Abstract
Study design
Retrospective chart audit.
Objectives
The National Early Warning Score (NEWS) is based on seven physiological parameters which can be altered in some individuals with spinal cord injuries (SCI). The aim was to start the development of adapted NEWS suitable for SCI population. The objective was to determine the SBP NEWS specificity based on neurological level of injury (NLI) and completeness of injury.
Setting
Tertiary centre in the UK.
Methods
Adult patients admitted for the first time to the National Spinal Injuries Centre between 1 January 2015 and 31 December 2016 were included if they were >6 months post injury. Data were extracted retrospectively including the last ten consecutive BP and heart rate readings before discharge. Data were analysed based on different AIS grades, completeness of injury and NLI.
Results
One hundred and ninety one patients were admitted in 2015 and 2016 and 142 patients were included in the primary analysis. The mean SBP ranged between 92 and 151 mmHg. Patients with the NLI of T6 and above (≥T6) motor complete lesions had a significantly lower SBP than motor incomplete lesions. The specificity of the SBP NEWS was 35.3% in ≥T6 motor complete individuals versus 80.3% in ≥T6 motor incomplete individuals.
Conclusion
The baseline BP is significantly lower in the ≥T6 motor complete SCI individuals (>6 months post injury) resulting in a very low specificity of 35.3% to SBP NEWS, which could lead to mismatch between clinical deterioration and NEWS resulting in lack of timely clinical response.
Similar content being viewed by others
Introduction
The level and degree of injury directly results in disruptions of cardiovascular control in spinal cord injuries (SCI) population [1]. As a result, some SCI result in altered parameters in respect of vital signs. The most notable change in baseline vital signs is an immediate drop in systolic blood pressure (SBP) following high SCI as a result of neurogenic shock. However, following the acute stage, there is a group of patients that continues to suffer from cardiovascular dysfunction. A meta-analysis [2] showed that the higher the neurological level of injury (NLI), the greater the degree of cardiovascular dysfunction. Individuals with lesions to the cervical cord have been reported to have a 15 mmHg lower resting SBP in a seated compared with supine position [2]. This can be explained by disruption of descending input to the sympathetic preganglionic neurones that results in loss of the splanchnic blood vessels tone, which leads to long lasting hypotension post injury [3, 4].
A systematic review of the SCI literature [5] suggests that there is no clear consensus that resting BP differs between neurologically complete and incomplete patients. However, as the descending vasomotor pathways are anatomically located adjacent and dorsolateral to the lateral descending motor corticospinal tract [6], it is not unreasonable to hypothesise that neurological completeness of injury may be related to cardiovascular dysfunction [6].
Several studies [7,8,9,10,11,12,13,14,15] reported results of daytime baseline BP. Some of them reported low baseline SBP (~110 mmHg) mainly in individuals with motor complete tetraplegia [8, 9], whereas others [13, 15] reported low baseline SBP (~103 mmHg, 111 mmHg) in individuals with motor complete and incomplete tetraplegia. Another study [14] reported low baseline SBP (~109 mmHg) for C4–T12 motor complete injuries. To the contrary, two studies [7, 10] reported a higher SBP of ~118 mmHg in individuals with incomplete tetraplegia, whereas another study [11] reported even a higher SBP of ~124 mmHg in individuals with complete tetraplegia. One study [15] reported a supine SBP of 113 mmHg in autonomically complete SCI compared with supine SBP of 128 mmHg in autonomically incomplete SCI.
