Abstract
Background
Lung cancer is the leading cause of cancer mortality in Wales. We conducted a before- and after- study to evaluate the impact of a four-week mass-media campaign on awareness, presentation behaviour and lung cancer outcomes.
Methods
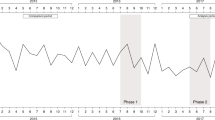
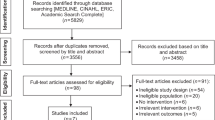
Population-representative samples were surveyed for cough symptom recall/recognition and worry about wasting doctors’ time pre-campaign (June 2016; n = 1001) and post-campaign (September 2016; n = 1013). GP cough symptom visits, urgent suspected cancer (USC) referrals, GP-ordered radiology, new lung cancer diagnoses and stage at diagnosis were compared using routine data during the campaign (July–August 2016) and corresponding control (July–August 2015) periods.
Results
Increased cough symptom recall (p < 0.001), recognition (p < 0.001) and decreased worry (p < 0.001) were observed. GP visits for cough increased by 29% in the target 50+ age-group during the campaign (p < 0.001) and GP-ordered chest X-rays increased by 23% (p < 0.001). There was no statistically significant change in USC referrals (p = 0.82), new (p = 0.70) or early stage (p = 0.27) diagnoses, or in routes to diagnosis.
Conclusions
Symptom awareness, presentation and GP-ordered chest X-rays increased during the campaign but did not translate into increased USC referrals or clinical outcomes changes. Short campaign duration and follow-up, and the small number of new lung cancer cases observed may have hampered detection effects.
Similar content being viewed by others
Background
Lung cancer has the highest mortality of all cancer types, accounting for a fifth of all cancer deaths worldwide.1 Lung cancer survival outcomes in the UK are amongst the worst of comparable high-income countries.2 High incidence and poor long-term survival mean that mortality rates are high,3 particularly in areas of high socioeconomic deprivation. Lung cancer incidence rises steeply with increasing deprivation and the survival inequality gap is widening.4 Delayed symptomatic presentation to a primary care physician and delays within and across primary and secondary care contribute to diagnosis of lung cancer in the later stages of disease.5,6,7 The possibility of curative treatment decreases with later-stage disease diagnosis; in the UK, less than a fifth of patients are eligible for surgical resection, in turn influencing outcomes.6,8
In the absence of routine lung cancer screening, early lung cancer diagnosis relies on prompt patient presentation and GP referral with symptoms indicative of lung cancer. Low public awareness of lung cancer symptoms is one possible barrier to prompt symptomatic presentation, contributing to normalisation and delay in reporting symptoms.9,10,11,12,13 Interventions are therefore required to raise lung cancer symptom awareness and reduce barriers to early presentation to expedite diagnosis.14 However, evidence of the impact of symptom awareness campaigns is limited.15 In 2008, the National Awareness and Early Diagnosis Initiative was formed in England with the aim of improving cancer outcomes through earlier diagnosis.16 Consequently, a national programme of cancer awareness activity was developed, including a focus on lung cancer, and there were also pockets of local activity. Evaluations of these interventions have suggested that these activities might have increased the number of lung cancers diagnosed at an earlier stage.17,18,19 However, to date, there is little evidence regarding the effectiveness of mass-media symptom awareness campaigns18 that have been adapted and implemented in different geographical settings and demographic contexts.
In response to poor lung cancer outcomes in Wales, and with evidence from the English Be Clear on Cancer (BCOC) campaign suggesting stage shift,18 the Welsh BCOC mass-media campaign was launched in 2016. The campaign was designed to increase public awareness of cough as a symptom of cancer and encourage adults over 50 years of age, especially among lower socioeconomic groups, to visit their GP if they had cough symptoms for three weeks or more. Cough is the most common presenting lung cancer symptom, and with reported low public awareness of cough as a cancer symptom, persistent cough was selected as the primary target symptom for the campaign.9,20,21,22,23,24
To evaluate the impact of the Welsh BCOC campaign, we conducted a quasi-experimental study with a before- and after- design, utilising survey responses and routinely collected data. Population based survey data to assess lung cancer symptom awareness and worry about wasting GP time as a perceived barrier to medical help seeking were compared one month before the campaign (pre-campaign period; June 2016) to one month after the campaign (post-campaign period; September 2016). Routine data including symptomatic presentations, primary care referrals, diagnostic testing and cancer diagnoses were compared in the campaign time period (July–August 2016) to the equivalent time period in 2015 (control period).
