Abstract
Background
Displaying heart rate characteristic (HRC) scores was associated with lower sepsis-associated mortality in very low birth weight (VLBW) infants in a multicenter randomized controlled trial (HeRO trial). The aim of this study was to test whether HRC indices rise before diagnosis of urinary tract infection (UTI) or meningitis, with and without concomitant BSI.
Methods
Blood, urine, and cerebrospinal fluid (CSF) culture data after 3 days of age and within 120 days of study enrollment were analyzed from 2989 VLBW infants. The HRC index was analyzed 12 h prior to positive cultures compared to 36 h prior, using paired signed-rank tests.
Results
UTI, meningitis, and BSI were diagnosed in 10%, 2%, and 24% of infants, respectively. The mean hourly HRC index was significantly higher 12 h prior to diagnosis of UTI and BSI compared to 36 h prior (UTI 2.07 versus 1.81; BSI 2.62 versus 2.25, both p < 0.0001). The baseline HRC index was higher for meningitis, compared to UTI or BSI, but without a statistically significant rise in the day prior to meningitis diagnosis.
Conclusions
In a large cohort of VLBW infants enrolled in the HeRO trial, the HRC index increased in the 24-h period prior to diagnosis of UTI and BSI but not meningitis.
Similar content being viewed by others
Introduction
Abnormal fetal heart rate characteristics (HRCs) such as decreased heart rate variability and transient decelerations have been used as a biomarker of fetal distress for over a century.1 More recently, technology has been developed to analyze electrocardiogram data from neonatal intensive care unit (NICU) bedside monitors to calculate an HRC index or HeRO score to indicate the fold increase in probability of sepsis being diagnosed in the following 24-h period.2 In a single-center study, elevation in the HRC index, which incorporates measures of low heart rate variability, increased decelerations, and low sample entropy, was associated not only with sepsis but also with urinary tract infection (UTI) and with mortality.3 A large randomized clinical trial (“HeRO trial”), which enrolled 3003 very low birth weight (VLBW; <1500 g birth weight) infants, demonstrated that displaying the HRC index to the clinician reduced all-cause mortality by 22%4 and septicemia-associated mortality by 40%.5 However, the performance of this test as a biomarker for infections in other sites such as urine and cerebrospinal fluid (CSF) has not been evaluated. Here we analyzed the rich dataset of cultures from HeRO trial participants to test the hypothesis that HRC monitoring may alert providers to the existence of UTI or meningitis, even in the absence of concomitant blood stream infection (BSI). We also sought to evaluate center-specific differences in collecting urine and CSF cultures around the time a blood culture was obtained for suspected infection. Finally, we examined the change in the HRC index during infection with coagulase negative staphylococci (CONS) versus other organisms and for infants on and off mechanical ventilation.
Methods
Patients
A total of 3003 VLBW infants were enrolled in a previously published randomized, controlled HRC monitoring trial at 8 centers from 2004 to 2010, and 2989 were included in the original and current analyses (the other 14 had consent withdrawn or were ineligible based on birth weight) (ClinicalTrials.gov: NCT00307333).4 The trial was approved by the institutional review boards at each enrollment site, and parental consent was obtained. Infants were randomly assigned to one of the two groups. One group of infants had their HRC index visible to the care team, and providers were able to use the HRC index at their discretion for clinical management. No specific action was required, based on an infant’s score. Infants in the control (standard) group had their HRC index recorded but not displayed to clinicians. Laboratory tests for suspected sepsis, including blood, CSF, and urine cultures, as well as decisions for antimicrobial therapy, were recorded but performed according to clinician discretion at each participating center.
Infections and HRC index
The objective for this secondary analysis was to determine whether the HRC index rises before diagnosis of UTI or meningitis, with or without concomitant BSI. Therefore, we analyzed the results of all urine, CSF, and blood cultures collected for suspicion of infection after 3 days of age and within 120 days after consent and randomization.
Late-onset BSI was defined, for the purpose of this substudy, as a positive blood culture in an infant at least 72 h of age with a bacterial or fungal organism not considered a contaminant and treated with at least 5 days of antimicrobials. For the 14 cases of multiple bacteria cultured from the blood considered to be true BSI, the organism thought to be the most virulent was included in the microorganism designation.
A 3-day window was allowed to determine whether urine or CSF cultures were taken at the time of blood culture for suspected infection.
UTI was defined as a positive urine culture obtained by suprapubic bladder aspiration or catheterization with a single organism, documentation of at least 5 days of antimicrobials, and no indication in the database that the culture yield was <10,000 colony-forming units and/or a suspected contaminant. Meningitis was defined as a positive CSF culture yielding a single organism and no indication in the database that it was a suspected contaminant.
