Abstract
Study design
Systematic scoping review.
Objectives
The purpose of this project was to conduct a scoping review to understand the amounts, types, correlates, and outcomes of physical activity (PA) participation for ambulators with SCI.
Methods
A systematic search was employed among five large databases and two theses/dissertation databases, yielding 3257 articles. Following a two-phase screening process by independent coders, 17 articles were included in the review. Data were charted and summarized, and correlates were coded using the COM-B model.
Results
11 studies were cross-sectional, 5 studies involved an exercise intervention, and 1 study used mixed methods. Overall, ambulators with SCI participated in low levels of PA. The type of PA investigated across all studies was leisure-time PA (e.g., sports, exercise). Psychological and physical capability (e.g., perceived behavioral control, fatigue), social and environmental opportunity (e.g., perceptions of disability, cost), and automatic and reflective motivation (e.g., boredom, intentions) were correlates of PA measured within studies. Exercise intervention studies measured physical (e.g., strength, fitness) and one psychological outcome (i.e., depression). No studies examined the quality of PA experiences.
Conclusions
Only leisure-time PA has been investigated among ambulators with SCI, and low levels of leisure-time PA have been reported. Correlates of leisure-time PA can be mapped onto all COM-B model constructs and are potential targets for PA-enhancing interventions. Further investigation is warranted into the physical and psychosocial outcomes across all types of LTPA in addition to understanding the quality of LTPA experiences.
Similar content being viewed by others
Introduction
Motor function and recovery after a spinal cord injury (SCI) largely depends on the completeness of the lesion [1]. More than half of SCIs are functionally incomplete, meaning that the possibility of motor recovery is more likely [2]. Indeed, there are estimates that up to 75% of individuals with incomplete injuries retain some ambulatory capacity [3, 4]. It is expected that this number will continue to grow for several reasons such as advancements in acute medical treatment and changing causes of injuries [5]. Given the increasing numbers of individuals with SCI who may ambulate (i.e., do not use a wheelchair for mobility), there is a demand for greater research to understand the unique participation experiences and needs of this population.
Physical activity (PA) is one aspect of participation in which individuals with SCI can experience several physical (e.g., fitness) and psychosocial (e.g., subjective well-being) benefits regardless of mode of mobility [6, 7]. International scientific SCI exercise guidelines were recently developed, clearly identifying the amount, duration, and intensity of PA required to improve fitness [8]. Despite this knowledge, very few individuals with SCI are participating in enough PA to achieve fitness and health benefits. Indeed, only 12% of persons with SCI in Canada are meeting the SCI guidelines [9] and up to 50% of persons with SCI are not doing any leisure-time PA (LTPA; activity that one chooses to do in their own time such as exercise or sport) [10].
Preliminary research suggests that people with SCI who ambulate participate in even less LTPA than wheelchair users with SCI [10]. For instance, a Canadian study estimated that wheelchair users with SCI participate in significantly more LTPA (M = 35.6 min/day) compared with persons with SCI who ambulate (M = 25.2 min/day) [10]. These concerning findings were supported by a more recent study that found that ambulators with SCI engage in significantly less planned exercise and organized sports compared with their wheelchair-using counterparts [11]. Despite greater functional capabilities of ambulators compared with wheelchair users with SCI, those who ambulate with SCI face barriers to participating in PA. For example, greater fatigue, pain [12], poorer wheelchair skills, and negative perceptions of PA due to excessive metabolic demands [13] may contribute to lower levels of PA participation.
Initial research has examined some factors relating to PA participation for individuals with SCI who ambulate [14]. However, a systematic investigation is required to examine how factors relating to PA participation can be improved using theory-informed interventions. Behavior change theories are useful for identifying factors that influence whether individuals engage (or withdraw) in health behaviors. Indeed, interventions designed to increase PA among people with disabilities are more effective when they are informed by behavior change theories [15].
One behavior change theory that has been employed across a variety of behaviors and settings (e.g., PA and rehabilitation) [16] is the COM-B model [17]. The COM-B model suggests that performance of a behavior (e.g., PA) requires capability (i.e., the physical or psychological ability to complete the behavior), opportunity (i.e., physical and social environment that enables the behavior), and motivation (i.e., reflective and automatic mechanisms that ignite or extinguish the behavior) [17]. In order to change PA, interventions need to target one or more of these three categories of factors. By using the COM-B model to map factors that influence PA behavior, researchers can then identify which behavior change techniques to incorporate when developing PA interventions [15, 18].
