Abstract
Background
Molecular biomarker tests are developed as diagnostic tools for prostate cancer (PCa) diagnosis. The SelectMDx (MDxHealth, Nijmegen, The Netherlands) test is a urinary-based biomarker test intended to be used to predict presence of high-grade PCa upon biopsy in men with elevated serum prostate-specific antigen (PSA) levels. Previous validation of the SelectMDx test revealed that 53% of the unnecessary biopsies (biopsies indicating no- or GG1 PCa) could be avoided using the SelectMDx test as a decision-tool to select men for prostate biopsy. The objective of this study is to examine the use of the commercially available SelectMDx test under routine, real-life practice.
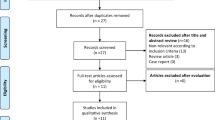
Methods
Men that underwent a SelectMDx test between May 2019 and December 2020 and that were originating from countries that perform the SelectMDx test on a regular basis were included in this study, resulting in 5157 cases from 10 European countries. Clinical parameters, urinary RNA scores, and test outcomes were compared between PSA groups, age groups, countries, and the validation cohort (described previously [4]) using the Mann–Whitney U test, Chi-Square test, Benjamini–Hochberg and Kruskal–Wallis tests.
Results
40.72% of the cases received a negative SelectMDx result. The test is also used in patients outside the intended-use population (PSA < 3 and >10 ng/mL). Clinical parameters (age, PSA density, DRE outcome) varied between patient population from individual countries and the validation cohort, resulting in differences in the potential number of saved biopsies using the test.
Conclusions
The potential number of reduced biopsies in clinical use was 40,72% using the SelectMDx test, assuming a negative SelectMDx test resulted in the decision not to biopsy the patient. This is higher compared to the validation cohort, which is explained by differences in patient population.
Similar content being viewed by others
Introduction
The PSA test is widely used as a risk marker for PCa. Increased use of the PSA test resulted in increasing controversy for its use, since the poor specificity of the PSA test results in overdiagnosis and overtreatment of low-risk cancers [1, 2]. The last decade, various molecular biomarker tests have been developed as diagnostic tools for early and non-invasive detection of PCa [3]. The SelectMDx test (MDxHealth, Nijmegen, The Netherlands) is one of these commercially available molecular tests, which predicts presence of high-grade PCa (Gleason score ≥ 7 (GS7)) upon biopsy. The used prediction model includes a molecular risk score based on post-DRE urinary-derived mRNA levels of the homeobox C6-gene (HOXC6) and Distal-Less Homeobox 1-gene (DLX1) combined with clinical variables digital rectal exam (DRE) result, age and PSA density. The test is intended to be used in patients with an abnormal PSA level to help in patient stratification for biopsy, thereby avoiding biopsies [4]. Moreover, using the SelectMDx test to select patients for multiparametric MRI (mp-MRI) is another good strategy, especially in situations with limited accessibility to mp-MRI [5]. Haese et al. [4] validated the SelectMDx test in a multi-center cohort of men waiting for initial biopsy. Of all patients, 35% had a negative SelectMDx result of whom in 95% of the biopsies showed no PCa or PCa GG1. In the subgroup including patients with PSA levels <10 ng/mL, 44% of all cases showed a negative SelectMDx result. Of these patients, again, 95% of the biopsies showed no PCa or PCa GG1. Therefore, 53% of the unnecessary biopsies (biopsies indicating no- or GG1 PCa) could have been avoided when using the SelectMDx test as a decision-tool for performing a biopsy. Since the SelectMDx test is commercially available for a few years now, data is available on the patient group requesting the SelectMDx test. The aim of this study is to obtain insight into the clinical use of the SelectMDx test in daily practice based on 5157 samples from ten European countries.
Patients and methods
Urine samples
All data used in this paper is derived from MDxHealth company database. Urine samples of patients were collected between May 2019 to December 2020 under routine practice conditions in several European countries. Urine sample collection and processing was conducted following standardized procedures for the SelectMDx test [6]. Briefly, first-void urine is collected by urologists after DRE (at least three strokes per lobe) and mixed with preservative. After transport (on ambient temperature) to the laboratory in Nijmegen, The Netherlands, urine samples are stored at −20 °C prior to analysis. Next, urinary mRNA expression levels of HOXC6 and DLX1 were quantified using RT-qPCR, followed by normalization for the prostate-specific gene KLK3, resulting in the ‘RNA scores’. Afterward, the SelectMDx RNA scores were combined with clinical variables age, PSA density and DRE result in an algorithm-based prediction model to obtain a patient’s individualized risk on PCa ≥ GS7. For cases reporting unknown prostate volume, risk scores were calculated using a different, previously validated prediction model excluding prostate volume as a variable [4]. Cases originating from countries that do not perform the SelectMDx test on a regular basis (less than 100 cases) were excluded from analysis, resulting in a population of 5157 cases from 10 European countries.
