Abstract
Study design
Cross-sectional survey.
Objectives
To evaluate the annual influenza vaccination coverage rate (IVCR) among community-dwelling individuals with spinal cord injury (SCI).
Setting
SCI community in Switzerland.
Methods
Participants were responders to the influenza vaccination question (n = 492) in the 2012 community survey of the Swiss Spinal Cord Injury (SwiSCI) cohort study. IVCR of SwiSCI participants were compared to the normative Swiss population, sampled in the Swiss Health Survey of 2012 using direct standardization, logistic regression standardization, and a genetic matching approach to control for differences in age, sex, and quarterly period of survey response.
Results
Individuals with SCI showed higher crude (26%, 95% confidence interval (CI): 22–30%) and age- and sex-standardized (24%, CI: 23–24%) IVCR than observed in the general population (15% CI, 14–15%). The adjustment for age and sex as well as quarterly period of survey response showed that the standardized IVCR of individuals with SCI (17%; CI: 12–23%) approached that of the general population. Low IVCR of about 10% were found among individuals with SCI younger than 45 years. IVCR were similar between men and women and between individuals with incomplete and complete paraplegia and tetraplegia.
Conclusion
The IVCR in individuals with chronic SCI was not higher than in the general population and much lower than guidelines recommend. The improvement of the IVCR is an important target of health policy in SCI in Switzerland as to reduce the evidenced excess burden in respiratory-disease related morbidity and mortality.
Similar content being viewed by others
Introduction
Influenza and pneumonia are among the main causes of death in individuals with spinal cord injury (SCI) [1,2,3] leading to increased mortality rates of up to 37-fold [4]. Individuals with traumatic SCI in Switzerland who survived at least one year after injury have a more than 4 times higher risk of dying from respiratory infections than the general population [5]. The risk of dying from influenza-related complications is increased due to impaired cough and less effective clearance of secretions, weak respiratory muscles, autonomic changes, including bronchoconstriction, and decreased overall mobility [6]. This is especially the case for individuals with tetraplegia and complete lesions who are at a particularly high risk of dying from respiratory infection-related complications [5].
A growing number of studies provide strong evidence that influenza vaccination reduces the risk of acquiring influenza or lessens the severity of the illness if the vaccine strains are identical or similar to the currently circulating influenza virus strains [7,8,9]. Therefore, death due to influenza-related complications is potentially preventable through vaccination. Individuals with SCI have shown to mount an appropriate antibody response to the inactivated influenza vaccine that is comparable to that of able-bodied individuals [10]. Thus, individuals with SCI would be expected to benefit equally from the influenza vaccination.
In line with the European Centre for Disease Prevention and Control [11] and similarly to the Advisory Committee on Immunization Practices of the United States (CDC) [12], the Swiss Federal Office of Public Health recommends the influenza vaccination for individuals aged 65 and older and among others to individuals with diabetes, and neurological, pulmonary, or cardiovascular disorders [13]. The CDC explicitly recommends the influenza vaccination for individuals with SCI [14]. The follow-up care guidelines of the Consortium for Spinal Cord Medicine, the SCI center Craig, and the Swiss SCI centers recommend the influenza vaccination to all individuals with SCI [15,16,17]. The guidelines of Craig and the Swiss SCI centers further recommend the influenza vaccination especially to those with injuries at T8 and higher [16] and to those with comorbidities [15].
The overall objective of this study was to evaluate the influenza vaccination coverage rate (IVCR) among community-dwelling individuals living with SCI in Switzerland, a country in which influenza vaccination is recommended by public health authorities to all individuals with SCI. In this paper we compare the IVCR of individuals with SCI to that of the general population in order to determine whether the healthcare system is sufficiently responding to the special needs of individuals with SCI. We further aim to identify possible predictors of influenza vaccination underuse by examining IVCR stratified by socio-demographic and medical factors. To the best of our knowledge, this is the first study to determine IVCR in a representative sample of individuals with chronic SCI living in the community.