Using theory to guide the mapping of research evidence is a first step in developing behavior change interventions. The literature on PA for people with SCI who ambulate needs to be summarized, and gaps and future directions need to be identified to begin the process of creating a theory-informed PA intervention. The purpose of this scoping review was to understand the extent of the literature on PA participation among individuals with SCI who ambulate. Specifically, this review identified the amount, types, correlates, and outcomes of PA, with respect to the COM-B model constructs.
Methods
Scoping reviews identify the parameters and gaps in the current literature [19, 20]. The five-stage methodological framework for scoping reviews developed by Arksey and O’Malley [19] was employed: (1) identify the research question, (2) identify relevant studies, (3) select studies, (4) chart the data, and (5) summarize the results. As recommended by Daudt et al. [20], stage 6 involved consultation with relevant stakeholders (see below). The protocol for this review was published on Open Science Framework on April 29, 2019 and can be found here: https://doi.org/10.17605/OSF.IO/R5CA.
Stage 1: identify the research question
Through an iterative process of consultation with the research team and stakeholders, the primary research question was: what is known from the literature about PA among individuals with SCI who ambulate? For the purpose of this review, we were interested in all types of PA (e.g., activities of daily living, LTPA) with the exception of rehabilitation activities (e.g., locomotor treadmill training). This is because there have been several reviews published on this topic [21, 22] and since our overarching goal is to increase PA, rehabilitative PA is not an appropriate activity to target.
Stage 2: identify relevant studies
The literature search strategy was developed by the lead author (SVCL) in conjunction with a Health Sciences Librarian and in consultation with the entire research team. The search terms were informed by previous systematic reviews of SCI and PA [7, 15]. Examples of search terms used included: tetrapleg*, parapleg*, spinal cord*, physical* activ*, sport*, walk*, ambulat*, and gait aid*. Multiple terms such as spin* lesion*, cauda equina syndrome, myelitis, and posterior cord syndrome were used to describe the varying terms used in the literature to describe SCI. The subject headings and syntax were adapted for each database. The complete search strategy for MedLine can be found in Supplementary Appendix 1.
The lead author (SVCL) conducted separate searches of articles published between 1980 and 2019 in the following databases: MedLine, PsycInfo, EMBASE, CINAHL, Web of Science, and Sport Discus. In addition, a gray literature search was conducted in Open Access Theses and Dissertations and ProQuest Dissertations and Theses. All articles were uploaded to the database software platform RefWorksTM where the de-duplication process was performed. The reference lists of included studies were hand searched by the first and second authors (SVCL and KRT) for additional relevant articles. A final list of the included studies was sent to all members of the research team for their records.
Stage 3: select studies
This review included a two-phase screening process: (1) title and abstract, and (2) full text. SVCL and KRT tested the reliability of the article selection tool using a sample of abstracts prior to the review. After independently screening the titles/abstracts of articles against the inclusion and exclusion criteria, the full texts of articles were retrieved. SVCL and KRT then independently screened the full texts of studies against the inclusion criteria, consulting the other authors (RBS or KAMG) when disagreements arose. Neither author was blinded to the study’s title, author, or institution.
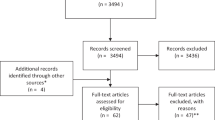
The full inclusion and exclusion criteria for articles are reported in the published protocol (https://doi.org/10.17605/OSF.IO/R5CAK). Briefly, all study designs were included. Participants had to be an adult (18 + years of age), have an SCI, and ambulate as their primary mode of mobility. Participants were not excluded based on whether they used a mobility device for walking or not. Any intervention or outcome had to examine some aspect related to PA. Although there was no restriction on setting, studies had to be published after 1980 and in English. Studies were excluded if data from ambulatory participants could not be differentiated from that of wheelchair users. If the study examined PA for the purpose of rehabilitation (i.e., interventions used to restore and/or recover functional ability or improve performance, such as therapeutic exercise, gait training, and prostheses) [23], the study was also excluded. A PRISMA flow chart [24] outlining the search strategy process can be seen in Fig. 1.
PRISMA-P flow diagram [23] of article selection process.
Stage 4: chart the data
Using a predetermined data abstraction tool adapted from Higgins and Deeks [25], the first (SVCL) and third (RBS) authors completed the data abstraction process. The authors discussed the tool before abstracting data to ensure clarity and consistency. The first author (SVCL) extracted the following information from each article: author(s); year of publication; type of article; title; study design; whether PA was an independent or dependent variable; type of PA; how PA was measured; total number of participants and their demographics (e.g., age, mobility devices used); research setting (e.g., lab, community); intervention details (if applicable); relevant results; and key conclusions. The third author (RBS) checked the abstractions to ensure that all relevant information was obtained from the included articles. Any discrepancies between authors were resolved through discussion. The authors were not blinded during the data abstraction and charting process.
