Abstract
Environmental factors are involved in the etiology of autism spectrum disorder (ASD) and may contribute to the raise in its incidence rate. It is currently unknown whether the increasing use of nanoparticles such as titanium dioxide (TiO2 NPs) in consumer products and biomedical applications may play a role in these associations. While nano-sized TiO2 is generally regarded as safe and non-toxic, excessive exposure to TiO2 NPs may be associated with negative health consequences especially when occurring during sensitive developmental periods. To test if prenatal exposure to TiO2 NPs alters fetal development and behavioral functions relevant to ASD, C57Bl6/N dams were subjected to a single intravenous injection of a low (100 µg) or high (1000 µg) dose of TiO2 NPs or vehicle solution on gestation day 9. ASD-related behavioral functions were assessed in the offspring using paradigms that index murine versions of ASD symptoms. Maternal exposure to TiO2 NPs led to subtle and dose-dependent impairments in neonatal vocal communication and juvenile sociability, as well as a dose-dependent increase in prepulse inhibition of the acoustic startle reflex of both sexes. These behavioral alterations emerged in the absence of pregnancy complications. Prenatal exposure to TiO2 NPs did not cause overt fetal malformations or changes in pregnancy outcomes, nor did it affect postnatal growth of the offspring. Taken together, our study provides a first set of preliminary data suggesting that prenatal exposure to nano-sized TiO2 can induce behavioral deficits relevant to ASD and related neurodevelopmental disorders without inducing major changes in physiological development. If extended further, our preclinical findings may provide an incentive for epidemiological studies examining the role of prenatal TiO2 NPs exposure in the etiology of ASD and other neurodevelopmental disorders.
Similar content being viewed by others
Introduction
Autism spectrum disorder (ASD) is a group of neurodevelopmental disorders with increasing incidence rates. According to the Center for Disease Control and Prevention, the prevalence of ASD has doubled within the last decade1, with current estimates suggesting that 1 in 68 American children is diagnosed with ASD1. Whilst increased awareness, reclassification, diagnostic expansion, and inclusion of milder neurodevelopmental deficits likely contribute to the marked increase in the rate of diagnosed ASD2, changes in the environment may add to this increase as well3,4. The latter hypothesis is supported by recent studies suggesting that 40–50% of variance in ASD liability may be determined by environmental risk factors5,6.
In accordance with the developmental origin of ASD, most of the identified environmental risk factors act during pre- or perinatal periods. Examples of pre- or perinatal risk factors include maternal exposure to infection and/or inflammation7,8,9,10, maternal allergic-asthma11,12, maternal autoantibodies reacting with fetal proteins13,14, obstetric complications such as maternal hypertension and preeclampsia15,16, and pre- and/or perinatal exposure to (traffic-related) air pollution17,18. The latter is of particular interest as it may be related to, or even driven by, the continuing urbanization, which in itself is considered an environmental risk factor of ASD19. In addition to air pollution, early-life exposure to various other environmental toxicants, including mercury, lead, arsenic, polychlorinated biphenyls and toluene, are known causes of neurodevelopmental disorders and may play a role in the etiology of ASD20.
The increasing use of nanoparticles (NPs) in various consumer products and biomedical applications may represent another challenge for public health21,22. NPs are particles with at least one dimension below 100 nm and can be engineered with distinctive compositions, sizes, shapes, and surface chemistries23. Among the most frequently produced and used NPs are those that are based on titanium dioxide (TiO2)24,25. Their unique physicochemical and optical properties enable the application of TiO2 NPs as additives in various consumer products, including toothpaste, sunscreen, paints, and food (E171)24,26. In 2005 the worldwide production of titanium powder was approximately 5 million tons27. According to recent estimations, the proportion of nano-sized TiO2 in titanium powder increased from 2.5% in 2009 to 10% in 201527,28.
Nano-sized particles such as TiO2 NPs can either penetrate intact cell membranes29 or can be taken up via endocytosis to cross biological barriers30,31. Hence, even if the majority of TiO2 NPs may be excreted rapidly upon uptake, a certain amount of nano-sized TiO2 particles can be absorbed and disseminated into various tissues by the systemic circulation26,32,33. While TiO2 NPs are generally regarded as safe and non-toxic, a number of studies have raised possible health concerns in relation to the increasing use of nano-sized TiO2 particles26,34,35. Exposure to TiO2 NPs may be associated with negative health consequences especially when occurring during developmental periods. For example, studies in mice have found that TiO2 NPs can cross the placental–fetal barrier and induce moderate to severe malformations of the developing fetuses36,37. Prenatal exposure to TiO2 NPs in mice was further shown to alter gene expression profiles in the developing brain38 and to change cortical neurotransmitter levels in adolescent offspring39. Moreover, recent studies suggest that prenatal TiO2 NP exposure can induce long-term behavioral deficits relevant to depression40 and cognitive impairments in rats41,42.
In keeping with the increasing use of TiO2 NPs and the rise in the incidence rates of ASD, we sought to evaluate whether prenatal exposure to nano-sized TiO2 may alter brain and behavioral development in a manner that is relevant to ASD. To this end, we exposed pregnant mice to distinct doses of TiO2 NPs or control treatment and explored ASD-related behavioral functions in the resulting offspring. The behavioral tests included paradigms assessing murine versions of core symptoms of ASD, including impairments in social interaction, deficits in verbal communication, and presence of stereotyped/repetitive behaviors43. We also included tests for anxiety-like behavior and prepulse inhibition in attempts to examine ASD-related symptoms of anxiety and altered sensorimotor gating44,45. To assess the distribution of TiO2 NPs following maternal exposure, we measured the contents of titanium (Ti) in distinct maternal tissues (liver, spleen, plasma), placenta, fetal liver, and fetal brain. All investigations were conducted in male and female offspring in order to reveal potential sex-dependent effects.
