Abstract
Background
Obesity is associated with poorly differentiated and advanced prostate cancer and increased mortality. In preclinical models, caloric restriction delays prostate cancer progression and prolongs survival. We sought to determine if weight loss (WL) in men with prostate cancer prior to radical prostatectomy affects tumor apoptosis and proliferation, and if WL effects other metabolic biomarkers.
Methods
In this Phase II prospective trial, overweight and obese men scheduled for radical prostatectomy were randomized to a 5–8 week WL program consisting of standard structured energy-restricted meal plans (1200–1500 Kcal/day) and physical activity or to a control group. The primary endpoint was apoptotic index in the radical prostatectomy malignant epithelium. Secondary endpoints were proliferation (Ki67) in the radical prostatectomy tissue, body weight, body mass index (BMI), waist to hip ratio, body composition, and serum PSA, insulin, triglyceride, cholesterol, testosterone, estradiol, leptin, adiponectin, interleukin 6, interleukin 8, insulin-like growth factor 1, and IGF binding protein 1.
Results
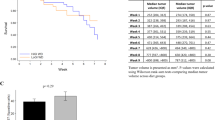
In total 23 patients were randomized to the WL intervention and 21 patients to the control group. Subjects in the intervention group had significantly more weight loss (WL:−3.7 ± 0.5 kg; Control:−1.6 ± 0.5 kg; p = 0.007) than the control group and total fat mass was significantly reduced (WL:−2.1 ± 0.4; Control: 0.1 ± 0.3; p = 0.015). There was no significant difference in apoptotic or proliferation index between the groups. Among the other biomarkers, triglyceride, and insulin levels were significantly decreased in the WL compared with the control group.
Conclusions
In summary, this short-term WL program prior to radical prostatectomy resulted in significantly more WL in the intervention vs. the control group and was accompanied by significant reductions in body fat mass, circulating triglycerides, and insulin. However, no significant changes were observed in malignant epithelium apoptosis or proliferation. Future studies should consider a longer term or more intensive weight loss intervention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Moller H, Roswall N, Van Hemelrijck M, Larsen SB, Cuzick J, Holmberg L, et al. Prostate cancer incidence, clinical stage and survival in relation to obesity: a prospective cohort study in Denmark. Int J Cancer. 2015;136:1940–7.
Haque R, Van Den Eeden SK, Wallner LP, Richert-Boe K, Kallakury B, Wang R, et al. Association of body mass index and prostate cancer mortality. Obes Res Clin Pract. 2014;8:e374–81.
Goris Gbenou MC, Peltier A, Schulman CC, Velthoven R. Increased body mass index as a risk factor in localized prostate cancer treated by radical prostatectomy. Urol Oncol. 2016;34:254 e1–6.
Allott EH, Masko EM, Freedland SJ. Obesity and prostate cancer: weighing the evidence. Eur Urol. 2013;63:800–9.
Giovannucci E, Liu Y, Platz EA, Stampfer MJ, Willett WC. Risk factors for prostate cancer incidence and progression in the health professionals follow-up study. Int J Cancer. 2007;121:1571–8.
Rodriguez C, Freedland SJ, Deka A, Jacobs EJ, McCullough ML, Patel AV, et al. Body mass index, weight change, and risk of prostate cancer in the Cancer Prevention Study II Nutrition Cohort. Cancer Epidemiol Biomarkers Prev. 2007;16:63–9.
Stocks T, Hergens MP, Englund A, Ye W, Stattin P. Blood pressure, body size and prostate cancer risk in the Swedish construction workers cohort. Int J Cancer. 2010;127:1660–8.
Bonn SE, Wiklund F, Sjolander A, Szulkin R, Stattin P, Holmberg E, et al. Body mass index and weight change in men with prostate cancer: progression and mortality. Cancer Causes Control. 2014;25:933–43.
Roberts DL, Dive C, Renehan AG. Biological mechanisms linking obesity and cancer risk: new perspectives. Annu Rev Med. 2010;61:301–16.
Ho E, Boileau TW, Bray TM. Dietary influences on endocrine-inflammatory interactions in prostate cancer development. Arch Biochem Biophys. 2004;428:109–17.
Saglam K, Aydur E, Yilmaz M, Goktas S. Leptin influences cellular differentiation and progression in prostate cancer. J Urol. 2003;169:1308–11.
Trayhurn P, Wood IS. Adipokines: inflammation and the pleiotropic role of white adipose tissue. Br J Nutr. 2004;92:347–55.
Hsing AW, Deng J, Sesterhenn IA, Mostofi FK, Stanczyk FZ, Benichou J, et al. Body size and prostate cancer: a population-based case-control study in China. Cancer Epidemiol Biomarkers Prev. 2000;9:1335–41.
