Abstract
Introduction
Due the impact of maturation on cardiovascular hemodynamics the degree of cardiovascular dysfunction, attributable to spinal cord injury (SCI), in the pediatric and adolescent population remains unclear. While few studies have begun to assess this, there is still a void in the literature regarding the prevalence of cardiovascular dysfunction and how best to identify and treat it in this population.
Case presentation
The purpose of this case series is to present the cardiovascular profile of three adolescent patients with chronic SCI, ages 14–16, following 2 or 3 days of 24-h Ambulatory Blood Pressure Monitoring (ABPM).
Discussion
We found that there are variations across the different cases in most cardiovascular hemodynamic categories and a clarification of the International Standards to document remaining Autonomic Function after Spinal Cord Injury (ISAFSCI) may be needed to accurately identify the remaining autonomic cardiovascular function in the adolescent SCI population.
Similar content being viewed by others
Introduction
Autonomic cardiovascular regulation is compromised in adult persons with SCI [1]. While the level and severity of injury, as assessed by the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI), may contribute to the degree of cardiovascular dysfunction, it is likely that the cardiovascular alterations following SCI are related to the degree of de-centralized autonomic cardiovascular control [1]. Repeated symptoms of severe symptomatic hypotension can occur throughout the day, including dizziness, lightheadedness, nausea, blurred vision, and syncope. These can be troublesome in terms of quality of life, leading to feelings of fatigue [2], decreased participation in activities of daily living and rehabilitation [3] and impaired cognitive function [4]. While blood pressure (BP) and heart rate (HR) have been studied in adults with SCI [5,6,7], there are few studies assessing normative values in the pediatric SCI population (0–18 years old) [8, 9]. In addition, there have been no studies to date that have examined these parameters in adolescents and young adults (16–21 years old), yet this is the most prominent age range for the onset of SCI in both males and females [10]. The appearance of complications, arising from altered BP and HR, may be different in each of these age ranges due to unique physiologic, cognitive and developmental factors [9]. In fact, a recent study [8] in youth and adolescents (14–16 years) with SCI found that systolic (SBP) and diastolic (DBP) blood pressure were increased and HR was reduced with increasing age.
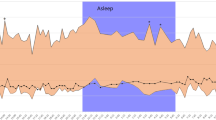
A single seated BP and HR recording is typically collected at each clinical visit; however, given the wide fluctuations in daily BP documented in the adult SCI population, this assessment may not capture the full hemodynamic profile in the adolescent SCI population. Therefore, in order to begin to more fully describe daily fluctuations in BP and HR in the adolescent SCI population, we collected 24-h hemodynamic data using an ambulatory blood pressure monitor (ABPM). The ABPM (Contec Medical; Chicago, IL, USA) is a fully automated, non-invasive method which monitors beat-to-beat BP and HR over the course of a typical day. The ABPM is lightweight, compact and portable. Measurements were taken from the upper arm every 30 min, and subjects were instructed to keep their arm extended and still during collection of the hemodynamic data. The ABPM method of hemodynamic assessments in youth and adolescents offers significant advantages as compared to the usual office BP measurement technique (standard mercury sphygmomanometer). These include, reduced observer bias and device inaccuracies (digit preference), capture of wide fluctuations in BP and limitations of the “white coat effect” [11, 12]. Although many studies [4, 6, 7, 13] have used ABPM to investigate daily fluctuations in BP and HR in adults with SCI, there are currently no reports of its usage in the youth and adolescent SCI population. Several studies have provided evidence that ABPM can be performed with success in the non-SCI population among individuals with different age ranges (infants to late teenagers) [14,15,16]. While most of the studies have used ABPM in the adult SCI population over the course of one typical 24-h period, we aimed to examined BP and HR over the course of 3 non-consecutive days in adolescents with SCI.
ABPM studies have begun to define cardiovascular dysfunction in the adult SCI population, however, additional research is needed to establish normative values for BP and HR in the developing youth and adolescent SCI population. Cardiovascular disturbances following SCI can lead to limitations in daily activities and social participation, and can contribute to cognitive impairment and life-threatening medical conditions. In this project, we present three cases of adolescents with SCI who underwent 24-h ABPM to assess hemodynamic changes over the course of a few non-consecutive days.
Case presentation
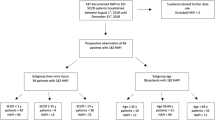
Demographic characteristics of the subjects and the results of their ABPM are presented (Table 1); it should be noted that all patients were chronically injured (>1 year post injury). Listed below is the description of the three subjects who underwent ABPM. The International Standards to document remaining Autonomic Function after Spinal Cord Injury (ISAFSCI) [17] was not completed at the bedside on these patients; therefore, classification had been performed retrospectively. The cases presented are part of a larger research study to address the effects hypotension on cerebral perfusion. This study was approved by Thomas Jefferson University and Western Institutional review boards.
