Abstract
Background
Retinol-binding protein 4 (RBP-4) is an adipokine involved in regulating insulin sensitivity which would affect fetal growth. It is unclear whether RBP-4 is associated with fetal overgrowth, and unexplored which fetal growth factor(s) may mediate the association.
Methods
In the Shanghai Birth Cohort, we studied 125 pairs of larger-for-gestational-age (LGA, birth weight >90th percentile, an indicator of fetal overgrowth) and optimal-for-gestational-age (OGA, 25–75th percentiles) control infants matched by sex and gestational age. We measured cord blood concentrations of RBP-4, insulin, proinsulin, insulin-like growth factor-I (IGF-I), and IGF-II.
Results
Cord blood RBP-4 concentrations were elevated in LGA vs. OGA infants (21.9 ± 6.2 vs. 20.2 ± 5.1 µg/ml, P = 0.011), and positively correlated with birth weight z score (r = 0.19, P = 0.003), cord blood proinsulin (r = 0.21, P < 0.001), IGF-I (r = 0.24, P < 0.001), and IGF-II (r = 0.15, P = 0.016). Adjusting for maternal and neonatal characteristics, each SD increment in cord blood RBP-4 was associated with a 0.28 (0.12–0.45) increase in birth weight z score (P < 0.001). Mediation analyses showed that IGF-I could account for 31.7% of the variation in birth weight z score in association with RBP-4 (P = 0.01), while IGF-II was not an effect mediator.
Conclusions
RBP-4 was positively associated with fetal overgrowth. IGF-I (but not IGF-II) may mediate this association.
Similar content being viewed by others
Introduction
RBP-4 is a soluble 21 kDa polypeptide with a binding site for retinol encoded by the RBP-4 gene localized at the chromosome 10q23-q24.1 It is synthesized mainly in adipose tissue and the liver, and is bound to retinol and transthyretin in the circulation.2,3 RBP-4 acts on the muscle and liver inhibiting glucose uptake in muscle tissues and glucose production in the liver in either a retinol-dependent or -independent way, and may be involved in the development of insulin resistance.4,5 Overexpression of RBP-4 has been associated with type 2 diabetes mellitus, gestational diabetes mellitus (GDM), obesity, insulin resistance, metabolic syndrome, polycystic ovary syndrome, and cardiovascular diseases.6,7,8,9,10,11 Since fetal growth would be affected by the sensitivity to the growth promoting effects of insulin and insulin-like growth factors (IGF), it is plausible that RBP-4 levels in mothers and fetuses may be associated with fetal growth.
Elevated maternal circulating levels of RBP-4 have been associated with fetal overgrowth12—a condition linked to increased risk of the metabolic syndrome related disorders such as type 2 diabetes,13,14 obesity15,16, and insulin resistance17,18 in adulthood. Several small studies (n < 100 in study groups) have been conducted to investigate the association between cord blood RBP-4 concentration and fetal growth, and most studies (3/4) reported a positive correlation.11,19,20,21 A small study has linked fetal overgrowth (n = 21) to elevated cord blood RBP-4 levels.20 In the present study, we sought to validate the hypothesis that fetal overgrowth is associated with elevated cord blood RBP-4 levels in a large cohort. Furthermore, we sought to assess for the first time whether any association between cord blood RBP-4 and fetal overgrowth may be mediated by specific fetal growth factors.
Methods
Study design
This study was based on the recently described Shanghai Birth Cohort (SBC).22 The SBC is a large, carefully phenotyped pregnancy/birth cohort with linked biospecimen bank for studies on perinatal determinants of infant growth, development and health outcomes. Women at both preconception and early pregnancy visits were recruited from six urban university-affiliated tertiary obstetric care hospitals in Shanghai between 2013 and 2016. There were a total of 4127 pregnancies and 3692 live births. The women were followed up at the first, second, and third trimesters of pregnancy and delivery. Data and specimens were collected at each study visit. All collected blood samples (maternal and cord blood; in EDTA tubes for plasma, in tubes without coagulants for serum) were kept on ice, stored temporarily in a 4 °C refrigerator and centrifuged within 2 h after the specimen collection. The separated serum and plasma samples were stored in multiple aliquots at −80 °C until assays. The study was approved by the research ethics committees of Shanghai Xinhua hospital (the coordination center, ref no. M2013-010) and all participating hospitals. Written informed consent was obtained from all study participants.