Moran Pascual E, Martinez Sarmiento M, Budia Alba A, Broseta Rico E, Camara Gomez R, Boronat Tormo F. Central body fat mass measured by bioelectrical impedanciometry but not body mass index is a high-grade prostate cancer risk factor. Urol Int. 2016;98:28–31.
Bhindi B, Trottier G, Elharram M, Fernandes KA, Lockwood G, Toi A, et al. Measurement of peri-prostatic fat thickness using transrectal ultrasonography (TRUS): a new risk factor for prostate cancer. BJU Int. 2012;110:980–6.
Tan WP, Lin C, Chen M, Deane LA. Periprostatic fat: a risk factor for prostate cancer? Urology. 2016;98:107–12.
Woo S, Cho JY, Kim SY, Kim SH. Periprostatic fat thickness on MRI: correlation with Gleason score in prostate cancer. AJR Am J Roentgenol. 2015;204:W43–7.
Kobayashi N, Barnard RJ, Said J, Hong-Gonzalez J, Corman DM, Ku M, et al. Effect of low-fat diet on development of prostate cancer and Akt phosphorylation in the Hi-Myc transgenic mouse model. Cancer Res. 2008;68:3066–73.
Mukherjee P, Sotnikov AV, Mangian HJ, Zhou JR, Visek WJ, Clinton SK. Energy intake and prostate tumor growth, angiogenesis, and vascular endothelial growth factor expression. J Natl Cancer Inst. 1999;91:512–23.
Buschemeyer WC 3rd, Klink JC, Mavropoulos JC, Poulton SH, Demark-Wahnefried W, Hursting SD, et al. Effect of intermittent fasting with or without caloric restriction on prostate cancer growth and survival in SCID mice. Prostate. 2010 ;70:1037–43.
Cho HJ, Kwon GT, Park H, Song H, Lee KW, Kim JI, et al. A high-fat diet containing lard accelerates prostate cancer progression and reduces survival rate in mice: possible contribution of adipose tissue-derived cytokines. Nutrients. 2015;7:2539–61.
Liss MA, Schenk JM, Faino AV, Newcomb LF, Boyer H, Brooks JD, et al. A diagnosis of prostate cancer and pursuit of active surveillance is not followed by weight loss: potential for a teachable moment. Prostate Cancer Prostatic Dis. 2016;19:390–4.
Bravata DM, Smith-Spangler C, Sundaram V, Gienger AL, Lin N, Lewis R, et al. Using pedometers to increase physical activity and improve health: a systematic review. J Am Med Assoc. 2007;298:2296–304.
Muzumdar RH, Ma X, Fishman S, Yang X, Atzmon G, Vuguin P, et al. Central and opposing effects of IGF-I and IGF-binding protein-3 on systemic insulin action. Diabetes. 2006;55:2788–96.
Kobayashi N, Barnard RJ, Henning SM, Elashoff D, Reddy ST, Cohen P, et al. Effect of altering dietary omega-6/omega-3 fatty acid ratios on prostate cancer membrane composition, cyclooxygenase-2, and prostaglandin E2. Clin Cancer Res. 2006;12:4662–70.
Ong CW, Kim LG, Kong HH, Low LY, Wang TT, Supriya S, et al. Computer-assisted pathological immunohistochemistry scoring is more time-effective than conventional scoring, but provides no analytical advantage. Histopathology. 2010;56:523–9.
Kim HS, Bowen P, Chen L, Duncan C, Ghosh L, Sharifi R, et al. Effects of tomato sauce consumption on apoptotic cell death in prostate benign hyperplasia and carcinoma. Nutr Cancer. 2003;47:40–7.
Goodwin PJ, Chlebowski RT. Obesity and cancer: insights for clinicians. J Clin Oncol. 2016;34:4197–202.
Iyengar NM, Gucalp A, Dannenberg AJ, Hudis CA. Obesity and cancer mechanisms: tumor microenvironment and inflammation. J Clin Oncol. 2016;34:4270–6.
Ngo TH, Barnard RJ, Tymchuk CN, Cohen P, Aronson WJ. Effect of diet and exercise on serum insulin, IGF-I, and IGFBP-1 levels and growth of LNCaP cells in vitro (United States). Cancer Causes Control. 2002;13:929–35.
Lin DW, Neuhouser ML, Schenk JM, Coleman IM, Hawley S, Gifford D, et al. Low-fat, low-glycemic load diet and gene expression in human prostate epithelium: a feasibility study of using cDNA microarrays to assess the response to dietary intervention in target tissues. Cancer Epidemiol Biomarkers Prev. 2007;16:2150–4.
