Abstract
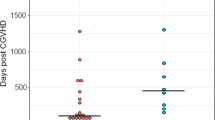
Stroke is an important complication following allogeneic hematopoietic stem cell transplantation (allo-HSCT). Nevertheless, few studies have been published to analyzed the occurrence and prognosis of stroke after allo-HSCT. From January 2007 to December 2018 in Peking University People’s Hospital, 6449 patients received HSCT and there were 2.3% of patients diagnosed with stroke after allo-HSCT (hemorrhagic: 1.0%, ischemic: 1.3%). The median time to hemorrhagic and ischemic stroke after HSCT was 161 days and 137 days, respectively. In total, 8.4% of patients experienced neurological sequelae. The outcome was much worse in patients with stroke than in control subjects. The comparison of prognosis showed no statistical differences between patients with hemorrhagic stroke and those with ischemic stroke. Significant risk factors for hemorrhagic stroke were pretransplant central nervous system leukemia (CNSL), and delayed platelet engraftment. Risk factors associated with the occurrence of ischemic stroke included high-risk disease, prior venous thromboembolism (VTE), grade III–IV acute graft-versus-host disease (aGVHD), and thrombotic microangiopathy (TMA). Haplo-identical transplantation was not a risk factor for stroke and had no impact on the prognosis compared with HLA-matched HSCT. Altogether, these results show that stroke is a severe complication after allo-HSCT. The prognosis of posttransplant stroke did not differ between hemorrhagic and ischemic stroke.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Montoro J, Sanz J, Sanz GF, Sanz MA. Advances in haploidentical stem cell transplantation for hematologic malignancies. Leukemia & Lymphoma. 2016;57:1766–75.
Zhang XH, Zhang JM, Han W, Chen H, Chen YH, Wang FR, et al. Viral encephalitis after haplo-identical hematopoietic stem cell transplantation: causative viral spectrum, characteristics, and risk factors. Eur J Haematol. 2017;98:450–8.
Zhang XH, Zhao X, Wang CC, Han W, Chen H, Chen YH, et al. IgG synthesis rate and anti-myelin oligodendrocyte glycoprotein antibody in CSF may be associated with the onset of CNS demyelination after haplo-HSCT. Ann Hematol. 2018;97:1399–406.
Iguchi A, Kobayashi R, Yoshida M, Kaneda M, Watanabe N, Cho Y, et al. Neurological complications after stem cell transplantation in childhood. Bone Marrow Transpl. 1999;24:647–52.
Dowling MR, Li S, Dey BR, McAfee SL, Hock HR, Spitzer TR, et al. Neurologic complications after allogeneic hematopoietic stem cell transplantation: risk factors and impact. Bone Marrow Transpl. 2018;53:199–206.
World Health Organization. Global status report on noncommunicable diseases 2014. Women. 2014;47:2562–3.
Peisker T, Koznar B, Stetkarova I, Widimsky P. Acute stroke therapy: a review. Trends Cardiovasc Med. 2017;27:59–66.
Coplin WM, Cochran MS, Levine SR, Crawford SW. Stroke after bone marrow transplantation: frequency, aetiology and outcome. Brain. 2001;124:1043–51.
Bleggi-Torres LF, de Medeiros BC, Werner B, Neto JZ, Loddo G, Pasquini R, et al. Neuropathological findings after bone marrow transplantation: an autopsy study of 180 cases. Bone Marrow Transpl. 2000;25:301–7.
Wang Y, Liu DH, Liu KY, Xu LP, Zhang XH, Han W, et al. Long-term follow-up of haploidentical hematopoietic stem cell transplantation without in vitro T cell depletion for the treatment of leukemia: nine years of experience at a single center. Cancer. 2013;119:978–85.
Chang YJ, Huang XJ. Use of G-CSF-stimulated marrow in allogeneic hematopoietic stem cell transplantation settings: a comprehensive review. Clin Transplant. 2011;25:13–23.
Shulman HM, Sullivan KM, Weiden PL, McDonald GB, Striker GE, Sale GE, et al. Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am J Med. 1980;69:204–17.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. Consensus conference on acute Gvhd grading. Bone Marrow Transpl. 1995;15:825–8.
Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, et al. National Institutes of Health Consensus Development Project on criteria for clinical trials in chronic graft-versus-host disease: I. The 2014 Diagnosis and Staging Working Group report. Biol Blood Marrow Transplant. 2015;21:389–401.
Huang XJ, Liu DH, Liu KY, Xu LP, Chen H, Han W, et al. Haploidentical hematopoietic stem cell transplantation without in vitro T-cell depletion for the treatment of hematological malignancies. Bone Marrow Transpl. 2006;38:291–7.
Yan CH, Xu LP, Wang FR, Chen H, Han W, Wang Y, et al. Causes of mortality after haploidentical hematopoietic stem cell transplantation and the comparison with HLA-identical sibling hematopoietic stem cell transplantation. Bone Marrow Transpl. 2016;51:391–7.
