Abstract
Background
This retrospective cohort study evaluated the association between gout and the risk of benign prostatic hyperplasia among men by using data from Taiwan’s National Health Insurance Research Database.
Methods
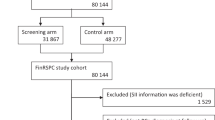
Population-based representative insurance (outpatient and inpatient) claims data of 29,269 patients with gout and 29,269 matched patients without gout (1:1 ratio) for the period of 1997–2010 in Taiwan were identified. The association between gout and benign prostatic hyperplasia was evaluated using the Cox proportional hazards model. The associations of age by gout and gout phenotypes with benign prostatic hyperplasia risk were estimated.
Results
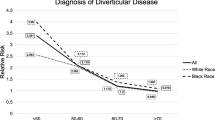
Patients with gout had a higher incidence rate of benign prostatic hyperplasia than those in the matched gout-free group (19.62 vs. 10.11 events per 1000 person-years). Compared with the gout-free group, the adjusted hazard ratios (HRs) (95% confidence intervals (CIs)) for benign prostatic hyperplasia were 1.30 (1.24–1.36). The gout-to-benign prostatic hyperplasia association was modified by age (Pinteraction < 0.0001) in gout patients the age groups of 20–40 years (adjusted HR 2.74, P < 0.0001) and 41–60 years (adjusted HR 1.39, P < 0.0001) but not in the age group of >60 years (adjusted HR 1.07, P = 0.063). Compared with gouty tophi, a higher risk of benign prostatic hyperplasia was noted in gouty nephropathy (adjusted HR 1.30, 95% CI 1.12–1.50).
Conclusions
Our results suggest that male gout is positively related to benign prostatic hyperplasia, particularly in young gout patients and those with gouty nephropathy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Wei JT, Calhoun E, Jacobsen SJ. Urologic diseases in america project: benign prostatic hyperplasia. J Urol. 2008;179:S75–80.
Thorpe A, Neal D. Benign prostatic hyperplasia. Lancet. 2003;361:1359–67.
Lee SWH,Chan EMC,Lai YK, The global burden of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: a systematic review and meta-analysis. Sci Rep. 2017;7:7984.
Unnikrishnan R, Almassi N, Fareed K. Benign prostatic hyperplasia: evaluation and medical management in primary care. Cleve Clin J Med. 2017;84:53–64.
Zhu Y, Pandya BJ, Choi HK. Prevalence of gout and hyperuricemia in the US general population: the National Health and Nutrition Examination Survey 2007–8. Arthritis Rheum. 2011;63:3136–41.
Kuo CF, Grainge MJ, See LC, Yu KH, Luo SF, Zhang W, et al. Epidemiology and management of gout in Taiwan: a nationwide population study. Arthritis Res Ther. 2015;17:13.
Dalbeth N, Merriman TR, Stamp LK. Gout. Lancet. 2016;388:2039–52.
Doherty M, Jansen TL, Nuki G, Pascual E, Perez-Ruiz F, Punzi L, et al. Gout: why is this curable disease so seldom cured? Ann Rheum Dis. 2012;71:1765–70.
Iseki K, Ikemiya Y, Inoue T, Iseki C, Kinjo K, Takishita S. Significance of hyperuricemia as a risk factor for developing ESRD in a screened cohort. Am J Kidney Dis. 2004;44:642–50.
Tsai CW, Lin SY, Kuo CC, Huang CC. Serum uric acid and progression of kidney disease: a longitudinal analysis and mini-review. PLoS ONE. 2017;12:e0170393.
Chou YH, Li WM, Li CC, Huang SP, Liu CC, Wu WJ, et al. Clinical study of uric acid urolithiasis. Kaohsiung J Med Sci. 2007;23:298–301.
Li WM, Chou YH, Li CC, Liu CC, Huang SP, Wu WJ, et al. Local factors compared with systemic factors in the formation of bladder uric acid stones. Urol Int. 2009;82:48–52.