Case report 1
A 12-year-old female awoke one morning in November of 2014 with leg weakness, leg numbness, chest pain, and headache. After a review of the MRI, physicians concluded her injury was consistent with transverse myelitis (TM) which resulted in T4 AIS D SCI. The subject received acute medical care and completed inpatient rehabilitation by the end of December 2014. As an inpatient in March of 2016 her BP was typically low when standing and the rehabilitation staff noticed a slight drop in SBP with standing and walking. At home the patient used an abdominal binder and compression stocking effectively to manage her low BP. She had no known history of autonomic dysreflexia (AD) and completed 3 days of ABPM in May of 2016. This suggested little evidence of hypotension, with bouts of orthostatic hypotension (OH), particularly diastolic, and evidence of hypertension without AD. Use of the ISAFSCI during her clinical visit would have indicated hypotension (i.e., SBP < 90 mmHg) with bouts of orthostatic hypotension (OH: fall in BP ≥ 20/10 mmHg).
Case report 2
In May of 2015 a 15-year-old male was involved in a diving accident and was diagnosed with C5 AIS B SCI. He immediately underwent decompression surgery and an anterior cervical fusion. After a two-week hospital stay he underwent acute SCI rehabilitation for five months before returning home. At his initial evaluation in May of 2016 he reported having no signs or symptoms of AD even though he experienced AD earlier during his injury. He also stated that his OH had improved over the 12-month period since his injury and that he no longer needed medication or an abdominal binder or compression stockings to maintain his BP. Based on his Medical History the patient would have a normal ISAFSCI evaluation; however, in October of 2016 he underwent 2 days of ABPM which suggests diastolic OH and the absence of a nocturnal dip in BP.
Case report 3
A 16-year-old male incurred a traumatic cervical injury at 6-months of age which resultant in a C5 AIS D SCI. At the time of the ABPM, there were no AD or BP concerns over the course of the previous five years, and his ISAFSCI exam would therefore reflect a normal cardiovascular profile. However, the ABPM suggested that the patient is hypotensive (16%) with little evidence of hypertension (3%). The patient has some evidence of OH, particularly diastolic OH, no evidence of AD and has a preserved nocturnal BP dip.
Discussion
The ABPM findings indicate significant variation in 24-h cardiovascular hemodynamics among adolescents with SCI. Like the ISNCSCI examination, the ISAFSCI examination was developed to be used in the adult SCI population. It is recommended that the ISAFSCI be used in conjunction with the International dataset to document the impact of SCI on cardiovascular function. While the International cardiovascular dataset (http://www.iscos.org.uk/international-sci-data-sets) is appropriate for use in any person with traumatic or non-traumatic SCI, the ISAFSCI was created for use in the traumatically injured adult SCI population. That said, the role that altered cardiovascular hemodynamics play in adolescents with SCI is still largely under-investigated. Given that the adolescent population is still developing, the effect of SCI on all systems of the body may not be the same as that demonstrated in adults with SCI. Depending on the age and severity of the injury, plasticity of the nervous system may result in an altered presentation of the cardiovascular profile. Because age affects cardiovascular parameters in uninjured pediatric and adolescent patients [18], revision of the ISAFSCI may be necessary for use in the pediatric and adolescent SCI populations.
In this study we presented three adolescent patients with chronic SCI who were relatively close in age. While Case 1 would have had resulted in abnormal findings for hypotension and OH using the ISAFSCI, the fact that it was diastolic OH and that the subject also showed evidence of hypertension would have been missed. Moreover Case 1 reflects spinal cord disease (SCD) rather than SCI, and the current ISAFSCI was created for use in the SCI population; however, we believe that the ISAFSCI can be used to document the impact of SCD on autonomic cardiovascular control. Case 2 and 3 illustrated normal ISAFSCI finding however after reviewing the ABPM data Case 2 had bouts of diastolic OH and an absent nocturnal dip while Case 3 described a subject that on average was hypotensive 16% of their day with episodic OH 32% of their day. While these symptoms were unnoticed by the subjects, their daily living could be impacted. For example, hypotension can lead to decreased cerebral profusion resulting in lower cognitive abilities while OH can increase the subject’s likelihood of falling.
While adults also present with asymptomatic findings of cardiovascular dysfunction, the ISAFSCI may need to be modified in order to meet the unique needs of the developing nervous and cardiovascular systems in those with adolescent SCI. Even though the ISAFSCI provides values for several hemodynamic parameters (e.g., OH: fall in BP of ≥ 20/10 mmHg), these values will likely need to be expended for use in the pediatric and adolescent SCI population due to the multiple factors related to maturation of the cardiovascular system. This study is the first to collect 24-h ABMP in adolescent patients with SCI. While obtaining multiple days of ABPM measurements presented some challenges, our findings illustrate the potential need to collect data over multiple time points in order to obtain a clear picture of the adolescent patient’s cardiovascular profile. Of importance, O’Sullivan [14] and colleges found a typical nocturnal dip in 1121 children ages 6–16 years old and only a small number of children manifested an increase in BP at night. This emphasizes the need for 24-h ABPM in adolescents and children with SCI given the finding of an absent nocturnal dip in one of the three cases presented here.
