Abstract
Corneal wounds usually heal quickly; but diabetic patients have more fragile corneas and experience delayed and painful healing. In the present study, we compared the healing capacity of corneal epithelial cells (CECs) between normal and diabetic conditions and the potential mechanisms. Primary murine CEC derived from wild-type and diabetic (db/db) mice, as well as primary human CEC were prepared. Human CEC were exposed to high glucose (30 mM) to mimic diabetic conditions. Cell migration and proliferation were assessed using Scratch test and MTT assays, respectively. Reactive oxygen species (ROS) production in the cells was measured using dichlorofluorescein reagent. Western blot was used to evaluate the expression levels of Akt. Transepithelial electrical resistance (TEER) and zonula occludens-1 (ZO-1) expression were used to determine tight junction integrity. We found that the diabetic CEC displayed significantly slower cell proliferation and migration compared with the normal CEC from both mice and humans. Furthermore, ROS production was markedly increased in CEC grown under diabetic conditions. Treatment with an antioxidant N-acetyl cysteine (NAC, 100 μM) significantly decreased ROS production and increased wound healing in diabetic CEC. Barrier function was significantly reduced in both diabetic mouse and human CEC, while NAC treatment mitigated these effects. We further showed that Akt signaling was impaired in diabetic CEC, which was partially improved by NAC treatment. These results show that diabetic conditions lead to delayed wound-healing capacity of CEC and impaired tight junction formation in both mice and human. Increased ROS production and inhibited Akt signaling may contribute to this outcome, implicating these as potential targets for treating corneal wounds in diabetic patients.
Similar content being viewed by others
Introduction
Diabetes mellitus is a common chronic endocrinopathy, characterized by hyperglycemia and either insulin insufficiency or insulin resistance. The World Health Organization estimates that the global prevalence of diabetes in 2014 was 9% and suggests that diabetes will be one of the top 10 leading causes of death by 2030 [1]. Nearly 29.1 million people in the United States alone live with diabetes, and the Centers for Disease Control estimates that approximately 86 million Americans were prediabetic in 2012. The impaired metabolism of glucose results in alterations in macro- and microvascular circulation, giving rise to multiple complications in patients with diabetes, including neuropathy, nephropathy, and cardiovascular complications [2]. In addition, morbidity related to ocular complications of diabetes is increasing considerably at a rate commensurate to nearly 1.4 million new diabetic cases diagnosed in the United States each year [1, 3].
Dysregulation of corneal homeostasis has been well documented in human diabetics [3, 4]. Nearly half of all diabetic patients develop some degree of degenerative corneal disease, termed diabetic keratopathy, due to compromised epithelial barrier function, morphologic changes to the epithelial and endothelial cells, hypertrophy of the epithelial basement membrane, and diminished corneal sensitivity [3, 5, 6]. Unfortunately, even minor disruptions to the diabetic cornea can lead to prolonged healing times or persistent epithelial defects [3, 5, 6]. Delayed healing predisposes diabetic patients to sight-threatening complications, such as progressive epithelial thinning, resulting in secondary corneal injury and induction of cytokines and thus increasing the potential for fibrotic scar formation [5,6,7,8]. As such, understanding the pathophysiology associated with the diabetic cornea is of great importance in maintaining the corneal integrity of diabetic patients [3, 4].
Rapid re-epithelialization and restoration of the epithelial barrier is critical in maintaining the structural integrity and normal function of the cornea [9]. As part of this process, tight junctions play an important role in the establishment of corneal homeostasis and epithelial barrier formation. Tight junctions are present in the corneal epithelium, and zonula occludens (ZO)-1 can be observed in a continuous pattern at the apical cell borders [10]. Elevation of reactive oxygen species (ROS) has been demonstrated to reduce tight junction proteins and epithelial barrier integrity [11, 12]. Furthermore, increased oxidative stress due to ROS production has been implicated as having a causative role in diabetic complications [13]. Regarding to the eye, there are reports associating alterations in ROS production to diabetic corneal complications [14,15,16]. To date, there is limited information on the effects of hyperglycemia on ROS production and restoration of corneal epithelial barrier function [17, 18].