Material and methods
Animals
C57Bl6/N mice were used throughout this study (Supplementary Information). All procedures involving animal experimentation had been previously approved by the Cantonal Veterinarian’s Office of Zurich, and all efforts were made to minimize the number of animals used and their suffering.
TiO2 NP suspension
TiO2 anatase NPs (NM-101) were provided by the Joint Research Center (JRC, Ispra, Italy). The TiO2 NP powder was dissolved in sterile and pyrogen-free phosphate-buffered saline (PBS) (D8537, Sigma-Aldrich, Switzerland) (5 mg/mL) via probe sonication (5 min at 13 W, on ice; Branson sonifier 250, Branson Ultrasonic Co., Danbury, CT, USA). Detailed information about the characterization of TiO2 NP suspension is provided in the Supplementary Information.
Prenatal TiO2 NP exposure
C57BL6/N female mice were subjected to a timed mating procedure as described previously46. Pregnant dams were subjected to a single intravenous injection of the 100 µg or 1000 µg TiO2 NP solution (see above) or vehicle solution (PBS) on gestation day 9 (GD) 9 (Supplementary Information). Two cohorts of pregnant mice were generated under identical experimental and housing conditions (see Supplementary Information). The first cohort of dams was designated to fetal developmental and Ti tissue distribution studies and the second cohort was used to generate offspring for behavioral studies (see Supplementary Information).
The methods used for maternal and fetal tissue collection for ICP-MS and evaluation of fetal development are described in the Supplementary Information.
Behavioral testing in the offspring
Male and female offspring were behaviorally tested in paradigms that indexed murine versions of ASD symptoms, including deficits in verbal communication, impairments in social interaction, and presence of stereotyped/repetitive behaviors43. Behavioral assessing also included tests for anxiety-like behavior and prepulse inhibition in attempts to examine ASD-related symptoms of anxiety and altered sensorimotor gating44,45. While verbal communication was assessed in neonatal mice on postnatal day (PND) 6, all other tests were conducted in a separate subgroup of offspring when they reached the juvenile stage (i.e., between PND 28 and 42). Juvenile offspring were repeatedly tested in the following order, with a testing-free resting period of 2 days between individual tests: (1) open field test, (2) social interaction test, (3) self-grooming test, and (4) prepulse inhibition (PPI) test. A detailed description of the test apparatuses and procedures is provided in the Supplementary Information.
Statistical analyses
All data met the assumptions of normal distribution and equality of variance. All data were analyzed using parametric analysis of variance (ANOVA) as described in the Supplementary Information. Whenever appropriate, all ANOVAs were followed by Fisher’s least significant difference (LSD) post-hoc tests. All statistical analyses were performed using StatView (version 5.0; Abacus, Phoenix, AZ, USA) implemented on a PC running the Windows XP operating system, and Prism software (version 7.0; GraphPad Software, La Jolla, CA, USA). Statistical significance was set at p < 0.05 for all tests. No exclusion criteria were applied.
Results
Tissue distribution of TiO2 NPs
Well-characterized anatase TiO2 NPs from the JRC repository (NM-101) were used for this study (see Supplementary Table 2). Ultrasensitive sector field-inductively coupled plasma mass spectrometry revealed that maternal TiO2 NP treatment led to a dose- and tissue-dependent accumulation of Ti, as supported by the significant main effect of prenatal treatment (F(2, 72) = 110.5, p < 0.001), tissue compartment (F(5, 72) = 62.36, p < 0.001), and their interaction (F(10,72) = 44.6, p < 0.001). As illustrated in Supplementary Fig. 1, Ti was found to accumulate in maternal liver and spleen. Post-hoc comparisons of maternal liver and spleen samples confirmed a dose-dependent increase in Ti between control animals (0 µg) and animals exposed to 100 µg (liver: p < 0.001, spleen: p < 0.001) or 1000 µg (liver: p < 0.001, spleen: p < 0.001), and between animals exposed to 100 µg and 1000 µg (liver: p < 0.001, spleen: p < 0.001). On the other hand, there was no significant accumulation of Ti in maternal plasma, placenta, fetal liver, and fetal brain (Supplementary Fig. 1).
Effects of maternal TiO2 NP exposure on pregnancy outcomes and offspring development
Maternal exposure to TiO2 NPs did not affect fetal length (F(2,21) = 0.129, p = 0.879), fetal weights (F(2,21) = 0.845, p = 0.444), and fetal brain weights (F(2,21) = 0.036, p = 0.964) (Supplementary Fig. 2b). Likewise, a gross examination of the fetal morphology did not reveal noticeable differences between fetuses of control dams and dams exposed to TiO2 NPs (Supplementary Fig. 2a). Hence, maternal exposure to TiO2 NPs did not cause overt signs of fetal malformations.
In agreement with these findings, maternal exposure to TiO2 NPs did not affect litter sizes (F(2,22) = 0.270, p = 0.766; Supplementary Fig. 2c) or the male/female ratio of the delivered pups (F(2,22) = 1.63, p = 0.23; Supplementary Fig. 2d). The offspring’s body weights were also not changed by the prenatal manipulation. As expected, the offspring’s body weights increased from neonatal (PND 6) to juvenile (PND 21 and 28) ages (main effect of age: F(2,149) = 2430.884, p < 0.001; Supplementary Fig 2e), and this age effect was not influenced by prenatal treatment (main effect of prenatal treatment: F(2,149) = 0.046, p = 0.955; interaction between prenatal treatment and age: F(4,149) = 0.394, p = 0.813). Female offspring generally weighed less than male offspring (main effect of sex: F(1,149) = 65.507, p < 0.001), regardless of their prenatal treatment conditions (interaction between prenatal treatment and sex: F(2,149) = 1.093, p = 0.338). Together, these findings indicate that maternal exposure to TiO2 NPs did not affect pregnancy outcomes or postnatal development of the offspring.