Stage 5: collating, summarizing, and reporting the results
The results were summarized according to amounts of PA (e.g., minutes of PA), types of PA (i.e., sport, exercise, or other), correlates of PA (i.e., barriers, facilitators, predictors, or outcomes), and outcomes of PA (i.e., physical or psychosocial). Correlates of PA were categorized using the COM-B model, whereby factors identified in selected articles were then analyzed using COM-B model constructs. Risk of bias and quality assessments of articles were not completed as these assessments do not align with the objectives of a scoping review [25].
Stage 6: stakeholder consultation
When conducting reviews, it is valuable to consult with stakeholders to provide insight on pertinent issues in the community [26]. Stakeholder consultation aligns with an integrated knowledge translation approach to research [27] as it ensures that the objectives of the review are relevant for end users. For this review, the executive director of a local SCI organization and three people ambulating with SCI were consulted during both the design of the research question, and during stages of the search strategy through informal interviews. Topics discussed included what they wanted to know about PA for ambulators with SCI, definitions of ambulators with SCI, PA programs for ambulators with SCI, and current PA practices.
Results
Articles retrieved
The search yielded 3257 articles (see Fig. 1). After title/abstract and full-text screening and hand searching of articles, 17 articles met the inclusion criteria (see Supplementary Appendix 2 for a list of included articles). Of these articles, 14 were original studies and three were secondary analyses. Two articles were unpublished theses. Characteristics of articles can be found in Table 1 and data extracted from each article are presented in Supplementary Appendix 3.
Article characteristics
Most articles were published between 2010 and 2018 (n = 16). Specifically, articles were published in 2005 (n = 1), 2010 (n = 1), 2011 (n = 1), 2012 (n = 1), 2013 (n = 1), 2014 (n = 1), 2015 (n = 2), 2016 (n = 5), 2017 (n = 3), and 2018 (n = 1). The number of ambulatory participants with SCI per article ranged between 1 and 161, with a total sample of 531 individuals. Across articles, 178 participants walked independently of an assistive device, 18 participants walked with a specifically identified aid (e.g., canes, orthotics), and 239 participants walked with an unidentified aid. Some articles did not report whether participants used an aid or not (n = 96 individuals).
Demographic characteristics were reported in six articles. In these six articles, the average age of participants was 46.31 years (n = 5 articles); SCIs were at the lumbar (n = 12), thoracic (n = 7), and cervical (n = 34) levels (n = 4 articles); the average time since injury was 9.62 years (n = 5 articles); and there were more male participants (n = 53) than female participants (n = 14). Sixteen articles were quantitative, and one article used a mixed-methods design (qualitative interviews with secondary analysis of quantitative cross-sectional data from a different sample). Of the quantitative studies, five involved an intervention (prepost design, n = 4; randomized controlled trial; n = 1), and 11 articles employed a cross-sectional design (3 of which were secondary analyses). Nine articles reported on the amount and prevalence of LTPA, one article examined other characteristics of LTPA, five articles examined correlates of LTPA, and four articles reported on outcomes from participating in LTPA. A detailed list of article characteristics can be found in Table 1.
Prevalence and amount of LTPA
Two articles reported that only 7% [28] and 10% [11] of individuals with SCI who ambulate participate in organized sports. One article reported that 66% of ambulators with SCI participate in planned exercise for a median of 4 h per week [11]. Other articles reported lower numbers, suggesting that 25–32% of ambulators with SCI participate in LTPA [29, 30] for an average of 3 h per week [31].
When activity was analyzed by intensity, participants spent an average of 3 h/week doing light LTPA, 2 h/week doing moderate LTPA, 1 h/week doing strenuous LTPA, and 1 h/week doing muscle-strengthening exercises [32]. Using this same sample, it was reported that 75% of individuals with SCI who ambulate are physically active, but only 39% meet the World Health Organization (WHO) guidelines on PA (i.e., 150 min of moderate-intensity aerobic PA) [33]. Another article reported that SCI ambulators participate in LTPA for 0–170 min per day for an average of 26 min per day [10]. It was also reported that older adults with SCI who do not use a wheelchair for mobility participate in LTPA for an average of 52 min per day and moderate-to-heavy LTPA for an average of 38 min per day [34].
Types of LTPA
All articles measured LTPA. Nine articles did not specify the type of LTPA. When articles did report particular types of LTPA, organized sport (n = 2), aerobic exercise (n = 4), resistance training (n = 1), and general exercise (n = 2) were measured. Measures used to assess LTPA included an author-developed self-report tool (n = 2), the Physical Activity Recall Assessment for People with SCI (PARA-SCI; n = 5), and the Physical Activity Scale for Individuals with Physical Disabilities (PASIPD; n = 4).