In the present study, we investigated corneal epithelial proliferation, wound healing, and barrier function in hyperglycemic conditions. Our findings indicate that increased ROS production, in response to high glucose treatment, impairs Akt signaling in the corneal epithelium and significantly decreases epithelial integrity.
Materials and methods
Cell culture
Mouse primary corneal epithelial cells (mCECs), diabetic mCECs (dmCECs), and human primary CECs (hCECs) were purchased from Cell Biologics, Inc. (Chicago, IL). mCEC and dmCEC were maintained in mouse epithelial cell medium (Cell Biologics, Inc., cat. no. M6621), and hCEC were maintained in human epithelial cell medium (Cell Biologics, Inc., cat. no. H6621) containing 5 mmol/L (normal glucose) or 30 mM D-glucose (high glucose); all were maintained in a 5% CO2 humidified incubator at 37 °C. A stratified CEC model (Lonza, Inc., Walkersville, MD), isolated from clinically normal corneal tissues of humans, was used to evaluate ROS production and transepithelial electrical resistance (TEER). For the stratified CEC model, cells were seeded on polyester membranes coated with rat tail collagen type I. Cultures were incubated at the air–liquid interface to achieve stratification of 6–7 cell layers. To achieve equilibration, tissue cultures were transferred from the supplied gel-based medium to a sterile plate, and supplemented corneal epithelial differentiation medium (Lonza) was added. Plates were incubated overnight at 37 °C with 5% CO2 and 95% humidity. After equilibration, tissue cultures were treated by application of either 5 or 30 mM D-glucose. Mannitol (20 mmol/L) was used as an osmotic control; no differences were noted in any experiments (data not shown).
Cell proliferation
Cells were first seeded onto a 96-well plate at a density of 1000 cells per well and then incubated for different times, as indicated. Subsequently, 3-(4, 5-dimethylthiazolyl-2)-2, 5-diphenyl-tetrazolium bromide (MTT) was added to each well at a final concentration of 0.5 mg/mL. After incubation for 4 h, formazan crystals were dissolved in 100 μL of dimethylsulfoxide (DMSO) and absorbance at 570 nm was measured using a plate reader. A separate group of cells was used for a colony formation assay. Briefly, 1 × 104 cells were initially seeded into each well of a six-well plate and maintained in growth medium. The medium was changed every 3 days. Six days after initial seeding, the cells were fixed with methanol and stained with 1% Rhodamine B for 15 min before being counted. The colony numbers were counted using ImageJ software. All experiments were repeated three times.
Cell migration
Cells were cultured in their respective medium with or without N-acetyl cysteine (NAC; 50 µM) for 24 h until they reached 90% confluence, subsequently scratched with a micropipette tip, and incubated. Images were taken at 0, 3, 6, 12, and 24 h after the initial scratch. Digital images of wound closure were used for quantitative assessment of migration using ImageJ software.
Measurement of intracellular ROS
For observation of intracellular ROS staining, cells were first seeded onto a 24-well plate and allowed to grow for 1 day. The cells were treated with ROS fluorescence probe ROS BriteTM570 (10 μM) and incubated for 30 min at 37 °C. Staining was observed and captured for quantification through the use of ImageJ software. To evaluate ROS production in the stratified human CEC, dichlorofluorescein reagent (Molecular Probes, Eugene, OR) was diluted (5 µM) with phosphate buffered saline (PBS) solution in accordance with the manufacturer’s instructions and added to each well. Cells were incubated with the dichlorofluorescein reagent at 37 °C for 30 min. The dichlorofluorescein reagent was removed and the cells were washed gently with PBS solution. The cells were then exposed to glucose or the control for 24 h. Fluorescence was measured with an automated microplate reader, with ROS production directly proportional to the measured fluorescence.
Western blot
Total protein was extracted from the indicated cells in RIPA buffer. Protein (30 µg) from each sample was separated using 10% sodium dodecyl sulfate polyacrylamide gel electrophoresis and transferred to polyvinylidene difluoride membranes at 4 °C. Membranes were blocked with 5% nonfat milk and incubated with the indicated primary antibodies overnight at 4 °C under rotation. Secondary antibodies, conjugated horseradish peroxidase anti-mouse or anti-rabbit IgG, were applied at a 1:5000 dilution and incubated for 1 h on a shaker at room temperature. Immunoblots were visualized with an ECL plus kit (Pierce, Rockford, IL). The antibodies used in this study were as follows: anti-p-Akt (S473) antibody (Cell Signaling Technology, Danvers, MA; cat. no. 4060), anti-Akt (pan) antibody (Cell Signaling Technology, cat. no. 4691), and anti-β-actin antibody (Sigma-Aldrich, St Louis, MO; cat. no. A5441).
