Abstract
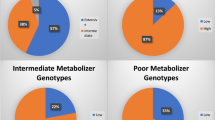
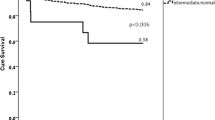
The effect of dual antiplatelet therapy, clopidogrel combined with aspirin, was influenced by CYP2C19 gene mutation and heterogeneity of population. Related studies remained controversial and limited, especially in Chinese. Total 3295 unrelated ACS Chinese patients undergoing percutaneous coronary intervention (PCI) were recruited and followed up to 1 year. Meanwhile, baseline and clinical data were retrieved. CYP2C19*2 and *3 were genotyped by sequencing. Associations of variants and metabolic types with platelet reactivity (PR) were analyzed by a logistic regression model. And, a Cox proportional hazards model was utilized to analyze survival data. Confounders included gender, age, smoking status, dosage of aspirin and clopidogrel, and BMI. It was found that patients with allele A in CYP2C19*2 and *3 were susceptibility to high PR (OR, 95%CI and P values were 1.34, 1.20–1.50, <0.0001 and 1.42, 1.13–1.79, 0.0029, respectively) after taking clopidogrel. The PR increased along with the number of loss of function (LOF) allele increased and did in order of haplotype*1, *2, and *3. This research suggested that LOF alleles and risk haplotypes in CYP2C19 could significantly attenuate the response to clopidogrel, which resulted in platelet aggregation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Fischman DL, Leon MB, Baim DS, Schatz RA, Savage MP, Penn I, et al. A randomized comparison of coronary-stent placement and balloon angioplasty in the treatment of coronary artery disease. Stent Restenosis Study Investigators. N Engl J Med. 1994;331:496–501.
Orford JL, Lennon R, Melby S, Fasseas P, Bell MR, Rihal CS, et al. Frequency and correlates of coronary stent thrombosis in the modern era: analysis of a single center registry. J Am Coll Cardiol. 2002;40:1567–72.
Mauri L, Kereiakes DJ, Yeh RW, Driscoll-Shempp P, Cutlip DE, Steg PG, et al. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med. 2014;371:2155–66.
Giustino G, Baber U, Sartori S, Mehran R, Mastoris I, Kini AS, et al. Duration of dual antiplatelet therapy after drug-eluting stent implantation: a systematic review and meta-analysis of randomized controlled trials. J Am Coll Cardiol. 2015;65:1298–310.
Frelinger AR, Bhatt DL, Lee RD, Mulford DJ, Wu J, Nudurupati S, et al. Clopidogrel pharmacokinetics and pharmacodynamics vary widely despite exclusion or control of polymorphisms (CYP2C19, ABCB1, PON1), noncompliance, diet, smoking, co-medications (including proton pump inhibitors), and pre-existent variability in platelet function. J Am Coll Cardiol. 2013;61:872–9.
Simon T, Verstuyft C, Mary-Krause M, Quteineh L, Drouet E, Meneveau N, et al. Genetic determinants of response to clopidogrel and cardiovascular events. N Engl J Med. 2009;360:363–75.
Pare G, Mehta SR, Yusuf S, Anand SS, Connolly SJ, Hirsh J, et al. Effects of CYP2C19 genotype on outcomes of clopidogrel treatment. N Engl J Med. 2010;363:1704–14.
Snoep JD, Hovens MM, Eikenboom JC, van der Bom JG, Jukema JW, Huisman MV. Clopidogrel nonresponsiveness in patients undergoing percutaneous coronary intervention with stenting: a systematic review and meta-analysis. Am Heart J. 2007;154:221–31.
Cannon CP, Brindis RG, Chaitman BR, Cohen DJ, Cross JJ, Drozda JJ, et al. 2013 ACCF/AHA key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes and coronary artery disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Acute Coronary Syndromes and Coronary Artery Disease Clinical Data Standards). Crit Pathw Cardiol. 2013;12:65–105.
Bliden KP, DiChiara J, Tantry US, Bassi AK, Chaganti SK, Gurbel PA. Increased risk in patients with high platelet aggregation receiving chronic clopidogrel therapy undergoing percutaneous coronary intervention: is the current antiplatelet therapy adequate? J Am Coll Cardiol. 2007;49:657–66.
Tantry US, Bonello L, Aradi D, Price MJ, Jeong YH, Angiolillo DJ, et al. Consensus and update on the definition of on-treatment platelet reactivity to adenosine diphosphate associated with ischemia and bleeding. J Am Coll Cardiol. 2013;62:2261–73.
Gurbel PA, Bliden KP, Navickas IA, Mahla E, Dichiara J, Suarez TA, et al. Adenosine diphosphate-induced platelet-fibrin clot strength: a new thrombelastographic indicator of long-term poststenting ischemic events. Am Heart J. 2010;160:346–54.