Other characteristics of LTPA
One article compared the physiological responses of ambulators with SCI to able-bodied individuals when participating in sub-maximal and maximal graded treadmill and cycling tests [35]. The researchers found that peak oxygen uptake (VO2 peak), heart rate, and intensity level are similar for treadmill and cycling tests. Lower mechanical efficiency occurs on a treadmill than when cycling, and individuals with SCI who ambulate achieve a significantly lower VO2 peak, peak heart rate, and workload than able-bodied individuals on both apparatuses.
Correlates of LTPA
Correlates (i.e., factors that related to LTPA levels) were mapped onto COM-B model constructs (see Fig. 2). All of the COM-B model constructs were represented within the scoping review. The most commonly investigated constructs were reflective motivation (e.g., attitudes and intentions), with seven different correlates measured seven times across articles, and physical capability (e.g., pain perceptions), with five different correlates measured eight times across articles. Included articles also examined environmental opportunity (e.g., financial costs of participating in exercise), with four different correlates measured five times across articles; psychological capability (e.g., perceived behavioral control), with three different correlates measured three times across articles; social opportunity (e.g., underestimated disability), with two different correlates measured across two articles; and automatic motivation (e.g., boring), with two different correlates measured across two articles. Each of the COM-B constructs are discussed in greater detail in the following paragraphs.
Physical capability
Two articles measured self-reported fatigue, one of which found no significant correlation with LTPA [31]. Martin Ginis et al. [14], however, reported fatigue as both a barrier to, and facilitator of LTPA using qualitative methods. Similarly, pain was also reported as a barrier and facilitator for LTPA [14], and another article found that 40% of ambulators with SCI report pain as a barrier to exercise [29]. Health conditions prevented exercising among 25% of participants while 17% perceived exercise to be too difficult [36]. Furthermore, participants (42%) identified lack of energy as a barrier to exercise [29, 36].
Psychological capability
There was a significant negative correlation between perceived behavioral control and LTPA for individuals with SCI who ambulate [14]. Only 8% of participants reported that they do not know how, or where, to exercise [36].
Environmental opportunity
Financial cost was a barrier to exercise participation for 32% [29] and 33% [36] of ambulators with SCI, respectively. Other environmental opportunity barriers to exercise were time (25%), unknown location (8%), and lack of transportation (8%) [14].
Social opportunity
Martin Ginis et al. [14] qualitatively reported that individuals with SCI who ambulate often feel that their disability is underestimated, and they lack a group identity which negatively influences their LTPA participation.
Automatic motivation
An article identified that participants view exercise as boring (42%) and they lack interest (33%), which acts as a barrier to participation [36].
Reflective motivation
There was a significant positive correlation between attitudes and intentions and LTPA for individuals with SCI who ambulate [14]. Furthermore, 58% perceive lack of motivation as a barrier to exercise and 25% of participants believe that exercise does not provide any benefit [36]. Exercise was believed to worsen, and not improve, existing health conditions by 25% of participants [36]. Laziness was a barrier to exercise for 50% of individuals [36]. Further, low wheelchair skill self-efficacy was qualitatively identified as a barrier to participating in wheelchair sports [14]. Lastly, it was demonstrated that men with SCI who ambulate have significantly lower barrier self-efficacy than manual wheelchair users with SCI and this type of self-efficacy significantly predicts LTPA [37].
Outcomes of participating in LTPA
Five intervention studies reported on outcomes from participating in LTPA. Outcomes were broadly categorized as physical (13 outcomes) or psychological (1 outcome). The 13 physical outcomes were further divided into 5 outcome sub-categories: strength, cardiovascular, body composition, pain and fatigue, and cognitive.
Physical outcomes
Strength-related benefits were reported from a 12-week periodized resistance training program completed twice per week [38]. Specifically, the participant reported a 22.2% increase in chest press weight and 12.8% increase in leg press weight [38]. Similarly, this resistance training program lead to cardiovascular improvements, as the participant was only training at 69% of their cardiovascular capacity postintervention compared with 81% of their capacity preintervention. The same resistance training program produced change in body composition, specifically a 0.9% decrease in fat mass. Cardiovascular benefits were obtained from a 6-week progressive aerobic exercise program completed three times per week, including an 18% increase in VO2 peak and a significant increase in the number of steps taken outside of training (~916 per day) [39, 40].