Effects of maternal TiO2 NP exposure on neonatal ultrasonic vocalization
Verbal communication was assessed in neonatal mice by measuring USV calls upon acute separation from their littermates and rearing mothers. Prenatal TiO2 NP exposure led to a dose-dependent decrease in the total numbers of USV calls emitted from pups that were separated from their mothers (main effect of prenatal treatment: F(2,43) = 5.361, p < 0.01) (Fig. 1b). Post-hoc analyses confirmed significantly decreased USV calls in neonates of mothers that were treated with 1000 µg TiO2 NPs relative to control neonates (p < 0.01) or to neonates of mothers that were treated with 100 µg TiO2 NPs (p < 0.05) (Fig. 1b). These effects were sex-independent (main effect of sex: F(1,43) = 1.703, p = 0.199; interaction between prenatal treatment and sex: F(2,43) = 0.028, p = 0.973). In contrast to its effects on the number of USVs, prenatal TiO2 NP exposure did not affect the mean duration of USV calls (main effect of prenatal treatment: F(2,43) = 1.187, p = 1.187; interaction between prenatal treatment and sex: F(2,43) = 0.035, p = 0.966) (Fig. 1c). There were also no group differences in terms of the mean dominant frequency of emitted USV calls (main effect of prenatal treatment: F(2,43) = 2.534, p = 0.091; interaction between prenatal treatment and sex: F(2,43) = 1.437, p = 0.249) (Fig. 1d).
a Representative spectrograms of USVs emitted from separated pups. b The bar plot represents the number of emitted USV calls. *p < 0.05 and ***p < 0.001. c The bar plot depicts the mean duration (ms) of emitted USV calls. d The bar plot depicts the mean dominant frequency of emitted USV calls in kHz. All data are based on N(0 µg) = 16 (8m, 8f), N(100 µg) = 16 (8m, 8f) and N(1000 µg) = 17 (9m, 8f). All values are means ± SEM
Effects of maternal TiO2 NP exposure on sociability and repetitive behavior
Sociability of juvenile offspring was assessed using a modified version of the three-chamber social interaction test46,47. In this test, sociability was indexed as the relative exploration time between an unfamiliar, congenic mouse of the same sex and an inanimate dummy object. Prenatal TiO2 NP exposure caused a dose-dependent deficit in social approach behavior (Fig. 2a), as supported by the main effect of prenatal treatment (F(2,53) = 4.838, p < 0.05) and by the subsequent post-hoc analyses revealing a significant difference between offspring of mothers that were treated with 1000 µg TiO2 NPs and control offspring (p < 0.05) or offspring of mothers that were treated with 100 µg TiO2 NPs (p < 0.05). The effect of prenatal TiO2 NP exposure on sociability emerged independently of sex (main effect of sex: F(1,53) = 0.959, p = 0.332; interaction between prenatal treatment and sex: F(2,53) = 0.091, p = 0.914) and was not associated with concomitant changes in locomotor activity (Fig. 2a). The latter was indexed by the total distance moved during the social interaction test, which did not yield any significant effects (main effect of prenatal treatment: F(2,53) = 0.771, p = 0.468; main effect of sex: F(1,53) = 2.740, p = 0.104; interaction between prenatal treatment and sex: F(2,53) = 0.247, p = 0.782).
a The bar plots depict the percent time spent with an unfamiliar mouse and the total distance moved during the social interaction test. *p < 0.05. b The bar plot depicts the time spent self-grooming during a period of 10 min. All data are based on N(0 µg) = 20 (10m, 10f), N(100 µg) = 19 (10m, 9f), N(1000 µg) = 20 (10m, 10f). All values are means ± SEM
A self-grooming test was used to explore repetitive behavior in juvenile offspring. As illustrated in Fig. 2b, offspring of mothers that were treated with TiO2 NPs showed a trend towards increased levels of self-grooming relative to control offspring (main effect of prenatal treatment: F(2,53) = 2.668, p = 0.079). The main effect of sex (F(1,53) = 0.924, p = 0.341) and its interaction with prenatal treatment (F(2,53) = 0.772, p = 0.462) were far from being significant.
Effects of maternal TiO2 NP exposure on sensorimotor gating
Sensorimotor gating was assessed in juvenile offspring using PPI of the acoustic startle reflex. Prenatal TiO2 NP exposure significantly altered % PPI, as indicated by the main effect of prenatal treatment (F(2,53) = 4.469, p < 0.05). Post-hoc analyses revealed that offspring prenatally exposed to 1000 µg TiO2 NPs displayed significantly increased % PPI relative to offspring exposed to 100 µg TiO2 NPs (p < 0.01) and control offspring (p < 0.05) (Fig. 3a). The effect of prenatal TiO2 NP exposure on % PPI was independent of sex (main effect of sex: F(1,53) = 1.710, p = 0.197; interaction with prenatal treatment and sex: F(2,53) = 0.260, p = 0.772). The increase in % PPI displayed in offspring of mothers that were exposed to 1000 µg TiO2 NPs appeared to be largest in conditions, in which 100 dBA stimuli served as pulse stimuli (Fig. 3a); however, the interaction between prenatal treatment and pulse stimulus was not significant (F(4,106) = 2.187, p = 0.085). The interaction between prenatal treatment and prepulse was far from being significant (F(4,106) = 0.209, p = 0.933), indicating that the effect of prenatal TiO2 NP exposure on % PPI emerged independently of prepulse intensity.
a The line plot depicts percent prepulse inhibition as a function of different pulse intensities (P-100, P-110 and P-120, corresponding to 110, 110, and 120 dBA) and prepulse intensities (+6, +12, and +18 dBA above background of 65 dBA). The bar plot shows the mean prepulse inhibition scores across all pulse and prepulse conditions. *p < 0.05. b The line plot depicts the startle response to pulse-alone stimuli as a function of pulse intensities (110, 110, and 120 dBA). c The line plot depicts the reactivity to prepulse-alone stimuli as a function of prepulse intensities (71, 77, and 83 dBA). All data are based on N(0 µg) = 20 (10m, 10f), N(100 µg) = 19 (10m, 9f), N(1000 µg) = 20 (10m, 10f). All values are means ± SEM
Prenatal TiO2 NP exposure did not affect the reactivity to pulse-alone trials (F(2,53) = 0.161, p = 0.852); (Fig. 3b) or prepulse-alone trials (F(2,53) = 0.477, p = 0.623); (Fig. 3c). As expected47, the reactivity to pulse-alone and prepulse-alone trials increased with increasing pulse and prepulse intensities, respectively (main effect of pulse: F(2,106) = 378.790, p < 0.001; main effect of prepulse: F(2,106) = 17.886, p < 0.001).