Xu L, Xu Z, Wang F, Mo X, Han T, Han W, et al. Unmanipulated haploidentical transplantation conditioning with busulfan, cyclophosphamide and anti-thymoglobulin for adult severe aplastic anaemia. Bone Marrow Transplant. 2018;53:188–92.
Muir KW. Stroke. Medicine. 2009;37:109–14.
Howard G, Robin S. The management of ischaemic stroke. Intensive Care Med. 2016;17:591–5.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Executive summary: heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133:447–54.
Granitto M, Galitz D. Update on stroke: the latest guidelines. Nurse Practitioner. 2008;33:39–46.
Khoury B, Kogan C, Daouk S. International Classification of Diseases 11th ed. (ICD-11). In: Zeigler-Hill V, Shackelford TK, editors. Encyclopedia of personality and individual differences. Springer International Publishing: Cham; 2017. p. 1–6.
Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Murray C. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. 2014;383:245–55.
Hankey GJ. Blacker DJJB. Is it a stroke? BMJ. 2015;350:h56.
Wintermark M, Sanelli PC, Albers GW, Bello JA, Derdeyn CP, Hetts SW, et al. Imaging recommendations for acute stroke and transient ischemic attack patients: a joint statement by the American Society of Neuroradiology, the American College of Radiology and the Society of NeuroInterventional Surgery. J Am Coll Radiol. 2013;34:E117–27.
Murdoch DR, Corey GR, Hoen B, Miro JM, Fowler VG Jr, Bayer AS, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009;169:463–73.
Rincon F, Dhamoon M, Moon Y, Paik MC, Boden-Albala B, Homma S, et al. Stroke location and association with fatal cardiac outcomes: Northern Manhattan Study (NOMAS). Stroke. 2008;39:2425–31.
Kang JM, Kim YJ, Kim JY, Cho EJ, Lee JH, Lee MH, et al. Neurologic complications after allogeneic hematopoietic stem cell transplantation in children: analysis of prognostic factors. Biol Blood Marrow Transplant. 2015;21:1091–8.
Chen CY, Tai CH, Cheng A, Wu HC, Tsay W, Liu JH, et al. Intracranial hemorrhage in adult patients with hematological malignancies. BMC Med. 2012;10:97–106.
Lin TA, Gau JP, Liu YC, Ko PS, Wang HY, Chien SH, et al. Cerebrovascular disease after allogeneic hematopoietic stem cell transplantation: incidence, risk, and clinical outcome. Int J Hematol. 2019;109:584–92.
Armitage JO. Bone marrow transplantation. N Engl J Med. 1994;330:827–38.
Gragert L, Eapen M, Williams E, Freeman J, Spellman S, Baitty R, et al. HLA match likelihoods for hematopoietic stem-cell grafts in the U.S. registry. N Engl J Med. 2014;371:339–48.
Xu LP, Jin S, Wang SQ, Xia LH, Bai H, Gao SJ, et al. Upfront haploidentical transplant for acquired severe aplastic anemia: registry-based comparison with matched related transplant. J Hematol Oncol. 2017;10:25–35.
Han LJ, Wang Y, Fan ZP, Huang F, Zhou J, Fu YW, et al. Haploidentical transplantation compared with matched sibling and unrelated donor transplantation for adults with standard-risk acute lymphoblastic leukaemia in first complete remission. Br J Haematol. 2017;179:120–30.
Siegal D, Keller A, Xu W, Bhuta S, Kim DH, Kuruvilla J, et al. Central nervous system complications after allogeneic hematopoietic stem cell transplantation: incidence, manifestations, and clinical significance. Biol Blood Marrow Transplant. 2007;13:1369–79.
Armenian SH, Sun CL, Mills G, Teh JB, Francisco L, Durand JB, et al. Predictors of late cardiovascular complications in survivors of hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2010;16:1138–44.
Chow EJ, Baker KS, Lee SJ, Flowers ME, Cushing-Haugen KL, Inamoto Y, et al. Influence of conventional cardiovascular risk factors and lifestyle characteristics on cardiovascular disease after hematopoietic cell transplantation. J Clin Oncol. 2014;32:191–8.
Hurst RW, Judkins A, Bolger W, Chu A, Loevner LA. Mycotic aneurysm and cerebral infarction resulting from fungal sinusitis: imaging and pathologic correlation. AJNR Am J Neuroradiol. 2001;22:858–63.
Chow EJ, Mueller BA, Baker KS, Cushing-Haugen KL, Flowers MED, Martin PJ, et al. Cardiovascular hospitalizations and mortality among recipients of hematopoietic stem cell transplantation. Ann Intern Med. 2011;155:21–32.
Markus HS. Stroke: causes and clinical features. Medicine. 2004;32:57–61.