Pain and fatigue outcomes were measured following an aerobic exercise program, resulting in a 25% decrease in pain intensity, 46% decrease in pain interference, and 20% decrease in fatigue [39, 40]. Lastly, the cognitive outcome was reported from a single session, locomotor treadmill test [41]. High-intensity exercise provided significantly higher levels of brain-derived neurotrophic factor (BDNF) compared with moderate-intensity exercise, and BDNF decreased significantly more 15- and 30-min post moderate-intensity exercise compared with high-intensity exercise. No relationships between BDNF and duration of exercise and insulin-like growth factor-1 and exercise were found.
Psychological outcomes
The only psychological outcome investigated was depressive symptomology, which decreased 60% following the aerobic exercise program [39, 40].
Discussion
This review identified 17 articles on PA involving individuals with SCI who ambulate. Sixty-nine percent of articles were published after 2014, highlighting the infancy of PA research for this population. The review charted literature according to the amount and prevalence, types, correlates, and outcomes of PA. The aim of this scoping review was to understand what is currently known about PA and ambulators with SCI. A scoping review was conducted to map the literature and in part, use theory to identify what evidence is needed next before creating an intervention in this population. While this review intended to capture information on all forms of nonrehabilitative PA, LTPA was the only form of PA measured in the included articles. Thus, the following discussion will refer to LTPA rather than PA.
Overall, a total of 531 individuals with SCI who ambulate were included in this review. Participants in the reviewed studies were predominantly male adults with cervical-level injuries who walk with a gait aid and were, on average, 10 years post injury. These demographic characteristics are representative of the general SCI population and current demographics of injury profiles [2]. Yet, only six articles reported demographic information specific to ambulators with SCI (e.g., age, sex). Future research reports must include greater details on participants (e.g., types of mobility aids) to contextualize the data and provide some indication of generalizability.
Many of the reviewed articles reported that individuals with SCI who ambulate participate in low levels of LTPA. In particular, only 7–10% of ambulators with SCI appear to be partaking in organized sport [11, 28] and only 39% are meeting the WHO guidelines for PA [33]. When compared with LTPA levels of wheelchair users with SCI, these numbers are especially discouraging. For instance, studies report that between 25 and 28% of people with SCI who use wheelchairs are involved in organized sport [11, 28]. Furthermore, four studies reported that manual wheelchair users with SCI participate in significantly more LTPA compared with ambulators with SCI [10, 11, 32, 33]. Yet, other research has not found significant differences in activity levels between individuals who use a wheelchair versus ambulate with SCI [29, 30, 34]. The discrepancies in activity levels underscore the need to examine other factors, in addition to mode of mobility, that may influence LTPA participation (e.g., age, pain and fatigue levels, access to resources). Overall, these figures support calls to develop evidence-informed LTPA-enhancing strategies for individuals with SCI who ambulate [14, 28, 32, 33]. These strategies should promote guidelines developed specifically for the SCI population [8] rather than for the general population (i.e., WHO guidelines) [33] as individuals with SCI can achieve benefits from less than 150 min of PA per week [8].
The correlates identified in this review were largely barriers (rather than facilitators) to LTPA participation. This finding aligns with the current landscape of research investigating LTPA for people with disabilities, which has prioritized identifying barriers over facilitators. Our review supports a call to move on from research that merely describes barriers to LTPA for people with disabilities, to research that develops, tests and implements strategies to alleviate barriers [42]. That said, physical capability (e.g., pain and fatigue) appears to be an important factor for participation in LTPA for ambulators with SCI. Indeed, salient facilitators of LTPA identified from a qualitative meta-synthesis include maintaining independence and restitution of physical recovery [6]. These facilitators warrant greater investigation among ambulators with SCI given ambulators’ potentially greater levels of independence and walking recovery compared with wheelchair users with SCI. Furthermore, the significant results were found for certain psychological capability (i.e., perceived behavioral control, barrier self-efficacy) and reflective motivation (i.e., attitudes and intentions) factors. A recent review of reviews, framed using a social ecological model, has identified similar intrapersonal factors related to LTPA for people with physical disabilities [42]. However, the review also identified several other influences on LTPA participation, including interpersonal, institutional, community, and policy factors [42]. Clearly, a more comprehensive and theoretically informed investigation is warranted of the most significant predictors of both the quantity, and quality of LTPA, for ambulators with SCI. This information can inform the development, testing, and dissemination of evidence-based strategies to improve LTPA experiences for persons with SCI who ambulate.