Wright JL, Plymate S, D’Oria-Cameron A, Bain C, Haugk K, Xiao L, et al. A study of caloric restriction versus standard diet in overweight men with newly diagnosed prostate cancer: a randomized controlled trial. Prostate. 2013;73:1345–51.
Heymach JV, Shackleford TJ, Tran HT, Yoo SY, Do KA, Wergin M, et al. Effect of low-fat diets on plasma levels of NF-kappaB-regulated inflammatory cytokines and angiogenic factors in men with prostate cancer. Cancer Prev Res. 2011;4:1590–8.
Fabian CJ, Kimler BF, Donnelly JE, Sullivan DK, Klemp JR, Petroff BK, et al. Favorable modulation of benign breast tissue and serum risk biomarkers is associated with >10 % weight loss in postmenopausal women. Breast Cancer Res Treat. 2013;142:119–32.
Demark-Wahnefried W, Nix JW, Hunter GR, Rais-Bahrami S, Desmond RA, Chacko B, et al. Feasibility outcomes of a presurgical randomized controlled trial exploring the impact of caloric restriction and increased physical activity versus a wait-list control on tumor characteristics and circulating biomarkers in men electing prostatectomy for prostate cancer. BMC Cancer. 2016;16:61.
Fruge AD, Ptacek T, Tsuruta Y, Morrow CD, Azrad M, Desmond RA, et al. Dietary changes impact the gut microbe composition in overweight and obese men with prostate cancer undergoing radical prostatectomy. J Acad Nutr Diet. 2016. [Epub ahead of print].
Mistry T, Digby JE, Desai KM, Randeva HS. Obesity and prostate cancer: a role for adipokines. Eur Urol. 2007;52:46–53.
Berger NA. Obesity and cancer pathogenesis. Ann N Y Acad Sci. 2014;1311:57–76.
Heidegger I, Massoner P, Sampson N, Klocker H. The insulin-like growth factor (IGF) axis as an anticancer target in prostate cancer. Cancer Lett. 2015;367:113–21.
Li Z, Aronson WJ, Arteaga JR, Hong K, Thames G, Henning SM, et al. Feasibility of a low-fat/high-fiber diet intervention with soy supplementation in prostate cancer patients after prostatectomy. Eur J Clin Nutr. 2008;62:526–36.
Ma HQ, Cui LH, Li CC, Yu Z, Piao JM. Effects of serum triglycerides on prostate cancer and breast cancer risk: a meta-analysis of prospective studies. Nutr Cancer. 2016;68:1073–82.
Waters L, George AS, Chey T, Bauman A. Weight change in control group participants in behavioural weight loss interventions: a systematic review and meta-regression study. BMC Med Res Methodol. 2012;12:120.
Smith MR. Changes in fat and lean body mass during androgen-deprivation therapy for prostate cancer. Urology. 2004;63:742–5.
O’Neill RF, Haseen F, Murray LJ, O’Sullivan JM, Cantwell MM. A randomised controlled trial to evaluate the efficacy of a 6-month dietary and physical activity intervention for patients receiving androgen deprivation therapy for prostate cancer. J Cancer Surviv. 2015;9:431–40.
Demark-Wahnefried W, Polascik TJ, George SL, Switzer BR, Madden JF, Ruffin MT, et al. Flaxseed supplementation (not dietary fat restriction) reduces prostate cancer proliferation rates in men presurgery. Cancer Epidemiol Biomarkers Prev. 2008;17:3577–87.
Acknowledgements
National Institute of Health P50CA92131 (WJA); Merit Review Award from the United States Department of Veterans Affairs. The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government. Statistical analyses were supported by NIH/National Center for Advancing Translational Science (NCATS) UCLA CTSI Grant Number UL1TR001881 (TG/DE).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Rights and permissions
About this article
Cite this article
Henning, S.M., Galet, C., Gollapudi, K. et al. Phase II prospective randomized trial of weight loss prior to radical prostatectomy. Prostate Cancer Prostatic Dis 21, 212–220 (2018). https://doi.org/10.1038/s41391-017-0001-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-017-0001-1
This article is cited by
-
White adipose tissue-derived factors and prostate cancer progression: mechanisms and targets for interventions
Cancer and Metastasis Reviews (2022)
-
Reply to “Phase II prospective randomized trial of weight loss prior to radical prostatectomy”
Prostate Cancer and Prostatic Diseases (2018)
-
Reply to the letter by Demark-Wahnefried et al.
Prostate Cancer and Prostatic Diseases (2018)