Birth weight was measured by a standardized electronic weighing scale to the nearest gram. Birth length was measured by a standardized measurement frame to the nearest 0.1 cm. Birth weight z scores were calculated using the Chinese sex- and gestational age-specific birth weight standards.23 Birth length z scores were calculated using the sex- and gestational age-specific reference values (means and SDs) based on the data on all singleton live births in the SBC cohort since there are no published birth length reference standards for Chinese infants.
A nested LGA study was conducted as part of the original SBC research protocol. LGA was defined as birth weight >90th percentile, according to the Chinese sex- and gestational age-specific birth weight standards.23 All study infants (LGA and controls) must meet the following inclusion criteria: (1) Han ethnicity (the majority ethnic group, >98%); (2) maternal age 20–45 years; (3) singleton infants of mothers without severe pre-pregnancy illnesses (e.g., pre-existing diabetes, essential hypertension, etc.), preeclampsia, eclampsia or other life-threatening pregnancy complications; (4) infants who were conceived without the use of artificial reproductive technology; (5) infants without any known birth defects; (6) gestational age at delivery >35 weeks (avoiding the confounding effect of severe prematurity); (7) cord blood specimen available for biomarker assays. All LGA infants met the inclusion criteria were included (n = 125). Controls were optimal-for-gestational-age (OGA, birth weight 25–75th percentiles) infants matched (1:1) to LGA infants by sex and gestational age (within 7 days) at delivery. The controls were randomly sampled from all eligible OGA infants in the SBC cohort. Therefore, a total of 125 matched pairs of LGA and control infants constituted the final study sample. The flowchart in the selection of study subjects is presented in Fig. 1.
Biochemical assays
Plasma RBP-4 was measured by an enzyme-linked immunosorbent assay (ELISA) kit (R&D system, Minnesota, USA), and the absorbance was determined using a microplate spectrophotometer (Beckman CX7, USA). Serum insulin and insulin-like growth factor 1 (IGF-I) concentrations were detected by chemiluminescent assays (ADVIA Centaur and Immulite2000, SIEMENS, Germany). Plasma IGF-II was measured by an ELISA kit from R&D system (Minnesota, USA), and plasma proinsulin by an ELISA kit from Mercodia system (Uppsala, Sweden), respectively. The detection limits were 0.22 ng/ml for RBP-4, 3.5 pmol/l for insulin, 1.7 pmol/l for proinsulin, 25 ng/ml for IGF-I, and 1.88 pg/ml for IGF-II, respectively. Intra-assay and inter-assay coefficients of variation were in the ranges of 2.0–6.5% for insulin and IGF-I, 5.0–8.6% for RBP-4 and proinsulin, and 2.4–9.3% for IGF-II, respectively. In all biomarker assays, the lab. technicians were blinded to the clinical status of study subjects.
Effect mediators
The primary associations of interest were whether LGA is associated with elevated cord blood RBP-4 levels, and whether any association between RBP-4 and fetal overgrowth may be mediated by fetal growth factors including insulin, proinsulin (a precursor to insulin), IGF-I, and IGF-II.
Statistical analysis
Data are presented as mean ± SD (standard deviation) and median (interquartile range) for continuous variables and frequency (percentage) for categorical variables. Pearson partial correlation coefficients were calculated to assess the associations between cord blood RBP-4 and fetal growth factors in log-transformed data controlling for gestational age at blood sampling. Generalized linear models were applied to assess the associations of cord blood RBP-4 and fetal growth factors with fetal growth (birth weight and length z scores) controlling for co-variables (potential confounders). The co-variables included maternal age (<35 or ≥35 years), primiparity (yes/no), education (university: yes or no), smoking (yes/no) or alcohol drinking (yes/no) during pregnancy, pre-pregnancy body mass index (BMI, kg/m2), family history of diabetes (yes/no), gestational hypertension (yes/no), gestational diabetes mellitus (yes/no), mode of delivery (cesarean/vaginal), infant sex (male/female), and gestational age at delivery (weeks). Co-variables that were not associated with the outcomes at P > 0.2 and did not affect the comparisons or effect estimates were excluded in the final models. There were no significant interactions (tests of multiplicative terms in generalized linear models) between variables affecting the regression models. To facilitate comparisons of effect sizes, we estimated the changes in birth weight and length z scores per SD increment in biomarkers. Mediation analyses were conducted to assess the potential mediation effects of fetal growth factors in the associations of cord plasma RBP-4 with birth weight and birth length z scores using the product (“Baron and Kenney”) method.24 Data management and analyses were conducted in SAS version 9.4 (SAS Institute, Cary, NC). Two-tailed P value < 0.05 was considered statistically significant in testing the primary hypothesis on the difference in cord blood RBP-4 concentration between LGA and control groups. P < 0.0125 was considered statistically significant in tests for the mediation effects of insulin, proinsulin, IGF-I, and IGF-II in the association of RBP-4 with birth weight z score—the indicator for defining LGA (Bonferroni correction for four tests).