Methods
The STROBE statement (strengthening the reporting of observational studies in epidemiology) guided reporting (Supplementary File 1).
Intervention
To inform the campaign, six focus groups (four groups of current or former smokers, two groups of never smokers, total n = 48 participants) were undertaken in Wales during August 2015 to gauge audience receptiveness to existing lung cancer campaign materials from England, Scotland and Northern Ireland, who had already run national public awareness campaigns. Following minor adaptations from the English campaign, the Welsh lung cancer awareness campaign was launched in 2016 with the strapline “If you’ve had a cough for three weeks or more, tell your doctor” in both Welsh and English (Supplementary Files 2–5; https://www.cancerresearchuk.org/health-professional/awareness-and-prevention/be-clear-on-cancer/lung-cancer-awareness-campaign-wales).
Campaign messages were disseminated between 11 July and 11 August 2016 on television (S4C and ITV), online, bus and radio adverts, and on posters in pharmacies and on buses. The TV advert was intentionally crafted to appeal to older adults and people from lower socioeconomic (C2DE) groups. Where possible, campaign elements were targeted to reach more deprived groups (i.e. television scheduling, locations for advertising). Primary care engagement in advance of the campaign included circulating health care professional briefing materials with details of the campaign to health boards and primary care networks (https://www.cancerresearchuk.org/health-professional/awareness-and-prevention/be-clear-on-cancer/lung-cancer-awareness-campaign-wales#BCOC_Lung_Wales_Essential0). The first national BCOC respiratory campaign ran in England during the same time period as the Welsh lung BCOC campaign (July–October 2016). This also included three-week cough messaging utilised in previous English lung cancer campaigns, which was promoted via a range of channels including digital television with reach into Wales. This alignment of campaign timing aimed to increase the dissemination of the three-week cough message in Wales. English BCOC lung cancer campaigns that had run prior to 2016 had also utilised media channels that had reached into Wales, providing opportunity for Welsh audiences to have heard the three-week cough message in advance of the dedicated Welsh national activity.
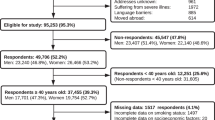
Participants and procedures
Survey data
Pre-campaign (June 2016) and post-campaign (September 2016) population samples were surveyed by Beaufort Research, a market research company. Survey questions were informed by the Cancer Awareness Measure25 and previous campaign evaluation tracking in England, and were included as part of an omnibus survey carried out with a representative sample of the Welsh population (aged 16+) using face-to-face interviews.
Survey questions included gender, age, social group, number of children in the household and area of residence (Cardiff and South East Wales, Mid/West Wales, North Wales, Valleys and West/South Wales). Each respondent was allocated to ‘ABC1’ or ‘C2DE’ based on their responses to a range of profiling questions for social group, with ABC1 reflecting less deprived, and C2DE reflecting more deprived groups. Lung symptom awareness was measured using recall (“There are many warning signs and symptoms of lung cancer. Please name as many as you are aware of”) and prompted recognition questions (“I’m now going to list some symptoms that may or may not be warning signs for lung cancer. For each one, can you tell me the extent to which you think it is a warning sign for lung cancer?”). For the recognition question, the symptoms listed were: a cough for three weeks or more that does not go away, breathlessness, coughing up blood, a persistent pain in your chest or shoulder, losing weight for no obvious reason and a cough that got worse or changes. Response options were: definitely a warning sign, probably a warning sign, probably not a warning sign, definitely not a warning sign and don’t know. Responses were dichotomised as definitely a warning sign/probably a warning sign versus definitely not a warning sign/probably not a warning sign. ‘Don’t know’ responses were not included in the regression analysis. To align with the focus of the campaign, data are reported for recognition/recall of cough symptom.
Worry about wasting the doctor’s time was measured using the question “I’m going to read you a statement that is sometimes made about lung cancer. Can you please tell me how much you agree or disagree with it – that is whether you strongly agree, agree, disagree or strongly disagree. If I had a cough, I would be worried about wasting the GP/doctor’s time”. Response options were dichotomised as strongly agree/agree versus strongly disagree/disagree.
