Abstract
Background
Maternal hypertensive disorders of pregnancy (HDP) are the major causes of maternal mortality. However, the association between HDP and offspring’s neurodevelopment remains unclear.
Method
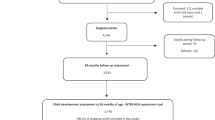
Participants were 4031 singleton live births from a prospective cohort study in Wuhan, China, during October 2013 to October 2014. Neurodevelopment of infant was evaluated by using Chinese version of Gesell Developmental Schedules at 0.5 year of age. Maternal HDP and potential confounders were ascertained by healthcare records at baseline.
Results
Generalized linear model analysis indicated that maternal chronic hypertension were significantly associated with development quotient on fine motor (β = −3.32, 95% CI: −6.33 to −0.31), adaptability (β = −2.87, 95% CI: −5.31 to −0.43), language (β = −1.23, 95% CI: −2.12 to −0.34) and social behavior (β = −2.53, 95% CI: −4.69 to −0.37), and gestational hypertension was significantly associated with development quotient on social behavior (β = −1.42, 95% CI: −2.03 to −0.81), even after adjustment of major confounders. Multivariable logistic regression analysis showed that maternal chronic hypertension also increased the risk of diagnosis of “neurodevelopmental delay” on fine motor (OR = 1.85, 95% CI: 1.19−2.89), adaptability (OR = 2.32, 95% CI: 1.42−3.78), language (OR = 2.86, 95% CI: 1.74−4.70), and social behavior (OR = 2.13, 95% CI: 1.73−2.59).
Conclusion
This study suggests that exposure to HDP is associated with an increased risk of neurodevelopment impairment in the offspring at the age of 0.5 year.
Similar content being viewed by others
Introduction
The concept of developmental origins of health and disease pointed out that adversity during pregnancy will not only affect the fetal outcome, but also affect many aspects of long-term health.1 Maternal hypertensive disorders of pregnancy (HDP) are the common adversities, accounting for 10% of all pregnancies, including four categories based on gestational age at the time of presentation: gestational hypertension, preeclampsia−eclampsia, chronic hypertension, and preeclampsia superimposed upon underlying hypertension.2 Maternal HDP are responsible for 10−15% of the maternal death and is the most common cause of perinatal death.3,4 The adversities also increase risk of adverse pregnancy events and outcomes, such as prematurity, restricted fetal growth,5 which lead to developmental disorders and diseases for their offspring. There is evidence that offspring of mothers with gestational hypertension and preeclampsia are more prone to fetal growth restriction and small head circumference at birth,6 which is associated with numerous adverse neurodevelopmental consequences.7
There are increasing number of researches around developmental origins of health and disease theory during recent years,3,4,5,6,7,8 but the association between maternal HDP and neurodevelopment of the offspring at preschool age has not been well investigated. It is difficult to infer and explain a causal association of maternal HDP with offspring’s neurodevelopment at preschool age based on the existing literatures. Firstly, although several studies have examined the associations of maternal hypertensive diseases with offspring neurodevelopment at preschool age, the results are not consistently reported in these studies.9,10,11,12,13,14,15,16 For example, Krakowiak et al.16 found maternal hypertension was not significantly associated with development delays (OR = 3.58, 95% CI: 0.93−13.78), while Girchenko et al.15 found that preeclampsia was associated with an increased risk of developmental delay. Secondly, although most of those studies were designed as cohort study, the sample size was generally small, and only two studies have adjusted for postnatal factors known to influence early neurodevelopment,12,15 both of which reduced the reliability of the conclusion greatly. Thirdly, all the previous studies were focused on gestational hypertension and/or preeclampsia; no study has examined the association of other types of maternal hypertensive diseases with neurodevelopment of offspring at preschool age. What’s more, all these studies were derived from high-income countries and regions; the findings could not be generalized to the whole world.
China has the largest population in the world, and had implemented one child policy for nearly 40 years.17 China’s progress in maternal and child healthcare during the past 20 years has been impressive.18 In this paper, we examined the data of longitudinal prospective cohort to assess the impacts of maternal HDP on neurodevelopment of offspring in the early age. We investigated whether maternal HDP increased the risk of poorer neurodevelopment, and the different impacts among different types of hypertensive diseases. We hypothesize that maternal HDP increase the risk for neurodevelopmental delay and/or poorer neurodevelopment, and different types of hypertensive diseases have different impacts on neurodevelopment at infant period.