Results
Maternal and infant characteristics
Table 1 presents maternal, delivery/neonatal characteristics of the study groups. Comparing LGA vs. OGA infants, there were no significant differences in maternal age, ethnicity, parity, education, smoking, family history of diabetes, and gestational age at delivery. Women bearing a LGA infant had higher pre-pregnancy BMI (mean: 22.3 vs. 21.3 kg/m2), and were more likely to have a cesarean section (61.4% vs. 26.3%). As expected, birth weight and birth length were substantially higher in LGA infants.
Cord blood RBP-4 and fetal growth factors
Adjusting for maternal and neonatal characteristics, LGA infants had significantly higher cord blood concentrations of RBP-4 (mean: 21.9 vs. 20.2 μg/ml, adjusted P = 0.011), insulin (40.7 vs. 33.2 pmol/l, P = 0.008), proinsulin (32.2 vs. 20.8 pmol/l, P = 0.004), IGF-I (89.9 vs. 68.4 ng/ml, P < 0.001), and IGF-II (202.6 vs. 187.8 ng/ml, P = 0.007) (Table 2).
Correlations
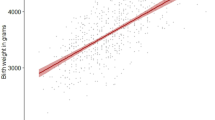
There were no significant interactions between LGA status and cord RBP-4 in relation to fetal growth factors (tests for interactions, all P > 0.1). Therefore, the correlations were reported for all study subjects together. Adjusting for gestational age at blood sampling, cord blood RBP-4 was positively correlated with birth weight z score (r = 0.19, P = 0.003) and cord blood proinsulin (r = 0.21, P < 0.001), IGF-I (r = 0.24, P < 0.001), and IGF-II (r = 0.15, P = 0.016) (Table 3, Fig. 2). There was a positive and weak non-significant correlation between cord blood RBP-4 and birth length z score (r = 0.12, P = 0.07).
Adjusted associations
Adjusting for maternal and delivery characteristics, each SD increment in cord blood RBP-4 was associated with a 0.28 (95% CI: 0.12–0.45) increase in birth weight z score (P < 0.001) (Table 4). The corresponding numbers were 0.12 (−0.04, 0.27) for cord blood insulin (P = 0.148), 0.24 (0.09, 0.38) for proinsulin (P = 0.002), 0.42 (0.26, 0.57) for IGF-I (P < 0.001), and 0.16 (−0.01, 0.33) for IGF-II (P = 0.07), respectively. Based on these standardized regression coefficients, IGF-I was most strongly associated with fetal growth (birth weight or length z score). Proinsulin, IGF-I, and IGF-II were all positively associated with birth length z score (all P < 0.05).
Mediation analyses
Mediation analyses observed mediation effects of cord blood IGF-I and proinsulin in the association of RBP-4 with birth weight z score (Table 4), but only IGF-I remained statistically significant if accounting for multiple tests for mediation effects. IGF-I and proinsulin could account for 31.7% and 20.6%, respectively, of the variation in birth weight z score in association with RBP-4. With adjustment for maternal and neonatal characteristics only, for each SD increment in RBP-4, birth weight z score increased by 0.28. When we added IGF-I z score into the model, the effect estimate for RBP-4 was attenuated by 29% (from 0.28 to 0.20) and remained significant (p = 0.017). When we introduced proinsulin z score instead into the model, the effect estimate for RBP-4 was attenuated by 18% (from 0.28 to 0.23) and remained significant (p = 0.009). The mediated effect was 0.09 (95% CI: 0.02, 0.15) for IGF-I, and 0.06 (95% CI: 0.001, 0.1) for proinsulin, in the association of cord RBP-4 with birth weight z score, respectively. When we added both IGF-I and proinsulin into the model, the effect estimate for RBP-4 was attenuated by 38% (from 0.29 to 0.18) and remained significant (p = 0.029). There were no significant effect mediations of insulin and IGF-II in the association of RBP-4 with birth weight z score. There was some indication of a mediation effect of IGF-I in the association of RBP-4 with birth length z score (p = 0.039) which was not significant if accounting for multiple tests.
Discussion
Main findings
Fetal overgrowth, as indicated by being LGA, was associated with elevated cord blood RBP-4 concentrations. Our study is the first to demonstrate that the positive association between RBP-4 and fetal overgrowth may be mediated by IGF-I.