Statistical analysis
Statistical analysis was performed using R Statistical Software (version 4.0.5; R Foundation for Statistical Computing, Vienna, Austria). The Mann–Whitney U test and Pearson Chi-Square test were used to compare respectively, continuous variables (age, PSA, PSA density, prostate volume) and categorial variables (proportions negative/positive SelectMDx results and abnormal/normal DRE result) between the clinical use population and the validation cohort described by Haese et al. [4]. Benjamini–Hochberg test post-hoc analysis was performed to calculate adjusted p values for multiple comparison of proportions negative/positive SelectMDx results between each individual country and the validation cohort. Continuous variables of individual countries were compared to the validation cohort using the Kruskal–Wallis multiple comparison post hoc test (Siegel and Castellan [7]). All reported p values are compared to 5% significance level.
Results
The clinical use population (N = 5157) showed a median age of 65 years (interquartile range (IQR): 60–71)), a median PSA level of 6.60 ng/mL (IQR: 4.90–9.06) and a median PSA density of 0.13 ng/ml2 (IQR: 0.09–0.19). Prostate volume was unknown for 94 cases, resulting in exclusion of these cases in analysis on PSA density. Abnormalities were observed during DRE in 17.82% of the patients. In 40.72% of the cases, the SelectMDx result was negative.
PSA groups
Although the SelectMDx test is intended to be used in patients with PSA levels between 3 and 10 ng/mL, SelectMDx analysis is also requested for patients with PSA levels below 3 and higher than 10 ng/mL. Therefore, SelectMDx results were analyzed per PSA group. 5.33% of the cases had a PSA value < 3 ng/mL, 76.65% of the cases reported a PSA value ≥ 3 and ≤10 ng/mL, 11.23% of the cases had a PSA value > 10 and ≤15 ng/mL and 6.79% showed a PSA value > 15 ng/mL (see Table 1).
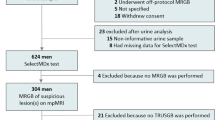
PSA 3–10 ng/mL (n = 3953)
In the intended use population of the SelectMDx test (PSA 3–10 ng/mL), the median age is 65 years (IQR: 59–70), median PSA density is 0.12 ng/ml2 (IQR: 0.09–0.17) and 15.79% of the patients showed DRE abnormalities. Analysis of the SelectMDx results per PSA group showed that 44.65% of the cases with PSA between 3–10 received a negative SelectMDx result, therefore biopsies were potentially saved in 1765 men in this intended-use population of the SelectMDx test (see Fig. 1).
PSA < 3 ng/mL (n = 275)
Age, prostate volume, PSA density and RNA score were lower compared to the other PSA groups. In contrast, the percentage of cases showing an abnormal DRE result is relatively high (29.82%), as compared to the patients with PSA between 3 and 10 (15.79%). A relatively high percentage of patients (75.27%) in this group received a negative SelectMDx result (Fig. 1). In patients with a PSA level below 3 and an abnormal DRE finding, the SelectMDx test reported 35 SelectMDx positive cases (43.67%) and 49 SelectMDx negative cases (58.33%).
PSA > 10 ng/mL (n = 929)
Age, prostate volume, and RNA score are higher in this group compared to the other PSA groups. Prostate volume slightly increases between the groups of PSA 10–15 and PSA > 15, in contrast to larger differences in PSA between both groups. This results in large differences in PSA density between these groups (0.19 ng/ml2 versus 0.31 ng/ml2). In cases with PSA levels > 10 and ≤15, only 19.34% (n = 112) received a negative result. The lowest percentage of negative results (4.57%) is found in patients with PSA levels > 15 ng/mL (n = 16), see Fig. 1.