Epithelial barrier assessment
Immunofluorescence for ZO-1 and TEER was used as indicators of epithelial barrier integrity. Cells were grown on 12 mm Transwell® filters (Corning Incorporated, Corning, NY). TEER was determined with an Evom2 epithelial voltohmmeter (World Precision Instruments, Sarasota, FL). Before each measurement, the Evom2 was zeroed according to the manufacturer's directions, and the background resistance was determined using cell-free filters. Cells were exposed to either 5 or 30 mM D-glucose and measurements were performed at 12 and 24 h. Background was subtracted and values were adjusted to ohms multiplied by area (1.12 cm2) of the Transwell® inserts.
Twenty-four hours after initially seeding cells on glass coverslips, CEC were treated with normal or high glucose for 24 h. The cells were subsequently stained for expression of ZO-1 (Invitrogen, Carlsbad, CA; cat. no. 40-2200). Briefly, the cells were rinsed with PBS, then fixed with 4% paraformaldehyde for 10 min at room temperature, and rinsed three times with PBS. The cells were permeabilized with 0.2% Triton X-100 for 10 min before blocking with 5% nonfat milk for 30 min. The cells were incubated with primary antibody overnight at 4 °C. The cells were rinsed with PBS three times, then incubated with secondary antibody and Hoechst 33258 for 1 h in the dark. The cells were washed with PBS and placed on coverslips mounted on glass slides and kept at 4 °C until imaged. Micrographs were acquired using a fluorescence microscope (Carl Zeiss LSM 780, Germany).
Statistical analysis
All data are expressed as the mean±S.D. Groups were compared by Student’s t-test and analysis of variance for repeated measures. A value of P < 0.05 was considered significant.
Results
Diabetic conditions reduce CEC proliferation and migration
To determine the influence of diabetic conditions on the proliferative capacity of CEC, the mCEC and dmCEC were cultured for 1–5 days. As observed in Fig. 1a, the growth rate of dmCEC was slower in comparison with normal mCEC. Furthermore, the proliferation rate of hCEC was impaired by high glucose treatment (Fig. 1b). This observation was also confirmed by colony formation assay (Fig. 1c), where the normal CECs formed about twice as many colonies as diabetic CECs during 6 days of culture (Fig. 1d).
Diabetes inhibits corneal epithelial cell proliferation. Mouse primary corneal epithelial cell (mCEC) and diabetic mCEC (dmCEC) proliferation was measured using an 3-(4, 5-dimethylthiazolyl-2)-2, 5-diphenyltetrazolium bromide (MTT) assay after growth for 1–5 days (a). Human primary CEC (hCEC) proliferation was measured using an MTT assay after growth for 1–5 days with normal glucose or high glucose (30 mM) (b). (c, d) A colony formation assay also showed higher colony-forming ability of both mCEC and hCEC over their diabetic counterparts, dmCEC and hCEC + glucose, respectively. n = 3 independent experiments. Mean ± S.D. *P < 0.05; **P < 0.01
To assess the effect of diabetes on CEC migration in vitro, a scratch healing model was used. The mCEC and hCEC cultured in normal glucose levels underwent the expected migration in response to scratch wounding. By comparison, dmCEC and high glucose-treated hCEC showed significant delays in cellular migration (Fig. 2). Collectively, these results indicate that CEC exhibit lower proliferation and migration rates under diabetic conditions.