Methods
Survey sample and data preparation in SCI
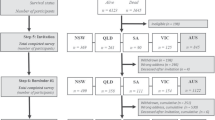
The study sample (n = 492) was derived from the first community survey of the nationwide Swiss Spinal Cord Injury (SwiSCI) Cohort Study [18]. The survey was conducted between late 2011 and early 2013 based on registries from the national association for individuals with SCI, three specialized SCI-rehabilitation centers, and a SCI-specific homecare institution. Eligible were individuals living in Switzerland, with traumatic or on-traumatic SCI aged 16 years or older. Questionnaires were distributed in three consecutive modules, with the question about influenza vaccination being part of the third module that received an overall, cumulative response rate of 43% with moderate response bias [19]. Participants of the third module were on average 3 years older than respondents to the initial survey module [18]. The influenza vaccination status was assessed by asking the participants “when have you had your last influenza vaccination”. Possible answers were “in the past 12 months”, “1 to 2 years ago”, “longer than 2 years ago”, and “never”. Participants who did not provide their vaccination status (n = 9) were coded as”never”. Age categories were created in consideration of recommendations given by Biering-Sørensen et al. [20] whereas the age categories 45–59, 60–74 and 75 + years were changed to 45–64 and to 65 + years in order to account for age-related influenza vaccination recommendations made by the Swiss Federal Office of Public Health [13]. Lesion severity was categorized into complete paraplegia, incomplete paraplegia, complete tetraplegia, and incomplete tetraplegia. Respiratory and cardiovascular disorders as well as diabetes were self-reported and coded as existent when present in the three months prior to answering the survey.
Survey sample and data preparation in the general population
IVCR of SwiSCI participants were compared to the normative Swiss population, sampled in the Swiss Health Survey (SHS) of 2012 [21]. The SHS surveyed basic information on the health state, health behavior, and health service use in a random sample of 21,597 individuals (0.27% of the Swiss population). The influenza vaccination status was assessed in 18,357 participants by asking “Have you ever had an influenza vaccination? If yes, please indicate the month and year of your last influenza vaccination”. In order to create a vaccination status that is equivalent to that of the SwiSCI survey, we calculated the time interval between the influenza vaccination and the date when participants answered the survey. Respiratory and cardiovascular disorders as well as diabetes were coded according to a recent study by Zürcher et al. who estimated IVCR in the general population based on SHS data [22]. Diabetes was defined by the use of any diabetic drug, cardiovascular disorders by the use of any heart medication, and pulmonary disorders were recorded as self-reported. Age was categorized into the same groups as the SCI sample. To match the age distribution to the SCI sample, participants younger than 16 years (n = 139) were excluded.
Statistical analysis
Age- and sex-standardized IVCR were calculated using direct standardization. Additional adjustment of IVCRs for the quarterly period of survey response as well as unit non-response [18] was achieved using logistic regression standardization, applying the R package “stdReg” that allows for estimation of standardized probabilities from a fitted regression model [23]. The logistic regression model was fitted with the vaccination status as the dependent variable and age, sex, quarterly period of survey response, and group (SCI or general population) as the independent variables. Survey weights were included in the model for both populations to correct for unit non-response bias [18]. Crude IVCR in SCI were compared across categories of personal characteristics, lesion severity, health conditions, and the quarterly period of survey response to an age- and sex-matched sample of the general population using two-sided Fisher’s exact tests. Every SwiSCI participant was case matched with four SHS participants. Matching was performed using a multivariate genetic search algorithm implemented in the R package Matching [24]. In a supplementary analysis, crude IVCR in SCI were compared to a sample of the general population that was matched based on age, sex, and the exact month and year of survey response. Statistical analyses and data preparation were performed using the R programming language version 3.5.1.