Methods
Study population and data sources
The participants were derived from the Wuhan Health Baby cohort, which was designed to determine the impact of maternal exposures on child health and was conducted in Wuhan, China.19 Pregnant women who lived in Wuhan and without a plan to migrate, and had no communicable diseases were recruited when they had pregnancy examination for the first time at 12 weeks of gestation. The present study was restricted to a subset of women who delivered during October 10, 2013 and October 10, 2014, who had a singleton live birth in Wuhan Maternal and Child Healthcare Hospital, and who had complete medical records on antenatal care, labor care and postnatal care. Healthcare records for their offspring within 0.5 year after birth were also a necessary condition. The final analysis included 4031 mother−infant pairs after excluding 279 pairs who had incomplete medical records (with missing data of >15%), 117 pregnant women with gestational diabetes and 18 infants with birth defect. The response rate in the sample was 90.7%.
We linked records of those mothers and their offspring in the medical information system of Wuhan Maternal and Child Healthcare Hospital. The unambiguous linkage of individual records is feasible because of the unique identifier assigned at birth and is used in the medical information system of the hospital.
Ethics statement
The study protocol was approved by the Ethical Committee of Huazhong University of Science and Technology and Wuhan Maternal and Child Healthcare Hospital. All the participants were asked to sign written informed consent when they came to the hospital for the first time for pregnancy examination.
Definition of maternal hypertensive disorders of pregnancy
According to the diagnostic criteria of American College of Obstetricians and Gynecologists and Task Force on Hypertension in Pregnancy,3 gestational hypertension was defined as having a blood pressure greater than 140/90 mm Hg, measured on two occasions at least 4 h apart in a woman who was normotensive before 20th week of gestation and whose blood pressure returned to normal postpartum. A diagnosis of preeclampsia−eclampsia additionally required de novo proteinuria (>300 mg/24 h). A diagnosis of preeclampsia superimposed on chronic hypertension required hypertension be presented before pregnancy or diagnosed before 20th week of gestation with new onset of proteinuria (>300 mg/24 h). A diagnosis of chronic hypertension was defined as having a blood pressure greater than 140/90 mm Hg that presented before pregnancy or diagnosed before 20th week of gestation or did not resolve postpartum.
Diagnosis of maternal HDP in the medical information system of Wuhan Maternal and Child Healthcare Hospital was coded by using the International Classification of Disease, Tenth Revision (ICD-10). We ascertained the following diagnosis: gestational hypertension (code O13.X51), preeclampsia−eclampsia (code O13.X52), preeclampsia superimposed on chronic hypertension (code O11.X53), and chronic hypertension (code O010.951). We also ascertained maternal HDP based on the related test data recorded in the medical information system.
Assessment of neurodevelopment
The Gesell Developmental Schedules were designed to provide a neurologic and intellectual evaluation of infant or child at the time of testing.20 The Chinese version of Gesell Developmental Schedules for 0−3-year-old child was modified by the Chinese Pediatric Association, with a good validation against Chinese reference population.21 It has been widely used to evaluate infant or child neurodevelopment,22 and to diagnose neurodevelopmental delay in clinic.23,24 The items of Chinese version of Gesell Developmental Schedules are grouped into five neurodevelopment domains: gross motor, fine motor, adaptability, language and social behavior. Specifically, the gross motor includes raising head, standing and walking; fine motor includes hand control and balance; adaptability includes imitation, discriminative performance, and perception; language is assessed by means of vocabulary, word comprehension, and conversation; and social behavior includes reactions to persons, personal habits, and acquired information.
According to the test items, the evaluators estimated a maturity age of neurodevelopment for each of the five domains. The maturity age can be used to calculate a development quotient, which is the maturity age divided by the chronologic age, multiplied by 100. Child can be classified as normal (with development quotient ≥ 85 on all domains), moderate delay (with development quotient between 70 and 85 on one or more domains), or severe delay (with development quotient < 70 on one or more domains).25 In the present study, as there were only 13 infants diagnosed as “severe delay”, therefore, we merged “moderate delay” and “severe delay” into one group.
Neurodevelopment of the offspring was assessed at the Developmental Neuropsychology Laboratory, Wuhan Maternal and Child Healthcare Hospital, by four trained pediatricians. To minimize the variability of the assessment, every effort was made to maximize reliability in scoring by performing standardized training procedures and regular self-checking.26 The evaluators were “blind” to the prenatal and perinatal backgrounds of the offspring.