Diabetes inhibits corneal epithelial cell migration in vitro. Cell migration was observed at the indicated time points after generation of the scratch (a, b). Relative migration distances for the indicated cells were quantified (c, d). n = 4 independent experiments. Mean ± S.D. *P < 0.05; **P < 0.01
Diabetic CECs increase intracellular ROS generation
To determine potential differences in diabetic corneal ROS production, ROS levels were evaluated in each of the CEC lines and culture conditions. Representative results show that the number of cells with high fluorescence intensity was significantly increased in diabetic CEC compared with normal CEC (Figs. 3a, b). To mimic the physiologic condition, a stratified human CEC model was exposed to normal and high glucose conditions. Consistent with our observations in the monolayer cultures, we demonstrate that high glucose treatment results in a significant increase in ROS production in stratified human CEC (Fig. 3c).
Diabetic corneal epithelial cells increase the generation of intracellular reactive oxygen species (ROS). Representative images were observed and captured after 24 h of culture (a), and the ROS Brite intensity was analyzed by ImageJ software (b). n = 4 independent experiments. In cultured stratified human primary CEC (hCEC), ROS production was significantly increased (c). n = 3 or 6 independent experiments. Mean ± S.D. **P < 0.01
NAC treatment improves diabetic CECs migration
To evaluate a causative relationship between ROS generation in diabetic conditions and delayed CEC migration, cells were treated with the nonspecific ROS scavenger, NAC. As observed in Fig. 4, NAC treatment could reverse the delayed migration observed under diabetic conditions, suggesting that excessive ROS generated by diabetic CEC may inhibit CEC migration.
N-acetyl cysteine (NAC) reverses the observed delay in migration under diabetic conditions. Cell migration was observed at the indicated time points after the scratch wound with or without NAC (100 µM; a, b). The relative migration distances for the indicated cells were quantified (c, d). n = 4 independent experiments. Mean ± S.D. *P < 0.05; **P < 0.01
Epithelial barrier formation is reduced in diabetic CECs
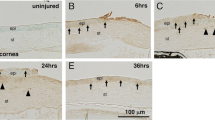
When stratified CEC were incubated with high levels of glucose for 24 h, a reduction in CEC layers was observed (Fig. 5a). TEER measurements confirmed that the integrity of the stratified CEC was compromised under hyperglycemic conditions; a significant reduction in TEER values was observed at both 12 and 24 h in cells treated with high glucose compared with cells with normal glucose (Fig. 5b). In CEC monolayers, TEER values were also significantly lower under diabetic conditions compared with normal conditions (Fig. 5c). Expression of ZO-1 confirmed that tight junction formation was reduced in dmCEC and hyperglycemia-treated hCEC (Fig. 5d). Application of NAC significantly improved TEER values in CEC cultured under diabetic conditions; ZO-1 expression was also restored with NAC treatment (Fig. 5).
Hyperglycemia compromises corneal epithelial barrier function. Stratified human primary CEC (hCEC) have a reduced number of corneal epithelial cell (CEC) layers (a) and significantly reduced transepithelial electrical resistance (TEER) values in the presence of high glucose (b). Significantly lower TEER values were observed in cellular monolayers under diabetic conditions at each indicated time point; treatment with NAC significantly restored barrier function (c, d). Expression of zonula occludens-1 (ZO-1) was reduced following treatment with high glucose and this effect was mitigated by NAC treatment (e). n = 6 independent experiments. Mean ± S.D. *P < 0.05; **P < 0.01
p-Akt signaling is altered in diabetic CECs
To elucidate the mechanism underlying diabetic condition-induced inhibition of growth and migration, we investigated phosphorylated Akt (p-Akt) in both normal and diabetic CEC. Expression of p-Akt was significantly downregulated in dmCEC and hCEC treated with high glucose; NAC treatment was able to mitigate these effects (Fig. 6).
Downregulation of phosphorylated Akt (p-Akt) pathways in diabetic corneal epithelial cells. The indicated cells were subjected to Western blot using antibodies to p-Akt, total Akt, and β-actin (loading control; a, b). The normalized expression level was analyzed by ImageJ software. n = 3 independent experiments (c, d). Mean ± S.D. **P < 0.01
Discussion
With rapid increases in the prevalence of diabetes mellitus worldwide, ocular complications have become a leading cause of blindness [19]. Further, because those afflicted with cardiometabolic syndrome are potentially insulin resistant and diabetic, there is a large population of individuals at risk for developing diabetic corneal complications [20]. It has been reported that between 47% and 64% of diabetic patients had evidence of corneal abnormalities upon examination; and delayed corneal epithelial healing is a serious complication of diabetes [14, 21, 22]. Notably, those undergoing cataract surgery or vitrectomy associated with diabetic retinopathy are at particular risk, as damage to the corneal epithelium during the procedure results in a considerable delay in re-epithelialization [3, 23,24,25]. In the present study, we investigated the in vitro alterations in CEC when grown under diabetic conditions. We found that hyperglycemia reduced CEC proliferation, migration, and barrier function; and this effect was reversed with NAC treatment.
