Abstract
Background
Nocturia (voids arising from sleep) is a ubiquitous phenomenon reflecting many diverse conditions but whether it has significance in its own right remains uncertain. We examined whether nocturia was an independent risk factor for mortality
Methods
These were observational analyses employing primarily North American and European participants and included 7343 men, aged 50–75 years participating in the REDUCE (Reduction by Dutasteride of Prostate Cancer Events) trial. Cox proportional hazards models were used to test the association between baseline nocturia (voiding ≥3 times per night) and all-cause mortality. Potential confounding variables included: age; race; region of origin; treatment group; self-reported coronary artery disease, diabetes mellitus, hypertension, and peripheral vascular disease; smoking; alcohol use; prostate volume; and diuretics. Self-reported sleep quality, as measured with the Medical Outcomes Study sleep scale, was entered as a final step in the model.
Results
Nocturia was associated with increased mortality risk (hazard ratio [HR] = 1.72; 95% CI 1.15–2.55) independent from demographics and medical comorbidities. Inclusion of disturbed sleep in the model reduced the magnitude of the association (HR = 1.43; 95% CI 0.93–2.19).
Conclusions
Although the findings are limited to men, half of whom ingested dutasteride, the interruption of sleep by nocturia may have long-term impact on health and may warrant targeted intervention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Asplund R, Aberg H. Health of the elderly with regard to sleep and nocturnal micturition. Scand J Prim Health Care. 1992;10:98–104.
Bing MH, Moller LA, Jennum P, Mortensen S, Lose G. Nocturia and associated morbidity in a Danish population of men and women aged 60-80 years. BJU Int. 2008;102:808–15.
Blanker MH, Bernsen RM, Ruud Bosch JL, Thomas S, Groenevelt FPMJ, Prins A, et al. Normal values and determinants of circadian urine production in older men: a population-based study. J Urol. 2002;168 Pt 1:1453–7.
Fitzgerald MP, Litman HJ, Link CL, McKinlay JB. The association of nocturia with cardiac disease, diabetes, body mass index, and diuretic use: results from the BACH survey. J Urol. 2007;177:1385–9.
Gourova LW, van de Beek C, Spigt MG, Nieman FHM, Van Kerrebroeck PE. Predictive factors for nocturia in elderly men: a cross-sectional study in 21 general practices. BJU Int. 2006;97:528–32.
Madhu C, Coyne K, Hashim H, Chapple C, Milsom I, Kopp Z. Nocturia: risk factors and associated comorbidities: findings from the EpiLUTS study. Int J Clin Pract. 2015;69:1508–16.
Rembratt A, Norgaard JP, Andersson K-E. Nocturia and associated morbidity in a community-dwelling population. BJU Int. 2003;92:726–30.
Tikkinen KAO, Auvinen A, Johnson TM 2nd, Weiss JW, Keranen T, Tiitinen A. et al. A systematic evaluation of factors associated with nocturia-the population-based FINNO study. Am J Epidemiol. 2009;170:361–8.
Yoshimura K, Terada N, Matsui Y, Terai A, Kinukawa N, Arai Y. Prevalence of and risk factors for nocturia: analysis of a health screening program. Int J Urol. 2004;11:282–7.
Bing MH, Moller LA, Jennum P, Mortensen S, Skovgaard LT, Lose G. Prevalence and bother of nocturia, and causes of sleep interruption in a Danish population of men and women aged 60–80 years. BJU Int. 2006;98:599–604.
Bliwise DL, Foley DJ, Vitiello MV, Ansari FP, Ancoli-Israel S, Walsh JK. Nocturia and disturbed sleep in the elderly. Sleep Med. 2009;10:540–8.
Bliwise DL, Friedman L, Hernandez B, Zeitzer JM, Kushida CA, Yesavage JA. Nocturia reported in nightly sleep diaries: common occurrence with significant implications? Health Psychol. 2014;33:1362–5.
Fung CH, Vaughan CP, Markland AD, Huang AJ, Mitchell MN, Bliwise DL, et al. Nocturia is associated with poor sleep quality among older women in the study of osteoporotic fractures. J Am Geriatr Soc. 2017;65:2502–9.
Maggi S, Langlois JA, Minicuci N, Grigoletto F, Pavan M, Foley DJ, et al. Sleep complaints in community-dwelling older persons: prevalence, associated factors, and reported causes. J Am Geriatr Soc. 1998;46:161–8.