Routine data
Relevant routine data were sourced for pre-campaign (May and June), campaign (July and August) and post-campaign (September and October) periods in 2016, and the same periods in 2015. For the main comparison, the campaign period (July and August 2016) was compared to the comparable time period in the previous year (control period; July and August 2015). Health care and clinical outcomes included:
Primary care presentations
Anonymised counts of visits to GP practices for the cough symptom were identified using defined Read codes extracted from the Securely Anonymised Information Linkage (SAIL) databank. Counts were extracted for any patient registered with a GP practice in Wales using GP data within SAIL for all time points. The number of visits per practice/per week for the target cough symptom and control symptoms including neck pain, knee pain, shoulder pain and urinary tract infections in people aged 50 years and older was calculated for all time points.
Urgent suspected cancer (USC) referrals
USC referrals (patients with suspected lung cancer who are urgently referred from primary care to a specialist, and who are confirmed as urgent by the specialist) were received from the Welsh Government both at all-Wales and local health board (hospital) level. Conversion rates were calculated using the USC referral data received from Welsh Government. To calculate the conversion rate (the proportion of urgent referrals that resulted in a lung cancer diagnosis), the number of lung cancers diagnosed as a result of an urgent suspected cancer referral was divided by the number of USC referrals.
Radiology requests
The number of chest X-rays and chest CT scans carried out in each month (including tests with or without abdomen) was extracted for each health board from their systems. The aggregated data for Wales were used to calculate a count for all time points split by GP-referred and ‘all-referred’ tests. GP-referred tests were adjusted for working days because most GP surgeries are open Monday-Friday, while ‘all-referred’ tests could include referrals from other pathways that can occur on weekends.
Number of new lung cancers diagnosed, stage, source of referral
Lung cancer (ICD10 codes C33-C34) incidence data for non-small cell and small cell were extracted from the Cancer Network Information System Cymru (CaNISC) electronic patient records and split by month and year. Non-small cell lung cancer cases included histological, cytological or clinical diagnoses. The number of lung cancer cases diagnosed for the 2016 time points was compared to the number of cases diagnosed in the corresponding time periods in 2015. Staging data for small cell and non-small cell lung cancers were combined and grouped into early stage (stages I and II) and late stage (III and IV). The proportion of early and late stage cancers for known stages were calculated. The source of referral was extracted for patients diagnosed with lung cancer for the 2016 and 2015 time periods. Numbers and percentages of patients diagnosed with lung cancer following emergency attendance, accident and emergency admission, GP referral and consultant referral were identified from the CaNISC records. Diagnosis following referral after emergency attendance and accident and emergency admission were combined to ‘emergency department referral’.
First treatment received and performance status
The number of lung cancer cases in each treatment category were extracted for the 2016 time periods and the corresponding time periods in 2015. The proportion of all lung cancer cases by treatment group was compared across the 2015 and 2016 time points. Performance status data for all lung cancer cases diagnosed in the corresponding 2015 and 2016 time periods was extracted, according to the following categories: 0 (able to carry out normal activity without restriction), 1 (restricted in physically strenuous activity but ambulatory and able to carry out light work), 2 (ambulatory and capable of all self-care but unable to carry out any work up to about >50% of waking hours), 3 (capable of only limited self-care, confined to bed or chair >50% of waking hours), 4 (completely disabled, cannot carry out any self-care, totally confined to bed or chair) and unknown. Proportions of lung cancer cases by performance status category were compared across the 2015 control time period and 2016 campaign period.
Statistical analysis
Multivariable logistic regression was used to investigate pre- to post- campaign differences in cough recall/recognition and worry about wasting the GP’s time, adjusting for demographic differences between survey samples. Survey data were weighted by age group within gender within Local Authority grouping, to be representative of the Welsh population. Interaction terms were used to test differences between social groups in awareness over time.
For the main comparison of the campaign period (July–August 2016) and the equivalent control period in the previous year (July–August 2015), changes in clinical outcomes were assessed using the two-sample test of proportions or the likelihood ratio tests for counts. The number of days was adjusted due to differences in the number of GP working days in each time period. The significance level was set at p < 0.001 to adjust for multiple testing.
Results
Survey sample characteristics
Sample characteristics are presented in Table 1. The pre-campaign (n = 1011) and post-campaign samples (n = 1013) were primarily female (pre-campaign 56.7%; post-campaign 53.1%), from the most deprived social group C2DE (pre-campaign 54.6%; post-campaign 53.8%), aged 45 years or over (pre-campaign 59.4%; post-campaign 60.7%) and resident in Cardiff/South East Wales (pre-campaign 26.2%; post-campaign 26.5%).