An important implication of cardiovascular dysfunction is in recognising and responding to a deteriorating in-patient. In the United Kingdom, the Royal College of Physicians (RCP) National Early Warning Score (NEWS) [16] has been adopted across the National Health Service (NHS) to identify early clinical deterioration in a patient. The NEWS scoring system is based on seven physiological parameters; respiratory rate, oxygen saturation, oxygen use, SBP, pulse rate, level of consciousness and body temperature. A score is allocated to each parameter, with zero assigned to a normal value and deviation triggering scores of 1–3 for each parameter. Scores are then added, and a combined NEWS score of 5 or more requires an urgent medical response. Whilst the system has been found to be effective and is a recommended surveillance system for all patients in hospitals [16], it is recognised that the NEWS may be unreliable in SCI, especially patients with tetraplegia or high paraplegia. Disruption of the autonomic nervous system and resulting fluctuations in pulse rate, temperature or blood pressure BP may lead to a low sensitivity of the NEWS [16]. Indeed Asafu-Adjaye and Gall [17] flagged a low sensitivity of NEWS in patients with tetraplegia and paraplegia, as well as low specificity in patients with tetraplegia. However, their study did not stratify injuries based on NLI or neurological completeness of injury. Despite clear advocacy for the use of a standard system for assessing and responding to acute illness [16], there is no evidence to form the basis for bespoke and valid guidance in the management of patients with SCI with different lesions in acute and ambulance settings.
This retrospective cohort study of patients with SCI was thus conducted to determine the SBP NEWS specificity based on NLI and completeness of injury and subsequently lay down the foundations for development of adapted NEWS suitable for this population.
Methods
Participants and experimental design
Patients with an SCI, admitted for the first time to the National Spinal Injuries Centre (NSIC) between 1 January 2015 and 31 December 2016, were eligible if they were adults (≥18 years) and >6 months from injury. Patients were excluded if they (a) were deemed to be clinically unwell by their treating doctor, or (b) died during their admission, or (c) were not yet discharged at the time of the study, or (d) did not have discharge NLI or AIS grade available, or (e) did not have observation charts available. This study was preliminary a retrospective chart audit therefore a priori sample size estimation was not performed and the number of cases during the study period determined the sample size. Due to the study’s retrospective nature, the clinical observations and determinations of NLI and AIS grade were made without being influenced by the study; in this manner observer bias was minimised. Data extracted were observed by two clinicians in an attempt to reduce investigator bias.
Data sources
This study used electronic medical records—Irish Medical Systems (IMS) and Evolve—of the NSIC, a tertiary specialist centre with a capacity of 103 SCI beds. IMS contains both clinical notes and neurological examination findings. Evolve contains all paper documents including NEWS observation charts, discharge summaries and International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) charts [18]. Using the unique NHS number of each patient, these data were cross referenced with clinical observation records stored in Evolve. The STROBE statement and checklist were used, plus RECORD extension was considered to guide study reporting.
Demographic data obtained from the NSIC coding department included NHS numbers, date of birth, age, sex, date of injury, admission and discharge dates. Ideally, neurological examination using the ISNCSCI chart is conducted for all patients on admission and prior to discharge and stored on IMS and Evolve. Admission and discharge NLI and AIS grades were obtained from ISNCSCI charts and discharge summaries. Data were extracted on confounding factors such as the number of patients on antihypertensive, antiarrhythmic or medications with known hypotensive effects.
Blood pressure recordings
Cardiovascular function was determined using NEWS chart developed by the RCP. The NEWS2 chart is the latest version approved in 2017 with no changes to the SBP NEWS chart (Fig. 1). These charts had been completed during admission by either nurses or health care assistants. BP observations were obtained from the patient in a supine position using the Mindray (Shanghai, China) automated sphygmomanometer (portable and fixed) and the portable Welch Allyn (New York, USA) automated sphygmomanometer. These observations were obtained at least twice per day (morning and evening prior to sleep) in the NSIC during routine practice on each of the four different adult wards. The last ten BP and pulse rate observations prior to discharge were obtained from Evolve. These BP readings were taken over a period of 5–7 days as at times there were missed readings on particular days as many individuals spend 1–2 days out of the NSIC during weekends.
