Abstract
It is important that dental extractions under general anaesthesia (GA) are planned appropriately to avoid a repeat GA in the future. Current guidelines recommend the input of an orthodontist when the treatment plan involves a permanent tooth extraction but the number of children undergoing GA extractions makes this challenging. A model has been developed where the records of children planned for GA extraction of permanent teeth are triaged, via secure email, by an orthodontist. The orthodontist identifies patients where modification of the extraction pattern could be beneficial to longer-term oral health. For some patients this is possible from review of the records alone, but the triage also identifies those patients with more complex occlusal problems who require a face to face orthodontic assessment. This service review found that 22% of the patients triaged had their treatment plan modified by the orthodontist. For 76% of the patients, a review of their records was sufficient before finalising the plan and only 24% needed a further face to face orthodontic assessment. This model has been successful in reducing the burden of an additional orthodontic assessment for most patients while providing personalised care.
Similar content being viewed by others
Key points
-
Demonstrates how orthodontic input in permanent teeth extraction can address occlusal and long-term oral health concerns in children.
-
Suggests an orthodontic email triage service can reduce the time and cost burden on the patient and their parents/carers as well as the dental services.
-
Argues email triage by an orthodontist may be of value to other teams extracting permanent teeth in children under general anaesthetic.
Introduction
It is important that dental extractions under general anaesthetic (GA) are planned appropriately to avoid a repeat GA later. The input of an orthodontist has been recommended,1,2 but the large number of children undergoing GA extractions and the increasing demands on orthodontic services make this challenging.
The number of children requiring dental extractions under GA is of great concern. There have been reports in both the dental press and wider media highlighting the number of children undergoing multiple extractions under GA. Approximately 25,000 operations for dental extractions under GA were carried out in England alone during 2017-18 on 5-9-year-olds.3 Dental caries remains the number one cause for children requiring hospital admission and undergoing general anaesthetic. There were approximately 43,000 hospital admissions in under 18s due to dental caries during 2017-18 in England.4 This can be an emotionally draining and upsetting event for the patient and their parents, but also has a significant impact on NHS resources. Approximately £30 million was spent by the NHS on hospital-based tooth extraction in under 18s in 2012-13.5 This highlights the importance of comprehensive treatment planning for children who require extractions under general anaesthetic, to minimise the need for a repeat GA in the future.
Providing dental treatment which requires local anaesthesia (LA) is often a challenge in children due to the accompanied anxiety and fear. Undergoing a dental extraction can be a very anxious moment for any patient. This is particularly difficult in children, many of whom will not comply to even go as far as having the LA. Even in those compliant children who can tolerate the LA stage, often the subsequent application of pressure during the extraction is too much to bear; many at that stage become non-compliant and it is then difficult for the dentist to complete the extraction. Hence, many children are referred in to the community dental services to have dental treatment such as extractions performed under some form of anxiety control, like conscious sedation or GA.
There are several reasons why a permanent tooth needs to be extracted in a child. In many cases, it is due to gross caries with or without pulpal involvement.6 The restorability and prognosis of these teeth can be further compromised due to conditions such as molar incisor hypoplasia (MIH).7 Many of these children can exhibit sub-satisfactory oral hygiene, along with a cariogenic diet, and often require multiple tooth extractions as a result. Other less common reasons include pre-orthodontic therapy extractions, trauma and presence of supernumerary teeth.
While modern GA is relatively safe, there are certain risks involved. The more common risks are post-GA nausea, dizziness and a mild headache. Although rare, there are, however, more serious risks which can include an allergic reaction to certain drugs used in anaesthesia and, in the most catastrophic situation, fatality can occur.8 Furthermore, since these children are often non-compliant with even a simple examination in the chair, the treatment plan needs to be as comprehensive as possible to avoid a repeat GA. This is vital, primarily from the patient safety perspective, but also from an efficiency point of view. Rather than just focusing on the teeth giving problems to the child at the time, the treatment plan should include any further extractions which may improve long-term oral health. The opinion of an orthodontist can, therefore, be beneficial when treatment planning such cases. The most common permanent tooth requiring treatment in children is the first permanent molar.9 The Royal College of Surgeons of England guidelines on the extraction of this tooth advises that treatment planning for such cases should ideally be made with input from an orthodontist.1 This is particularly emphasised when the extraction is being carried out under general anaesthetic.2
Development of the email triage model
West Dorset is largely a rural community. Many patients travel a moderate distance to access the community dental and orthodontic services. Some rely on public transport which results in a heavy burden on time missed from school by patients, and work by their parents/carers. Reducing the number of appointments could help decrease the time and cost burdens.
