020. J. Natl Cancer Inst. 103, 117–128 (2011).
Colditz, G. A., Wolin, K. Y. & Gehlert, S. Applying what we know to accelerate cancer prevention. Sci. Transl. Med. 4, 127rv124 (2012).
World Health Organization. ‘Best buys’ and other recommended interventions for the prevention and control of noncommunicable diseases. http://www.who.int/iris/handle/10665/259232 (2017).
World Cancer Research Fund/American Institute for Cancer Research. Continuous update project expert report 2018. Recommendations and public health and policy implications. https://www.wcrf.org/sites/default/files/Cancer-Prevention-Recommendations-2018.pdf (2018).
Bagnardi, V., Blangiardo, M., La Vecchia, C. & Corrao, G. Alcohol consumption and the risk of cancer: a meta-analysis. Alcohol Res. Health 25, 263–270 (2001).
Gandini, S., Botteri, E., Iodice, S., Boniol, M., Lowenfels, A. B., Maisonneuve, P. et al. Tobacco smoking and cancer: a meta-analysis. Int J. Cancer 122, 155–164 (2008).
Sung, H., Siegel, R. L., Torre, L. A., Pearson-Stuttard, J., Islami, F., Fedewa, S. A. et al. Global patterns in excess body weight and the associated cancer burden. CA Cancer J. Clin. 69, 88–112 (2019).
Schwingshackl, L. & Hoffmann, G. Diet quality as assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension Score, and health outcomes: a systematic review and meta-analysis of cohort studies. J. Acad. Nutr. Diet. 115, 780–800 (2015).
Moore, S. C., Lee, I. M., Weiderpass, E., Campbell, P. T., Sampson, J. N., Kitahara, C. M. et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Intern. Med. 176, 816–825 (2016).
Bälter, K., Möller, E. & Fondell, E. The effect of dietary guidelines on cancer risk and mortality. Curr. Opin. Oncol. 24, 90–102 (2012).
Jin, M., Cai, S., Guo, J., Zhu, Y., Li, M., Yu, Y. et al. Alcohol drinking and all cancer mortality: a meta-analysis. Ann. Oncol. 24, 807–816 (2013).
Kenfield, S. A., Stampfer, M. J., Rosner, B. A. & Colditz, G. A. Smoking and smoking cessation in relation to mortality in women. JAMA 299, 2037–2047 (2008).
Li, Y., Gu, M., Jing, F., Cai, S., Bao, C., Wang, J. et al. Association between physical activity and all cancer mortality: dose–response meta‐analysis of cohort studies. Int J. Cancer 138, 818–832 (2016).
McGee, D. L. Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Ann. Epidemiol. 15, 87–97 (2005).
Kohler, L. N., Garcia, D. O., Harris, R. B., Oren, E., Roe, D. J. & Jacobs, E. T. Adherence to diet and physical activity cancer prevention guidelines and cancer outcomes: A systematic review. Cancer Epidemiol. Biomark. Prev. 25, 1018–1028 (2016).
Stroup, D. F., Berlin, J. A., Morton, S. C., Olkin, I., Williamson, G. D., Rennie, D. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283, 2008–2012 (2000).
Zhang Y., Pan X. F., Chen J., Xia L., Cao A., Zhang Y. et al. Combined lifestyle factors and risk of incident type 2 diabetes and prognosis among individuals with type 2 diabetes: a systematic review and meta-analysis of prospective cohort studies. Diabetologia 63, 21–33 (2019
Lloyd-Jones, D. M., Hong, Y., Labarthe, D., Mozaffarian, D., Appel, L. J., Van Horn, L. et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 121, 586–613 (2010).
Artero, E. G., España-Romero, V., Lee, D. C., Sui, X., Church, T. S., Lavie, C. J. et al. Ideal cardiovascular health and mortality: Aerobics Center Longitudinal Study. Mayo Clin. Proc. 87, 944–952 (2012).
Bonaccio, M., Di Castelnuovo, A., Costanzo, S., De Curtis, A., Persichillo, M., Cerletti, C. et al. Impact of combined healthy lifestyle factors on survival in an adult general population and in high-risk groups: prospective results from the Moli-sani Study. J. Intern. Med. 286, 207–220 (2019).