Cough symptom awareness and worry about wasting the doctor’s time
As shown in Table 2, there was a statistically significant 13.3% increase in recall (p < 0.001) and 4.4% increase in recognition (p < 0.001) of the cough symptom pre- to post-campaign. There was a statistically significant 7.5% increase in recall of shortness of breath (p < 0.001) and 11.7% reduction in the number of people who could not recall any symptoms of lung cancer (p < 0.001) pre-to-post campaign. The relationship between social group and recognition of the cough symptom was not significant (p = 0.370 for the interaction term).
There was a statistically significant 6.4% reduction in worry about wasting the GP’s time pre- to post-campaign (p < 0.001). There was a statistically significant 10% decline in worry about wasting GP time for C2DE (the most deprived group) pre- to post-campaign (p = 0.001), but a non-statistically significant 1.6% decline for ABC1 (the more affluent group) (p = 0.33).
GP presentations
The number of GP visits for cough symptoms increased significantly between the control and campaign period in all age groups apart from 10–19-year olds (Table 3). The total number of people of all ages presenting to their GP with a cough during the 2016 campaign period increased significantly by 21.4% (p < 0.001) compared to the corresponding control period in 2015. In the target age group of people aged 50 years and over, there was a statistically significant 24.3% increase (p < 0.001) in the number of visits to a GP for cough during 2016 compared to the equivalent 2015 control period.
Among the target over 50 s age group, the number of presentations with a cough increased from 6.0 per GP practice per week during 2015 to 7.7 per GP practice per week during the campaign period in 2016, equivalent to a statistically significant increase of 28.9% (p < 0.001). In the same time period, there was no significant increase in the number of GP presentations among the over 50 age group for each of the four control symptoms of urinary tract infection (p = 0.77), neck pain (p = 0.26), shoulder pain (p = 0.23) or knee pain (p = 0.37) (Table 3).
Urgent suspected cancer referrals and conversion rate
There was a non-significant 1.2% reduction (p = 0.82) in the total number of USC referrals for suspected lung cancer, and a non-significant 1.4% reduction (p = 0.56) in the number of USC referrals resulting in a lung cancer diagnosis (conversion rate) between the 2016 campaign period and the equivalent time period in 2015 (Table 4).
Radiology requests
A statistically significant increase of 23.4% in GP-referred chest X-rays (p < 0.001), and 8.1% increase in chest X-rays from all referral sources (p < 0.001) was reported in the 2016 campaign period compared to the equivalent time period in 2015 (Table 5).
There was a non-statistically significant 9.6% increase in GP-referred chest CT scans in the 2016 campaign period compared to the equivalent time period in 2015 (p = 0.06). There was a statistically significant 10.1% increase in the number of chest CT scans from all referral sources (p < 0.001) in the 2016 campaign period compared to the equivalent time period in 2015 (Table 5).
Number and stage of new lung cancers diagnosed
There were no statistically significant changes in the number of new diagnoses of non-small cell lung cancer (p = 0.34), small cell lung cancer (p = 0.38) or the total number of new lung cancer diagnoses (p = 0.70) in the 2016 campaign period compared to the equivalent time period in 2015 (Table 6).
There were no statistically significant differences in staging data. There was a non-statistically significant 3.5% increase in the total number of early stage (I and II) cases of lung cancer cases (p = 0.27) and a 3.5% non-significant decrease in the total number of late stage (III and IV) cases of lung cancer (p = 0.27) in the 2016 campaign period compared to the equivalent time period in 2015 (Table 6).
Referral source of number of lung cancers diagnosed
There were no statistically significant changes in the number of new lung cancer diagnoses from all referral sources. There was a non-statistically significant increase in the proportion of new lung cancer diagnoses after referral through emergency department (6.3% increase; p = 0.04), referral through from an inpatient consultant (1.8% increase; p = 0.22) and referral from other sources (2.4% increase; p = 0.02) during the 2016 campaign to the equivalent time period in 2015 (Table 6).
There was a non-statistically significant decrease in the proportion of new lung cancer diagnoses after referral through from a non-accident and emergency department consultant (7.2% decrease; p = 0.02), and referral from the GP (3.3% decrease; p = 0.35) during the 2016 campaign period to the equivalent time period in 2015 (Table 6).