Historically, our community dental and orthodontic teams have developed good working relationships as both share the same hospital site. The teams have previously worked together to improve orthodontic services for patients with autism and/or learning disabilities.10 The teams already hold joint clinics for those patients with autism and/or learning disabilities who may not cope with a routine orthodontic assessment. Ideally, all patients undergoing GA would have a similar joint appointment, but this is impractical due to the sheer number of such cases. Initially there was an informal arrangement where orthodontic input was provided by secure email on a case by case, ad hoc basis. With an increase in the number of community dentists assessing and listing children for permanent teeth extraction under GA, the need to formalise arrangements for orthodontic assessment became apparent and an email triage model evolved.
Current model
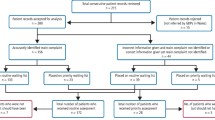
During the initial examination appointment at the community dental services, a clinical and radiographic investigation is completed. The clinician also notes the skeletal and occlusal relationship along with any orthodontic abnormalities (crowding, impactions etc). Consideration is given to balancing and compensating extractions when a first permanent molar is planned, following the Royal College of Surgeons of England Guidelines.1 A provisional treatment plan is formulated which would include extraction of at least one permanent tooth. In the first instance, orthodontic triage of the clinical details and radiographs is requested via a secured NHS email exchange. The patient's information is anonymised as much as possible. The orthodontist then determines whether the treatment plan may need to be modified because of orthodontic concerns and whether a face to face consultation is required for more complex cases. In such cases, a written referral is sent and after the orthodontic consultation the treatment plan is finalised for the treatment under GA (Fig. 1).
Protecting the patient's information and transferring it safely between organisations is of utmost importance. This is further emphasised following the implementation of the General Data Protection Regulations (GDPR) across the European Union in May 2018. Therefore, before requesting any orthodontic input, the patient and their parent/carer are informed, and consent is gained. The information is anonymised as much as practically possible and only exchanged via the secure NHS email.
The aim of this service evaluation was to evaluate the effectiveness of this model; specifically, to determine the percentage of patients where the provisional treatment plan was modified following orthodontic assessment and looking at the percentage of patients needing a face to face consultation with the orthodontist before finalising the treatment plan.
Data collection method
Before commencing the project, formal approval for a service evaluation was gained from both Dorset County Hospital NHS Foundation Trust and Somerset Partnership NHS Foundation Trust. Subjects were identified retrospectively. Children (16 years or younger) for whom orthodontic triage had been requested between September 2016 and March 2018 were included; fifty children meeting the criteria were identified. The electronic dental records of these patients were accessed to gather the information needed for the evaluation. These data were collected using a Microsoft Excel spreadsheet, with any identifiable patient details being anonymised.
Results
The age range of patients reviewed was between six and 14 years (Fig. 2). The median age of the patients was nine-years-old and the mean age was 9.6 years. As expected, the primary reason for children requiring a permanent tooth extraction was due to caries (Fig. 3). This was part of the diagnosis for 90% of the patients.
The severity of the tooth breakdown caused by caries can be exaggerated by the presence of hypoplasia.11 MIH was a factor in 42% of the cases requiring further permanent teeth extractions due to their guarded prognosis. Of the 50 patients analysed, 76% did not require a face to face orthodontic assessment and only 13% of these patients had their provisional treatment plan modified following review of the records by the orthodontist. Of the 24% who had a face to face orthodontic assessment before finalising the extraction treatment plan, 50% had their extraction plan modified (Fig. 4).
Details of the patients who had a change in their treatment plan can be seen in Table 1 and Table 2. Overall, 22% of the total patients had changes made between the provisional and finalised treatment plan, following an orthodontic input.
Case profile one: extraction pattern modified after review of records only
A 13-year-old girl was referred to the community dental department by her general dental practitioner for extraction of her carious hypomineralised first permanent molars. On assessment she was fit and well, but had been diagnosed with autistic spectrum disorder, mild learning disabilities and attention deficit hyperactivity disorder. Her oral hygiene was poor and she had a highly cariogenic diet. She had experienced recurrent pain from her carious first permanent molars.
Clinical examination found gross caries affecting the upper and lower left first permanent molars (26 and 36). The 26 tooth had been dressed. There was less severe caries affecting the upper and lower right first permanent molars (16 and 46). Although the lower second permanent molars were fully erupted, there was no sign intraorally of the upper second permanent molars. The patient had a Class I occlusion, with no crowding or other obvious orthodontic concerns.
Radiographic examination confirmed the presence of all permanent teeth including the third molars. The caries in the 26 and 36 extended into pulp. Although the caries in the 16 and 46 was less extensive, there was both occlusal and interproximal decay. Caries was also noted in the upper right premolar teeth. The upper second molars were impacted and in close relationship with the upper third molars; the 17 appeared to have abnormal root form. The 48 was noted to be mesioangulated with incomplete root formation (Fig. 5).