Re-epithelialization, proliferation, and restoration of barrier function are integral for wound healing and normal function of the cornea. Our data highlight the role of suppressed cellular migration and proliferation as underlying mechanisms for delayed epithelial wound healing in the diabetic cornea. Our results on reduced CEC migration under diabetic conditions are in agreement with other studies [14, 15, 18]. There are, however, discrepant results on the effects of diabetes on CEC proliferation. Both in vitro and in vivo studies have documented impaired cellular proliferation in hyperglycemic corneas [14, 21, 26,27,28]. Clinically, several studies have additionally demonstrated lower basal epithelial cell density in diabetic corneas and have suggested that this reduction in density is due, in part, to diminished proliferative capacity [29,30,31]. In contrast, others have documented that high glucose increases cell proliferation [32,33,34]. These discrepancies may be due to differences in the type of model used to evaluate changes in diabetic corneas. As an example, Chikama et al. [33] observed increased CEC proliferative capacity in GK rats; however, the authors suggest that this rodent model has an immature phenotype, which may explain the differences observed.
Loss of junctional proteins can lead to a number of corneal pathologies ranging from epithelial defects to corneal infections [35, 36]. We report that ZO-1 expression is decreased under diabetic conditions. This reduction in ZO-1 staining occurs with a concomitant decrease in barrier function, as revealed by the measurement of TEER values. Consistent with our findings, Huang et al. found delayed reformation of tight junctions in a diabetic rat model [17]. It is well documented in other cell types that increased oxidative stress can result in decreased expression of tight junction proteins [37,38,39,40]. In the present study, not only did antioxidant treatment restore CEC proliferation and migration under diabetic conditions, NAC also improved both TEER values and ZO-1 expression. These data suggest that there is a causative relationship between ROS production and corneal barrier function.
Excess oxidative stress, resulting from enhanced accumulation of ROS and impaired antioxidant capabilities in response to hyperglycemia, has been postulated as an important pathological mechanism in diabetes. In comparison, the reduction of ROS has been shown to attenuate the progression of various diabetes complications, including complications in the cornea [41,42,43,44,45,46,47]. While the effects of hyperglycemia on oxidative stress within the cornea remain an active area of research, this study indicates that the impaired Akt signaling response is a major cause for increased ROS production and delayed epithelial wound healing. The PI3-kinase/Akt pathway is integral in normal corneal migration and proliferation and has previously been shown to play an important role in the diabetic cornea [48,49,50]. As such, it is not surprising that both Akt activation and corneal healing are impaired in our work. Interestingly, there has only been one other publication documenting the role of ROS-mediated Akt signaling in the diabetic cornea and no published reports regarding the involvement of tight junctions relative to the Akt pathway under diabetic conditions. Application of the antioxidant, NAC, mitigated these negative effects in CEC, implicating excessive oxidative stress via the Akt pathway in the underlying pathophysiology of diabetic corneal complications. It is also worth mentioning that different subtypes of Akt might play differential roles in physiology and pathophysiology [51]. Thus, our future studies will focus on dissecting specific roles of each subtype of Akt in diabetic corneal wound healing.
An obvious limitation of this work is that all experiments were performed in vitro and only evaluated the effects of hyperglycemia in the corneal epithelium. Both corneal nerves and corneal stromal cells have been shown to respond to changes in glucose and have impaired signaling in the diabetic cornea [52]. Future work should expand on the presented data to incorporate three-dimensional models and the in vivo condition. In support of our data, the use of both mouse and human primary CEC confirms that our findings have potential relevance in multiple species.