Covariables
We measured covariables, including numerous prenatal and perinatal factors, which were known to have effects on neurodevelopment of child, including gestational age (divided into four categories: <34 weeks, 34−37 weeks, 37−40 weeks, 40−42 weeks), model of delivery (natural or cesarean delivery), asphyxia neonatorum (yes or no, defined as Apgar scores ≤ 7 at 1 or 5 min), maternal active or passive smoking (yes or no), drinking (yes or no), folic acid supplementation (yes or no), birth weight, sex of child (boy or girl), maternal age at conception, maternal and father’s education level.
Statistical analysis
Mean standard deviation or percentages of variables were used to describe the characteristics of the study participants and compare for outcomes, predictors and control variables. We calculated development quotient and made a neurodevelopmental diagnosis for the five domains for each infant, and both development quotient and diagnosis were examined as the outcomes. Infants who were diagnosed for delay at least on one domain were defined as “neurodevelopment delay” when analyzing the associations between outcomes and demographic characteristics.
The associations between development quotient and HDP were examined in two ways. First, we compared the mean of development quotient among different types of maternal hypertensive diseases by using one-way ANOVA. Then, the association of maternal HDP and infants’ development quotient was evaluated by the generalized linear model with adjustment for other covariables.
The associations between the diagnosis of neurodevelopmental domains and maternal HDP were also examined in two ways. First, chi-square tests were used to compare the incidences of neurodevelopmental delay among different types of hypertensive diseases. Then, binary logistic regression models were used to examine the associations between the diagnosis of neurodevelopmental domains and maternal hypertensive disorders under multivariable context. Odds ratios (OR) and its 95% confidence intervals were calculated for the associations between diagnosis of neurodevelopment domains and different types of maternal hypertensive diseases.
To examine the robustness of our findings, we preformed sensitivity analysis for both the association of maternal hypertensive disorders with offspring’s neurodevelopment quotient and diagnosis by merging gestational hypertension and preeclampsia into one group. In the modeling analysis, we used the multiple imputation technique to deal with missing data.27 In the models, we adjusted for maternal demographic factors (maternal age, gestational weeks, education level of father and mother), prenatal factors (maternal smoking and drinking, folic acid supplementation) and perinatal factors (delivery model, asphyxia neonatorum, birth weight). The significance level was set at 0.05, and all the tests were two-sided, and statistical analyses were conducted using SPSS version 15.0 for Windows (SPSS Inc., Chicago, IL).
Results
Overview
The sociodemographic and clinical characteristics of the participants were shown in Table 1. Of 4031 pairs of mother−infants, 362(9.0%) of the mothers had HDP, of which 88, 233 and 41 were chronic hypertension, gestational hypertension and preeclampsia−eclampsia. Mean value of mothers’ age was 26.8 ± 3.5 years, while 79.0% of the mothers’ and 77.0% of the fathers’ education level was university and above, 54.2% of the mother had folic acid supplementation before pregnancy, 1.8% of the mother had passive smoking exposure during the pregnancy. The mean gestation week of the infants was 38.8 ± 1.3, 55.7% of the infants were male and 75.5% were delivery by cesarean, the birth weight was 3300.4 ± 456.9 g; 99.8% of them had no asphyxia neonatorum. According to the diagnosis criteria for the Chinese version of Gesell Developmental Schedule, 500 (12.4%) infants were classified into neurodevelopmental delay. There were significant associations of neurodevelopmental delay with maternal age, gestation week, father and mother’s educational level, birth weight, asphyxia neonatorum, and maternal hypertensive disorders.
Development quotient and maternal hypertensive disorders
Tables 2 and 3 showed the infant’s developmental quotient and its associations with maternal HDP and its different types. One-way ANOVA found significant differences in development quotient on fine motor (F = 9.226, p < 0.001), adaptability (F = 6.767, p < 0.001), language (F = 2.819, p = 0.038) and social behavior (F = 7.651, p < 0.001) among different types of hypertensive diseases. Generalized linear model analyses demonstrated a negative linear relationship between chronic hypertension and development quotient on fine motor (β = −3.32, 95% CI: −6.33 to −0.31), adaptability (β = −2.87, 95% CI: −5.31 to −0.43), language (β = −1.23, 95% CI: −2.12 to −0.34) and social behavior (β = −2.53, 95% CI: −4.96 to −0.37). But gestational hypertension was only significantly associated with decreasing development quotient on social behavior (β = −1.42, 95% CI: −2.03 to −0.81). T test also found significant differences in development quotient on fine motor, adaptability, language and social behavior between infants whose mother had or not had maternal hypertensive disorders. However, negative linear relationship was only found between maternal hypertensive disorders and social behavior (β = −1.76, 95% CI: −2.43 to −1.09). In the sensitivity analysis in which gestational hypertension and preeclampsia were merged as a group (Table 3), maternal hypertensive disorders were only found associated with decreasing development quotient on social behavior (β = −1.27, 95% CI: −1.91 to −0.63).