Li J, Wang Y, Wang H. Distribution of CYP2C19 polymorphisms in Mongolian and Han nationals and the choice of specific antiplatelet drugs. Int J Clin Pharm. 2017;39:791–7.
Sorich MJ, Rowland A, McKinnon RA, Wiese MD. CYP2C19 genotype has a greater effect on adverse cardiovascular outcomes following percutaneous coronary intervention and in Asian populations treated with clopidogrel: a meta-analysis. Circ Cardiovasc Genet. 2014;7:895–902.
Wang Y, Zhao X, Lin J, Li H, Johnston SC, Lin Y, et al. Association between CYP2C19 loss-of-function allele status and efficacy of clopidogrel for risk reduction among patients with minor stroke or transient ischemic attack. JAMA. 2016;316:70–8.
Hasan MS, Basri HB, Hin LP, Stanslas J. Genetic polymorphisms and drug interactions leading to clopidogrel resistance: why the Asian population requires special attention. Int J Neurosci. 2013;123:143–54.
Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, Brandt JT, et al. Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med. 2009;360:354–62.
Park KH, Jeong MH, Ahn Y, Ahn TH, Seung KB, Oh DJ, et al. Comparison of short-term clinical outcomes between ticagrelor versus clopidogrel in patients with acute myocardial infarction undergoing successful revascularization; from Korea Acute Myocardial Infarction Registry-National Institute of Health. Int J Cardiol. 2016;215:193–200.
Li C, Zhang L, Wang H, Li S, Zhang Y, You L, et al. Gene variants in responsiveness to clopidogrel have no impact on clinical outcomes in Chinese patients undergoing percutaneous coronary intervention—A multicenter study. Int J Cardiol. 2017;240:360–6.
Han Y, Lv HH, Liu X, Dong Q, Yang XL, Li SX, et al. Influence of genetic polymorphisms on clopidogrel response and clinical outcomes in patients with acute ischemic stroke CYP2C19 genotype on clopidogrel response. CNS Neurosci Ther. 2015;21:692–7.
Tsantes AE, Ikonomidis I, Papadakis I, Bonovas S, Gialeraki A, Kottaridi C, et al. Impact of the proton pump inhibitors and CYP2C19*2 polymorphism on platelet response to clopidogrel as assessed by four platelet function assays. Thromb Res. 2013;132:e105–11.
De Morais SM, Wilkinson GR, Blaisdell J, Nakamura K, Meyer UA, Goldstein JA. The major genetic defect responsible for the polymorphism of S-mephenytoin metabolism in humans. J Biol Chem. 1994;269:15419–22.
De Morais SM, Wilkinson GR, Blaisdell J, Meyer UA, Nakamura K, Goldstein JA. Identification of a new genetic defect responsible for the polymorphism of (S)-mephenytoin metabolism in Japanese. Mol Pharmacol. 1994;46:594–8.
Simon T, Bhatt DL, Bergougnan L, Farenc C, Pearson K, Perrin L, et al. Genetic polymorphisms and the impact of a higher clopidogrel dose regimen on active metabolite exposure and antiplatelet response in healthy subjects. Clin Pharmacol Ther. 2011;90:287–95.
Bauer T, Bouman HJ, van Werkum JW, Ford NF, Ten BJ, Taubert D. Impact of CYP2C19 variant genotypes on clinical efficacy of antiplatelet treatment with clopidogrel: systematic review and meta-analysis. BMJ. 2011;343:d4588.
Geisler T, Bigalke B, Schwab M. CYP2C19 genotype and outcomes of clopidogrel treatment. N Engl J Med. 2011;364:481–2.
Acknowledgements
We thank all the patients participating in this study. This study was supported by Starting Fund for 1000 Youth Talents (No.2013-RSQ02) and Beijing Science and Technology innovation base cultivating and developing special project (No. Z151100001615054).
Author contributions
ZZ, YT, and ZW designed this research and drafted the manuscript. ZL, WW, YF, WC, and XZ contributed to the acquisition and interpretation of the data. ZW and WL contributed to the analysis of the data.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Wang, Z., Liu, Z., Wang, W. et al. Two common mutations within CYP2C19 affected platelet aggregation in Chinese patients undergoing PCI: a one-year follow-up study. Pharmacogenomics J 19, 157–163 (2019). https://doi.org/10.1038/s41397-018-0036-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41397-018-0036-2
This article is cited by
-
The Impact of CYP2C19 Genotype on the Platelet Reactivity Index (PRI) among Chronic Coronary Syndromes (CCS) Patients Undergoing Percutaneous Coronary Intervention (PCI): Affectability of Rapid Genetic Testing
Cardiovascular Drugs and Therapy (2024)
-
Clopidogrel versus ticagrelor in the treatment of Chinese patients undergoing percutaneous coronary intervention: effects on platelet function assessed by platelet function tests and mean platelet volume
Thrombosis Journal (2021)