Statistical analysis
All data were analysed using the Statistical Package for Social Sciences (version 25; SPSS Chicago, IL). Normality and homogeneity of variance were confirmed by the Shapiro–Wilk and Levene’s test, respectively, where appropriate. Mean BP and co-efficient of variation for the last ten BP observations before discharge were calculated for each individual and used in subsequent analysis. Individuals were further assigned the NEWS that related to their mean SBP. A score of zero assigned to a normal value and deviation from the normal value triggering scores of 1–3. For data analysis, patients were assigned as triggering either a (1) normal value (NEWS of 0) or (2) a deviation from normal (NEWS 1 or 2). Specificity refers to the percentage of patients who were correctly diagnosed using SBP NEWS as not triggering because of their mean SBP reading, i.e. triggering SBP NEWS 0.
For the main analysis, groups were formed according to AIS grades (A–D), motor complete (AIS A and B) and motor incomplete (AIS C and D). A sub-analysis was performed considering level of injury (≥T6) and motor index score (MIS) (0–25, 26–50, 51–100). The MIS is the sum of all key muscles motor scores. These bands of MIS were chosen based on clinical hypothesis that (a) MIS 0–25 would include a majority of patients with motor complete tetraplegia, (b) MIS 26–50 would include a mixture of patients with motor incomplete tetraplegia and motor complete paraplegia, and (c) MIS 51–100 would include a majority of patients with motor incomplete tetraplegia and paraplegia. Between group differences were determined using a one way ANOVA with post hoc analysis conducted using pairwise comparisons with a Bonferroni correction for continuous data and chi-squared tests (Χ2) from the cross tabs procedure for NEWS score categorical data. Significance was accepted at an alpha of 0.05.
Results
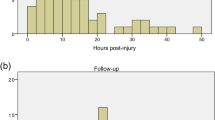
The total number of new admissions to the NSIC in the calendar years of 2015 and 2016 was 191. Figure 2 shows of the 191 new admissions, 142 patients, who had complete data, were included in analysis. Most of the 142 patients (n = 135) were admitted for specialist rehabilitation <1 year post injury with a mean of 85 days (range 6–297 days). Only three patients were admitted between 1 and 3 years and four were admitted >3 years post injury for fixed admission to address specific rehabilitation goals.
Systolic blood pressure
The total number of SBP readings analysed was 1420 and the mean SBP ranged from 92 to 151 mmHg. Demographic data of the 142 patients included in the primary analysis are displayed in Table 1.
ASIA Impairment Scale
Co-efficient of variation showed intra-individual variability was low (SBP mean: CoV 0.09 ± 0.04 mmHg) demonstrating patient BP was stable over the ten observations. ANOVA revealed a significant difference in SBP between AIS grades, with SBP lower in AIS A than AIS C (p = 0.03) and AIS B lower than AIS C (p = 0.001) and AIS D (p = 0.003). The AIS grade of a patient had a significant effect on their SBP triggering of NEWS score, when analysed using a patient’s AIS grade (Χ2 = 25.47, p < 0.001) or according to the motor completeness of their injury (Χ2 = 23.55, p < 0.001). 59.1% of patients with a motor complete injury (AIS A & B) triggered a NEWS score (1 or 2) compared with 18.4% of those with motor incomplete injuries (AIS C & D). Therefore, the specificity of the SBP NEWS was 40.9% in the motor complete group compared with 81.6% in the motor incomplete group. Comparison of the mean SBP, diastolic BP (DBP) and mean arterial pressure (MAP) of different AIS groups is shown in Table 1. The difference in the NEWS specificity between the motor complete group and motor incomplete group is clinically relevant and significant.