Neurodevelopmental diagnosis and maternal hypertensive disorders
The impact of maternal HDP and its different types on neurodevelopmental diagnosis is shown in Tables 4 and 5. The infants whose mothers had maternal hypertensive diseases were more likely to be diagnosed as neurodevelopmental delay; significant differences were found in fine motor (χ2 = 15.770, p = 0.001), adaptability (χ2 = 34.865, p < 0.001), language (χ2 = 32.819, p < 0.001) and social behavior (χ2 = 8.868, p = 0.031). After controlling for maternal demographic factors, prenatal factors, perinatal factors, chronic hypertension remained to have increased the risk of neurodevelopmental delay on fine motor (OR = 1.85, 95% CI: 1.19−2.89), adaptability (OR = 2.32, 95% CI: 1.42−3.78), language (OR = 2.86, 95% CI: 1.74−4.70), and social behavior (OR = 2.13, 95% CI: 1.73−2.59). However, the impact of gestational hypertension and preeclampsia−eclampsia on neurodevelopmental delay was not significant. Sensitivity analysis also indicated that the impact of maternal hypertensive disorders on neurodevelopmental delay was not significant when we merged gestational hypertension and preeclampsia−eclampsia as a group.
Discussion
Main findings
The present study examined a large-scale cohort data of mother−infant in China to investigate the association of maternal HDP with offspring’s neurodevelopment at an early age. The findings indicated that maternal chronic hypertension was significantly associated with development quotient and neurodevelopmental diagnosis on fine motor, adaptability, language and social behavior, while gestational hypertension was only significantly associated with development quotient on social behavior. Our study findings are different from those in previous studies.9,10,11,12,13,14
Interpretation
It has been widely reported that maternal hypertensive disorders may result in inadequate fetal nutrition, hypoxia, systemic inflammation, or overexposure to maternal glucocorticoids.28,29 However, the impact of maternal HDP on neurodevelopment at an early age has been poorly understood.9,10,11,12,13,14,15,16 Although several studies have examined the impact of maternal HDP on neurodevelopment at preschool age child,9,10,11,12,13,14,15,16 their findings were not consistently reported and had various limitations. Four studies have reported that preeclampsia have negative effect on offspring neurodevelopment,9,10,11,15 and two of them without adjustment.9,11 However, some studies reported there was no association of HDP with offspring’s neurodevelopment at preschool age.12,13,16 For example, Krakowiak et al. found that maternal hypertension was not associated with developmental delay of preschool-aged child (OR = 3.58, 95% CI: 0.93−13.78), although maternal metabolic conditions may be broadly associated with developmental delay in children compared with maternal who were free of metabolic conditions (OR = 2.35, 95% CI: 1.43−3.88).16 Two other studies conducted in Australia also reported that maternal HDP have no impacts on children’s neuro and behavior development at an early age,12,13 although both of these two studies failed to define the cases clearly, which may lead to underestimating of the impacts of maternal hypertensive disorders. In the present study, we found that not all types of maternal hypertensive diseases had impacts on offspring’s neurodevelopment at early age, which indicated that maternal hypertensive diseases have different impacts and/or mechanisms model on offspring’s neurodevelopment.