Age groups
Next, subgroup analysis was performed to compare data on clinical risk factors and SelectMDx results by age groups. Most of the patients have an age ≥65 and <75 (44.23%), followed by the age group ≥55 and <65 (36.77%) (see Table 2). Prostate volume (median), RNA score (median) and percentage abnormal DRE findings increase with increasing age group (except for prostate volume in two highest age groups). PSA density was shown to be stable over the age groups <75 years (PSA density 0.12–0.13 ng/ml2) and showed a sharp increase in age group 75–85 years (PSA density 0.15 ng/ml2) and age group >85 years (PSA density 0.24 ng/ml2). This can be explained by the combination of increasing PSA and a stable prostate volume. Although the PSA density and percentage abnormal DRE findings between age group 45–55 years and 55–65 years are similar, the percentage of cases with a positive SelectMDx result is 17.53% higher in the 55–65 years age group. This could be explained by the increase in age and RNA score in the 55–65 years age group. Overall, the percentage negative SelectMDx results decrease with age, ranging from 83.87% negative results in patients aged <45 years to 0% negative SelectMDx results in patients aged >85 years (see Fig. 2). However, age is a confounding factor in this last analysis since age is included in the SelectMDx algorithm.
Comparing countries and the validation cohort
Subgroup analysis was performed comparing patient groups from different countries (see Table 3). Most of the requests for SelectMDx tests originated from the Netherlands (34.83%) followed by Spain (31.12%) and Italy (7.27%). Differences were found in patient characteristics between countries, with PSA (median) ranging from 5.87 ng/mL in Slovenia to 7.67 ng/mL in Belgium and median age ranging from 63 years in Belgium to 69 years in France. PSA density varied from 0.11 ng/ml2 (Italy) to 0.16 ng/ml2 (Belgium). Considering DRE outcome, cases from Switzerland (45.3%) and Germany (36.9%) have higher percentage abnormal DRE, compared to all other countries (17.82%). PSA density ranges from 0.11 ng/ml2 (Italy) to 0.16 ng/ml2 (Belgium). Next, the percentage of cases with PSA levels below 3 ng/mL varies from 2.43% in Spain to 12.79% in Poland. These differences in patient characteristics between countries are translated into differences in test results: the percentage negative SelectMDx test results range from 30.3% in France to 46.93% in Italy.
In the validation cohort (all PSA levels) of the SelectMDx test, 35.70% of all SelectMDx tests resulted in a negative result. When comparing the ratio of positive/negative SelectMDx result between the clinical use population and the validation cohort, the number of cases with a negative SelectMDx result was significantly higher in the clinical use population compared to the validation cohort: χ2 (1) = 8.18, p < 0.05 (see Table 4). No significant differences were found in PSA levels and age between the clinical use population and the validation cohort. In contrast, prostate volume was significantly higher in the clinical use population compared to the validation cohort, and therefore, PSA density was significantly lower in clinical use cohort compared to the validation cohort. The validation cohort included significantly more cases with an abnormal DRE result as compared to the clinical use population.
Next, the ratio positive and negative SelectMDx test results were compared between each country and the validation cohort. A significantly higher percentage negative SelectMDx result was observed in Italy (χ2 (1) = 14.12, adjusted p < 0.05) and Spain (χ2 (1) = 10.03, adjusted p < 0.05) compared to the validation cohort (Fig. 3). These differences in SelectMDx results could be partly explained by differences in patients selected for a SelectMDx test in these countries. Post-hoc analysis on Italy and Spain showed that PSA density is significantly lower in Spain and Italy compared to the validation cohort. However, PSA is significantly higher in Spain compared to the validation cohort. PSA density is the lowest in Italy, contributing to the higher number of negative SelectMDx results in Italy (see Supplementary Data).
Discussion
During the development and optimization of biomarker tests, studies are conducted including a defined patient population, resulting in test performance characteristics for a specified population. For SelectMDx test, validation studies included men waiting for biopsy having an elevated PSA [4, 8]. The SelectMDx test is intended to be used after a PSA test in patients with a PSA level between 3 and 10 ng/mL and who did not undergo a biopsy yet to guide clinicians in further (biopsy) decision-making. This paper provides a detailed insight into the clinical use of the SelectMDx test in routine practice. Data on SelectMDx test results, clinical risk factors and RNA scores are compared in more detail between PSA groups, age groups and countries.