Middelkoop HA, Smilde-van den Doel DA, Neven AK, Kamphuisen HA, Springer CP. Subjective sleep characteristics of 1485 males and females aged 50-93: effects of sex and age, and factors related to self-evaluated quality of sleep. J Gerontol A Biol Sci Med Sci. 1996;51:M108–15.
Zeitzer JM, Bliwise DL, Hernandez B, Friedman L, Yesavage JA. Nocturia compounds nocturnal wakefulness in older individuals with insomnia. J Clin Sleep Med. 2013;9:259–62.
Parthasarathy S, Fitzgerald M, Goodwin JL, Unruh M, Guerra S, Quan SF. Nocturia, sleep-disordered breathing, and cardiovascular morbidity in a community-based cohort. PLOS ONE. 2012;7:e30969.
Endeshaw YW, Johnson TM, Kutner MH, Ouslander JG, Bliwise DL. Sleep-disordered breathing and nocturia in older adults. J Am Geriatr Soc. 2004;52:957–60.
Umlauf MG, Chasens ER, Greevy RA, Arnold J, Burgio KL, Pillion DJ. Obstructive sleep apnea, nocturia and polyuria in older adults. Sleep. 2004;27:139–44.
Asplund R. Hip fractures, nocturia and nocturnal polyuria in the elderly. Arch Gerontol Geriatr. 2006;43:319–26.
Nakagawa H, Niu K, Hozawa A, Ikeda Y, Kaiho Y, Ohmori-Matsuda K, et al. Impact of nocturia on bone fracture and mortality in older individuals: a Japanese longitudinal cohort study. J Urol. 2010;184:1413–8.
Parsons JK, Mougey J, Lambert L, Wilt TJ, Fink HA, Garzotto M, et al. Lower urinary tract symptoms increase the risk of falls in older men. BJU Int. 2009;104:63–8.
Stenhagen M, Ehstrom H, Nordell E, Elmstahl S. Falls in the general elderly population: a 3- and 6-year prospective study of risk factors using data from the longitudinal population study ‘Good ageing in Skane. BMC Geriatr. 2013;13:81.
Stewart RB, Moore MT, May FE, Marks RG, Hale WE. Nocturia: a risk factor for falls in the elderly. J Am Geriatr Soc. 1992;40:1217–20.
Temmi C, Ponholzer A, Gutjahr G, Berger I, Marszalek M, Madersbacher S. Nocturia is an age-independent risk factor for hip-fracture in men. Neurourol Urodyn. 2009;28:949–52.
Vaughan CP, Brown CJ, Goode PS, Burgio KL, Allman RM, Johnson TM 2nd, et al. The association of nocturia with incident falls in an elderly community-dwelling cohort. Int J Clin Pract. 2010;64:577–83.
Asplund R, Aberg H. Nocturnal micturition, sleep and well-being in women of ages 40–64 years. Maturitas. 1996;24:73–81.
Kupelian V, Wei JT, O’Leary MP, Norgaard JP, Rosen RC, McKinlay JB. Nocturia and quality of life: results from Boston area community health survey. Eur Urol. 2012;61:78–84.
Tikkinen KA, Johnson TM 2nd, Tammela TL, Sintonen H, Haukka J, Huhtala H, et al. Nocturia frequency, bother and quality of life: how often is too often? A population-based study in Finland. Eur Urol. 2010;57:488–96.
Yu HJ, Chen FY, Huang PC, Chen TH, Chie WC, Liu CY. Impact of nocturia on symptom-specific quality of life among community-dwelling adults aged 40 years and older. Urology. 2006;67:713–8.
Kupelian V, Fitzgerald MP, Kaplan SA, Norgaard JP, Chiu GR, Rosen RC. Association of nocturia and mortality: results from the Third National Health and Nutrition Examination Survey. J Urol. 2011;185:571–7.
Van Doorn B, Kok ET, Blanker MH, Westers P, Bosch JL. Mortality in older men with nocturia: a 15-year follow up of the Krimpen Study. J Urol. 2012;187:1727–31.
Bursztyn M, Jacob J, Stessman J. Usefulness of nocturia as a mortality risk factor for coronary heart disease among persons born in 1920 or 1921. Am J Cardiol. 2006;98:1311–5.