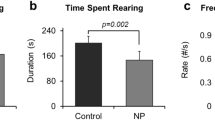
Effects of maternal TiO2 NP exposure on anxiety-like behavior
Innate anxiety-like behavior was assessed in juvenile offspring using the open-field exploration task. As illustrated in Fig. 4a, prenatal TiO2 NP exposure did not affect the time spent in the center zone of the open field during 10 min of free exploration (main effect of prenatal treatment: F(2,53) = 0.773, p = 0.467; main effect of sex: F(1,53) = 1.167, p = 0.285; interaction between prenatal treatment and sex: F(2,53) = 0.349, p = 0.707). Likewise, the prenatal manipulation did not influence general locomotor activity indexed by the total distance moved (main effect of prenatal treatment: F(2,53) = 2.800, p = 0.070) (Fig. 4b). As expected48, the total distance moved was generally higher in female as compared to male offspring (main effect of sex: F(1,53) = 13.76, p < 0.001), and this effect similarly emerged in all prenatal treatment groups (interaction between prenatal treatment and sex: F(2,53) = 1.976, p = 0.149).
Innate anxiety-like behavior was assessed using a 10 min open field test. a The bar plot represents the time spent in the center zone of the open field arena. b The bar plot depicts the total distance moved in the entire arena. All data are based on N(0 µg) = 20 (10m, 10f), N(100 µg) = 19 (10m, 9f), and N(1000 µg) = 20 (10m, 10f). All values are means ± SEM
Discussion
The present study demonstrates that maternal exposure to nano-sized TiO2 leads to a dose-dependent disruption of behavioral functions in mice. The spectrum of behavioral deficits induced by prenatal TiO2 NP exposure included impairments in neonatal vocal communication and juvenile social interaction, as well as increased PPI of the acoustic startle reflex in juvenile offspring. The neonatal deficits in vocal communication were manifest as a reduction in USV rates when pups were separated from their littermates and rearing mother and thus likely reflect altered affective states promoting separation-induced vocal responses. The dose-dependent deficit in social approach behavior induced by prenatal TiO2 NP exposure was not associated with concomitant alterations in innate anxiety-like behavior, and therefore, it likely represents a genuine impairment in sociability towards unfamiliar conspecifics. Finally, the observed increase in PPI of the acoustic startle reflex may reflect hypersensitivity to sensory information. The consensus is that PPI reflects the ability to filter out irrelevant information in the early stages of processing so that attention can be directed to more salient environmental features49. Generally, stronger and/or more salient prepulses induce higher levels of PPI as they are more efficient in inhibiting the processing of the subsequent pulse stimulus. On speculative grounds, prepulses may be more salient for offspring that were prenatally exposed to the highest dose of TiO2 as compared to control offspring, and consequently, they would be more efficacious in inhibiting the subsequent pulse-stimulus processing in TiO2-exposed offspring, thereby leading to increased PPI.
Interestingly, the TiO2-induced disruption of behavioral functions was independent of the offspring’s sex, indicating similar vulnerabilities of the male and female sex to this environmental hazard. Prenatal exposure to nano-sized TiO2 did also not cause overt fetal malformations or changes in pregnancy outcomes, nor did it affect postnatal growth of the offspring. Taken together, our mouse model suggests that prenatal TiO2 exposure can induce behavioral abnormalities in both sexes without inducing major changes in physiological development.
Relevance to autism spectrum disorder and beyond
A number of behavioral alterations emerging in offspring that were prenatally exposed to the highest dose of nano-sized TiO2, including impairments in vocal communication and social interaction, resemble core features of ASD50. These core deficits often emerge as early as in the first years of life and tend to persist throughout life in ASD subjects51,52. It should be noted, however, that our study does not offer a direct link between these two behavioral impairments, given that vocal communication was measured in neonatal offspring, whereas social interaction was assessed at the juvenile stage of life. In addition to vocal and social deficits, the TiO2-induced changes in PPI may also have some relevance for ASD. While PPI was found to be decreased in a subset of adults with ASD53,54, increased PPI of the acoustic startle reflex has been reported for children with ASD55. Our findings recapitulate the latter, given that our study examined PPI in juvenile offspring of TiO2-exposed mothers and controls. Increased PPI in children with ASD has been related to hypersensitivity to sensory information, which may stem from changes in the perceived salience of seemingly irrelevant stimuli such as prepulses of low intensity.
Despite the fact that prenatal TiO2 exposure resulted in ASD-related behavioral deficits, it should be noted that these deficits were relatively subtle and did not extend to other core behavioral abnormalities that are frequently observed in ASD, including repetitive and anxiety-like behaviors43. Furthermore, our findings do by no means imply that prenatal TiO2 exposure may cause behavioral abnormalities that are specific to ASD. In fact, this environmental hazard may also contribute to other brain disorders, including depression-like behavior and cognitive deficits. For example, a previous study in rats showed that prenatal exposure to TiO2 caused anhedonic behavior and behavioral despair, as assessed using the sucrose preference test and forced swimming test, respectively40. Furthermore, maternal administration of TiO2 in rats was found to impair various cognitive functions, including spatial and non-spatial learning and memory41,42. Since our study did not assess functions in these behavioral and cognitive domains, we cannot directly compare our data to these previous findings. Taken together, however, the available data suggest that prenatal exposure to TiO2 may be a general vulnerability factor for various brain disorders with neurodevelopmental etiologies.