The review identified several physical outcomes (e.g., increased strength and cardiovascular fitness) for individuals with SCI who ambulate following participation in aerobic and/or resistance training exercise interventions. This is not surprising, given the several randomized controlled trials and systematic reviews that outline the relationships between exercise and physical health outcomes for people with SCI [7]. Interestingly, in the present review, aerobic exercise led to a decrease in pain and fatigue outcomes [39, 40]. However, this review identified that pain and fatigue were also frequently viewed as barriers to LTPA participation [14, 29]. Thus, LTPA messaging in programs and research should focus on how LTPA may improve, rather than worsen, feelings of pain and fatigue. Lastly, only one psychological outcome was reported across interventions in this review (i.e., 60% decrease in depressive symptomology) [39, 40], suggesting a need for greater investigation into psychosocial and general participation outcomes (e.g., employment, quality of life) following LTPA interventions.
In cataloging the literature, several shortcomings became apparent. First, no articles accounted for other forms of PA like activities of daily living or occupational PA. This is important because evidence suggests that activities of daily living and occupational PA may contribute to overall daily PA for people with SCI [43, 44]. The results from this review may be underestimating the total PA levels of ambulators with SCI. Second, most of the interventions only incorporated aerobic exercise. This is a problem because the SCI exercise guidelines prescribe both aerobic and strength training for improving muscle strength and cardiorespiratory fitness [8]. Third, none of the articles looked at the quality of PA participation. Full and effective PA participation is not simply a matter of doing PA, but also experiencing autonomy, belongingness, challenge, engagement, mastery, and meaning [45, 46]. Researchers need to incorporate measures of the quality of PA experiences in future studies. Fourth, the term “ambulator” was not consistently described as there is no standard definition of an ambulator with SCI. For instance, some authors defined ambulators as individuals who walk in the community, whereas other authors referred to ambulators as individuals who retained some ambulatory capacity that is not necessarily functional for daily activities. Importantly, future research should clarify “ambulator” definitions for people with SCI to reduce ambiguity.
Strengths and limitations
The strengths of this review include the rigorous, systematic search strategy guided by the expertise of a Health Sciences Librarian. We also registered the protocol onto Open Science Framework prior to searching, which reduces bias in our review [47]. The use of the COM-B model [17] to analyze extracted data contributes to our theoretical understanding of behavior change factors that influence PA among individuals with SCI who ambulate. Finally, stakeholders were consulted to ensure that relevant and appropriate questions were answered in this review, strengthening the real-world applicability of the findings.
This review is not without its limitations. Importantly, the conclusions made from this review apply only to LTPA despite our attempts to synthesize the literature on all types of nonrehabilitative PA. Furthermore, there are likely many other PA studies that included participants with SCI who ambulate, but these studies could not be included because they did not report mode of mobility or separate results based on mobility status. Because of this, we likely did not capture all studies that include PA information on ambulators with SCI. This review should be treated as complementary evidence to earlier reviews on PA participation among individuals with SCI.
Conclusion
In summary, this review identified predominantly quantitative studies that examined LTPA among individuals with SCI who ambulate. These individuals have low LTPA levels. Further research is required to understand demographic characteristics that may moderate PA participation. Using a behavior change theory-informed approach to systematically investigate factors relating to LTPA participation (beyond just physical capability) is necessary. This can lead to the development of comprehensive, behavior change theory-informed interventions to improve the quantity, and quality of LTPA for this population [15]. Outcomes tested in PA interventions need to go beyond strength and cardiovascular fitness and also assess participation and psychosocial outcomes. Diverse study designs and methodologies are necessary to unravel what constitutes quality LTPA experiences for ambulators with SCI. Most importantly, future research should continue to collaborate with stakeholders to ensure appropriate research questions are answered for end users.
Data availability
All data generated or analyzed during this study are included in this published article (and its Supplementary information files). The protocol for this scoping review can be found on Open Science Framework here: https://doi.org/10.17605/OSF.IO/R5CAK.
References
Maynard F, Bracken M, Creasey G, Ditunno Jr JF, Donovan WH, Ducker TB, et al. International standards for neurological and functional classification of spinal cord injury. Spinal Cord. 1997;35:266–74.
DeVivo M, Chen Y. Trends in new injuries, prevalent cases, and aging with spinal cord injury. Arch Phys Med Rehabilit. 2011;92:332–8.
Waters RL, Adkins RH, Yakura JS, Sie I. Motor and sensory recovery following incomplete paraplegia. Arch Phys Med Rehabilit. 1994;75:67–72.
Waters RL, Adkins RH, Yakura JS, Sie I. Motor and sensory recovery following incomplete tetraplegia. Arch Phys Med Rehabilit. 1994;75:306–11.
Nijendijk JHB, Post MWM, Van Asbeck FWA. Epidemiology of traumatic spinal cord injuries in the Netherlands in 2010. Spinal Cord. 2014;52:258–63.
Williams TL, Smith B, Papathomas A. The barriers, benefits and facilitators of leisure time physical activity among people with spinal cord injury: a meta-synthesis of qualitative findings. Health Psychol Rev. 2014;8:404–25.