Infections were considered a single episode if the same organism was cultured within a 7-day time period. The hourly HRC index was analyzed 5 days prior to and after the infection diagnosis (defined as the time the positive culture was sent). To illustrate the trend in the HRC index in infants without suspected or proven infection, the mean hourly HRC index in infants undergoing cultures indicated in the study database as screening and not suspected infection was also calculated.
Statistics
Results are presented as number and percentage or mean and standard deviation unless otherwise noted. Changes in the mean hourly HRC index 12 h versus 36 h prior to infection diagnosis (culture time) were compared using Wilcoxon signed-rank tests. Statistical analyses were performed in MatLab (MathWorks, Natick, MA, USA) with p < 0.05 considered statistically significant.
Results
Demographics and outcomes
The demographics of all infants and of the subgroups with and without positive cultures are shown in Table 1. Of the 2989 infants, 863 (29%) had at least 1 late-onset infection (UTI, meningitis or BSI, as defined in Methods). Late-onset UTI, meningitis, and BSI were detected in 10%, 2%, and 24% of the tested infants, respectively (Table 2), with no significant difference between infants randomized to HRC display versus control. The mean gestational age and birth weight of infants with any infection was 26 weeks and 822 g, respectively. Infants with infection were more premature, had lower birth weight, and were more likely to be male (60%). After controlling for gestational age and birth weight, infants with infection also had more days on mechanical ventilation and longer length of stay in the NICU (p < 0.05). All-cause mortality in the period of the randomized controlled trial (RCT) (120 days from randomization) was 9%. Mortality was increased among infected infants (16%) compared to infants who had cultures obtained but no documented infection (7%).
Cultures and infections
Figure 1 shows results of all blood cultures sent for suspicion of infection and the associated urine and CSF cultures. The total number of cultures was 13,859 (8206 blood cultures in 1649 infants; 3603 urine cultures in 1189 infants; 2050 CSF cultures in 923 infants). Infants randomized to the HRC index display group had 10% more blood cultures, 16% more urine cultures, and 6% more CSF cultures sent than those in the control group but did not have a significant difference in the number of infections.
Of the 8206 blood cultures obtained for suspicion of sepsis, 991 (12%) were diagnostic of BSI. Of the 991 BSI cases, 107 (11%) were associated with UTI and 30 (3%) with meningitis. Of the 7215 infection workups with negative blood culture, 359 (5%) were associated with UTI and 34 (0.5%) with meningitis. Of the 466 UTIs, 107 (23%) were associated with BSI, and of the 64 cases of meningitis, 30 (47%) were associated with BSI. In 30 cases of UTI and 2 cases of meningitis, no blood culture was reported within 3 days of the positive culture result.
The majority of blood cultures were not accompanied by a urine or CSF culture. Overall, urine and CSF cultures were sent around the time of blood cultures in 44% of cases (center range 6–77%) and 24% of cases (center range 7–49%), respectively. Differences between centers are shown in Supplementary Table 1.
Of the 8206 blood cultures obtained, 991 (12%) were diagnostic of BSI. Of the 3633 urine cultures sent for suspected infection, including 30 sent without blood culture, 466 (13%) were diagnostic of UTI in 305 infants. An additional 17% of urine cultures yielded either mixed organisms or were indicated as contaminants in the study database. Of the 2052 CSF cultures sent for suspected infection, including 2 with no associated blood culture, 66 (3%) were diagnostic of meningitis in 61 infants, and an additional 26 yielded one or multiple organisms indicated in the database as suspected contaminants. In summary, the yield of blood, urine, and CSF cultures sent for suspected infection for diagnosis of BSI, UTI and meningitis was 12%, 13%, and 3%, respectively.
Figure 1 shows that, of the 991 cases of BSI, 107 (11%) were associated with a urine culture indicating UTI and 30 (3%) with a CSF culture indicating meningitis. Of the 7215 infection workups with negative blood culture, 359 (5%) were associated with UTI and 34 (0.5%) with meningitis. Of the 466 UTIs, 107 (23%) were associated with a BSI, and of the 64 cases of meningitis, 30 (47%) were associated with a BSI. In 30 cases of UTI and 2 cases of meningitis, no blood culture was reported within 3 days of the positive urine or CSF culture.
Table 2 shows characteristics of infants with culture-positive infections. Of all the infants enrolled in the original trial, 715 (24%) were diagnosed with BSI, 305 (10%) with UTI, and 61 (2%) with meningitis. Some infants had two or more infections. Infants with UTI, meningitis, and BSI were of similar mean gestational age and birth weight. UTI was diagnosed at a later age (mean 43 days versus 31 days for meningitis and 26 days for BSI).