Tissue distribution of TiO2 NPs and possible mediating mechanisms
In line with previous systemic exposure studies in rodents33,56,57, we found that Ti accumulated primarily in the maternal liver and spleen after i.v. administration of TiO2 NPs. By contrast, we did not detect increased Ti levels in the placenta or in fetal brain and liver tissues, suggesting that the majority of the maternally administered TiO2 particles did not accumulate in or cross the maternal-fetal interface. Therefore, it seems unlikely that a direct fetal exposure to TiO2 NPs is responsible for the subsequent emergence of behavioral abnormalities. Rather, the effects of prenatal TiO2 exposure may be driven by pathophysiological processes that arise in the maternal system and induce secondary effects in the offspring.
At present, the nature of these pathophysiological processes remains elusive and warrants identification in future studies. One candidate mechanism may involve alterations in the maternal immune system. In support of this hypothesis, it was previously shown that exposure to TiO2 NPs can induce signs of inflammation and other immune abnormalities, both in vivo and in vitro58,59,60. Given that abnormal immune functions and maternal inflammation have themselves been implicated in the etiology of ASD7,8,9,10,11,12,13,14, a link between prenatal exposure to TiO2, immune abnormalities, and emergence of ASD-related deficits seems biologically plausible. This hypothesis also warrants further exploration in view of the parallels between our findings and those reported in animal models of prenatal inflammation and other immune abnormalities. Indeed, prenatal exposure to immune challenges such as viral- or bacterial-like acute phase responses7,61,62,63 or allergy-like immune imbalances11,64 have been shown to induce similar ASD-related behavioral abnormalities as those reported here.
An alternative (but mutually not exclusive) possibility is that maternal TiO2 exposure could cause abnormal development and functions of the placenta even in the absence of placental accumulation of TiO2 NPs. The role of placental abnormalities in the etiology of ASD has received increasing recognition in recent years15,65. Being the critical sustenance delivery system for the fetus, placental health is critical for fetal growth and development66. Importantly, acting as the interface to communicate maternal nutritional and environmental statuses, the placenta rapidly responds to alterations in the maternal milieu and integrates the pathophysiological effects induced by a number of environmental adversities66. While various NPs have been associated with reproductive toxicity67, recent evidence suggests that this may also be the case for TiO2 NPs. For example, it was recently shown in mice that maternal exposure to TiO2 starting from conception to late gestation affected placental micronutrients and reduced placental weights68. Hence, the disruption of placental development and function may represent another possible mechanism by which maternal exposure to nano-sized TiO2 can induce ASD-relevant behavioral abnormalities in the offspring.
A third possible mechanism underlying the disruption of behavioral development following prenatal TiO2 exposure may involve changes in the maternal microbiota69. This hypothesis warrants exploration in view of the accumulating evidence suggesting that dysbiosis of the maternal microbiome can induce altered brain and behavioral development in the offspring with relevance to ASD and beyond70. In fact, alterations in the maternal microbiome may represent a common pathophysiological mechanism mediating the negative effects of a number of prenatal adversities, including maternal exposure to stress71, immune activation72, and high-fat diets73.
Extrapolation to human exposures
The continuous rise in TiO2-containing products increases the human exposure to nano-sized TiO2. For example, the dietary intake of TiO2 in the US is estimated to be 1–2 mg/kg body weight per day for children, and 0.2–0.7 mg/kg body weight per day for other age groups24,26. Food-grade TiO2 particles are frequently used as white colorant and typically have a mean size of >100 nm, thus exceeding nano-size scales24. Nevertheless, approximately up to one third of TiO2 particles in common food products are nano-sized (<100 nm)24,26, suggesting that the daily ingestion of TiO2 NPs via common food products is considerable. According to recent bioavailability studies in humans, however, only a small proportion (~0.1%) of the ingested TiO2 NPs reaches the systemic circulation74. The low bioavailability of orally administered TiO2 NPs contrast the bioavailability of TiO2 NPs in our study, which was 100% as a result of the i.v. administration regimen. Given these differences in bioavailability, one could argue that our findings are artificial, and therefore, irrelevant for human conditions, where most of the TiO2 NPs reach the body via the oral route or inhalation26,34,35,75. While we appreciate the limitations of the chosen experimental design, we deem our study relevant for various reasons. First, given that TiO2 NPs can persist in tissues such as liver and spleen once absorbed33, it is likely that even limited systemic absorption can result in tissue accumulation, especially upon chronic exposure26,33. Secondly, our study emphasizes that a single exposure to high doses of TiO2 NPs in prenatal life is sufficient to induce long-term behavioral changes. Nano-sized TiO2 has been in discussion for the future use in biomedical applications, whereby the particles would serve as drug carriers and administered via the i.v. route35,76. Thus, together with other preclinical studies that were based on prenatal i.v. exposure to TiO2 NPs33,37,56,57,77, our findings emphasize the need of a careful assessment of the possible benefits and risks of administering nano-sized TiO2 to pregnant women.
Limitations
Our study has a number of limitations. First, it did not aim at identifying the post-acute mechanisms mediating the effects of maternal TiO2 exposure on behavioral development in the offspring. Second, the characterization of the negative effects of prenatal TiO2 exposure was conducted exclusively at the behavioral level and did not encompass investigations of brain specimen. Hence, our study did not provide a link between TiO2-induced behavioral alterations and dysfunctions in specific neuronal and/or glial systems. Finally, even if we included a number of behavioral tests, the behavioral characterization of the effects of prenatal TiO2 exposure was far from exhaustive and did, for example, not involve the assessment of cognitive functions. With respect to the latter, future studies should also investigate whether this environmental hazard affects cognitive flexibility and working memory, both of which are altered in a subset of cases with ASD and related neurodevelopmental disorders78,79.