Performing the SelectMDx test for all patients resulted in a positive SelectMDx result for 59.28% of the patients and a corresponding 40.72% of the patients received a negative result. Therefore, the potential number of reduced biopsies is 40.72% using the SelectMDx test, considering a negative SelectMDx test resulted in the decision not to biopsy the patient. Another clinical utility study on biomarker tests for PCa showed similar results for the urinary ExosomeDx Prostate IntelliScore (potentially saving 39.9% of unnecessary biopsies) and less saved biopsies with the 4K-score (29.5%) [9]. In our study, most cases (>75%) had a PSA between 3 and 10 ng/mL. Using the SelectMDx test as a decision tool for performing a subsequent biopsy and a negative test result will lead to the decision not to perform a biopsy, most biopsies can be saved in patients with PSA below 10 ng/mL.
Although it is not common to take further diagnostic actions in men with PSA below 3 ng/mL, 275 SelectMDx requests were obtained from patients in this PSA group. Multiple factors might play a role in the clinicians’ decision to request a SelectMDx test for these patients, e.g., patients request for further diagnostic actions, urologist is not well informed on the recommended intended population of the test or aberrant clinical parameters other than PSA value were observed, such as a family history of PCa or abnormalities observed during DRE. The last factor is observed in current data: the percentage of patients with an abnormal DRE result is relatively high in the patient group with PSA < 3 ng/mL (29.28%) as compared to the patient group with PSA levels between 3 and 10 ng/mL (15.79%). Using SelectMDx in this subgroup (PSA < 3 and abnormal DRE) showed that 58.33% could have been saved. On the other hand, performing the SelectMDx test for patients with PSA levels higher than 15 ng/mL was shown to be less useful, since almost all these requests (>95%) resulted in a positive result.
Shore and co-authors examined the clinical utility of the SelectMDx test as a decision tool for performing biopsy in men waiting for initial biopsy in the United States [6]. Of all patients (n = 418) with a negative SelectMDx result, 12.5% had a subsequent biopsy, in contrast to 60.7% of the patients with a positive SelectMDx result, indicating that the SelectMDx results affects biopsy decision making procedures. In addition, time between SelectMDx test and biopsy was significantly shorter for SelectMDx positive cases compared to SelectMDx negative cases. A larger percentage of these men showed a negative SelectMDx test (61%) compared to the European clinical use population evaluated in this paper (40.72%) and the validation cohort (35.70%) which might be explained by a higher median PSA level in the European clinical use population (PSA: 6.6 ng/mL) and the validation cohort (PSA: 6.37 ng/mL) compared to the US clinical utility population (PSA: 5.1 ng/mL).
Current analysis comparing SelectMDx test results and clinical risk factor values (PSA, PSA density, age, and abnormal DRE) by country, showed differences on all these risk factors and SelectMDx outcome. This could indicate that the diagnostic path for PCa diagnosis varies between countries, which would result in differences in patient populations requesting SelectMDx tests. Complementary use of the SelectMDx test with other diagnostic tools for early detection of PCa, such as other blood- or urinary biomarker tests, risk calculators or mp-MRI is likely. The EAU guidelines recommend the use of risk calculators or imaging tools in risk-assessment of men with elevated PSA levels (2–10 ng/mL) and a normal DRE result [10]. Variation in diagnostic tools used between or within countries could affect the patient population for SelectMDx in routine practice and therefore the number of biopsies saved by the SelectMDx test. The complementary use of the SelectMDx test with other tools was studied before. Maggi et al. [11] examined several diagnostic strategies incorporating SelectMDx test and mp-MRI for detecting PCa and clinically significant PCa. Combining mp-MRI with the SelectMDx showed best performance for detecting PCa and cs-PCa, when compared to the combinations of MRI and either PSA or PSA density. The authors concluded as best strategy that biopsies should be taken if initial MRI is positive (PI-RADS 4–5) or if SelectMDx test is positive, which should be conducted after negative MRI [11]. The potential of combining SelectMDx and mp-MRI was also demonstrated by Hendriks et al. [5], although these authors opted to use SelectMDx first, prior to mp-MRI to avoid biopsies.
A limitation of this study is the missing information on biopsy decision following a SelectMDx test result. To obtain insight in the effect of a (negative) SelectMDx outcome on further decision-making regarding biopsy, and in fact biopsy-outcome, more information is required. Therefore, the clinical utility as such cannot be assessed and was not considered a primary aim of this study.