Neurological level of injury and motor completeness
ANOVA showed SBP was lower in the group of patients with NLI ≥ T6 (n = 98, 117 ± 12 mmHg) compared with those with NLI < T6 (n = 44, 123 ± 14, p = 0.07). ANOVA also showed in the group of patients with the NLI ≥ T6, the motor complete patients (n = 34, 111 ± 12 mmHg) had a significantly lower SBP than motor incomplete patients (n = 64, 120 ± 12 mmHg, p = 0.001). Furthermore, there was no significant difference in the mean SBP of tetraplegia (C1–C8) individuals (111 mmHg) when compared with high paraplegia (T1–T6) individuals (109 mmHg) in those who were ≥T6 motor complete injuries. For patients with NLI ≥ T6, motor completeness had a significant effect on a patient’s NEWS (Χ2 = 19.06, p < 0.001). 64.7% of ≥T6 motor complete patients (62.5% in tetraplegia group and 70% in high paraplegia group) triggered NEWS of 1 or 2 compared with 19.7% of the ≥T6 motor incomplete. As a result, the specificity of the SBP NEWS was 35.3% in ≥T6 motor complete patients (37.5% in tetraplegia group and 30% in high paraplegia group) and 80.3% in ≥T6 motor incomplete patients. The difference in NEWS specificity based on NLI (≥T6 versus <T6) stratification and motor complete versus motor incomplete injuries is the most meaningful and clinically significant finding that conforms with our clinical findings since the introduction of the NEWS by the RCP in 2012.
Motor Index Score (sum of all key muscles motor scores)
Out of the 142 patients, 83 patients had discharge MIS available, including 55 with NLI ≥ T6 and 28 with NLI < T6. The mean MIS was 33 in ≥T6 motor complete compared with 64 in ≥T6 motor incomplete individuals. In comparison, the mean MIS was 59 in <T6 motor complete compared with 83 in <T6 motor incomplete individuals. The majority (89%) of individuals with MIS (0–25) had motor complete tetraplegia, whereas, the majority (81%) of individuals with MIS (51–100) had motor incomplete tetraplegia. Further details of numbers of individuals and mean MIS in each AIS group is detailed in Table 2.
In the NLI of T6 and above group (n = 55 patients), the SBP tended to be lower in patients with a MIS (0–25) (108 ± 12 mmHg) compared with MIS (26–50) (116 ± 13 mmHg) and MIS (51–100) (120 ± 11 mmHg), though this did not reach significance on ANOVA (p = 0.08). A patient’s MIS score had a significant effect on their NEWS (Χ2 = 11.58, p = 0.003). Out of the 55 patients that had a discharge MIS, 67.3% had a NEWS of 0. Sixty two percent of patients with NEWS 0 had a MIS of (51–100), whereas 50.0% of patients with NEWS 1 or 2 had MIS (26–50). Within the MIS (0–25) group, 83.3% triggered NEWS 1 or 2, whilst 85.2% of the MIS (51–100) group had NEWS of 0 (Table 2). The differences in SBP and percentage of NEWS trigger based on MIS bands emphasise the clinical relevance of difference based on motor completeness noted in the previous sections.
National Early Warning Score (NEWS) and hypothetical systolic BP spinal cord injury-NEWS
From our data, we have noticed that by dropping the lower normal SBP in the NEWS chart from 111 mmHg to 101 mmHg, the mean SBP of the majority of individuals with ≥T6 motor complete lesions would move from NEWS score of 1 to a NEWS score 0 (Fig. 3).
In order to have a more accurate, reflective and specific SBP NEWS chart that helps to better identify the risk of clinical deterioration with timely intervention for ≥T6 motor complete patients specifically, we propose a new Spinal Cord Injury SBP NEWS (SCI-NEWS) chart (Fig. 4). This new chart was synthesised by adapting the current SBP NEWS chart by introducing two new cut-offs for the lowest (101 mmHg) and the highest (149 mmHg) normal SBP. The new lowest normal SBP was based on the improvement of specificity as shown in Fig. 3. The new highest normal was based on the recommended SBP of 150 mmHg as guidance for introduction of medical treatment of autonomic dysreflexia. The SBP SCI-NEWS chart would generate similar trigger scores (0, 1, 2, and 3), which are added to the six other parameters (respiratory rate, O2 saturation, O2 supply, pulse rate, consciousness and temperature) scores to generate the NEWS aggregate. This is then assessed with the same NEWS thresholds and triggers, which will be applicable to assess clinical risk and response (Table 3). Application of the SCI-NEWS systolic BP monitoring chart on the mean SBP readings of our cohort improved the specificity from 35 to 82% (from 38 to 79% in tetraplegia group and from 30 to 90% in high paraplegia group). Comparison between the SBP NEWS and SBP-SCI NEWS scoring systems is given in Table 4.