Holmang S, Marin P, Lindstedt G, Hedelin H. Effect of long-term oral testosterone undecanoate treatment on prostate volume and serum prostate-specific antigen concentration in eugonadal middle-aged men. Prostate. 1993;23:99–106.
Pejcic T, Tosti T, Tesic Z, Milkovic B, Dragicevic D, Kozomara M, et al. Testosterone and dihydrotestosterone levels in the transition zone correlate with prostate volume. Prostate. 2017;77:1082–92.
Pui K, Waddell C, Dalbeth N. Early onset of hyperuricaemia and gout following treatment for female to male gender reassignment. Rheumatology. 2008;47:1840–1.
Marinello E, Riario-Sforza G, Marcolongo R. Plasma follicle-stimulating hormone, luteinizing hormone, and sex hormones in patients with gout. Arthritis Rheum. 1985;28:127–31.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9.
Vignozzi L, Gacci M, Maggi M. Lower urinary tract symptoms, benign prostatic hyperplasia and metabolic syndrome. Nat Rev Urol. 2016;13:108–19.
Shih HJ, Huang CJ, Lin JA, Kao MC, Fan YC, Tsai PS. Hyperlipidemia is associated with an increased risk of clinical benign prostatic hyperplasia. Prostate. 2018;78:113–20.
Emmerson B. Hyperlipidaemia in hyperuricaemia and gout. Ann Rheum Dis. 1998;57:509–10.
Choi HK, Mount DB, Reginato AM. American college of P, American Physiological S. Pathogenesis of gout. Ann Intern Med. 2005;143:499–516.
Richette P, Perez-Ruiz F, Doherty M, Jansen TL, Nuki G, Pascual E, et al. Improving cardiovascular and renal outcomes in gout: what should we target? Nat Rev Rheumatol. 2014;10:654–61.
Zhu Y, Pandya BJ, Choi HK. Comorbidities of gout and hyperuricemia in the US general population: NHANES 2007–8. Am J Med. 2012;125:679–87 e671.
Lusco MA, Fogo AB, Najafian B, Alpers CE. AJKD atlas of renal pathology: gouty nephropathy. Am J Kidney Dis. 2017;69:e5–6.
Abou-Elela A. Epidemiology, pathophysiology, and management of uric acid urolithiasis: a narrative review. J Adv Res. 2017;8:513–27.
Sangkop F, Singh G, Rodrigues E, Gold E, Bahn A. Uric acid: a modulator of prostate cells and activin sensitivity. Mol Cell Biochem. 2016;414:187–99.
Vodo S, Bechi N, Petroni A, Muscoli C, Aloisi AM. Testosterone-induced effects on lipids and inflammation. Mediat Inflamm. 2013;2013:183041.
Kelly DM, Jones TH. Testosterone: a vascular hormone in health and disease. J Endocrinol. 2013;217:R47–71.
Coletta RD, Reynolds MA, Martelli-Junior H, Graner E, Almeida OP, Sauk JJ. Testosterone stimulates proliferation and inhibits interleukin-6 production of normal and hereditary gingival fibromatosis fibroblasts. Oral Microbiol Immunol. 2002;17:186–92.
Veldhuis J, Yang R, Roelfsema F, Takahashi P. Proinflammatory cytokine infusion attenuates LH’s feedforward on testosterone secretion: modulation by age. J Clin Endocrinol Metab. 2016;101:539–49.
Kurahashi H, Watanabe M, Sugimoto M, Ariyoshi Y, Mahmood S, Araki M, et al. Testosterone replacement elevates the serum uric acid levels in patients with female to male gender identity disorder. Endocr J. 2013;60:1321–7.
Tung YC, Lee SS, Tsai WC, Lin GT, Chang HW, Tu HP. Association between gout and incident type 2 diabetes mellitus: a retrospective cohort study. Am J Med. 2016;129:1219 e1217–25.
Vargas-Santos AB, Neogi T. Management of gout and hyperuricemia in CKD. Am J Kidney Dis. 2017;70:422–39.