Results
The 492 participants with SCI in the SwiSCI survey were on average older (57 vs. 49 years) than participants of the SHS survey and more likely male (71% vs. 47%) (Table 1). Among participants with SCI, incomplete paraplegia was the most frequent lesion characteristic (39%), followed by complete paraplegia (30%), incomplete tetraplegia (22%), and complete tetraplegia (9%). The median time since SCI onset was 12 years (interquartile range 6–25 years). The occurrence of diabetes and cardiovascular disorders in the last three months were similarly reported by about 10% of study participants with SCI. Respiratory disorders were more frequent and reported by 23% of study participants. More than half of SwiSCI participants answered the survey in the last quarter of the year 2011, whereas response by SHS participants was more equally distributed across all quarters of 2012. The crude, self-reported IVCR in the year prior to the survey was higher in individuals with SCI (26%) than the general population (15%). Likewise, the fraction of individuals who reported ever having had an influenza vaccination was higher in individuals with SCI (49%) than in the general population (33%).
Table 2 compares IVCR of individuals with SCI to IVCR of the age- and sex-matched sample of the general population by personal characteristics, lesion severity, health conditions, and quarterly period of survey response. Overall, individuals with SCI were slightly more often vaccinated against influenza (26, 95% confidence interval (CI): 22–30%) than the individuals of the matched sample of the general population (18%; CI: 16–19%). Similar IVCR were found for men and women with SCI, and across individuals with different lesion severity. IVCR were higher in the elderly and consistently higher in individuals with SCI than in the general population. Individuals with SCI and respiratory disorders were 1.5 times more often vaccinated than those from the general population with respiratory disorders. IVCR of individuals with cardiovascular disorders or diabetes were similar between the two populations. SwiSCI and SHS study participants were about equally often vaccinated when they answered the surveys in the first three quarters of the year 2012 whereas SwiSCI participants who answered the survey in the last quarter of 2011 were more often vaccinated and SHS participants who answered the survey in the fourth quarter of 2012 were less often vaccinated.
The crude (26%, CI: 22–30%) and age and sex- standardized (24% CI: 23–24%) estimates of IVCRs in individuals with SCI were higher than in the general population (15% CI, 14–15%). When adjusting for age, sex, the quarterly period of survey response, and when including survey weights, the standardized IVCR of individuals with SCI (17%; CI: 12–23%) approached that of the general population. A sensitivity analysis that used a matching approach to control for differences in age, sex and month and year of survey response between the SCI and general populations confirmed the similarity of IVCR rates (Tables S1 and S2).
Discussion
The crude IVCR of individuals with SCI in Switzerland (26%) was higher than that of the general population (15%). However, the adjusted analysis suggested that the difference is essentially explained by differences in age structures and survey period between the survey in SCI and the general population. IVCR were highest in individuals aged 65 years or older, and in those with diabetes, cardiovascular and respiratory disorders, but did not exceed 50%. Low IVCR of about 10% were found among individuals with SCI younger than 45 years. IVCR were similar between men and women and between groups with different lesion severity.
There is a remarkably scant evidence-base regarding IVCR in community-dwelling individuals with SCI. Most evidence comes from studies that investigated interventions to increase influenza vaccination rates in veterans with SCI in the United States [25, 26]. Weaver et al. reported IVCR in veterans aged 65 years or older of 34% [25]. This is lower than the 42% that we report for our study population with SCI aged 65 years or older. A Canadian survey among physicians in the family practice found that 33 of 60 (55%) patients with SCI had been vaccinated against influenza [27]. The median time since influenza vaccination of these patients with an average age of 52 years was 19 months. This finding is therefore not directly comparable to the annual IVCR reported in this study, but it is similar to the proportion of individuals with SCI in our study who reported having ever had an influenza vaccination (49%).