Pulse rate
A total of 1420 pulse rate readings (last 10 readings for each patient) were analysed. ANOVA showed no significant differences noted between motor complete and motor incomplete individuals in the ≥T6 lesions or those <T6. In the group of ≥T6 lesions, the mean pulse rate was 72 beats/min (71 beats/min in tetraplegia versus 75 in high paraplegia) in motor complete individuals compared with 74 beat/min (73 beats/min tetraplegia versus 79 beats /min in high paraplegia) in motor incomplete individuals. Whereas, in the group of <T6 lesions, the mean pulse rate was 76 beats/min in motor complete individuals compared with 78 beats/min in motor incomplete individuals. These results showed no clinical significance or meaning as none of these readings would trigger any NEWS score.
Discussion
The results of this study confirm that altered cardiovascular function results in lower BP in some patients with an SCI. To our knowledge, this is the first large scale study to provide preliminary data describing typical BP responses reporting on how this affects the NEWS based on SBP whilst being clinically well. Our findings suggest that the ≥T6 motor complete lesions have lower baseline SBP, and subsequently lower NEWS specificity compared with the ≥T6 motor incomplete lesions.
Common causes of low SBP in individuals with SCI include orthostatic hypotension, dehydration and sepsis. However, our data and that of others [2, 19] suggest that some individuals with an SCI have low baseline SBP when they are well. Autonomic dysreflexia is an emergency autonomic condition due to sympathetic hyperactivity resulting in increasing severe hypertension typically in ≥T6 patients. It happens more commonly, but not exclusively, in patients who are motor complete usually as a result of a trigger below the patient’s NLI. Common triggers include bladder and bowel distention. A sudden increase of 20–40 mmHg in BP above the baseline may be a sign of autonomic dysreflexia [20] and requires treatment, if the SBP exceeds 150 mmHg.
The present study’s findings may have important implications for detecting and responding to deteriorating patients with SCI. The RCP’s NEWS score [16] has shown to be proficient at discriminating risk of serious clinical deterioration and acute mortality as one of the best existing systems and better than most [21]. The only paper that has discussed the relationship of the current NEWS and patients with SCI was a letter [17] to the RCP reporting an audit conducted in the London Spinal Injuries Centre. In their audit of NEWS records from 100 patients, the authors [17] studied the sensitivity (the ability of NEWS to trigger urgent clinical reviews for unwell patients i.e. score of ≥5) and the specificity of the NEWS (the ability of NEWS not to trigger urgent clinical reviews for well patients i.e. score of ≤4). Forty-nine patients with tetraplegia and 51 patients with paraplegia were included with a sensitivity of 63% for patients with tetraplegia compared with 35% for patients with paraplegia and a specificity of 37% for patients with tetraplegia compared with 100% for paraplegia. The NEWS missed 37% of unwell patients with tetraplegia, whose main pathology was autonomic dysreflexia and surprisingly it also missed 65% of unwell patients with paraplegia, which included cases of pulmonary embolism and viral illness. Their results were skewed by the lack of stratification using NLI and AIS grades. In comparison, our study showed a specificity of 35.3% in ≥T6 motor complete patients.