Microorganisms
Among the 991 cases of BSI, CONS was isolated, and antibiotics continued at least 5 days in 487 (49%). CONS was considered a contaminant in 124 positive blood cultures (<5 days antibiotics and/or indicated as contaminant in the study database). CONS was isolated and treated in 16% of UTIs and in 45% of cases of meningitis.
The majority of UTIs were caused by Gram-negative organisms (58%) in contrast to BSI (23%) or meningitis (18%). The most common organism isolated were Klebsiella sp. for UTI and CONS for meningitis and BSI (Table 2). A fungal organism was isolated in cultures from 12%, 8%, and 6% of infants with UTI, meningitis and BSI, respectively.
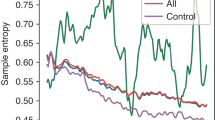
HRC index around the time of infections
Figure 2 shows the mean hourly HRC index for 5 days before and after diagnosis of BSI, UTI, or meningitis only or all cases of UTI and meningitis, which may include concomitant BSI. In addition, for infants without suspicion of infection, as described in “Methods”, the mean HRC index is shown, with no significant change around the time of a screening culture (n = 920). In contrast, the HRC index rose significantly in the day prior to diagnosis of UTI and BSI compared to the prior day. For cases in which paired HRC index data were available at 36 and 12 h prior to the positive culture, the mean HRC index rose from 1.81 (standard error (SE) = 0.117) to 2.07 (SE = 0.123) for UTI only (n = 233, p < 0.0001) and from 2.25 (SE = 0.076) to 2.62 (SE = 0.080) for BSI only (n = 693, p < 0.0001). For the combined UTI with BSI, there was a rise in mean HRC from 2.20 (SE = .217) to 2.55 (SE = .233) but this effect size was not statistically significant (n = 89, p = 0.36) for this smaller sample size.
Mean hourly HRC index is shown in the 5-day period before and after time of positive culture, day zero indicated by vertical dotted line. From lower to upper curves: UTI only (thin dotted) all UTI including BSI (dashed), BSI only (thick solid), meningitis only (thick dotted), and all meningitis including BSI (thick dashed).
In infants with meningitis, the mean HRC index was higher at baseline, rose several days prior to diagnosis, and remained high after diagnosis (Fig. 2). For cases in which paired HRC index data were available at 36 and 12 h prior to the positive culture, the mean HRC index did not rise significantly (2.91 versus 3.07, n = 31, p = 0.87) for this small sample size.
Figure 3 shows that, comparing all CONS and non-CONS infections (n = 543 and 756, respectively), there was a similar rise in the HRC index prior to diagnosis. The figure additionally shows that, comparing infants on or off mechanical ventilation at the time of infection, those on a ventilator (46% of the total) had a higher baseline HRC index and a smaller relative rise prior to diagnosis.
Mean hourly HRC index is shown in the 5-day period before and after time of positive culture, day zero indicated by vertical dashed line. From lower to upper curves: infants with non-CONS infections not on mechanical ventilation (thick dotted), CONS infections not on ventilator (solid), and non-CONS and CONS infections on ventilator (dashed and thin dotted, respectively).
Discussion
Changes in HRCs (decreased HR variability and superimposed transient decelerations) as part of the host response to infection have been demonstrated in VLBW infants with septicemia, but the diagnostic value for other infections has not previously been demonstrated.6 Here we present a subanalysis of a large randomized clinical trial (“HeRO” trial) including culture data from blood, urine, and CSF in 2989 VLBW infants for 120 days from randomization. We found a statistically significant rise in the HRC index in infants with UTI even as a localized infection in the absence of BSI.
The incidence of infection and the organism distribution we report are consistent with other reports of VLBW late-onset sepsis in the time period studied, with 23% incidence of BSI and a predominance of CONS.7,8,9 UTIs are common beyond day 3 of age,10,11,12 and the number of VLBW infants in our study diagnosed with this infection was 10%, similar to previously reported rates13,14 A lack of guidelines or incomplete adherence to guidelines among NICUs as to whether to obtain a urine culture when getting a blood culture for infants with suspected infection is one explanation for the practice variation we observed among centers. For the 30 cases of UTI, no blood culture results were reported, yet we found that 23% of UTIs were associated with bacteremia.