Van der Scheer JW, Martin Ginis KA, Ditor DS, Goosey-Tolfrey VL, Hicks AL, West CR, et al. Effects of exercise on fitness and health of adults with spinal cord injury: a systematic review. Neurology. 2017;89:736–45.
Martin Ginis KA, van der Scheer JW, Latimer-Cheung AE, Barrow A, Bourne C, Carruthers P, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord. 2018;56:308–21.
Rocchi M, Routhier F, Latimer-Cheung AE, Martin Ginis KA, Noreau L, Sweet SN. Are adults with spinal cord injury meeting the spinal cord injury-specific physical activity guidelines? A look at a sample from a Canadian province. Spinal Cord. 2017;55:454–9.
Martin Ginis KA, Latimer AE, Arbour-Nicitopoulos KP, Buchholz AC, Bray SR, Craven BC, et al. Leisure time physical activity in a population-based sample of people with spinal cord injury part I: demographic and injury-related correlates. Arch Phys Med Rehabilit. 2010;91:722–8.
Garshick E, Mulroy S, Graves DE, Greenwald K, Horton JA, Morse LR. Active lifestyle is associated with reduced dyspnea and greater life satisfaction in spinal cord injury. Arch Phys Med Rehabilit. 2016;97:1721–7.
Saunders LL, Krause JS, DiPiro ND, Kraft S, Brotherton S. Ambulation and complications related to assistive devices after spinal cord injury. J Spinal Cord Med. 2013;36:652–9.
Bateni H, Maki BE. Assistive devices for balance and mobility: benefits, demands, and adverse consequences. Arch Phys Med Rehabilit. 2005;86:134–45.
Martin Ginis KA, Papathomas A, Perrier M-J, Smith B. Psychosocial factors associated with physical activity in ambulatory and manual wheelchair users with spinal cord injury: a mixed-methods study. Disabil Rehabilit. 2017;39:187–92.
Ma JK, Martin Ginis KA. A meta-analysis of physical activity interventions in people with physical disabilities: content, characteristics, and effects on behaviour. Psychol Sport Exerc. 2018;37:262–73.
Parry SM, Knight LD, Connolly B, Baldwin C, Puthucheary Z, Morris P, et al. Factors influencing physical activity and rehabilitation in survivors of critical illness: a systematic review of quantitative and qualitative studies. Intensive Care Med. 2017;43:531–42.
Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42.
Latimer AE, Martin Ginis KA, Arbour KP. The efficacy of an implementation intention intervention for promoting physical activity among individuals with spinal cord injury: a randomized controlled trial. Rehabilit Psychol. 2006;51:273–80.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res. 2005;8:19–32.
Daudt HML, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med Res Methodol. 2013;13:48.
Mekki M, Delgado AD, Fry A, Putrino D, Huang V. Robotic rehabilitation and spinal cord injury: a narrative review. Neurotherapeutics. 2018;15:604–17.
Morawietz C, Moffat F. Effects of locomotor training after incomplete spinal cord injury: a systematic review. Arch Phys Med Rehabilit. 2013;94:2297–308.
Hall AM, Ferreira PH, Maher CG, Latimer J, Ferreira ML. The influence of the therapist-patient relationship on treatment outcome in physical rehabilitation: a systematic review. Phys Ther. 2010;90:1099–110.
Moher D, Liberati A, Tetzlaff J, Altman DG, the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9.
Higgins JPT, Green S, editorss. Cochrane handbook for systematic reviews of interventions: Cochrane Book Series. Chichester: The Cochrane Collaboration and Wiley; 2008.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2013;5:69.
Straus SE, Tetroe J, Graham ID. Knowledge translation in health care: moving from evidence to practice. Chichester: Wiley; 2013.
Blauwet C, Sudhakar S, Doherty AL, Garshick E, Zafonte R, Morse LR. Participation in organized sports is positively associated with employment in adults with spinal cord injury. Am J Phys Med Rehabilit. 2013;92:393–401.
Roberton T, Bucks RS, Skinner TC, Allison GT, Dunlop SA. Barriers to physical activity in individuals with spinal cord injury: a Western Australian study. Aust J Rehabilit Couns. 2011;17:74–88.
Mat Rosly M, Halaki M, Hasnan N, Mat Rosly H, Davis GM, Husain R. Leisure time physical activity participation in individuals with spinal cord injury in Malaysia: barriers to exercise. Spinal Cord. 2018;56:806–18.
Freixes O, Rivas ME, Agrati PE, Bochkezanian V, Waldman SV, Olmos LE. Fatigue level in spinal cord injury AIS D community ambulatory subjects. Spinal Cord. 2012;50:422–5.