Wiseman, M. The second World Cancer Research Fund/American Institute for Cancer Research expert report. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Proc. Nutr. Soc. 67, 253–256 (2008).
Romaguera, D., Vergnaud, A. C., Peeters, P. H., van Gils, C. H., Chan, D. S., Ferrari, P. et al. Is concordance with World Cancer Research Fund/American Institute for Cancer Research guidelines for cancer prevention related to subsequent risk of cancer? Results from the EPIC study. Am. J. Clin. Nutr. 96, 150–163 (2012).
Cook, D. A. & Reed, D. A. Appraising the quality of medical education research methods: the Medical Education Research Study Quality Instrument and the Newcastle-Ottawa Scale-Education. Acad. Med. 90, 1067–1076 (2015).
Higgins, J. P. T. & Green, S. Cochrane Handbook for Systematic Reviews of Interventions. (John Wiley & Sons, Ltd., Chichester, UK, 2006).
Borenstein, M., Hedges, L. V., Higgins, J. P. T. & Rothstein, H. R. Introduction to Meta-Analysis. (John Wiley & Sons, Ltd, Chichester, 2009).
Stewart, B. W. & Wild, C. P. World Cancer Report 2014. (The International Agency for Research on Cancer, Lyon, France, 2014).
Kushi, L. H., Doyle, C., McCullough, M., Rock, C. L., Demark-Wahnefried, W., Bandera, E. V. et al. American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J. Clin. 62, 30–67 (2012).
Lertkhachonsuk, A.-a., Yip, C. H., Khuhaprema, T., Chen, D.-S., Plummer, M., Jee, S. H. et al. Cancer prevention in Asia: resource-stratified guidelines from the Asian Oncology Summit 2013. Lancet Oncol. 14, e497–e507 (2013).
Heitz, A. E., Baumgartner, R. N., Baumgartner, K. B. & Boone, S. D. Healthy lifestyle impact on breast cancer-specific and all-cause mortality. Breast Cancer Res. Treat. 167, 171–181 (2018).
Inoue-Choi, M., Robien, K. & Lazovich, D. Adherence to the WCRF/AICR guidelines for cancer prevention is associated with lower mortality among older female cancer survivors. Cancer Epidemiol. Biomark. Prev. 22, 792–802 (2013).
Romaguera, D., Ward, H., Wark, P. A., Vergnaud, A. C., Peeters, P. H., van Gils, C. H. et al. Pre-diagnostic concordance with the WCRF/AICR guidelines and survival in European colorectal cancer patients: a cohort study. BMC Med. 13, 107 (2015).
Dartois, L., Fagherazzi, G., Boutron-Ruault, M. C., Mesrine, S. & Clavel-Chapelon, F. Association between five lifestyle habits and cancer risk: results from the E3N cohort. Cancer Prev. Res. (Philos.) 7, 516–525 (2014).
Kabat, G. C., Matthews, C. E., Kamensky, V., Hollenbeck, A. R. & Rohan, T. E. Adherence to cancer prevention guidelines and cancer incidence, cancer mortality, and total mortality: a prospective cohort study. Am. J. Clin. Nutr. 101, 558–569 (2015).
Behrens, G., Niedermaier, T., Berneburg, M., Schmid, D. & Leitzmann, M. F. Physical activity, cardiorespiratory fitness and risk of cutaneous malignant melanoma: Systematic review and meta-analysis. PLoS ONE 13, e0206087 (2018).
Cerhan, J. R., Potter, J. D., Gilmore, J. M., Janney, C. A., Kushi, L. H., Lazovich, D. et al. Adherence to the AICR cancer prevention recommendations and subsequent morbidity and mortality in the Iowa Women’s Health Study cohort. Cancer Epidemiol. Biomark. Prev. 13, 1114–1120 (2004).
Greenlee, H., Strizich, G., Lovasi, G. S., Kaplan, R. C., Biggs, M. L., Li, C. I. et al. Concordance with prevention guidelines and subsequent cancer, cardiovascular disease, and mortality: a longitudinal study of older adults. Am. J. Epidemiol. 186, 1168–1179 (2017).