Meningitis is rare in VLBW infants but associated with high morbidity and mortality. The rate reported in our cohort (2%) is similar to that reported by other centers in the United States.15 In regard to CSF analysis during sepsis evaluations, we also noticed practice variation among centers (7–49%), but the mean (24%) was similar to the reported 30% lumbar punctures performed in VLBW infants in other centers.15 In that report, approximately one third of VLBW infants with meningitis had negative blood cultures, whereas in our cohort it was more than half (53%). Our data support that urine and CSF cultures should be considered at the time of sepsis workups in VLBW infants, since negative blood cultures do not rule out UTI or meningitis.16
Although the number of meningitis cases was relatively small, the HRC pattern was distinct from BSI and UTI in that the baseline HRC index was higher and, after rising around the time of diagnosis, it remained higher. Since heart rate variability is regulated by sympathetic and parasympathetic signals, this abnormal HRC pattern may indicate a stronger autonomic nervous system response to brain inflammation compared to systemic inflammation in bacteremia or focal inflammation in UTI or delayed diagnosis of meningitis. Future studies including cytokine or other inflammatory marker measurements with HRC indices may confirm this hypothesis.
Another difference we found in HRC index patterns is that infants receiving mechanical ventilation had a higher baseline and a smaller rise around the time of infection. The higher baseline may indicate a greater level of physiologic instability or increased sedation, reflected by lower heart rate variability. Since apnea is a common presenting sign of infection and the associated heart rate decelerations factor into the HRC index, it is not surprising that infants receiving mechanical ventilation have a smaller relative rise in the HRC index around the time of infection. Nonetheless, a significant rise in the HRC index occurs in some infants both on and off mechanical ventilation as much as 12–24 h prior to clinicians recognizing signs and starting antibiotics.
Although this report includes data on a large number of cultures in the largest RCT of VLBW infants published to date, several limitations deserve consideration. We did not have data on urinalysis or CSF cell counts or chemistries to substantiate the diagnosis of UTI or meningitis. In addition, the RCT had a pragmatic design with no mandate on when or how to perform a sepsis evaluation. Consequently, there was significant center variation in obtaining urine and CSF cultures at the time of blood culture for suspected infection, raising the possibility that UTI and meningitis were underdiagnosed in some centers. Finally, we included cases of CONS BSI, UTI, and meningitis if the culture was positive and antibiotics continued at least 5 days, and we did not have additional laboratory values such as C-reactive protein to assess for an acute phase response. The diagnosis of CONS meningitis is controversial,17 and some cases included as CONS infection may represent contamination. However, some cases of meningitis in this cohort may have been associated with central nervous system shunts, where CONS are frequently isolated.18 Notably, the change in HRC index was not significantly different between CONS versus non-CONS infections.
A final consideration is that the HRC index was developed and externally validated as the fold increased chance of sepsis diagnosis within the next day for a VLBW infant, compared to the chance for all VLBW infants. As such, since on any given day the risk of infection is quite low, and since a high score may represent other pathologic processes, the HRC index is only one element to consider when deciding whether to administer antibiotics. In a single-center retrospective study of both term and preterm infants, elevated HRC scores were not uncommon and were usually not associated with sepsis;19 however, the lack of an accepted consensus definition for neonatal sepsis makes direct comparison between studies difficult.20 Another concern associated with the HRC index monitor is the possible increase in blood cultures and antibiotic administration. As previously reported, the tradeoff for 2% lower mortality in VLBW infants whose HRC index was displayed in the RCT was a 10% increase in blood cultures (p = 0.05) and a 5% increase in antibiotic days (p = 0.31) compared to the non-displayed group.4
Conclusion
The HRC index rises significantly in some VLBW infants prior to diagnosis of UTI or BSI. Cases of meningitis are less common, are associated with higher HRC index at baseline, and warrant further study to determine whether worsening HRC can assist in earlier detection.
References
Obladen, M. From "apparent death" to "birth asphyxia": a history of blame. Pediatr. Res. 83, 403–411 (2018).
Griffin, M. P. et al. Abnormal heart rate characteristics preceding neonatal sepsis and sepsis-like illness. Pediatr. Res. 53, 920–926 (2003).
Griffin, M. P. et al. Heart rate characteristics: novel physiomarkers to predict neonatal infection and death. Pediatrics 116, 1070–1074 (2005).
Moorman, J. R. et al. Mortality reduction by heart rate characteristic monitoring in very low birth weight neonates: a randomized trial. J. Pediatr. 159, 900–906 (2011).
Fairchild, K. et al. Septicemia mortality reduction in neonates in a heart rate characteristics monitoring trial. Pediatr. Res. 74, 570–575 (2013).