The comparably low IVCR rate in individuals with SCI is surprising, given that national and international guidelines recommend the influenza vaccination for individuals with neurological impairments, or for individuals with SCI specifically. IVCRs were for instance considerably below the coverage rate of 75% that is recommended by influenza vaccination guidelines issued by the European Centre for Disease Prevention and Control for individuals older than 65 years and other risk groups [11]. Particularly unexpected were the low IVCR in individuals with SCI and concomitant risk factors for influenza–related complications. Only 33% of individuals with complete tetraplegia, 37% with respiratory disorders, 48% with cardiovascular disorders, and 37% with diabetes were vaccinated against influenza. In accordance with guideline recommendations for the general population, individuals with SCI aged 65 years and older were more likely vaccinated than their younger counterparts. Similarly, those with cardiovascular disorders or diabetes were more often vaccinated than those without these health conditions. However, when compared to the general population with the same age or with the same health conditions, we found that IVCR were not markedly elevated in individuals with SCI. This suggests that influenza vaccination recommendations were partly followed with respect to conditions that are common in the general population, but guideline recommendations related to the neurological impairments of individuals with SCI seem to be insufficiently considered.
Physicians should be encouraged to recommend the influenza vaccination to individuals with SCI given the low IVCR in these individuals and the high influenza-related mortality [5]. Weaver et al. showed that it is possible to increase IVCR using patient reminder letters and education, provider reminders, and computerized clinical reminders. They were able to increase annual IVCR from 34 to 67% in veterans with SCI treated at 23 veterans SCI centers [25]. A similar intervention to increase IVCR in the community-dwelling individuals with chronic SCI of this study would likely require an involvement of general practitioners as they visit specialized centers less frequently than the US veterans and rely more often on general practitioner services [28,29,30]. The authors of the Canadian survey among physicians in family practices concluded that it would be relatively easy to increase influenza vaccination uptake in individuals with SCI with high potential gains, particularly as all responding physicians reported comfort with providing vaccinations [27].
This study was subject to several limitations. First, SwiSCI and SHS participants answered the surveys at different time points. A majority of SwiSCI participants answered the survey in the fourth quarter of the year 2011, whereas all SHS participants answered the survey in the year 2012. A significant portion of the SwiSCI respondents were therefore reporting on the influenza season 2010/11 whereas all SHS respondents reported on the season 2011/12. The influenza season 2010/11 was of moderate severity and the influenza vaccination was considered effective whereas the season 2011/12 was of mild severity and the influenza vaccination was considered only partly effective [31]. It is therefore possible that crude IVCR in individuals with SCI were overestimated as compared to the general population. To account for this problem, we adjusted in the logistic regression standardization for the quarter of the year when the survey was answered. Second, the data was recorded in the year 2012 and might be therefore considered outdated. However, there is strong evidence that the situation has not changed in more recent years. When dividing the sold vaccination doses by the Swiss population size, the numbers remain mostly constant over the past years (Table S3). Third, the data in both surveys is self-reported and therefore subject to recall bias.
Conclusion
Influenza vaccination rates in individuals living with chronic SCI in Switzerland were not higher than in the general population. This is an unexpected finding, considering that all relevant guidelines recommend the vaccination to individuals with SCI. The improvement of influenza vaccination rates is an important target of health policy in SCI in Switzerland as to reduce the evidenced excess burden in respiratory-disease related morbidity and mortality.
Data archiving
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Frankel HL, Coll JR, Charlifue SW, Whiteneck GG, Gardner BP, Jamous MA, et al. Long-term survival in spinal cord injury: a 50 year investigation. Spinal Cord. 1998;36:266–74.
Leite VF, Souza DR de, Imamura M, Battistella LR. Post-discharge mortality in patients with traumatic spinal cord injury in a Brazilian hospital: a retrospective cohort. Spinal Cord. 2018. https://doi.org/10.1038/s41393-018-0183-y.
Chamberlain JD, Meier S, Mader L, von Groote PM, Brinkhof MWG. Mortality and longevity after a spinal cord injury: systematic review and meta-analysis. Neuroepidemiology. 2015;44:182–98.