Overall, we demonstrate that under diabetic conditions, CEC have reduced migration and barrier functions, which correlate to impaired Akt signing and increased ROS production. Use of an antioxidant counteracts the effects of corneal epithelial hyperglycemia. The current standard of care for corneal disease associated with diabetes is insufficient to retain comfort and vision in affected patients, and the need exists to explore alternative or adjunctive therapies for better control of diabetic ocular surface disease [4]. As such, our promising in vitro results suggest that mitigating oxidative stress within the diabetic cornea could work as a therapeutic approach, serving to minimize the morbidity and associated health care costs related to the treatment of diabetic keratopathy.
References
Mendis S, Davis S, Norrving B. Organizational update the World Health Organization global status report on noncommunicable diseases 2014; one more landmark step in the combat against stroke and vascular disease. Stroke. 2015;46:E121–E2.
Rask-Madsen C, King GL. Vascular complications of diabetes: mechanisms of injury and protective factors. Cell Metab. 2013;17:20–33.
Kaji Y. Prevention of diabetic keratopathy. Br J Ophthalmol. 2005;89:254–5.
Abdelkader H, Patel DV, McGhee CNJ, Alany RG. New therapeutic approaches in the treatment of diabetic keratopathy: a review. Clin Exp Ophthalmol. 2011;39:259–70.
Gekka M, Miyata K, Nagai Y, Nemoto S, Sameshima T, Tanabe T, et al. Corneal epithelial barrier function in diabetic patients. Cornea. 2004;23:35–7.
Azar DT, Spurrmichaud SJ, Tisdale AS, Gipson IK. Altered epithelial basement-membrane interactions in diabetic corneas. Arch Ophthalmol-Chic. 1992;110:537–40.
Desai BM, Lavingia BC. Cornea thickness and tear glucose levels in diabetes mellitus and normal persons. Indian J Ophthalmol. 1987;35:130–2.
Wilson SE, Liu JJ, Mohan RR. Stromal-epithelial interactions in the cornea. Prog Retin Eye Res. 1999;18:293–309.
Yin J, Yu FS. Rho kinases regulate corneal epithelial wound healing. Am J Physiol Cell Physiol. 2008;295:C378–87.
McCartney MD, Cantu-Crouch D. Rabbit corneal epithelial wound repair: tight junction reformation. Curr Eye Res. 1992;11:15–24.
Li J, Zhang R, Wang C, Wang X, Xu M, Ma J, et al. Activation of the small GTPase Rap1 inhibits choroidal neovascularization by regulating cell junctions and ROS generation in rats. Curr Eye Res. 2018;43:934–40.
Yu L, Gan X, Liu X, An R. Calcium oxalate crystals induces tight junction disruption in distal renal tubular epithelial cells by activating ROS/Akt/p38 MAPK signaling pathway. Ren Fail. 2017;39:440–51.
Dehdashtian E, Mehrzadi S, Yousefi B, Hosseinzadeh A, Reiter RJ, Safa M, et al. Diabetic retinopathy pathogenesis and the ameliorating effects of melatonin; involvement of autophagy, inflammation and oxidative stress. Life Sci. 2018;193:20–33.
Xu KP, Li Y, Ljubimov AV, Yu FS. High glucose suppresses epidermal growth factor receptor/phosphatidylinositol 3-kinase/Akt signaling pathway and attenuates corneal epithelial wound healing. Diabetes. 2009;58:1077–85.
Zhang Z, Hu X, Qi X, Di G, Zhang Y, Wang Q, et al. Resolvin D1 promotes corneal epithelial wound healing and restoration of mechanical sensation in diabetic mice. Mol Vis. 2018;24:274–85.
Shi L, Chen HM, Yu XM, Wu XY. Advanced glycation end products delay corneal epithelial wound healing through reactive oxygen species generation. Mol Cell Biochem. 2013;383:253–9.
Huang CC, Liao RF, Wang F, Tang ST. Characteristics of reconstituted tight junctions after corneal epithelial wounds and ultrastructure alterations of corneas in type 2 diabetic rats. Curr Eye Res. 2016;41:783–90.
Yin J, Huang J, Chen C, Gao N, Wang F, Yu FSX. Corneal complications in streptozocin-induced type I diabetic rats. Invest Ophth Vis Sci. 2011;52:6589–96.
Lutty GA. Effects of diabetes on the eye. Invest Ophth Vis Sci. 2013; 54:ORSF81-ORSF87.