Conclusion
Our study provides a first set of preliminary data suggesting that prenatal exposure to nano-sized TiO2 can induce behavioral deficits relevant to ASD and related neurodevelopmental disorders. Human epidemiological studies exploring associations between TiO2 exposure and health outcomes are still rare and largely confined to the research of cancer and pulmonary diseases80,81,82. Hence, our findings cannot be compared directly to human epidemiological data collected in the context of ASD, nor should they be taken to predict ASD risk in human populations. At the same time, however, our findings may provide an incentive for epidemiologists and basic scientists alike to further examine the role of prenatal TiO2 exposure in the etiology of ASD and other neurodevelopmental disorders. Such studies may also help to ascertain whether the increasing use of NPs such as nano-sized TiO2 contributes in some way to the rise in the incidence rates of these disorders.
References
Baio, J. et al. Prevalence of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2014. Morb. Mortal. Wkly. Report. Surveill. Summ. 67, 1–23 (2018).
Hansen, S. N., Schendel, D. E. & Parner, E. T. Explaining the increase in the prevalence of autism spectrum disorders: the proportion attributable to changes in reporting practices. JAMA Pediatr. 169, 56–62 (2015).
Modabbernia, A., Velthorst, E. & Reichenberg, A. Environmental risk factors for autism: an evidence-based review of systematic reviews and meta-analyses. Mol. Autism 8, 13 (2017).
Ye, B. S., Leung, A. O. W. & Wong, M. H. The association of environmental toxicants and autism spectrum disorders in children. Environ. Pollut. 227, 234–242 (2017).
Gaugler, T. et al. Most genetic risk for autism resides with common variation. Nat. Genet. 46, 881–885 (2014).
Hallmayer, J. et al. Genetic heritability and shared environmental factors among twin pairs with autism. Arch. General. Psychiatry 68, 1095–1102 (2011).
Vuillermot, S., Luan, W., Meyer, U. & Eyles, D. Vitamin D treatment during pregnancy prevents autism-related phenotypes in a mouse model of maternal immune activation. Mol. Autism 8, 9 (2017).
Brown, A. S. et al. Elevated maternal C-reactive protein and autism in a national birth cohort. Mol. Psychiatry 19, 259–264 (2014).
Jones, K. L. et al. Autism with intellectual disability is associated with increased levels of maternal cytokines and chemokines during gestation. Mol. Psychiatry 22, 273–279 (2017).
Jiang, H. Y. et al. Maternal infection during pregnancy and risk of autism spectrum disorders: a systematic review and meta-analysis. Brain Behav. Immun. 58, 165–172 (2016).
Schwartzer, J. J., Careaga, M., Chang, C., Onore, C. E. & Ashwood, P. Allergic fetal priming leads to developmental, behavioral and neurobiological changes in mice. Transl. Psychiatry 5, e543 (2015).
Patel S., et al. Social impairments in autism spectrum disorder are related to maternal immune history profile. Mol. Psychiatry (2017). [Epub ahead of print]
Edmiston, E., Ashwood, P., Van & de Water, J. Autoimmunity, autoantibodies, and autism spectrum disorder. Biol. Psychiatry 81, 383–390 (2017).
Braunschweig, D., Van & de Water, J. Maternal autoantibodies in autism. Arch. Neurol. 69, 693–699 (2012).
Walker, C. K. et al. Preeclampsia, placental insufficiency, and autism spectrum disorder or developmental delay. JAMA Pediatr. 169, 154–162 (2015).
Polo-Kantola, P. et al. Obstetric risk factors and autism spectrum disorders in Finland. J. Pediatr. 164, 358–365 (2014).
Thirtamara Rajamani, K. et al. Prenatal and early-life exposure to high-level diesel exhaust particles leads to increased locomotor activity and repetitive behaviors in mice. Autism Res. Off. J. Int. Soc. Autism Res. 6, 248–257 (2013).
Volk, H. E., Lurmann, F., Penfold, B., Hertz-Picciotto, I. & McConnell, R. Traffic-related air pollution, particulate matter, and autism. JAMA Psychiatry 70, 71–77 (2013).
Lauritsen, M. B. et al. Urbanicity and autism spectrum disorders. J. Autism Dev. Disord. 44, 394–404 (2014).
Rossignol, D. A., Genuis, S. J. & Frye, R. E. Environmental toxicants and autism spectrum disorders: a systematic review. Transl. Psychiatry 4, e360 (2014).
Kunzmann, A. et al. Toxicology of engineered nanomaterials: focus on biocompatibility, biodistribution and biodegradation. Biochim. Et. Biophys. Acta 1810, 361–373 (2011).
Pelaz, B. et al. Diverse applications of nanomedicine. ACS Nano 11, 2313–2381 (2017).
Dahoumane, S. A., Jeffryes, C., Mechouet, M. & Agathos, S. N. Biosynthesis of inorganic nanoparticles: a fresh look at the control of shape, size and composition. Bioengineering 4, 14 (2017).
Weir, A., Westerhoff, P., Fabricius, L., Hristovski, K. & von Goetz, N. Titanium dioxide nanoparticles in food and personal care products. Environ. Sci. Technol. 46, 2242–2250 (2012).
Piccinno, F., Gottschalk, F., Seeger, S. & Nowack, B. Industrial production quantities and uses of ten engineered nanomaterials in Europe and the world. J. Nanopart. Res. 14, 1109 (2012).
Winkler, H. C., Notter, T., Meyer, U. & Naegeli, H. Critical review of the safety assessment of titanium dioxide additives in food. J. Nanobiotechnol. 16, 51 (2018).
Skocaj, M., Filipic, M., Petkovic, J. & Novak, S. Titanium dioxide in our everyday life; is it safe? Radiol. Oncol. 45, 227–247 (2011).
Robichaud, C. O., Uyar, A. E., Darby, M. R., Zucker, L. G. & Wiesner, M. R. Estimates of upper bounds and trends in nano-TiO2 production as a basis for exposure assessment. Environ. Sci. Technol. 43, 4227–4233 (2009).