Fairchild, K. D. et al. Endotoxin depresses heart rate variability in mice: cytokine and steroid effects. Am. J. Physiol. Regul. Integr. Comp. Physiol. 297, R1019–R1027 (2009).
Stoll, B. J. et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics 110, 285–291 (2002).
Greenberg, R. G. et al. Late-onset sepsis in extremely premature infants: 2000-2011. Pediatr. Infect. Dis. J. 36, 774–777 (2017).
Stoll, B. J. & Hansen, N. Infections in VLBW infants: studies from the NICHD Neonatal Research Network. Semin. Perinatol. 27, 293–301 (2003).
Weitkamp, J. H., Ozdas, A., LaFleur, B. & Potts, A. L. Fluconazole prophylaxis for prevention of invasive fungal infections in targeted highest risk preterm infants limits drug exposure. J. Perinatol. 28, 405–411 (2008).
Riskin, A. et al. Is it justified to include urine cultures in early (<72 h) neonatal sepsis evaluations of term and late preterm infants? Am. J. Perinatol. 30, 499–504 (2013).
Tamim, M. M., Alesseh, H. & Aziz, H. Analysis of the efficacy of urine culture as part of sepsis. Pediatr. Infect. Dis. J. 22, 805–808 (2003).
Drumm, C. M., Siddiqui, J. N., Desale, S. & Ramasethu, J. Urinary tract infection is common in VLBW infants. J. Perinatol. 39, 80–85 (2019).
Bauer, S. et al. Urinary tract infection in very low birth weight preterm infants. Pediatr. Infect. Dis. J. 22, 426–430 (2003).
Stoll, B. J. et al. To tap or not to tap: high likelihood of meningitis without sepsis among very low birth weight infants. Pediatrics 113, 1181–1186 (2004).
Garges, H. P. et al. Neonatal meningitis: what is the correlation among cerebrospinal fluid cultures, blood cultures, and cerebrospinal fluid parameters? Pediatrics 117, 1094–1100 (2006).
Isaacs, D., on behalf of the Australasian Study Group For Neonatal Infections. A ten year, multicentre study of coagulase negative staphylococcal infections in Australasian neonatal units. Arch. Dis. Child. Fetal Neonatal Ed. 88, F89–F93 (2003).
Duhaime, A. C. Evaluation and management of shunt infections in children with hydrocephalus. Clin. Pediatr. 45, 705–713 (2006).
Wynn, J. L. Defining neonatal sepsis. Curr. Opin. Pediatr. 28, 135–140 (2016).
Coggins, S. A. et al. Heart rate characteristic index monitoring for bloodstream infection in an NICU: a 3-year experience. Arch. Dis. Child. Fetal Neonatal Ed. 101, F329–F332 (2016).
Acknowledgements
We thank the parents for allowing their infants to participate in this study. The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the Medical Predictive Science Corporation (MPSC). HeRO trial sites were Wake Forest University, University of Alabama at Birmingham, University of Miami/Jackson Memorial Hospital, Vanderbilt University Medical Center, Greenville South Carolina Hospital System, Winnie Palmer Children’s Hospital, Pennsylvania State University, and University of Virginia.
Author information
Authors and Affiliations
Contributions
Each author has met the Pediatric Research authorship requirements as listed: Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: J.L.A., W.A.C., E.B., J.A.P., C.T.N., R.L.S., M.W.W., P.P., T.M.O., C.P., D.E.L., K.D.F. Drafting the article or revising it critically for important intellectual content and final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Competing interests
D.E.L. has equity shares and is a consultant for Medical Predictive Science Corporation; all the other authors do not declare any conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Results of this work have been displayed in part during a platform presentation at the Annual Meeting of the American Pediatric Society and Society for Pediatric Research, in Toronto, Canada, in May 2018.
Supplementary information
Rights and permissions
About this article
Cite this article
Weitkamp, JH., Aschner, J.L., Carlo, W.A. et al. Meningitis, urinary tract, and bloodstream infections in very low birth weight infants enrolled in a heart rate characteristics monitoring trial. Pediatr Res 87, 1226–1230 (2020). https://doi.org/10.1038/s41390-019-0701-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0701-4
This article is cited by
-
Neonatal sepsis and cardiovascular dysfunction I: mechanisms and pathophysiology
Pediatric Research (2023)
-
Vital signs as physiomarkers of neonatal sepsis
Pediatric Research (2022)
-
Fetal heart rate variability is a biomarker of rapid but not progressive exacerbation of inflammation in preterm fetal sheep
Scientific Reports (2022)
-
Vital sign metrics of VLBW infants in three NICUs: implications for predictive algorithms
Pediatric Research (2021)