Clinicians and the masses have been deeply aware that chronic hypertension contributes to both development and progression of cerebrovascular disease and cognitive decline.30 However, no study, to date, has explored the impacts of maternal chronic hypertension on offspring’s neurodevelopment at an early age. As far as we are concerned, the present study is the first to provide evidences on the impact of maternal chronic hypertension on the intelligence developmental outcomes of offspring at infancy. The most striking finding of this study was that maternal chronic hypertension mainly effected the development of fine motor, adaptability, language and social behavior at infancy, which suggested that the long-term and specific effects of maternal hypertensive disease could be more pronounced. This evidence was supported by some long-term follow-up studies; for example, Robinson and colleagues have conducted a prospective study which followed up the children at age 2, 5, 8, 10, and 14 years, and found that children of women with gestational hypertension were shown to have poorer behavior from 8 years on. Additionally, maternal chronic hypertension has an earlier and more lasting effect on neurodevelopment on children’s fine motor, adaptability, language and social behavior, which was similar with the previous study.31
The present study had not found significant associations between gestational hypertension and/or preeclampsia and offspring’s neurodevelopment except for social behaviors, which was similar with some previous studies but contradicted with other studies. Five studies have examined the association between gestational hypertension and cognitive outcomes of the offspring in child during 2012−2014; three of them reported associations but one reported lack of association.9,15,32,33,34 Some reasons may contribute to those inconsistent conclusions.
First, it is reported that gestational hypertension and preeclampsia−eclampsia may affect fetal brain development, specifically the development of behavior inhibition.31 However, this kind of effect may be latent to the age when most children have established more firm behavioral control. As such, the time of assessing neurodevelopment can effect this association, although effect of gestational hypertension and preeclampsia may start from the fetal period.35 Robinson et al. also reported that a significant relationship between gestational hypertension and behavior was not observed until the age of 8 years.31
Second, gestational hypertension and preeclampsia−eclampsia may lead to premature delivery and even abortion; thus, the recruited offspring may be hardly representative. The results may be also associated with the number of gestational hypertension/preeclampsia−eclampsia cases, which may draw a conclusion by chance if the number is small.36
Third, results from other studies have also suggested that in relation to neurodevelopment, gestational hypertension and preeclampsia may be conceptually dissimilar predictors,37 as the latter is a disease driven by immunological maladaptation with vascular and genetic components,38 while the former is a milder transient condition that may be operated through other mechanisms, which may include maternal mental health status or maternal obesity.39 Additionally, antihypertensive agents prescribed to the mother may also impact offspring’s neurodevelopment, although a number of agents have been shown to have no significant adverse fetal outcomes.40
Strength and limitations
The main strength of this study was the use of a large cohort that provided detailed data collected from 12 weeks of gestation and prospectively throughout 0.5-year-old newborn, thus allowing for multiple analysis of risk factors of offspring’s neurodevelopment. Additionally, in this study, it is possible to distinguish different subtypes of maternal hypertensive disorders such as maternal chronic hypertension, gestational hypertension and preeclampsia, so that their different effects on neurodevelopment can be evaluated. What is more, we are able to adjust the potential confounding factors that may influence infants’ neurodevelopment, which make the results of our study more reliable. However, several limitations also need to be addressed. First, neurodevelopment is a long-term process and neurodevelopmental delay could not be discovered when the follow-up time is not long enough; therefore, we assessed neurodevelopment at 0.5 year of age may underestimate the association between maternal hypertensive disorders and offspring’s neurodevelopment. Additionally, this study was conducted in the biggest tertiary hospital for women and children in Wuhan, where the cesarean delivery rate and the maternal educational level were relatively high, both of which might limit the generalization of our findings. The other limitation is that data on medication for maternal hypertension disorders were not collected in the present study, which may overestimate or underestimate the strength of the association between maternal hypertension disorders and the offspring’s neurodevelopment.39,40 As noted above, continued follow-up of the present cohort and the collection of more related information will determine whether maternal HDP is a risk factor for offspring’s neurodevelopment.
Conclusion
Different types of maternal HDP have different effects on offspring’s neurodevelopment; distinguishing different types of maternal HDP is essential for pregnancy and child healthcare. Maternal chronic hypertension has greater effect on neurodevelopment in the offspring at the age of 0.5 year. Longer follow-up and study on pathogenic mechanism are essential to provide more evidence on how maternal HDP affect offspring’s neurodevelopment. These findings also highlight the need for greater pediatric surveillance of infants whose mother are exposed to HDP, to allow early intervention that may help to improve neurodevelopmental outcome.
References
Kent, A. L. & Health, C. Developmental origins of health and adult disease: what should neonatologists/paediatricians be considering about the long-term health of their patients? J. Paediatr. 48, 730–734 (2012).
American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet. Gynecol. 122, 1122-1131 (2013).