Labrador J, Lopez-Anglada L, Perez-Lopez E, Lozano FS, Lopez-Corral L, Sanchez-Guijo FM, et al. Analysis of incidence, risk factors and clinical outcome of thromboembolic and bleeding events in 431 allogeneic hematopoietic stem cell transplantation recipients. Haematologica. 2013;98:437–43.
Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Au R, Kannel WB, et al. The lifetime risk of stroke: estimates from the Framingham Study. Stroke. 2006;37:345–50.
Reeves MJ, Bushnell CD, Howard G, Gargano JW, Duncan PW, Lynch G, et al. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008;7:915–26.
Hankey G. Stroke. Lancet. 2017;389:641–54.
Neil P. What does the odds ratio estimate in a case-control study? Int J Epidemiol. 1993;22:1189–92.
Rosner B, Cengage L. Fundamentals of biostatistics. Am Stn. 2011;61:183.
Zhang XH, Liu X, Wang QM, He Y, Zhu XL, Zhang JM, et al. Thrombotic microangiopathy with concomitant GI aGVHD after allogeneic hematopoietic stem cell transplantation: Risk factors and outcome. Eur J Haematol. 2018;100:171–81.
Raiola AM, Dominietto A, di Grazia C, Lamparelli T, Gualandi F, Ibatici A, et al. Unmanipulated haploidentical transplants compared with other alternative donors and matched sibling grafts. Biol Blood Marrow Transplant. 2014;20:1573–9.
Ciurea SO, Mulanovich V, Saliba RM, Bayraktar UD, Jiang Y, Bassett R, et al. Improved early outcomes using a T cell replete graft compared with T cell depleted haploidentical hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2012;18:1835–44.
Najima Y, Ohashi K, Miyazawa M, Nakano M, Kobayashi T, Yamashita T, et al. Intracranial hemorrhage following allogeneic hematopoietic stem cell transplantation. Am J Hematol. 2009;84:298–301.
Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol. 2009;8:355–69.
Pihusch R, Salat C, Schmidt E, Gohring P, Pihusch M, Hiller E, et al. Hemostatic complications in bone marrow transplantation: a retrospective analysis of 447 patients. Transplantation. 2002;74:1303–9.
Nassar AA. Haploidentical stem cell transplantation. Hematol/Oncol Stem Cell Ther. 2012;5:73–83.
Ferrara J. Graft-versus-host disease. N Engl J Med. 2009;373:1550–61.
Teshima T, Ordemann R, Reddy P, Gagin S, Liu C, Cooke KR, et al. Acute graft-versus-host disease does not require alloantigen expression on host epithelium. Nat Med. 2002;8:575–81.
Zhang XH, Wang QM, Chen H, Chen YH, Han W, Wang FR, et al. Clinical characteristics and risk factors of Intracranial hemorrhage in patients following allogeneic hematopoietic stem cell transplantation. Ann Hematol. 2016;95:1637–43.
Gardner AW, Montgomery PS, Casanegra AI, Silva-Palacios F, Ungvari Z, Csiszar A. Association between gait characteristics and endothelial oxidative stress and inflammation in patients with symptomatic peripheral artery disease. Age (Dordr). 2016;38:64–73.
Hilgendorf I, Wilhelm S, Prall F, Junghanss C, Steiner B, Wolff D, et al. Headache after hematopoietic stem cell transplantation: being aware of chronic bilateral subdural hematoma. Leuk Lymphoma. 2006;47:2247–9.
Morgenstern LB, Hemphill JC, Anderson C, Becker K, Broderick JP, Connolly ES, et al. Guidelines for the management of spontaneous intracerebral hemorrhage A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2010;41:2108–29.
Naidech AM. Intracranial hemorrhage. Am J Respir Crit Care Med. 2011;184:998–1006.
Isabel C, Calvet D, Mas JL. Stroke prevention. La Presse Médicale. 2016;45:e457–71.
Acknowledgements
The authors would like to thank all the patients and medical staff who took part in the study. The authors also thank the department of medical record library for providing data. This work was supported by National Natural Science Foundation of China (No. 81670116), Key Program of National Natural Science Foundation of China (No. 81730004), Beijing Natural Science Foundation (Nos. 7171013, H2018206423), Beijing Municipal Science and Technology Commission (No. Z171100001017084), the National Key Research and Development Program of China (No. 2017YFA0105500, No. 2017YFA0105503), and the Foundation for Innovative Research Groups of the National Natural Science Foundation of China (81621001).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Cai, X., Fu, HX., Mo, XD. et al. Comparison of hemorrhagic and ischemic stroke after allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 55, 2087–2097 (2020). https://doi.org/10.1038/s41409-020-0903-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-020-0903-8
This article is cited by
-
Clinical risk factors and prognostic model for patients with bronchiolitis obliterans syndrome after hematopoietic stem cell transplantation
Bone Marrow Transplantation (2023)