Further analysis, albeit using the available MIS data (55 patients), emphasised the significant association between the motor function and NEWS score as 67.3% with MIS score did not trigger NEWS (i.e. NEWS 0). In addition to that, 83.3% of those with low MIS (0–25) were motor complete and the majority of that group (83.3%) triggered NEWS 1 or 2. On the other hand 100% of those with high MIS (51–100) were motor incomplete patients and the majority of that group (85.2%) did not trigger NEWS (i.e. NEWS 0). These results confirm that the current SBP NEWS chart may not be reliable for ≥T6 motor complete patients with 35.3% NEWS specificity. This would certainly affect the overall cumulative NEWS score, consequently affecting the patients at risk of clinical deterioration and the facilitation of timely and effective response. Therefore, our study has identified the ≥T6 motor complete patients as a group of largest concern using the current NEWS. To the contrary, the NEWS has a high specificity of around 81% in motor incomplete patients, which suggests that it is possibly valid to use in this group of patients. The mean SBP for the majority (92%) of our patients was between 101 and 149 mmHg and the maximum recorded was 151 mmHg. Treatment of autonomic dysreflexia using anti-hypertensive medication is widely recommended for high SBP of 150 mmHg and above [20]. Based on our study results, 64.7% of ≥T6 motor complete patients triggered SBP NEWS score, when they were well with only 35.3% specificity. Therefore, we proposed a hypothetical SBP SCI-NEWS as detailed in the ‘Results’ section.
The effect of SCI on cardiovascular function is best understood in the acute setting. Tuli et al. [22] demonstrated higher SBP and heart rate in motor incomplete patients following acute cervical cord injury, and showed greater incidence of neurogenic shock in motor complete compared with motor incomplete patients. In addition, studies have shown a greater prevalence of persistent bradycardia and hypotension in motor complete injuries [19, 23]. Our results of low baseline SBP (111 mmHg) in ≥T6 motor complete lesions are similar to other reports in the literature [8, 9] that reported low baseline SBP (~110 mmHg) in individuals with motor complete tetraplegia. Although, we did not have data on autonomical completeness of injury, our results are also comparable to the study [15] that reported a supine SBP of 113 mmHg in autonomically complete SCI. In contrast, our results showed a lower baseline SBP to the one (~124 mmHg) reported by Frisbie et al. [11] in individuals with complete tetraplegia. Even when our SBP data of the ≥T6 motor complete lesions were split into tetraplegia (C1–C8) and high paraplegia (T1–T6), the baseline SBP was still low averaging 111 and 109 mmHg, successively. These results were contrary to those of Rosado-Rivera et al. [12] and of Goh et al. [14] that showed relatively higher baseline SBP (115 mmHg and 117 mmHg). Similar to other studies [9,10,11,12], our data showed relatively higher baseline SBP (123 mmHg) in the group of low paraplegia (NLI < T6). It is worth empathising that our study population of 142 patients is very large compared with the population of the aforementioned single studies (excluding meta-analysis and systematic review). Whilst there is less evidence in chronic injury, a meta-analysis by West et al. [2] demonstrated that patients with a higher NLI have the lower BP and heart rate. Our results of lower mean SBP in those with NLI of ≥T6 are consistent with the finding of the meta-analysis. However, our data also demonstrated that low BP was associated with ≥T6 motor complete injuries. This is due to the disruption of descending input to the sympathetic preganglionic neurons that control the vital splanchnic vascular bed leading to long-lasting hypotension post injury [24]. The descending vasomotor pathways are located adjacent and dorsolateral to the lateral corticospinal tract [6], and hence motor complete patients (with motor tract injuries) are more susceptible to autonomic cardiovascular dysfunction. A recent systematic review [5] suggested that autonomic completeness is more strongly correlated to cardiovascular function than neurological completeness of injury. As the present study was retrospective and there was no autonomic test (such as sympathetic skin response) routinely performed in these patients, the relationship between autonomic completeness and cardiovascular function was not studied.