Rauch A, Hinrichs T, Oberhauser C, Cieza A, for the SwiSCI study Group. Do people with spinal cord injury meet the WHO recommendations on physical activity? Int J Public Health. 2016;61:17–27.
Rauch A, Hinrichs T, Cieza A. Associations with being physically active and the achievement of WHO recommendations on physical activity in people with spinal cord injury. Spinal Cord. 2017;55:235–43.
Jörgensen S, Martin Ginis KA, Lexell J. Leisure time physical activity among older adults with long-term spinal cord injury. Spinal Cord. 2017;55:848–56.
Wouda MF, Wejden L, Lundgaard E, Strøm V. Energetic and cardiovascular responses to treadmill walking and stationary cycling in subjects with incomplete spinal cord injury. Spinal Cord. 2016;54:51–6.
Scelza WM, Kalpakjian CZ, Zemper ED, Tate DG. Perceived barriers to exercise in people with spinal cord injury. Am J Phys Med Rehabilit. 2005;84:576–83.
Stapleton J, Martin Ginis KA. Sex differences in theory-based predictors of leisure time physical activity in a population-based sample of adults with spinal cord injury. Arch Phys Med Rehabilit. 2014;95:1787–90.
Bowditch J. The effect of a periodized resistance training program on strength and ambulation in an individual with incomplete chronic spinal cord injury [dissertation]. Fort Myers, FL: Florida Gulf Coast University; 2015.
DiPiro MND. Effects of aerobic exercise training on walking and health-related outcomes in individuals with chronic incomplete spinal cord injury [dissertation]. Charleston, SC: Medical University of South Carolina; 2015.
DiPiro ND, Embry AE, Fritz SL, Middleton A, Krause JS, Gregory CM. Effects of aerobic exercise training on fitness and walking-related outcomes in ambulatory individuals with chronic incomplete spinal cord injury. Spinal Cord. 2016;54:675–81.
Leech KA, Hornby TG. High-intensity locomotor exercise increases brain-derived neurotrophic factor in individuals with incomplete spinal cord injury. J Neurotrauma. 2017;34:1240–8.
Martin Ginis KA, Ma JK, Latimer-Cheung AE, Rimmer JH. A systematic review of review articles addressing factors related to physical activity participation among children and adults with physical disabilities. Health Psychol Rev. 2016;10:478–94.
Ma JK, McCracken LA, Voss C, Chan FHN, West CR, Martin Ginis KA. Physical activity measurement in people with spinal cord injury: comparison of accelerometry and self-report (the physical activity recall assessment for people with spinal cord injury). Disabil Rehabilit. 2020;42:240–6.
Sinden KE, Martin Ginis KA, the SHAPE-SCI Research Group. Identifying occupational attributes of jobs performed after spinal cord injury: implications for vocational rehabilitation. Int J Rehabilit Res. 2013;36:196–204.
Martin Ginis KA, Evans MB, Mortenson WB, Noreau L. Broadening the conceptualization of participation of persons with physical disabilities: a configurative review and recommendations. Arch Phys Med Rehabilit. 2017;98:395–402.
Evans B, Shirazipour C, Allan V, Zanhour M, Sweet S, Martin Ginis KA, et al. Quality participation in parasport: integrating evidence and community insights to develop a conceptualization of optimal parasport experiences. Psychol Sport Exerc. 2018;37:79–90.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
Acknowledgements
We thank Matthew Vis Dunbar for his assistance and expertise in developing the review methodology for this study.
Funding
This research is supported by a partnership grant from the Social Sciences and Humanities Research Council of Canada (grant no. 895-2013-1021) for the Canadian Disability Participation Project (www.cdpp.ca). KAMG holds the Reichwald Family UBC Southern Medical Program Chair in Preventive Medicine.
Author information
Authors and Affiliations
Contributions
SVCL was responsible for designing the review protocol, conducting the search, screening potentially eligible studies, extracting and analyzing data, interpreting results, creating tables, and writing the report. KRT was responsible for designing the review protocol, screening potentially eligible studies, interpreting results, and providing feedback on the report. RBS was responsible for designing the review protocol, arbitrating potentially eligible studies, extracting data, interpreting results, and providing feedback on the report. KAMG was responsible for designing the review protocol, arbitrating potentially eligible studies, interpreting results, and providing feedback on the report.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lawrason, S.C., Todd, K.R., Shaw, R.B. et al. Physical activity among individuals with spinal cord injury who ambulate: a systematic scoping review. Spinal Cord 58, 735–745 (2020). https://doi.org/10.1038/s41393-020-0460-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-0460-4