Lo, J. O., Mission, J. F. & Caughey, A. B. Hypertensive disease of pregnancy and maternal mortality. Curr. Opin. Obstet. Gynecol. 25, 124–132 (2013).
Filippi, V. et al. Interventions to Reduce Maternal and Newborn Morbidity and Mortality (The International Bank for Reconstruction and Development/The World Bank, Washington, DC, 2016).
Gemmell, L. et al. Hypertensive disorders of pregnancy and outcomes of preterm infants of 24 to 28 weeks’ gestation. J. Perinat. 36, 1067–1072 (2016).
Beukers, F. et al. Catch-up growth in children born growth restricted to mothers with hypertensive disorders of pregnancy. Arch. Dis. Child. 98, 30–35 (2013).
Ghods, E. et al. Head circumference catch-up growth among preterm very low birth weight infants: effect on neurodevelopmental outcome. J. Perinat. Med. 39, 579–586 (2011).
Mendezfigueroa, H., Truong, V. T. T., Pedroza, C. & Chauhan, S. P. Morbidity and mortality in small-for-gestational-age infants: a secondary analysis of nine MFMU network studies. Am. J. Perinatol. 34, 323–332 (2016).
Many, A. et al. Neurodevelopmental and cognitive assessment of children born growth restricted to mothers with and without preeclampsia. Hypertens. Pregnancy 22, 25–29 (2009).
Shao-Wen, C. et al. Delivery before 32 weeks of gestation for maternal pre-eclampsia: neonatal outcome and 2-year developmental outcome. Early Hum. Dev. 76, 39–46 (2004).
Warshafsky, C. et al. Prospective assessment of neurodevelopment in children following a pregnancy complicated by severe pre-eclampsia. BMJ Open 6, e010884 (2016).
Robinson, M. et al. Hypertensive diseases of pregnancy and the development of behavioral problems in childhood and adolescence: the Western Australian Pregnancy Cohort Study. J. Pediatr. 154, 218–224.e212 (2009).
Matić, M. et al. Maternal hypertensive disorders are associated with increased use of respiratory support but not chronic lung disease or poorer neurodevelopmental outcomes in preterm neonates at <29 weeks of gestation. J. Paediatr. Child Health 53, 391 (2017).
Silveira, R. C. et al. Growth and neurodevelopment outcome of very low birth weight infants delivered by preeclamptic mothers. Acta Peadiatr. 96, 1738–1742 (2007).
Girchenko, P. et al. Maternal early pregnancy obesity and related pregnancy and pre-pregnancy disorders: associations with child developmental milestones in the prospective PREDO Study. Int. J. Obes. 42, 995–1007 (2018).
Krakowiak, P. et al. Maternal metabolic conditions and risk for autism and other neurodevelopmental disorders. Pediatrics 129, e1121 (2012).
Zeng, Y. & Hesketh, T. The effects of China’s universal two-child policy. Lancet 388, 1930–1938 (2016).
Requejo, J., Victora, C. & Bryce, J. Countdown to 2015: A Decade of Tracking Progress for Maternal Newborn and Child Survival. The 2015 Report (United Nations International Children’s Emergency Fund and World Health Organization, Geneva, 2015).
Yang, J. et al. Maternal urinary cadmium concentrations in relation to preterm birth in the Healthy Baby Cohort Study in China. Environ. Int. 94, 300–306 (2016).
Gesell, A. & Amatruda, C. S. Developmental diagnosis: normal and abnormal child development. Clinical methods and practical applications (New York: Hoeber, 1941).
Song, J. & Zhu, Y. M. Children’s Neuropsychological Tests 2nd edn (Shanghai Scientific and Technological Publishing Company, Shanghai, China, 1987).
Tang, D. et al. Effects of prenatal exposure to coal-burning pollutants on children’s development in China. Environ. Health Perspect. 116, 674–679 (2008).
Liu, Z., Li, Y., Lu, Y. & Chen, J. Clinical research on intelligence seven needle therapy treated infants with brain damage syndrome. Chin. J. Integr. Med. 22, 451–456 (2016).
Tang, D. et al. Molecular and neurodevelopmental benefits to children of closure of a coal burning power plant in China. PLoS ONE 9, e91966 (2013).
Yang, Y. F. Rating Scales for Children’s Developmental Behavior and Mental Health (People’s Medical Publishing House, Peking, 2016).