First treatment received and performance status of lung cancers diagnosed
For all forms of treatment including surgical resection, there was no statistically significant difference during the 2016 campaign period to the equivalent time period in 2015 (Supplementary File 6). There were no statistically significant changes in all performance status categories for new lung cancer patients during the 2016 campaign to the equivalent time period in 2015 (Supplementary File 7).
Discussion
We evaluated the impact of the first nationwide mass-media lung cancer symptom awareness campaign to be conducted in Wales. The campaign was successful in raising public awareness of cough as a symptom of lung cancer and in reducing barriers to symptomatic presentation. A greater reduction in worry about wasting GP time was observed after the campaign, especially among socioeconomically deprived groups. Behavioural changes were observed during the campaign, with an increase in the number of patients presenting to their GP with a cough symptom for the target over 50 s target group. Although GP-ordered chest X-rays increased during the campaign, this did not extend to USC referrals or the number and stage distribution of new lung cancer diagnoses.
The first national BCOC lung cancer campaign in England, involving a four-week regional pilot in the central TV region in 2011 and eight-week national mass-media campaign in 2012, reported increased symptom awareness, primary care cough symptom presentations and GP requested chest X-rays.17,18 A subsequent community-based lung cancer awareness campaign run over an extended period of time, combining public awareness activities with open-access walk-in chest X-ray for those with symptoms that could indicate lung cancer and GP education19 also reported improved lung cancer outcomes including a highly significant stage shift and higher treatment rates. We found a significant increase in the number of GP presentations with a cough symptom and GP-ordered chest X-ray requests. However, when comparing the campaign time period in 2015 to the pre- and post-campaign time period data for 2015 (Tables 3 and 5), the reported number of cough symptom presentations and GP-ordered chest X-rays are substantially lower. The lower number of cough presentations and radiology requests in the 2015 campaign period may either be lower by chance (thus artificially inflating our findings), or reflect the time of year when the 2016 campaign was run (July–August) outside of flu season.
We found no impact of the Welsh BCOC campaign on USC referrals or other clinical outcomes. Our findings likely reflect the need for higher-intensity briefings for health-professionals with information about campaign activities and symptoms for referral. Further, it is possible that despite the increase in cough presentations, system and access barriers from primary care to secondary care in Wales may have led to no increase in the proportion of lung cancer cases diagnosed through the GP referral route, reflecting the need for service redesign.
The current campaign was designed to target adults over the age of 50, particularly from C2DE audiences. However, public-facing materials did not display age-related risk information to maintain simple campaign messaging. Campaign developers selected actors for the campaign materials to implicitly reinforce age. It is possible that without explicit advice on age-related risk, younger and lower risk individuals presented to primary care with symptoms, impacting USC referrals. We report the largest reduction in worry about wasting GP time as a psychosocial barrier to help seeking in the target deprived group. Our findings may reflect successful strategic targeting of campaign messages to areas of high socioeconomic deprivation in Wales to modify salient barriers to help seeking.
Low campaign dose and intensity limited the impact of the Welsh BCOC campaign on health care activity and clinical outcomes. Additionally, possible contamination from previous English Be Clear on Cancer lung campaigns into Wales (principally via digital channels) may have potentially diluted the effect of the Welsh Be Clear on Cancer campaign because people in Wales may have previously been exposed to campaign messaging. Due to funding constraints, the dedicated Welsh campaign materials were delivered through fewer outlets and with lower intensity, and the duration of the campaign was half the dose of the first eight-week English BCOC campaign.17,18 Longer campaign duration, together with a more comprehensive and multi-faceted mode of delivery, may lead to larger effects, for example the five-year community-based Leeds lung cancer campaign reported an increase of 80% in chest X-ray referrals.19
The methodological limitations associated with the evaluation of cancer awareness campaigns may also explain these findings.16 Small numbers of new cases during the campaign and comparison periods hampered effect detection for new/early stage lung cancer diagnoses. Due to funding limitations and the time-sensitive nature of the project, it is possible that the follow-up period restricted the capture of changes to clinical outcomes and is a limitation of the evaluation. A long follow-up period is required to account for the time lag between campaign implementation and radiology/suspected cancer referral, and to collect clinical data for patients presenting with symptoms during the campaign who were subsequently diagnosed with lung cancer. Further, data were obtained from two sources, including Omnibus surveys and routinely collected data records. Variation in data collection time points precluded direct comparison of data at each time point. Future campaign evaluations could assess the possible negative effects of the campaign, such as increased health anxiety.