Roughley MJ, Belcher J, Mallen CD, Roddy E. Gout and risk of chronic kidney disease and nephrolithiasis: meta-analysis of observational studies. Arthritis Res Ther. 2015;17:90.
Bostanci Y, Kazzazi A, Momtahen S, Laze J, Djavan B. Correlation between benign prostatic hyperplasia and inflammation. Curr Opin Urol. 2013;23:5–10.
Gandaglia G, Briganti A, Gontero P, Mondaini N, Novara G, Salonia A, et al. The role of chronic prostatic inflammation in the pathogenesis and progression of benign prostatic hyperplasia (BPH). BJU Int. 2013;112:432–41.
Hung SF, Chung SD, Kuo HC. Increased serum C-reactive protein level is associated with increased storage lower urinary tract symptoms in men with benign prostatic hyperplasia. PLoS ONE. 2014;9:e85588.
Kuo TM, Yeh KT, Hsu HT, Chiang SL, Chang JG, Huang CM, et al. ALPK1 affects testosterone mediated regulation of proinflammatory cytokines production. J Steroid Biochem Mol Biol. 2015;154:150–8.
Merriman TR. An update on the genetic architecture of hyperuricemia and gout. Arthritis Res Ther. 2015;17:98.
Yamada Y, Nishida T, Ichihara S, Kato K, Fujimaki T, Oguri M, et al. Identification of chromosome 3q28 and ALPK1 as susceptibility loci for chronic kidney disease in Japanese individuals by a genome-wide association study. J Med Genet. 2013;50:410–8.
Ko AM, Tu HP, Liu TT, Chang JG, Yuo CY, Chiang SL, et al. ALPK1 genetic regulation and risk in relation to gout. Int J Epidemiol. 2013;42:466–74.
Yamada Y, Matsui K, Takeuchi I, Oguri M, Fujimaki T. Association of genetic variants of the alpha-kinase 1 gene with type 2 diabetes mellitus in a longitudinal population-based genetic epidemiological study. Biomed Rep. 2015;3:347–54.
Evans SA, Doblado M, Chi MM, Corbett JA, Moley KH. Facilitative glucose transporter 9 expression affects glucose sensing in pancreatic beta-cells. Endocrinology. 2009;150:5302–10.
Doring A, Gieger C, Mehta D, Gohlke H, Prokisch H, Coassin S, et al. SLC2A9 influences uric acid concentrations with pronounced sex-specific effects. Nat Genet. 2008;40:430–6.
Tu HP, Chung CM, Min-Shan Ko A, Lee SS, Lai HM, Lee CH, et al. Additive composite ABCG2, SLC2A9 and SLC22A12 scores of high-risk alleles with alcohol use modulate gout risk. J Hum Genet. 2016;61:803–10.
Liu WC, Hung CC, Chen SC, Lin MY, Chen LI, Hwang DY, et al. Thers1014290 polymorphism of the SLC2A9 gene is associated with type 2 diabetes mellitus in Han Chinese. Exp Diabetes Res. 2011;2011:527520.
Tu HP, Chen CJ, Tovosia S, Ko AM, Lee CH, Ou TT, et al. Associations of a non-synonymous variant in SLC2A9 with gouty arthritis and uric acid levels in Han Chinese subjects and Solomon Islanders. Ann Rheum Dis. 2010;69:887–90.
Acknowledgements
We thank the National Health Insurance Administration, Ministry of Health and Welfare, Taiwan for its support. This works was supported by grants from Ministry of Science and Technology (MOST 106-2314-B-037-034 and MOST 106-2314-B-037-058), Kaohsiung Medical University Hospital (KMUH103-3T06 and KMUH104-4T03), and Kaohsiung Medical University Research Foundation (KMU-M106006 and KMU-M106032).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
These authors contributed equally: Yi-Ching Tung, Hung-Pin Tu.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Li, WM., Pasaribu, N., Lee, SS. et al. Risk of incident benign prostatic hyperplasia in patients with gout: a retrospective cohort study. Prostate Cancer Prostatic Dis 21, 277–286 (2018). https://doi.org/10.1038/s41391-018-0047-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-018-0047-8