DeVivo MJ, Black KJ, Stover SL. Causes of death during the first 12 years after spinal cord injury. Arch Phys Med Rehabil. 1993;74:248–54.
Chamberlain JD, Buzzell A, Gmünder HP, Hug K, Jordan X, Moser A, et al. Comparison of all-cause and cause-specific mortality of persons with traumatic spinal cord injuries to the general Swiss population: results from a national cohort study. Neuroepidemiology. 2019;52:205–13.
Whiteneck GG, Jawad MH, Charlifue SW, Charlifue S. Aging with spinal cord injury. New York: Demos Medical Publishing; 1993.
Restivo V, Costantino C, Bono S, Maniglia M, Marchese V, Ventura G, et al. Influenza vaccine effectiveness among high-risk groups: a systematic literature review and meta-analysis of case-control and cohort studies. Hum Vaccin Immunother. 2018;14:724–35.
Osterholm MT, Kelley NS, Sommer A, Belongia EA. Efficacy and effectiveness of influenza vaccines: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:36–44.
Ahmed AH, Nicholson KG, Nguyen-Van-Tam JS. Reduction in mortality associated with influenza vaccine during 1989-90 epidemic. Lancet. 1995;346:591–5.
Trautner BW, Atmar RL, Hulstrom A, Darouiche RO. Inactivated influenza vaccination for people with spinal cord injury. Arch Phys Med Rehabil. 2004;85:1886–9.
Nokleby H, Nicoll A. Risk groups and other target groups—Preliminary ECDC guidance for developing influenza vaccination recommendations for the season 2010-11. Eur Surveill. 2010;15:1–4.
Grohskopf LA, Sokolow LZ, Broder KR, Walter EB, Fry AM, Jernigan DB. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices—United States, 2018–19 influenza season. MMWR Recomm Rep. 2018;67:1–20.
Federal Office of Public Health. Seasonal flu (influenza). 2018. https://www.bag.admin.ch/bag/en/home/krankheiten/krankheiten-im-ueberblick/grippe.html.
Budd A, Blanton L, Grohskopf L, Campbell A, Dugan V, David; et al. Surveillance Manual—Chapter 6: Influenza. https://www.cdc.gov/vaccines/pubs/surv-manual/chpt06-influenza.pdf. Accessed 27 Feb 2019.
Spreyermann R, Lüthi HJ, Michel F, Baumberger M, Curt A, Wirz M, et al. Vorsorge und Nachsorge II, Gesundheitscoaching bei querschnittgelähmten Patientinnen und Patienten. Ludwig‐guttmann‐pr der DMGP; 2013.
Hosack K. Spinal cord injury re-evaluations and follow-up care made in initial rehabilitation. Englewood, Colorado 2014. https://craighospital.org/uploads/CraigHospital.ReevaluationWhitepaper_2014.pdf. Accessed 20 Mar 2019.
Cosortium for Spinal Cord Medicine. Respiratory management following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2005;28:259–93.
Brinkhof MWG, Fekete C, Chamberlain JD, Post MWM, Gemperli A. Swiss national community survey of functioning after spinal cord injury: protocol, characteristics of participants and determinants of non-response. J Rehabil Med. 2016;48:120–30.
Fekete C, Segerer W, Gemperli A, Brinkhof MWG. Participation rates, response bias and response behaviours in the community survey of the Swiss Spinal Cord Injury Cohort Study (SwiSCI). Bmc Med Res Methodol. 2015;15:80.
Biering-Sørensen F, DeVivo MJ, Charlifue S, Chen Y, New PW, Noonan V, et al. International spinal cord injury core data set (version 2.0)—including standardization of reporting. Spinal Cord. 2017;55:759–64.
Swiss Federal Office of Statistics. Swiss Health Survey 2012. Berne: Swiss Federal Office of Statistics; 2013.