Meng, L., Maskarinec, G., Lee, J. & Kolonel, L. N. Lifestyle factors and chronic diseases: application of a composite risk index. Prev. Med. 29, 296–304 (1999).
Bennett, J. E., Stevens, G. A., Mathers, C. D., Bonita, R., Rehm, J., Kruk, M. E. et al. NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet 392, 1072–1088 (2018).
Gakidou, E., Afshin, A., Abajobir, A. A., Abate, K. H., Abbafati, C., Abbas, K. M. et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1345–1422 (2017).
Hay, S. I., Abajobir, A. A., Abate, K. H., Abbafati, C., Abbas, K. M., Abd-Allah, F. et al. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1260–1344 (2017).
Foraker, R. E., Abdel-Rasoul, M., Kuller, L. H., Jackson, R. D., Van Horn, L., Seguin, R. A. et al. Cardiovascular health and incident cardiovascular disease and cancer: the Women’s Health Initiative. Am. J. Prev. Med. 50, 236–240 (2016).
Eguchi, E., Iso, H., Honjo, K., Yatsuya, H. & Tamakoshi, A. No modifying effect of education level on the association between lifestyle behaviors and cardiovascular mortality: the Japan Collaborative Cohort Study. Sci. Rep. 7, 39820 (2017).
Acknowledgements
We thank James R. Cerhan, MD, PhD (Mayo Clinic), Jian-Min Yuan, MD, PhD (University of Pittsburgh), Vanessa Er, PhD (University of Bristol), Randi Foraker, PhD (Washington University in St. Louis), Theresa A. Hastert, MPH (University of Michigan), Nour Makarem, MS (New York University), and Zhensheng Wang, PhD (University of Pittsburgh) for providing extra information for our analyses.
Author information
Authors and Affiliations
Contributions
Y.-B.Z., X.-F.P., G.L., and A.P. conceptualised the study and developed the research protocol; Y.-B.Z., J.C., A.C., Y.-G.Z., L.X., J.W., and H.L. identified articles for full-text review, extracted data from studies, and matched inclusion criteria. Y.-B.Z. and A.P. did the statistical analyses. Y.-B.Z. drafted the study. All authors critically revised the paper, approved the final study, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The systematic review and meta-analysis used previously published data and did not use any unpublished data. As such, ethical approval to conduct the analysis was not sought.
Consent to publish
Not applicable.
Data availability
Data are available from Dr. An Pan (panan@hust.edu.cn) with a reasonable request.
Competing interests
The authors declare no competing interests.
Funding information
This work was supported by funding from the National Key Research and Development Program of China (2017YFC0907504), the National Nature Science Foundation of China (no. 81773517 and no. 81930124), the Hubei Province Science Fund for Distinguished Young Scholars (2018CFA033), the China Postdoctoral Science Foundation (176596), and the International Postdoctoral Exchange Fellowship of the China Postdoctoral Council (20180062). The funders of the study had no role in the study design, data collection, data analysis, data interpretation, or the writing of the report.
Additional information
Note This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution 4.0 International (CC BY 4.0).
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, YB., Pan, XF., Chen, J. et al. Combined lifestyle factors, incident cancer, and cancer mortality: a systematic review and meta-analysis of prospective cohort studies. Br J Cancer 122, 1085–1093 (2020). https://doi.org/10.1038/s41416-020-0741-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-020-0741-x
This article is cited by
-
Associations of combined lifestyle index with migraine prevalence and headache frequency: a cross-sectional study from the MECH-HK study
The Journal of Headache and Pain (2024)
-
Polygenic risk score model for renal cell carcinoma in the Korean population and relationship with lifestyle-associated factors
BMC Genomics (2024)
-
Does health literacy influence health-related lifestyle behaviors among specialists of health management? A cross-sectional study
BMC Primary Care (2024)
-
Lifestyle changes in middle age and risk of cancer: evidence from the European Prospective Investigation into Cancer and Nutrition
European Journal of Epidemiology (2024)
-
Genetic factors, adherence to healthy lifestyle behaviors, and risk of bladder cancer
BMC Cancer (2023)