Galizia G, Langellotto A, Cacciatore F, Mazzella F, Testa G, Della-Morte D, et al. Association between nocturia and falls-related long-term mortality risk in the elderly. J Am Med Dir Assoc. 2012;13:640–4.
Lightner DJ, Krambeck AE, Jacobson DJ, McGree ME, Jacobson SJ, Lieber MM, et al. Nocturia is associated with an increased risk of coronary heart disease and death. BJU Int. 2012;110:848–53.
Asplund R. Mortality in the elderly in relation to nocturnal micturition. BJU Int. 1999;84:297–301.
Chung MS, Chuang YC, Lee JJ, Lee WC, Chancellor MB, Liu RT. Prevalence and associated risk factors of nocturia and subsequent mortality in 1,301 patients with type 2 diabetes. Int Urol Nephrol. 2014;46:1269–75.
Endeshaw YE, Schwartz AV, Stone K, Caserotti P, Harris T, Smagula S, et al. Nocturia, insomnia symptoms and mortality among older men: the Health, Aging and Body Composition Study. J Clin Sleep Med. 2016;12:789–96.
Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleepÿ duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:285–92.
Andriole G, Bostwick D, Brawley OW, Gomella L, Marberger M, Montorsi F, et al. The effect of dutasteride on the usefulness of prostate specific antigen for the diagnosis of high grade and clinically relevant prostate cancer in men with a previous negative biopsy: results from the REDUCE study. J Urol. 2011;185:126–31.
Andriole G, Bostwick D, Brawley O, Gomella L, Marberger M, Tindall D, et al. Chemoprevention of prostate cancer in men at high risk: rationale and design of the reduction by dutasteride of prostate cancer events (REDUCE) trial. J Urol. 2004;172 Pt 1:1314–7.
Andriole G, Bostwick D, Brawley O, Gomella L, Marberger M, Montorsi F, et al. Effect of dutasteride on the risk of prostate cancer. N Engl J Med. 2010;362:1192–202.
Thomas JA 2nd, Gerber L, Banez LL, Moreira DM, Rittmaster RS, Andriole GL, et al. Prostate cancer risk in men with baseline history of coronary artery disease: results from the REDUCE study. Cancer Epidemiol Biomarkers Prev. 2012;21:576–81.
Bosch JL, Hop WC, Kirkels WJ, Schroder FH. The International Prostate Symptom Score in a community-based sample of men between 55 and 74 years of age: prevalence and correlation of symptoms with age, prostate volume, flow rate and residual urine volume. Br J Urol. 1995;75:622–30.
Hays RD, Stewart AL. Sleep measures. In: Stewart AL, Ware JE Jr, editors. Measuring functioning and well-being: the Medical Outcomes Study approach. Durham: Duke University Press; 1992. p. 235–59.
Hays RD, Martin SA, Sesti AM, Spritzer KL. Psychometric properties of the Medical Outcomes Study Sleep measure. Sleep Med. 2005;6:41–4.
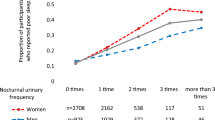
Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50:1306–14.
Tikkinen KA, Tammela TLJ, Huhtala H, Auvinen A. Is nocturia equally common among men and women? A population-based study in Finland. J Urol. 2006;175:596–600.
Johnson TM 2nd, Burgio KL, Redden DT, Wright KC, Goode PS. Effects of behavioral and drug therapy on nocturia in older incontinent women. J Am Geriatr Soc. 2005;53:846–50.
Johnson TM 2nd, Markland AD, Goode PS, Vaughan CP, Colli JL, Ouslander J, et al. Efficacy of adding behavioural treatment or antimuscarinic drug therapy to alpha-blocker therapy in men with nocturia. BJU Int. 2013;112:100–8.
Batista JE, Kolbl H, Herschorn S, Rechberger T, Cambronero J, Halaska M, et al. The efficacy and safety of mirabegron compared with solifenacin in overactive bladder patients dissatisfied with previous antimuscarinic treatment due to lack of efficacy: results of a noninferiority, randomized, phase IIIb trial. Ther Adv Urol. 2015;7:167–79.