Promisingly, our findings show that a mass-media cough campaign can increase symptom awareness, symptomatic presentation and, potentially, GP-ordered diagnostic testing. We found evidence of reach and reduced barriers to help seeking in socioeconomically deprived groups.
Conclusion
Increased public awareness, cough symptom presentation and GP-ordered diagnostic testing did not translate into increased USC referrals, new lung cancer diagnoses or stage shift following a national mass-media lung cancer awareness campaign in Wales. This reflected limitations of campaign delivery and methodological issues associated with its evaluation. Earlier diagnosis might be achieved by more intensive, sustained and targeted campaigns, by improving GP diagnostic and referral systems, and through secondary care pathway redesign.
References
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R., Torre, L. & Jemal, A. GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68, 394–424 (2018).
Allemani, C., Matsuda, T., Di Carlo, V., Harewood, R., Matz, M., Niksic, M. et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37513025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 391, 1023–1075 (2018).
Cancer Research UK. Lung cancer statistics [website]. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/lung-cancer. (2019).
Welsh Cancer Intelligence and Surveillance Unit. Cancer statistics [website]. http://www.wcisu.wales.nhs.uk/home. (2019).
Barrett, J. & Hamilton, W. Pathways to the diagnosis of lung cancer in the UK: a cohort study. BMC Fam. Pract. 9, 31 (2008).
Walters, S., Maringe, C., Coleman, M. P., Peake, M. D., Butler, J., Young, N. et al. Lung cancer survival and stage at diagnosis in Australia, Canada, Denmark, Norway, Sweden and the UK: a population-based study, 2004–2007. Thorax 68, 551–564 (2013).
Tørring, M. L., Frydenberg, M., Hansen, R. P., Olesen, F. & Vedsted, P. Evidence of increasing mortality with longer diagnostic intervals for five common cancers: A cohort study in primary care. Eur. J. Cancer 49, 2187–2198 (2013).
National Cancer Registration and Analysis Service. Chemotherapy, Radiotherapy and Tumour Resections in England [website]. https://www.cancerdata.nhs.uk/treatments. (2019).
Simon, A. E., Juszczyk, D., Smyth, N., Power, E., Hiom, S., Peake, M. D. et al. Knowledge of lung cancer symptoms and risk factors in the UK: development of a measure and results from a population-based survey. Thorax 67, 426–432 (2012).
Quaife, S. L., Forbes, L. J. L., Ramirez, A. J., Brain, K. E., Donnelly, C., Simon, A. E. et al. Recognition of cancer warning signs and anticipated delay in help-seeking in a population sample of adults in the UK. Br. J. Cancer 110, 12–18 (2014).
Crane, M., Scott, N., O’Hara, B. J., Aranda, S., Lafontaine, M., Stacey, I. et al. Knowledge of the signs and symptoms and risk factors of lung cancer in Australia: mixed methods study. BMC Public Health 16, 508 (2016).
McLachlan, S., Mansell, G., Sanders, T., Yardley, S., van der Windt, D., Brindle, L. et al. Symptom perceptions and help-seeking behaviour prior to lung and colorectal cancer diagnoses: a qualitative study. Fam. Pract. 32, 568–577 (2015).
McCutchan, G., Hiscock, J., Hood, K., Murchie, P., Neal, R., Newton, G. et al. Engaging high-risk groups in early lung cancer diagnosis: a qualitative study of symptom presentation and intervention preferences among the UK’s most deprived communities. BMJ Open 9, e025902 (2019).
Weller, M., Peake, M., Field, J. Presentation of lung cancer in primary care. Primary Care Resp Med. https://doi.org/10.1038/s41533-019-0133-y (2019).
Austoker, J., Bankhead, C., Forbes, L. J. L., Atkins, L., Martin, F., Robb, K. et al. Interventions to promote cancer awareness and early presentation: systematic review. Br. J. Cancer 101(Suppl 2), S31–S39 (2009).
Richards, M. A. The National Awareness and Early Diagnosis Initiative in England: assembling the evidence. Br. J. Cancer 101(S 2), S1–S4 (2009).
Public Health England: National Cancer Registration and Analysis Service [online PDF]. Be Clear on Cancer: Regional and national lung cancer awareness campaigns 2011 to 2014. Final evaluation results. http://www.ncin.org.uk/cancer_type_and_topic_specific_work/topic_specific_work/be_clear_on_cancer/ (2018).