As in the adult SCI population, it is important to consider the impact of level of injury on the likelihood of alteration in cardiovascular autonomic control. In particular, it is apparent that diastolic OH is prevalent in these three adolescent cases with SCI/D at or above T4. Revision of the ISAFSCI should perhaps give consideration to the likelihood of the recognized cardiovascular abnormalities given the level of injury. As the ISAFSCI evolves, informing clinicians and researchers about the additive value of collecting 24-h ABPM data on multiple days can lead to an increase awareness of each individual patients cardiovascular-autonomic profile, which in turn will inform clinical decision making and result in an increase in the patients’ quality of life.
References
Wecht JM, Bauman WA. Decentralized cardiovascular autonomic control and cognitive deficits in persons with spinal cord injury. J Spinal Cord Med. 2013;36:74–81. http://www.ncbi.nlm.nih.gov/pubmed/23809520.
Wessely S, Nickson J, Cox B. Symptoms of low blood pressure: a population study. BMJ. 1990;301:362–5.
Illman A, Stiller K, Williams M. The prevalence of orthostatic hypotension during physiotherapy treatment in patients with an acute spinal cord injury. Spinal Cord. 2000;38:741–7.
Jegede AB, Rosado-Rivera D, Bauman WA, Cardozo CP, Sano M, Moyer JM, et al. Cognitive performance in hypotensive persons with spinal cord injury. Clin Auton Res. 2010;20:3–9. http://www.ncbi.nlm.nih.gov/pubmed/19842013.
Frisbie JH. Unstable baseline blood pressure in chronic tetraplegia. Spinal Cord. 2007;45:92–95. http://www.ncbi.nlm.nih.gov/pubmed/16568144.
Rosado-Rivera D, Radulovic M, Handrakis JP, Cirnigliaro CM, Jensen AM, Kirshblum S, et al. Comparison of 24-hour cardiovascular and autonomic function in paraplegia, tetraplegia, and control groups: implications for cardiovascular risk. J Spinal Cord Med. 2011;34:395-403. http://www.ncbi.nlm.nih.gov/pubmed/21903013.
Seabra-Garcez JD, Matos-Souza JR, Goulart D, Pithon KR, Abib E, Etchebehere M, et al. Ambulatory blood pressure is associated with subclinical atherosclerosis in spinal cord injury subjects. Int J Cardiol. 2012;154:89–90. http://www.ncbi.nlm.nih.gov/pubmed/22062895.
Hwang M, Zebracki K, Betz RR, Mulcahey MJ, Vogel LC. Normative blood pressure and heart rate in pediatric spinal cord injury. Top Spinal Cord Inj Rehabil. 2013;19:87–95. http://www.ncbi.nlm.nih.gov/pubmed/23671378.
Zebracki K, Hwang M, Patt PL, Vogel LC. Autonomic cardiovascular dysfunction and vitamin D deficiency in pediatric spinal cord injury. J Pediatr Rehabil Med. 2013;6:45–52. http://www.ncbi.nlm.nih.gov/pubmed/23481891.
WHO. Spinal cord injury. www.who.int/mediacentre/factsheets/fs384/en/. Updated 2013. Accessed 22 Aug 2014.
Gillman MW, Cook NR. Blood pressure measurement in childhood epidemiological studies. Circulation. 1995;92:1049–57. http://www.ncbi.nlm.nih.gov/pubmed/7641339.
Lurbe E, Thijs L, Redon J, Alvarez V, Tacons J, Staessen J. Diurnal blood pressure curve in children and adolescents. J Hypertens. 1996;14:41–46. http://www.ncbi.nlm.nih.gov/pubmed/12013493.
Hubli M, Krassioukov AV. Ambulatory blood pressure monitoring in spinal cord injury: clinical practicability. J Neurotrauma. 2014;31:789–97. http://www.ncbi.nlm.nih.gov/pubmed/24175653.
O’Sullivan JJ, Derrick G, Griggs P, Foxall R, Aitkin M, Wren C. Ambulatory blood pressure in school children. Arch Dis Child. 1999;80:529–32. http://www.ncbi.nlm.nih.gov/pubmed/10332001.
Khan IA, Gajaria M, Stephens D, Balfe JW. Ambulatory blood pressure monitoring in children: a large center’s experience. Pediatr Nephrol. 2000;14:802–5. http://www.ncbi.nlm.nih.gov/pubmed/10955931.
Varda NM, Gregoric A. Twenty-four-hour ambulatory blood pressure monitoring in infants and toddlers. Pediatr Nephrol. 2005;20:798–802. http://www.ncbi.nlm.nih.gov/pubmed/15856318.
Krassioukov A, Biering-Sorensen F, Donovan W, Kennelly M, Kirshblum S, Krough K, et al. International standards to document remaining autonomic function after spinal cord injury. J Spinal Cord Med. 2012;35:201–10. https://doi.org/10.1179/1079026812Z.00000000053.
Flynn JT, Kaelber DC, Baker-Smith CM, Blowery D, Carroll A, Stephan DR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 2017;140:e20171904.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Krisa, L., Vogel, L.C. & Wecht, J.M. Use of ambulatory blood pressure monitoring in adolescents with SCI: a case series. Spinal Cord Ser Cases 3, 17095 (2017). https://doi.org/10.1038/s41394-017-0034-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-017-0034-7