Limitations of our study include single centre, retrospective design and relatively high percentage (25%) of patients excluded, which could all add to the risk of bias. Possible confounding factors that could affect BP recordings were inadequate resting time after physical activity, possible bladder and bowel distention prior to recordings. These could not be controlled given the retrospective nature of the study. A major limitation of the study is exclusion of other chronic SCI, who were re-admitted for instance for orthopaedics/plastics/urology procedures or even top-up rehabilitation. The intention of the study was to analyse the SBP data after all the patients with SCI had well passed the phase of spinal shock, i.e. >6 months post injury. It should also be considered that patients on anti-hypertensive medication (or medicines with hypotensive effects) were included, but the proportion of those in all AIS groups was similar (25%) apart from those in the AIS A group (14.3%). The retrospective use of records also resulted in the lack of available discharge MIS data (43 absent records in the ≥T6 group). Another limitation is the small number (n = 34) of ≥T6 motor complete patients, which meant that the study power was lower in this sub analysis.
In conclusion, the study has identified that patients with ≥T6 motor complete injuries have a low specificity for the NEWS SBP chart. Based on our results, an adapted SCI–NEWS SBP chart was synthesised, resulting in improvement of the NEWS specificity from 35 to 82%. However, further research is required to validate the SCI–NEWS and determine whether sensitivity is also improved. To do this, a large scale prospective multicentre trial would be recommended. In addition, the relationship between autonomic completeness and motor completeness of injuries could be explored further by performing an autonomic test, such as sympathetic skin responses in this group of patients.
Data archiving
All data generated or analysed during this study are included in this published article [and its supplementary information files].
References
Hagen E, Rekand T, Gronning M, Faerestrand S. Cardiovascular complications of spinal cord injury. Tidsskr Nor Legeforen. 2012;132:1115–20.
West CR, Mills P, Krassioukov AV. Influence of the neurological level of spinal cord injury on cardiovascular outcomes in humans: a meta-analysis. Spinal Cord. 2012;50:484–92.
Hubli M, Krassioukov A. Ambulatory blood pressure monitoring in spinal cord injury: clinical practicability. J Neurotrauma. 2014;31:789–97.
Claydon VE, Steeves JD, Krassioukov A. Orthostatic hypotension following spinal cord injury: understanding clinical pathophysiology. Spinal Cord. 2006;44:341–51.
West CR, Bellantoni A, Krassioukov AV. Cardiovascular function in individuals with incomplete spinal cord injury: a systematic review. Spinal Cord. 2013;19:267–78.
Furlan JC, Fehlings MG, Shannon P, Norenberg MD, Krassioukov AV. Descending vasomotor pathways in humans: correlation between axonal preservation and cardiovascular dysfunction after spinal cord injury. J Neurotrauma. 2003;20:1351–63.
Krum H, Louis WJ, Brown DJ, Jackman GP, Howes LG. Diurnal blood pressure variation in quadriplegic chronic spinal cord injury patients. Clin. Sci. 1991;80:271–6.
Nitsche B, Perschak H, Curt A, Dietz V. Loss of circadian blood pressure variability in complete tetraplegia. J Hum. Hypertens. 1996;10:311–7.
Munakata M, Kameyama J, Kanazawa M, Nunokawa T, Moriai N, Yoshinaga K. Circadian blood pressure rhythm in patients with higher and lower spinal cord injury: simultaneous evaluation of autonomic nervous activity and physical activity. J Hypertens. 1997;15:1745–9.
Curt A, Nitsche B, Rodic B, Schurch B, Dietz V. Assessment of autonomic dysreflexia in patients with spinal cord injury. J Neurol. Neurosurg. Psychiatry. 1997;62:473–7.
Frisbie JH. Unstable baseline blood pressure in chronic tetraplegia. Spinal Cord. 2007;45:92–5.
Rosado-Rivera D, Radulovic M, Handrakis JP, Cirnigliaro CM, Jensen AM, Kirshblum S, et al. Comparison of 24-hour cardiovascular and autonomic function in paraplegia, tetraplegia, and control groups: implications for cardiovascular risk. J Spinal Cord. Med. 2011;34:395–403.
Scabra-Garcez JD, Matos-Souza JR, Goulart D, Pithon KR, Abib E, Etchebehere M, et al. Ambulatory blood pressure is associated with subclinical atherosclerosis in spinal cord injury subjects. Int J Cardiol. 2012;154:89–90.