Zhang YM, Whaley-Connell AT, Sowers JR, Ren J. Autophagy as an emerging target in cardiorenal metabolic disease: from pathophysiology to management. Pharmacol Ther. 2018;191:1–22.
Zagon IS, Klocek MS, Sassani MW, McLaughlin P. Use of topical insulin to normalize corneal epithelial healing in diabetes mellitus. Arch Ophthalmol-Chic. 2007;125:1082–8.
Schultz RO, Peters MA, Sobocinski K, Nassif K, Schultz KJ. Diabetic keratopathy as a manifestation of peripheral neuropathy. Am J Ophthalmol. 1983;96:368–71.
Friend J, Ishii Y, Thoft RA. Corneal epithelial changes in diabetic rats. Ophthalmic Res. 1982;14:269–78.
Schulze SD, Sekundo W, Kroll P. Autologous serum for the treatment of corneal epithelial abrasions in diabetic patients undergoing vitrectomy. Am J Ophthalmol. 2006;142:207–11.
Basher AWP, Roberts SM. Ocular manifestations of diabetes-mellitus-diabetic cataracts in dogs. Vet Clin N Am-Small. 1995;25:661–76.
Di GH, Du XL, Qi X, Zhao XW, Duan HY, Li SX, et al. Mesenchymal stem cells promote diabetic corneal epithelial wound healing through TSG-6-dependent stem cell activation and macrophage switch. Invest Ophth Vis Sci. 2017;58:4344–54.
Yan CX, Gao N, Sun HJ, Yin J, Lee P, Zhou L, et al. Targeting imbalance between IL-1 beta and IL-1 receptor antagonist ameliorates delayed epithelium wound healing in diabetic mouse corneas. Am J Pathol. 2016;186:1466–80.
Nagai N, Ito Y. Therapeutic effects of sericin on diabetic keratopathy in Otsuka Long-Evans Tokushima Fatty rats. World J Diabetes. 2013;4:282–9.
Qu JH, Tian L, Zhang XY, Sun XG. Early central and peripheral corneal microstructural changes in type 2 diabetes mellitus patients identified using in vivo confocal microscopy: a case-control study. Medicine 2017; 96:e7960.
Chang PY, Carrel H, Huang JS, Wang IJ, Hou YC, Chen WL, et al. Decreased density of corneal basal epithelium and subbasal corneal nerve bundle changes in patients with diabetic retinopathy. Am J Ophthalmol. 2006;142:488–90.
Quadrado MJ, Popper M, Morgado AM, Murta JN, Van Best JA. Diabetes and corneal cell densities in humans by in vivo confocal microscopy. Cornea. 2006;25:761–8.
McDermott AM, Kern TS, Murphy CJ. The effect of elevated extracellular glucose on migration, adhesion and proliferation of SV40 transformed human corneal epithelial cells. Curr Eye Res. 1998;17:924–32.
Chikama T, Wakuta M, Liu Y, Nishida T. Deviated mechanism of wound healing in diabetic corneas. Cornea. 2007;26:S75–S81.
Goto Y, Suzuki K, Ono T, Sasaki M, Toyota T. Development of diabetes in the non-obese NIDDM rat (GK rat). Adv Exp Med Biol. 1988;246:29–31.
Elizondo RA, Yin ZH, Lu XW, Watsky MA. Effect of vitamin D receptor knockout on cornea epithelium wound healing and tight junctions. Invest Ophth Vis Sci. 2014;55:5245–51.
Yi X, Wang Y, Yu FSX. Corneal epithelial tight junctions and their response to lipopolysaccharide challenge. Invest Ophth Vis Sci. 2000;41:4093–100.
Cho YE, Song BJ. Pomegranate prevents binge alcohol-induced gut leakiness and hepatic inflammation by suppressing oxidative and nitrative stress. Redox Biol. 2018;18:266–78.
Lu L, Wang M, Wei X, Li W. 20-HETE inhibition by HET0016 decreases the blood-brain barrier permeability and brain edema after traumatic brain injury. Front Aging Neurosci. 2018;10:207.