Rothen-Rutishauser, B. M., Schurch, S., Haenni, B., Kapp, N. & Gehr, P. Interaction of fine particles and nanoparticles with red blood cells visualized with advanced microscopic techniques. Environ. Sci. Technol. 40, 4353–4359 (2006).
Brun, E. et al. Titanium dioxide nanoparticle impact and translocation through ex vivo, in vivo and in vitro gut epithelia. Part. Fibre Toxicol. 11, 13 (2014).
Grafmueller, S. et al. Bidirectional transfer study of polystyrene nanoparticles across the placental barrier in an ex vivo human placental perfusion model. Environ. Health Perspect. 123, 1280–1286 (2015).
Wang, J. et al. Acute toxicity and biodistribution of different sized titanium dioxide particles in mice after oral administration. Toxicol. Lett. 168, 176–185 (2007).
Geraets, L. et al. Tissue distribution and elimination after oral and intravenous administration of different titanium dioxide nanoparticles in rats. Part. Fibre Toxicol. 11, 30 (2014).
Shakeel, M. et al. Toxicity of nano-titanium dioxide (TiO2-NP) through various routes of exposure: a review. Biol. Trace Elem. Res. 172, 1–36 (2016).
Shi, H., Magaye, R., Castranova, V. & Zhao, J. Titanium dioxide nanoparticles: a review of current toxicological data. Part. Fibre Toxicol. 10, 15 (2013).
Takeda, K. et al. Nanoparticles transferred from pregnant mice to their offspring can damage the genital and cranial nerve systems. J. Health Sci. 55, 95–102 (2009).
Yamashita, K. et al. Silica and titanium dioxide nanoparticles cause pregnancy complications in mice. Nat. Nanotechnol. 6, 321–328 (2011).
Umezawa, M., Tainaka, H., Kawashima, N., Shimizu, M. & Takeda, K. Effect of fetal exposure to titanium dioxide nanoparticle on brain development—brain region information. J. Toxicol. Sci. 37, 1247–1252 (2012).
Takahashi, Y., Mizuo, K., Shinkai, Y., Oshio, S. & Takeda, K. Prenatal exposure to titanium dioxide nanoparticles increases dopamine levels in the prefrontal cortex and neostriatum of mice. J. Toxicol. Sci. 35, 749–756 (2010).
Cui, Y. et al. Prenatal exposure to nanoparticulate titanium dioxide enhances depressive-like behaviors in adult rats. Chemosphere 96, 99–104 (2014).
Mohammadipour, A. et al. Maternal exposure to titanium dioxide nanoparticles during pregnancy; impaired memory and decreased hippocampal cell proliferation in rat offspring. Environ. Toxicol. Pharmacol. 37, 617–625 (2014).
Engler-Chiurazzi, E. B. et al. Impacts of prenatal nanomaterial exposure on male adult Sprague-Dawley rat behavior and cognition. J. Toxicol. Environ. Health Part A 79, 447–452 (2016).
Pasciuto, E. et al. Autism spectrum disorders: translating human deficits into mouse behavior. Neurobiol. Learn. Mem. 124, 71–87 (2015).
South, M., Rodgers, J. & Van Hecke, A. Anxiety and ASD: current progress and ongoing challenges. J. Autism Dev. Disord. 47, 3679–3681 (2017).
Cheng, C. H., Chan, P. S., Hsu, S. C. & Liu, C. Y. Meta-analysis of sensorimotor gating in patients with autism spectrum disorders. Psychiatry Res 262, 413–419 (2017).
Notter, T. et al. Translational evaluation of translocator protein as a marker of neuroinflammation in schizophrenia. Mol. Psychiatry 23, 323–334 (2017).
Weber-Stadlbauer, U. et al. Transgenerational transmission and modification of pathological traits induced by prenatal immune activation. Mol. Psychiatry 22, 102–112 (2017).
Schwendener, S., Meyer, U. & Feldon, J. Deficient maternal care resulting from immunological stress during pregnancy is associated with a sex-dependent enhancement of conditioned fear in the offspring. J. Neurodev. Disord. 1, 15–32 (2009).
Swerdlow, N. R., Geyer, M. A. & Braff, D. L. Neural circuit regulation of prepulse inhibition of startle in the rat: current knowledge and future challenges. Psychopharmacology 156, 194–215 (2001).
Constantino, J. N. & Charman, T. Diagnosis of autism spectrum disorder: reconciling the syndrome, its diverse origins, and variation in expression. Lancet Neurol. 15, 279–291 (2016).
Landa, R. J., Holman, K. C. & Garrett-Mayer, E. Social and communication development in toddlers with early and later diagnosis of autism spectrum disorders. Arch. General. Psychiatry 64, 853–864 (2007).
Rapin, I. & Tuchman, R. F. Autism: definition, neurobiology, screening, diagnosis. Pediatr. Clin. North Am. 55, 1129–1146 (2008). viii.
Perry, W., Minassian, A., Lopez, B., Maron, L. & Lincoln, A. Sensorimotor gating deficits in adults with autism. Biol. Psychiatry 61, 482–486 (2007).
McAlonan, G. M. et al. Brain anatomy and sensorimotor gating in Asperger’s syndrome. Brain J. Neurol. 125(Pt 7), 1594–1606 (2002).
Madsen, G. F., Bilenberg, N., Cantio, C. & Oranje, B. Increased prepulse inhibition and sensitization of the startle reflex in autistic children. Autism Res. Off. J. Int. Soc. Autism Res. 7, 94–103 (2014).
Kreyling, W. G. et al. Quantitative biokinetics of titanium dioxide nanoparticles after intravenous injection in rats: part 1. Nanotoxicology 11, 434–442 (2017).
Fabian, E. et al. Tissue distribution and toxicity of intravenously administered titanium dioxide nanoparticles in rats. Arch. Toxicol. 82, 151–157 (2008).
Huang, C. et al. Titanium dioxide nanoparticles prime a specific activation state of macrophages. Nanotoxicology 11, 737–750 (2017).