Data interpretation and comparisons to findings in previous studies
Fetal growth is affected by maternal nutritional, environmental and metabolic factors, fetal genetic potential and intrauterine endocrine factors.25 RBP-4 is an adipokine involved in the regulation of insulin sensitivity.4,26,27 A small study reported a positive association between fetal overgrowth (n = 21) and cord blood RBP-4.20 Our data confirmed this association in a large Chinese birth cohort. Our data suggest that fetal growth factors may mediate the association between RBP-4 and fetal growth. Mediation analyses showed that cord blood IGF-I and proinsulin (a precursor to insulin) were potential mediators in the positive correlation between RBP-4 and birth weight z score (Fig. 3), and IGF-I remained significant after accounting for multiple tests. Higher levels of RBP-4 are associated with lower insulin sensitivity;6 this may induce some compensated increased secretion of insulin and IGFs which are key fetal growth factors28,29 driving enhanced fetal growth. Indeed, cord blood RBP-4 was positively correlated to proinsulin, IGF-I, and IGF-II. Mediation analyses suggest that IGF-I may be a key player in mediating the positive association of RBP-4 with fetal growth.
Our findings suggest the possible involvement of RBP-4 in the regulation of fetal growth, suggesting that RBP-4 may play an important role in metabolic health homeostasis during fetal life. Previous studies have suggested that RBP-4 may have a regulatory role in glucose homeostasis: (1) overexpression of RBP-4, or injection of recombinant RBP-4 in normal mice induces insulin resistance;4 (2) insulin resistance is associated with elevated RBP-4 level in humans.4
It should be cautioned that the current observational study could not differentiate whether elevated cord blood RBP-4 levels are a cause, consequence, or accomplice of fetal overgrowth. An alternative possibility is that fetal overgrowth may cause elevated cord blood RBP-4 levels. Also, the observed absolute differences in cord blood RBP-4 levels are relatively modest between LGA and OGA infants (mean difference = 8%), suggesting that RBP-4 is of much less clinical utility than IGF-I (mean difference = 31%) in differentiating infants with excessive vs. normal fetal growth.
Strengths and limitations
The main strengths of the study include the prospective large birth cohort, timely collection and processing of blood specimens and high-quality biochemical assays (low inter-assay and intra-assay coefficients of variation). The main limitation is the observational nature of the study. We could not rule out the possibility of reverse causality. Also, the study is limited to Chinese Han ethnicity subjects. While this confers the advantage of enhanced power to uncover biological relationships in the absence of the potential confounding effects of race/ethnicity, it also calls for more studies in other race/ethnic groups to understand the generalizability of the study findings.
Conclusions
RBP-4 was positively associated with fetal overgrowth. This association may be mediated by IGF-I (but not IGF-II).
References
Esteve, E., Ricart, W. & Fernandez-Real, J. M. Adipocytokines and insulin resistance: the possible role of lipocalin-2, retinol binding protein-4, and adiponectin. Diabetes Care 32, S362–S367 (2009).
Zabetian-Targhi, F., Mahmoudi, M. J., Rezaei, N. & Mahmoudi, M. Retinol binding protein 4 in relation to diet, inflammation, immunity, and cardiovascular diseases. Adv. Nutr. 6, 748–762 (2015).
Noy, N., Li, L., Abola, M. V. & Berger, N. A. Is retinol binding protein 4 a link between adiposity and cancer? Horm. Mol. Biol. Clin. Investig. 23, 39–46 (2015).
Yang, Q. et al. Serum retinol binding protein 4 contributes to insulin resistance in obesity and type 2 diabetes. Nature 436, 356–362 (2005).
Abel, E. D. et al. Adipose-selective targeting of the GLUT4 gene impairs insulin action in muscle and liver. Nature 409, 729–733 (2001).
Graham, T. E. et al. Retinol-binding protein 4 and insulin resistance in lean, obese, and diabetic subjects. N. Engl. J. Med. 354, 2552–2563 (2006).
Lin, C. C. et al. Relationship between serum retinol-binding protein 4 and visfatin and the metabolic syndrome. Diabetes Res. Clin. Pr. 85, 24–29 (2009).
Solini, A., Santini, E., Madec, S., Rossi, C. & Muscelli, E. Retinol-binding protein-4 in women with untreated essential hypertension. Am. J. Hypertens. 22, 1001–1006 (2009).
Olszanecka-Glinianowicz, M. et al. Are plasma levels of visfatin and retinol-binding protein 4 (RBP4) associated with body mass, metabolic and hormonal disturbances in women with polycystic ovary syndrome? Eur. J. Obstet. Gynecol. Reprod. Biol. 162, 55–61 (2012).