Wang, Y. et al. Prenatal and postnatal exposure to organophosphate pesticides and childhood neurodevelopment in Shandong, China. Environ. Int. 108, 119–126 (2017).
Ananth, C. V. et al. Association between temporal changes in neonatal mortality and spontaneous and clinician-initiated deliveries in the United States, 2006−2013. JAMA Pediatr. 172, 949–957 (2018).
Aufdenblatten, M. et al. Prematurity is related to high placental cortisol in preeclampsia. Pediatr. Res. 65, 198 (2009).
Redman, C. W. G. & Sargent, I. L. Immunology of pre‐eclampsia. Am. J. Reprod. Immunol. 63, 534–543 (2010).
Wiles, N. J., Peters, T. J., Leon, D. A. & Lewis, G. Birth weight and psychological distress at age 45-51 years: results from the Aberdeen Children of the 1950s cohort study. Brit J. Psychiat. 187, 21–28 (2005).
Liu, X., Zhou, X., Yan, H. & Wang, D. Use of maternal healthcare services in 10 provinces of rural western China. Int. J. Gynecol. Obstet. 114, 260–264 (2011).
Martikainen, M. A., Airaksinen, E. M., Heinonen, K. M. & Castren, M. L. The neurological condition of the newborn infant with maternal hypertension, examined at term. Early Hum. Dev. 16, 107–118 (1988).
Nelson, P. T. et al. Alzheimer’s disease is not “brain aging”: neuropathological, genetic, and epidemiological human studies. Acta Neuropathol. 121, 571–587 (2011).
Roberts, J. M. & Redman, C. W. G. Pre-eclampsia: more than pregnancy-induced hypertension. Lancet 341, 1447–1451 (1993).
Ngene, N. C. & Moodley, J. Role of angiogenic factors in the pathogenesis and management of pre-eclampsia. Int. J. Gynecol. Obstet. 141, 5–13 (2018).
Doherty, D. A. et al. Pre-pregnancy body mass index and pregnancy outcomes. Int. J. Gynecol. Obstet. 95, 242–247 (2006).
Muntner, P., Bowling, C. B. & Shimbo, D. Systolic blood pressure goals to reduce cardiovascular disease among older adults. Am. J. Med. Sci. 348, 129–134 (2014).
Chen, R., Clifford, A., Lang, L. & Anstey, K. J. Is exposure to secondhand smoke associated with cognitive parameters of children and adolescents?—a systematic literature review. Ann. Epidemiol. 23, 652–661 (2013).
Lopezarana, S., Burdorf, A. & Avendano, M. Trends in overweight by educational level in 33 low- and middle-income countries: the role of parity, age at first birth and breastfeeding. Obes. Rev. 14, 806–817 (2013).
Weir, S., Juhasz, A., Puelles, J. & Tierney, T. S. Relationship between initial therapy and blood pressure control for high-risk hypertension patients in the UK: a retrospective cohort study from the THIN general practice database. BMJ Open 7, e015527 (2017).
Acknowledgements
We would like to acknowledge all participating families for their continuing participation in the study. We also would like to acknowledge pediatricians and other study staffs for their commitment to data collection. This study was supported by the National Natural Science Foundation of China (grant numbers: 81273083, 91643207). The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Contributions
Z.C. and B.Z. conceived and designed the study. R.L. and J.Z. assisted with study design. Z.C. and H.L. contributed to statistical analysis and wrote the manuscript. J.D., L.Q., Y.Z. and C.X. provided statistical advice and C.Y. assisted with data collection. R.Y. reviewed and edited the manuscript. All authors approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, Z., Li, R., Liu, H. et al. Impact of maternal hypertensive disorders on offspring’s neurodevelopment: a longitudinal prospective cohort study in China. Pediatr Res 88, 668–675 (2020). https://doi.org/10.1038/s41390-020-0794-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0794-9
This article is cited by
-
Association between maternal hypertension and infant neurodevelopment in extremely preterm infants
Journal of Perinatology (2024)
-
Study protocol for the sheMATTERS study (iMproving cArdiovascular healTh in new moThERS): a randomized behavioral trial assessing the effect of a self-efficacy enhancing breastfeeding intervention on postpartum blood pressure and breastfeeding continuation in women with hypertensive disorders of pregnancy
BMC Pregnancy and Childbirth (2023)
-
A review of infant growth and psychomotor developmental outcomes after intrauterine exposure to preeclampsia
BMC Pediatrics (2022)