Weiss JP, Herschorn S, Albei CD, van der Meulen EA. Efficacy and safety of low dose desmopressin orally disintegrating tablet in men with nocturia; results of a multicenter, randomized, double-blind, placebo-controlled, parallel group study. J Urol. 2013;190:965–72.
Miyazato M, Tohyama K, Touyama M, Nakamura H, Oshiro T, Ueda S, et al. Effect of continuous positive airway pressure on nocturnal urine production in patients with obstructive sleep apnea syndrome. Neurourol Urodyn. 2017;36:376–9.
Fitzgerald MP, Mulligan M, Parthasarathy S. Nocturic frequency is related to severity of obstructive sleep apnea, improves with continuous positive airways treatment. Am J Obstet Gynecol. 2006;194:1399–403.
Margel D, Shochat T, Getzler O, Livne PM, Pillar G. Continuous positive airway pressure reduces nocturia in patients with obstructive sleep apnea. Urology. 2006;67:974–7.
Araujo AB, Yaggi HK, Yang M, McVary KT, Fang SC, Bliwise DL. Sleep related problems and urological symptoms: testing the hypothesis of bidirectionality in a longitudinal, population-based study. J Urol. 2014;191:100–6.
Tyagi S, Resnick NM, Perera S, Monk TH, Hall MH, Buysse DJ. Behavioral treatment of chronic insomnia in older adults—does nocturia matter? Sleep. 2014;37:681–7.
Tyagi S, Resnick NM, Perera S, Monk TH, Hall MH, Buysse DJ. Behavioral treatment of insomnia: also effective for nocturia? J Am Geriatr Soc. 2014;62:54–60.
Centers for Disease Control and Prevention, National Center for Health Statistics. Compressed Mortality File 1999-2007. CDC WONDER On-line Database, compiled from Compressed Mortality File 1999-2007 Series 20 No. 2M. 2010. http://wonder.cdc.gov/cmf-icd10-archive2007.html. Accessed 28 Mar 2018.
Avidan AY, Fries BE, James ML, Szafara KL, Wright GT, Chervin RD. Insomnia and hypnotic use recorded in the minimum data set, as predictors of falls and hip fractures in Michigan nursing homes. J Am Geriatr Soc. 2005;53:955–62.
Brassington GS, King AC, Bliwise DL. Sleep problems as a risk factor for falls in a sample of community-dwelling adults aged 64-99 years. J Am Geriatr Soc. 2000;48:1234–40.
Latimer Hill E, Cumming RG, Lewis R, Carrington S, Le Couteur DG. Sleep disturbances and falls in older people. J Gerontol A Biol Sci Med Sci. 2007;62:62–6.
Mesas AE, Lopez-Garcia E, Rodriguez-Artalejo F. Self-reported sleep duration and falls in older adults. J Sleep Res. 2011;20 Pt 1:21–7.
Stone KL, Ancoli-Israel S, Blackwell T, Ensrud KE, Cauley JA, Redline S, et al. Actigraphy-measured sleep characteristics and risk for falls in older women. Arch Intern Med. 2008;168:1768–75.
Acknowledgements
This work was supported by K24 CA160653 (to SJF). GlaxoSmithKline provided the data but had no role in the conception of this work, analyses of the data, or the preparation of the manuscript
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Trial registration: The REDUCE trial was a registered clinical trial (Clinical Trials.gov number NCT00056407).
Rights and permissions
About this article
Cite this article
Bliwise, D.L., Howard, L.E., Moreira, D.M. et al. Nocturia and associated mortality: observational data from the REDUCE trial. Prostate Cancer Prostatic Dis 22, 77–83 (2019). https://doi.org/10.1038/s41391-018-0090-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-018-0090-5
This article is cited by
-
Modeling study of the effect of placebo and medical therapy on storage and voiding symptoms, nocturia, and quality of life in men with prostate enlargement at risk for progression
Prostate Cancer and Prostatic Diseases (2023)
-
Glucocorticoids coordinate the bladder peripheral clock and diurnal micturition pattern in mice
Communications Biology (2023)
-
Partial Validation of the Sleep Health Construct in the Medical Outcomes Study Sleep Questionnaire
Journal of Clinical Psychology in Medical Settings (2021)
-
Managing Nocturia in Frail Older Adults
Drugs & Aging (2021)
-
Relationship between nocturia and mortality: are we missing the forest for the trees?
Prostate Cancer and Prostatic Diseases (2019)