Kim, B. G., Lee, P. H., Lee, S. H., Park, M. K. & Jang, A. S. Effect of TiO(2) nanoparticles on inflammasome-mediated airway inflammation and responsiveness. Allergy Asthma Immunol. Res. 9, 257–264 (2017).
Tsugita, M., Morimoto, N. & Nakayama, M. SiO2 and TiO2 nanoparticles synergistically trigger macrophage inflammatory responses. Part. Fibre Toxicol. 14, 11 (2017).
Fernandez de Cossio, L., Guzman, A., van der Veldt, S. & Luheshi, G. N. Prenatal infection leads to ASD-like behavior and altered synaptic pruning in the mouse offspring. Brain Behav. Immun. 63, 88–98 (2017).
Bauman, M. D. et al. Activation of the maternal immune system during pregnancy alters behavioral development of rhesus monkey offspring. Biol. Psychiatry 75, 332–341 (2014).
Kirsten, T. B. & Bernardi, M. M. Prenatal lipopolysaccharide induces hypothalamic dopaminergic hypoactivity and autistic-like behaviors: repetitive self-grooming and stereotypies. Behav. brain Res. 331, 25–29 (2017).
Schwartzer, J. J. et al. Behavioral impact of maternal allergic-asthma in two genetically distinct mouse strains. Brain Behav. Immun. 63, 99–107 (2017).
Hsiao, E. Y. & Patterson, P. H. Placental regulation of maternal–fetal interactions and brain development. Dev. Neurobiol. 72, 1317–1326 (2012).
Nugent, B. M. & Bale, T. L. The omniscient placenta: metabolic and epigenetic regulation of fetal programming. Front. Neuroendocrinol. 39, 28–37 (2015).
Brohi, R. D. et al. Toxicity of nanoparticles on the reproductive system in animal models: a review. Front. Pharmacol. 8, 606 (2017).
Hong, F., Zhou, Y., Zhao, X., Sheng, L. & Wang, L. Maternal exposure to nanosized titanium dioxide suppresses embryonic development in mice. Int. J. Nanomed. 12, 6197–6204 (2017).
Pietroiusti, A., Magrini, A. & Campagnolo, L. New frontiers in nanotoxicology: gut microbiota/microbiome-mediated effects of engineered nanomaterials. Toxicol. Appl. Pharmacol. 299, 90–95 (2016).
Borre, Y. E. et al. Microbiota and neurodevelopmental windows: implications for brain disorders. Trends Mol. Med. 20, 509–518 (2014).
Jasarevic E., et al. The maternal vaginal microbiome partially mediates the effects of prenatal stress on offspring gut and hypothalamus. Nature Neurosci. (2018).
Lammert, C. R. et al. Cutting edge: critical roles for microbiota-mediated regulation of the immune system in a prenatal immune activation model of autism. J. Immunol 201, 845–850 (2018).
Buffington, S. A. et al. Microbial reconstitution reverses maternal diet-induced social and synaptic deficits in offspring. Cell 165, 1762–1775 (2016).
Jones, K. et al. Human in vivo and in vitro studies on gastrointestinal absorption of titanium dioxide nanoparticles. Toxicol. Lett. 233, 95–101 (2015).
Heringa, M. B. et al. Risk assessment of titanium dioxide nanoparticles via oral exposure, including toxicokinetic considerations. Nanotoxicology 10, 1515–1525 (2016).
Zhao, J. & Castranova, V. Toxicology of nanomaterials used in nanomedicine. J. Toxicol. Environ. Health Part B Crit. Rev. 14, 593–632 (2011).
van Ravenzwaay, B. et al. Comparing fate and effects of three particles of different surface properties: nano-TiO(2), pigmentary TiO(2) and quartz. Toxicol. Lett. 186, 152–159 (2009).
Dajani, D. R. & Uddin, L. Q. Demystifying cognitive flexibility: implications for clinical and developmental neuroscience. Trends Neurosci. 38, 571–578 (2015).
Wang, Y. et al. A meta-analysis of working memory impairments in autism spectrum disorders. Neuropsychol. Rev. 27, 46–61 (2017).
Boffetta, P. et al. Exposure to titanium dioxide and risk of lung cancer in a population-based study from Montreal. Scand. J. Work Environ. Health 27, 227–232 (2001).
Boffetta, P. et al. Mortality among workers employed in the titanium dioxide production industry in Europe. CCC 15, 697–706 (2004).
Fryzek, J. P. et al. A cohort mortality study among titanium dioxide manufacturing workers in the United States. J. Occup. Environ. Med. 45, 400–409 (2003).
Acknowledgements
The research leading to these results was supported by the 2017 “Forschungskredit” granted by the University of Zurich to T.N. Further support was provided by the Swiss National Science Foundation (310030_169544) and the Foundation for Research in Science and the Humanities at the University of Zurich to U.M.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Notter, T., Aengenheister, L., Weber-Stadlbauer, U. et al. Prenatal exposure to TiO2 nanoparticles in mice causes behavioral deficits with relevance to autism spectrum disorder and beyond. Transl Psychiatry 8, 193 (2018). https://doi.org/10.1038/s41398-018-0251-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-018-0251-2
This article is cited by
-
Multigenerational inheritance of breathing deficits following perinatal exposure to titanium dioxide nanoparticles in the offspring of mice
Discover Nano (2024)
-
Chronic maternal exposure to titanium dioxide nanoparticles alters breathing in newborn offspring
Particle and Fibre Toxicology (2022)
-
Exposure to two-dimensional ultrathin Ti3C2 (MXene) nanosheets during early pregnancy impairs neurodevelopment of offspring in mice
Journal of Nanobiotechnology (2022)
-
A novel inactivated virus system (InViS) for a fast and inexpensive assessment of viral disintegration
Scientific Reports (2022)
-
Ingestion of titanium dioxide nanoparticles: a definite health risk for consumers and their progeny
Archives of Toxicology (2022)