Goh MY, Millard MS, Wong ECK, Brown DJ, Frauman AG, O’Callaghan CJ. Diurnal blood pressure and urine production in acute spinal cord injury compared with controls. Spinal Cord. 2017;55:39–46.
Inskip JA, Ravensbergen H(Rianne)JC, Sahota IS, Zawadzki C, McPhailL T, Borisoff JF, et al. Dynamic wheelchair seating positions impact cardiovascular function after spinal cord injury. PLoS One. 2017;12:e0180195.
https://www.rcplondon.ac.uk/projects/outputs/national-early-warning-score-news-2. Accessed 22 Oct 2018].
Asafu-Adjaye K, Gall A. Letter to the Royal College of Physicians regarding the suitability of the National Early Warning Score in the assessment of the unwell spinal cord injury patient. Clin. Med. 2015;15:406–7.
https://asia-spinalinjury.org/wpcontent/uploads/2016/02/International_Stds_Diagram_Worksheet.pdf. Accessed 22 Oct 2018].
Lehamann KG, Lane JG, Piepmeier JM, Batsford WP. Cardiovascular abnormalities accompanying acute spinal cord injury in humans: incidence, time, course and severity. J Am Coll. Cardiol. 1987;10:46–52.
Linsenmeyer TA, Baker ER, Cardenas DD, Mobley T, Perkash I, Vogel LC et al. Overview and recommendations and supporting evidence. In: Acute management of autonomic dysreflexia: individuals with spinal cord injury presenting to the health-care facilities. 2nd edn. USA: Eastern Paralysed Veterans Association; 2001. p. 8–18.
Smith GB, Prytherch DR, Meredith P, Schmidt P, Featherstone PI. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation. 2013;84:465–70.
Tuli S, Tuli J, Coleman WP, Geisler FH, Krassioukov AV. Haemodynamic parameters and timing of surgical decompression in acute cervical spinal cord injury. J Spinal Cord Med. 2007;30:482–90.
Piepmeier JM, Lehmann KB, Lane JG. Cardiovascular instability following acute cervical spinal cord trauma. J Neurotrauma. 1985;2:153–60.
Krassioukov AV. Autonomic function following cervical spinal cord injury. Respir Physiol Neurobiol. 2009;169:157–64.
Acknowledgements
We would like to express our gratitude and special thanks to Dr Sarah Gannon for her contribution in the data collection. We would also like to extend our special thanks to our medical staff team colleagues in the National Spinal Injuries Centre who provided peer support and contributed to discussions about the proposed SCI-NEWS.
Funding
No financial assistance was received in support of the study.
Author information
Authors and Affiliations
Contributions
WA has contributed to the study design, data extraction, data analysis, drafting and revising the manuscript, approving the final version and takes accountability for all aspects of the work. AR has contributed to the study design, data extraction, data analysis, drafting and revising the manuscript, approving the final version and takes accountability for all aspects of the work. KG has contributed to the statistical analysis (i.e. important role interpreting the results), revised the manuscript, approved the final version and takes accountability for all aspects of the work. JC has contributed to the statistical analysis (i.e. important role in interpreting the results), revised the manuscript, approved the final version and takes accountability for all aspects of the work. HD has contributed to the statistical analysis (i.e. important role in interpreting the results), revised the manuscript, approved the final version and takes accountability for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
No ethical approval was required for our study as this was a retrospective observational study. Patients’ confidentiality and anonymity were fully respected in data handling and storage.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ahmed, W.A., Rouse, A., Griggs, K.E. et al. Poor specificity of National Early Warning Score (NEWS) in spinal cord injuries (SCI) population: a retrospective cohort study. Spinal Cord 58, 165–173 (2020). https://doi.org/10.1038/s41393-019-0330-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-019-0330-0
This article is cited by
-
Vital sign differences between septic patients with tetraplegia and paraplegia
Spinal Cord Series and Cases (2022)