Conclusion
To conclude, between May 2019 and December 2020, 5175 urine samples were analyzed by the SelectMDx test and tested in this study. The potential number of reduced biopsies was 40.72% using the SelectMDx test, assuming a negative SelectMDx test resulted in the decision not to biopsy the patient. This number is higher compared to the cohort in which the SelectMDx test was validated, which can be explained by the significant lower numbers of cases with abnormal DRE and lower PSA density in the clinical use population. Although the intended-use population for the SelectMDx test is patients with a PSA level between 3 and 10 ng/mL, SelectMDx tests were requested for patients with other PSA levels. Using the SelectMDx as decision tool in patients with a PSA < 3 ng/mL, the number of potentially saved biopsies increased to 75.27%. Next, variation in patient groups were observed between countries, which affects the ratio positive/negative SelectMDx results and therefore the number of biopsies saved using the SelectMDx test.
Data availability
The datasets cannot be made openly available due to its proprietary nature. An extended description of the data from validation cohort can be found at https://doi.org/10.1097/JU.0000000000000293.
References
Lewis R, Hornberger B. Beyond the PSA test: how to better stratify a patient’s risk of prostate cancer. J Am Acad PAs. 2017;30:51–4.
Thompson IM. Overdiagnosis and overtreatment of prostate cancer. Am Soc Clin Oncol Educ B. 2012;32:e35–9. https://doi.org/10.14694/EdBook_AM.2012.32.98.
Visser WCH, de Jong H, Melchers WJG, Mulders PFA, Schalken JA. Commercialized blood-, urinary-and tissue-based biomarker tests for prostate cancer diagnosis and prognosis. Cancers. 2020;12:3790.
Haese A, Trooskens G, Steyaert S, Hessels D, Brawer M, Vlaeminck-Guillem V, et al. Multicenter optimization and validation of a 2-gene mRNA urine test for detection of clinically significant prostate cancer before initial prostate biopsy. J Urol. 2019;202:256–62.
Hendriks RJ, van der Leest MMG, Israël B, Hannink G, YantiSetiasti A, Cornel EB, et al. Clinical use of the SelectMDx urinary-biomarker test with or without mpMRI in prostate cancer diagnosis: a prospective, multicenter study in biopsy-naïve men. Prostate Cancer and Prostatic Diseases. 2021;24.4:1110-1119.
Shore N, Hafron J, Langford T, Stein M, DeHart J, Brawer M, et al. Urinary molecular biomarker test impacts prostate biopsy decision making in clinical practice. Urol Pr. 2019;6:256–61.
Siegel, S, & Castellan Jr., NJ. Nonparametric statistics for the behavioral sciences. 2nd ed. Mcgraw-Hill Book Company;1988. New York, US.
Van Neste L, Hendriks RJ, Dijkstra S, Trooskens G, Cornel EB, Jannink SA, et al. Detection of high-grade prostate cancer using a urinary molecular biomarker–based risk score. Eur Urol. 2016;70:740–8.
de la Calle CM, Fasulo V, Cowan JE, Lonergan PE, Maggi M, Gadzinski AJ, et al. Clinical utility of 4Kscore®, ExosomeDxTM and magnetic resonance imaging for the early detection of high grade prostate cancer. J Urol. 2021;205:452–60.
EAU Guidelines. Edn. presented at the EAU Annual Congress Amsterdam, the Netherlands 2020. Arnhem, The Netherlands: EAU Guidelines Office.
Maggi M, Del Giudice F, Falagario UG, Cocci A, Russo GI, Di Mauro M, et al. SelectMDx and multiparametric magnetic resonance imaging of the prostate for men undergoing primary prostate biopsy: a prospective assessment in a multi-institutional study. Cancers. 2021;13:2047.
Author information
Authors and Affiliations
Contributions
Determine the concept of paper and data interpretation: WCHV, HdJ, WJGM, PFAM, and JAS. Statistical analysis: WCHV and SS. Drafting of the manuscript: WCHV. Supervision: HdJ, WJGM, PFAM, and JAS.
Corresponding author
Ethics declarations
Competing interests
WCHV, HdJ, and WJGM are employees of MDxHealth. JAS and SS are consultants for MDxHealth. The remaining author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Visser, W.C.H., de Jong, H., Steyaert, S. et al. Clinical use of the mRNA urinary biomarker SelectMDx test for prostate cancer. Prostate Cancer Prostatic Dis 25, 583–589 (2022). https://doi.org/10.1038/s41391-022-00562-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00562-1
This article is cited by
-
Best of 2022 in prostate cancer and prostatic diseases
Prostate Cancer and Prostatic Diseases (2023)
-
The evolving clinical use of prostate cancer biomarkers
Prostate Cancer and Prostatic Diseases (2022)