Zürcher K, Zwahlen M, Berlin C, Egger M, Fenner L, Berlin C et al. Trends in influenza vaccination uptake in Switzerland: Swiss Health Survey 2007 and 2012. Swiss Med Wkly. 2019;149: 4–11.
Sjölander A. Regression standardization with the R package stdReg. Eur J Epidemiol. 2016;31:563–74.
Sekhon JS. Multivariate and propensity score matching software with automated balance optimization: the matching package for R. Social Science Research Network: Rochester, NY; 2008.
Weaver FM, Smith B, LaVela S, Wallace C, Evans CT, Hammond M, et al. Interventions to increase influenza vaccination rates in veterans with spinal cord injuries and disorders. J Spinal Cord Med. 2007;30:10–19.
Goldstein B, Miskevics S, Etingen B, LaVela S, Weaver F, Goldstein B, et al. Factors associated with H1N1 influenza vaccine receipt in a high-risk population during the 2009–2010 H1N1 influenza pandemic. Top Spinal Cord Inj Rehabil 2012;18:306–14.
Lofters A, Chaudhry M, Slater M, Schuler A, Milligan J, Lee J et al. Preventive care among primary care patients living with spinal cord injury. J Spinal Cord Med. 2018. https://doi.org/10.1080/10790268.2018.1432308 [Epub ahead of print].
Ronca E, Scheel-Sailer A, Koch HG, Gemperli A. Health care utilization in persons with spinal cord injury: Part 2 - determinants, geographic variation and comparison with the general population. Spinal Cord. 2017. https://doi.org/10.1038/sc.2017.38.
St. Andre J, Smith B, Stroupe K, Burns S, Evans C, Ripley D, et al. A comparison of costs and health care utilization for veterans with traumatic and nontraumatic spinal cord injury. Top Spinal Cord Inj Rehabil. 2011;16:27–42.
Ronca E, Scheel-Sailer A, Koch HG, Metzger S, Gemperli A. Inpatient migration patterns in persons with spinal cord injury: A registry study with hospital discharge data. SSM Popul Heal. 2016. https://doi.org/10.1016/j.ssmph.2016.04.004.
Swiss Federal Office of Statistics. Seasonal influenza reports. https://www.sentinella.ch/de/publications/. Accessed 19 Mar 2019.
Acknowledgements
We are grateful to all the participants of the SwiSCI and SHS surveys for their time and effort spent in responding to the questions. This study has been financed in the framework of the SwiSCI study, supported by the Swiss Paraplegic Foundation.
Members of the SwiSCI Steering Committee
Xavier Jordan4, Bertrand Léger4, Michael Baumberger5, Hans Peter Gmünder5, Armin Curt6, Martin Schubert6, Margret Hund-Georgiadis7, Kerstin Hug7, Thomas Troger8, Daniel Joggi9, Hardy Landolt10, Nadja Münzel11, Mirjam Brach1, Gerold Stucki1, Christine Fekete12,
Funding
All authors were salaried by organizations financially compensated by the Swiss Paraplegic Foundation.
Author information
Authors and Affiliations
Consortia
Contributions
ER and MM were responsible for data analysis. ER and MB were responsible for research design. ER, MM, and MB were responsible for introduction, methods, results, discussion, and conclusion sections.
Corresponding author
Ethics declarations
Statement of ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. All SwiSCI participants signed a written consent form before completing the survey. The study was approved by the ethics committee of northwest/central Switzerland. Data of the SHS were anonymized before analysis. The permission to analyze and publish the data was obtained through a contract with the Swiss Federal Office of Statistics.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ronca, E., Miller, M., Brinkhof, M.W.G. et al. Poor adherence to influenza vaccination guidelines in spinal cord injury: results from a community-based survey in Switzerland. Spinal Cord 58, 18–24 (2020). https://doi.org/10.1038/s41393-019-0333-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-019-0333-x