Ironmonger, L., Ohuma, E., Ormiston-Smith, N., Gildea, C., Thomson, C. S. & Peake, M. D. An evaluation of the impact of large-scale interventions to raise public awareness of a lung cancer symptom. Br. J. Cancer 112, 207 (2014).
Kennedy, M. P. T., Cheyne, L., Darby, M., Plant, P., Milton, R., Robson, J. M. et al. Lung cancer stage-shift following a symptom awareness campaign. Thorax 0, 1–9 (2018).
Hamilton, W., Peters, T., Round, A. & Sharp, D. What are the clinical features of lung cancer before the diagnosis is made? A population based case-control study. Thorax 60, 1059–1065 (2005).
Hamilton, W. The CAPER studies: five case-control studies aimed at identifying and quantifying the risk of cancer in symptomatic primary care patients. Br. J. Cancer 101, S80 (2009).
Lövgren, M., Leveälahti, H., Tishelman, C., Runesdotter, S., Hamberg, K. & Koyi, H. Time spans from first symptom to treatment in patients with lung cancer – The influence of symptoms and demographic characteristics. Acta Oncologica 47, 397–405 (2008).
Kvale, P. A. Chronic Cough Due to Lung Tumors: ACCP Evidence-Based Clinical Practice Guidelines. Chest 129, 147S–153S (2006).
Shim, J., Brindle, L., Simon, M. & George, S. A systematic review of symptomatic diagnosis of lung cancer. Fam. Pract. 31, 137–148 (2014).
Stubbings, S., Robb, K., Waller, J., Ramirez, A., Austoker, J., Macleod, U. et al. Development of a measurement tool to assess public awareness of cancer. Br. J. Cancer 101, S13–S17 (2009).
Acknowledgements
We would like to thank the members of the Welsh Lung Cancer Initiative Virtual Reference group (Jane Hanson, John Watkins, Gareth Collier, Clare Bath, Karen Gully, Carol Owen and Richard Neal) for their input into the development and implementation of the campaign. Thanks to Sian Howell who coordinated campaign delivery and Sara Roberts who supported campaign implementation. We would also like to thank Beaufort Research and the Welsh Cancer and Intelligence Unit, who collected the data, and Katie Connor of Cancer Research UK who supported analysis of the survey data.
Author contributions
A.B. contributed to the development of the campaign. K.B., J.M., L.I., G.M. and S.S. contributed to the development of the campaign and campaign evaluation from an advisory capacity. D.H., R.T., L.I. and C.S. analysed the data. G.M. and S.S. prepared the manuscript. All authors were involved in the development of the manuscript. All authors read and approved the final version.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The survey was conducted as part of an omnibus survey conducted by Beaufort’s Research; therefore, ethical approval was not obtained for the omnibus. Beaufort Research operate to standard codes of conduct.
Consent to publish
Not applicable
Data availability
Requests for data-sharing will be considered by the senior authors. Please submit requests to the corresponding author.
Competing interests
The authors declare no competing interests.
Funding information
The pre-campaign testing and elements of the evaluation were funded by the Early Diagnosis team at Cancer Research UK. Public Health England funded the development of the assets used in the campaign. NHS Wales funded the Welsh campaign and evaluation. Dr Grace McCutchan is supported by Health and Care Research Wales as part of the Wales Cancer Research Centre (Grant reference no: CA05). Dr Stephanie Smits is supported by a Health and Care Research Wales Fellowship.
Additional information
Note This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution 4.0 International (CC BY 4.0).
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
McCutchan, G., Smits, S., Ironmonger, L. et al. Evaluation of a national lung cancer symptom awareness campaign in Wales. Br J Cancer 122, 491–497 (2020). https://doi.org/10.1038/s41416-019-0676-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-019-0676-2
This article is cited by
-
Primary healthcare professionals’ perspectives on patient help-seeking for lung cancer warning signs and symptoms: a qualitative study
BMC Primary Care (2022)
-
An evaluation of a national mass media campaign to raise public awareness of possible lung cancer symptoms in England in 2016 and 2017
British Journal of Cancer (2022)
-
COVID-19 and the multidisciplinary care of patients with lung cancer: an evidence-based review and commentary
British Journal of Cancer (2021)
-
Randomised controlled trial and economic evaluation of a targeted cancer awareness intervention for adults living in deprived areas of the UK
British Journal of Cancer (2021)