Zhang S, An Q, Wang T, Gao S, Zhou G. Autophagy- and MMP-2/9-mediated reduction and redistribution of ZO-1 contribute to hyperglycemia-increased blood-brain barrier permeability during early reperfusion in stroke. Neuroscience. 2018;377:126–37.
Ko JA, Sotani Y, Ibrahim DG, Kiuchi Y. Role of macrophage migration inhibitory factor (MIF) in the effects of oxidative stress on human retinal pigment epithelial cells. Cell Biochem Funct. 2017;35:426–32.
Forbes JM, Cooper ME. Mechanisms of diabetic complications. Physiol Rev. 2013;93:137–88.
Gorin Y, Block K. Nox as a target for diabetic complications. Clin Sci. 2013;125:361–82.
Anderson EJ, Kypson AP, Rodriguez E, Anderson CA, Lehr EJ, Neufer PD. Substrate-specific derangements in mitochondrial metabolism and redox balance in the atrium of the type 2 diabetic human heart. J Am Coll Cardiol. 2009;54:1891–8.
Song BB, Scheuner D, Ron D, Pennathur S, Kaufman RJ. Chop deletion reduces oxidative stress, improves beta cell function, and promotes cell survival in multiple mouse models of diabetes. J Clin Invest. 2008;118:3378–89.
Bhatt MP, Lim YC, Hwang J, Na S, Kim YM, Ha KS. C-peptide prevents hyperglycemia-induced endothelial apoptosis through inhibition of reactive oxygen species-mediated transglutaminase 2 activation. Diabetes. 2013;62:243–53.
Uruno A, Furusawa Y, Yagishita Y, Fukutomi T, Muramatsu H, Negishi T, et al. The Keap1-Nrf2 system prevents onset of diabetes mellitus. Mol Cell Biol. 2013;33:2996–3010.
Kim J, Kim CS, Kim H, Jeong IH, Sohn E, Kim JS. Protection against advanced glycation end products and oxidative stress during the development of diabetic keratopathy by KIOM-79. J Pharm Pharmacol. 2011;63:524–30.
Couture C, Desjardins P, Zaniolo K, Germain L, Guerin SL. Enhanced wound healing of tissue-engineered human corneas through altered phosphorylation of the CREB and AKT signal transduction pathways. Acta Biomater. 2018;73:312–25.
Yang LL, Di GH, Qi X, Qu ML, Wang Y, Duan HY, et al. Substance P promotes diabetic corneal epithelial wound healing through molecular mechanisms mediated via the neurokinin-1 receptor. Diabetes. 2014;63:4262–74.
Xu KP, Yu FSX. Impaired epithelial wound healing and EGFR signaling pathways in the corneas of diabetic rats. Invest Ophth Vis Sci. 2011;52:3301–8.
Wang S, Zhu X, Xiong L, Ren J. Ablation of Akt2 prevents paraquat-induced myocardial mitochondrial injury and contractile dysfunction: role of Nrf2. Toxicol Lett. 2017;269:1–14.
Priyadarsini S, Rowsey TG, Ma JX, Karamichos D. Unravelling the stromal-nerve interactions in the human diabetic cornea. Exp Eye Res. 2017;164:22–30.
Acknowledgements
This work was supported by grants from the National Institutes of Health (NIH) to HZ (AR067766 and HL124122) and a fellowship from the China Scholarship Council (CSC no. 201706780018) to QJ.
Author contributions
JH, ZS, JM, YL, HC and HZ designed research and provided valuable inputs during the progress of the project; QJ, DK, JF, CL, BG, TT and HC performed research; QJ, YL, HC and HZ analyzed data; QJ, HC and HZ wrote the paper.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Jiang, Qw., Kaili, D., Freeman, J. et al. Diabetes inhibits corneal epithelial cell migration and tight junction formation in mice and human via increasing ROS and impairing Akt signaling. Acta Pharmacol Sin 40, 1205–1211 (2019). https://doi.org/10.1038/s41401-019-0223-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-019-0223-y
Keywords
This article is cited by
-
Top Five Stories of the Cellular Landscape and Therapies of Atherosclerosis: Current Knowledge and Future Perspectives
Current Medical Science (2024)
-
Rutin alleviates colon lesions and regulates gut microbiota in diabetic mice
Scientific Reports (2023)