Diet advice and oral hygiene instruction were given; follow up was arranged with the referring dentist, with a recommendation of prescription of high fluoride toothpaste and close monitoring. A provisional management plan was formulated which involved extraction of all four first permanent molars and restoration of the carious upper premolars under general anaesthetic. Because of the impaction of the upper second molars, an orthodontic opinion was sought through the secure email triage service.
Upon review of the radiograph the orthodontist confirmed that the impaction of the 17 was a concern, and without intervention neither the 17 or 18 were likely to erupt. The situation in the upper left quadrant was of lesser concern and it was hoped that following the loss of the 26, the 27 would erupt normally. It was recommended that the 18 be extracted during the GA and the eruption of the 17 then monitored.
Since the 18 would require surgical extraction, the community dental team liaised with the local oral and maxillofacial surgery team. A joint GA was planned so that the extractions and restorations could be carried out together. The patient was warned about the possible fusion of the 17 and 18, and that the 17 was not guaranteed to erupt. A follow-up has been arranged with her general dental practitioner.
Case profile two: extraction pattern modified after face to face orthodontic assessment
A 10-year-old boy was referred to the community dental department by his general dental practitioner for extraction of his carious lower first permanent molars (36 and 46). He had experienced some short-lived spontaneous pain from the 46. On assessment, he was fit and well. He had had no learning disabilities or additional needs but was anxious about dental care and unwilling to consider extractions under local anaesthetic.
On examination he was in the permanent dentition; his oral hygiene was poor and there was gross caries present in both the 36 and 46. There was early, restorable, caries present in the lower left first premolar tooth (34). Crowding was noted in the upper arch, with the upper permanent canines (13 and 23) erupting buccally. Radiographic examination confirmed the presence of all permanent teeth, including the third molars. The decay in the 36 and 46 extended into pulp. The decay in the 34 was minimal, but had extended beyond enamel and into dentine (Fig. 6). Because of the presence of upper arch crowding, an orthodontic opinion was sought through the secure email triage service. After triage, the orthodontist recommended a face to face consultation to assess the crowding.
On orthodontic examination the patient presented with a Class I incisor relationship on a Class I skeletal base, with normal vertical facial proportions. There was severe upper arch crowding, with both the 13 and 23 erupting buccally. There was a crossbite associated with the 16, but no displacement on closure. Overjet and overbite were normal. Buccal segment relationships were a half unit Class II.
The extraction of the 36 and 46 was dictated by caries and the orthodontic examination confirmed that restoration of the 34, rather than loss, was the most appropriate plan. It was explained to the patient and his mother that although there may be some spontaneous drift of the lower second permanent molars following the loss of the first molars, there was likely to be some tipping of these teeth and residual lower arch spacing. This could be closed orthodontically in the long-term, should the patient's oral health improve sufficiently.
The options for management of the upper arch crowding were also discussed. These included:
Accept: however, the patient already had aesthetic concerns about the canines
Extract upper canines: this would compromise long-term aesthetics, but was an option if the patient was unwilling to consider future orthodontic care
Extract upper first premolars: as the upper canines were not yet fully erupted, it was hoped that there may be some drift of the canines and improvement in aesthetics. However, the patient was warned that, for good alignment, fixed appliances may be considered later, should oral health improve sufficiently.
After discussion, the patient and his mother agreed that the extraction of upper first premolars (14 and 24) was the most appropriate plan. The final permanent teeth extractions performed under GA included: 14, 24, 36 and 46. The patient is planned for an orthodontic review in 12 months.
Discussion
The average age of the child undergoing permanent tooth GA extraction was nine-years-old. This is not unexpected since gaining compliance for an extraction in the chair under LA is often difficult in children of this age or younger. This is often due to their level of cognitive maturity and inability to comprehend the importance of having treatment to address their oral health.
Dental caries plus or minus MIH was the main reason for permanent tooth extraction. Relief of crowding and the management of unerupted/impacted permanent teeth were the other reasons necessitating permanent teeth extractions. This is where an orthodontic input is of greatest value as early interceptive orthodontic extractions can be beneficial in the long-term management of the dentition and provides a more comprehensive treatment.
It is good practice to involve the orthodontist in the treatment planning for any paediatric case which may involve a permanent tooth extraction. This is highly recommended by the guidelines currently published by the Royal College of Surgeons of England.1 The benefits of an orthodontic input are clear to see as 22% of the patients had changes in their treatment plans following their advice. Most of these changes were due to factors such as crowding of the dentition and prognosis of the hypoplastic teeth. Early interceptive orthodontics can, therefore, be hugely important for these patients. Not only does it help relieve crowding (which may obviate the need for future orthodontics or simplify future orthodontic treatment), it also gives an opportunity to plan the loss of teeth that are already carious, restored or of poor long-term prognosis to the orthodontic treatment.
The initiative to triage patients via a secure email pathway has proved beneficial. It gives an opportunity for the patient to receive a personalised care plan. Although guidelines for balancing and compensating extraction of first permanent molars are considered, review of the records by an orthodontist provides greater reassurance that all factors have been considered. The use of a secured email maximises efficiency. In this service evaluation, 76% of patients avoided a face to face assessment. A small number (13%) of these patients did have their treatment plan modified, but the changes could be made without the need for an additional visit. As well as the reduced time burden to the patient, this reduces the overall cost of care to the NHS.
For those patients who were identified as requiring a face to face assessment, the treatment plan was changed in 50% of cases. In the other 50%, the patient and parent/carer could be reassured that there were no additional concerns or that the additional issue could be corrected at a later stage. These patients could be counselled on the need for future orthodontic treatment where appropriate.
Other services who undertake GA extractions may struggle to liaise with orthodontic colleagues as they may not be sharing the same site. This is where a good working relationship with colleagues of other specialties is important and creating a means for a secure electronic exchange can be of benefit. Email is a much easier way to liaise with orthodontic colleagues than letters or face to face appointments which can be time consuming as well as costly in terms of NHS finances.
Since there are multiple clinicians referring for an orthodontic input, there can be a few differences in the information provided when referring to the orthodontist. Although this doesn't result in any significant difference in the orthodontic input received, it can sometimes delay the process as the orthodontist may ask further questions regarding the patient and the clinical scenario to assist in arriving at the final advice. We are currently developing a referral proforma to ensure that the information provided is as comprehensive as possible. This will standardise the process of obtaining orthodontic input and will make it easier for both departments to liaise effectively. From a governance and audit perspective, it will be simpler to keep a record of these referrals.
Conclusion
This evaluation has confirmed the value of an orthodontic review of patients planned for extraction of permanent teeth under general anaesthetic. This model of triaging of records by the orthodontist via email has proved successful in West Dorset. Other general anaesthetic providers should also consider this model.
References
Cobourne M T, Williams A, Harrison M. National clinical guidelines for the extraction of first permanent molars in children. Br Dent J 2014; 217: 643-648.
Gill D S, Lee R T, Tredwin C J. Treatment planning for the loss of first permanent molars. Dent Update 2001; 28: 304-308.
NHS Digital. Hospital Admitted Patient Care Activity 2017-18: Procedures and Interventions. 2018. Available at https://files.digital.nhs.uk/B6/E239FA/hosp-epis-stat-admi-proc-2017-18-tab.xlsx (accessed May 2019).
NHS Digital. Hospital Admitted Patient Care Activity 2017-18: Diagnosis. 2018. Available at https://files.digital.nhs.uk/B2/5CEC8D/hosp-epis-stat-admi-diag-2017-18-tab.xlsx (accessed May 2019).
The Faculty of Dental Surgery. The state of children's oral health in England. London: Royal College of Surgeons of England, 2015. Available at https://www.rcseng.ac.uk/-/media/files/rcs/about-rcs/government-relations-consultation/childrens-oral-health-report-final.pdf (accessed May 2019).
Alsheneifi T, Hughes C V. Reasons for dental extractions in children. Pediatr Dent 2001; 23: 109-112.
Patel A, Chawla R, Dunkley S. Managing Young Patients with Molar Incisor Hypomineralization. Dent Update 2018; 45: 471-472.
Royal College of Anaesthetists. Your child's general anaesthetic: Information for parents and guardians of children. 5th ed. 2017. Available at https://www.rcoa.ac.uk/system/files/07-ChildsAnaestheticweb.pdf (accessed May 2019).
Albadri S, Zaitoun H, McDonnell S T, Davidson L E. Extraction of first permanent molar teeth: results from three dental hospitals. Br Dent J 2007; 203: E14.
Ellis P E, Silverton S, Hollingsworth L. How can we improve orthodontic care for patients with autism and/or learning disabilities? Orth Update 2016; 9: 15-22.
da Costa-Silva C M, Jeremias F, de Souza J F, Cordeiro Rde C, Santos-Pinto L, Zuanon A C. Molar incisor hypomineralization: prevalence, severity and clinical consequences in Brazilian children. Int J Paediatr Dent 2010; 20: 426-434.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tahir, M., Ellis, P. & Hollingsworth, L. An email triage model for personalising paediatric permanent tooth extractions under general anaesthesia. Br Dent J 226, 979–984 (2019). https://doi.org/10.1038/s41415-019-0408-2
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0408-2