Aeberli, I. et al. Serum retinol-binding protein 4 concentration and its ratio to serum retinol are associated with obesity and metabolic syndrome components in children. J. Clin. Endocrinol. Metab. 92, 4359–4365 (2007).
Chan, T. F. et al. Increased serum retinol-binding protein 4 concentrations in women with gestational diabetes mellitus. Reprod. Sci. 14, 169–174 (2007).
Mazaki-Tovi, S. et al. Retinol-binding protein 4: a novel adipokine implicated in the genesis of LGA in the absence of gestational diabetes mellitus. J. Perinat. Med. 38, 147–155 (2010).
Rich-Edwards, J. W. et al. Birthweight and the risk for type 2 diabetes mellitus in adult women. Ann. Intern Med. 130, 278–284 (1999).
Harder, T., Rodekamp, E., Schellong, K., Dudenhausen, J. W. & Plagemann, A. Birth weight and subsequent risk of type 2 diabetes: a meta-analysis. Am. J. Epidemiol. 165, 849–857 (2007).
Ogonowski, J., Miazgowski, T., Engel, K. & Celewicz, Z. Birth weight predicts the risk of gestational diabetes mellitus and pregravid obesity. Nutrition 30, 39–43 (2014).
Zhao, Y., Wang, S. F., Mu, M. & Sheng, J. Birth weight and overweight/obesity in adults: a meta-analysis. Eur. J. Pediatr. 171, 1737–1746 (2012).
Giapros, V. et al. Serum adiponectin and leptin levels and insulin resistance in children born large for gestational age are affected by the degree of overweight. Clin. Endocrinol. 66, 353–359 (2007).
Evagelidou, E. N. et al. Prothrombotic state, cardiovascular, and metabolic syndrome risk factors in prepubertal children born large for gestational age. Diabetes Care 33, 2468–2470 (2010).
Giacomozzi, C. et al. Retinol-binding protein 4 in neonates born small for gestational age. J. Endocrinol. Invest. 33, 218–221 (2010).
Chan, T. F. et al. The positive correlation between cord serum retinol-binding protein 4 concentrations and fetal growth. Gynecol. Obstet. Invest. 72, 98–102 (2011).
Laudes, M. et al. Human fetal adiponectin and retinol-binding protein (RBP)-4 levels in relation to birth weight and maternal obesity. Exp. Clin. Endocrinol. Diabetes 117, 146–149 (2009).
Zhang, J. et al. Cohort profile: the Shanghai Birth Cohort. Int J. Epidemiol. 48, 21–21g (2019).
Zhu, L. et al. Chinese neonatal birth weight curve for different gestational age. Zhonghua Er Ke Za Zhi 53, 97–103 (2015).
VanderWeele, T. J. Mediation analysis: a practitioner’s guide. Annu Rev. Public Health 37, 17–32 (2016).
Langer, O. Fetal macrosomia: etiologic factors. Clin. Obstet. Gynecol. 43, 283–297 (2000).
Yao-Borengasser, A. et al. Retinol binding protein 4 expression in humans: relationship to insulin resistance, inflammation, and response to pioglitazone. J. Clin. Endocrinol. Metab. 92, 2590–2597 (2007).
Kotnik, P., Fischer-Posovszky, P. & Wabitsch, M. RBP4: a controversial adipokine. Eur. J. Endocrinol. 165, 703–711 (2011).
Gluckman, P. D. & Pinal, C. S. Regulation of fetal growth by the somatotrophic axis. J. Nutr. 133, S1741–S1746 (2003).
Luo, Z. C. et al. Maternal and fetal IGF-I and IGF-II levels, fetal growth, and gestational diabetes. J. Clin. Endocrinol. Metab. 97, 1720–1728 (2012).
Acknowledgements
We gratefully acknowledged all research staff who had contributed to patient recruitment and data collection in the Shanghai Birth Cohort. This work was accepted for presentation in abstract form at the DOHaD 2019 World Congress in Melbourne, Australia, October 20–23, 2019. Supported by research grants from the National Natural Science Foundation of China (81571451 and 81673178 to Z.C.L. and F.O.), the Canadian Institutes of Health Research (158616 to Z.C.L.), the Shanghai Municipal Health and Family Planning Commission, Shanghai Jiao-Tong University 985 program, the National Human Genetic Resources Sharing Service Platform (2005DKA21300 to J.Z.) and the Ministry of Science and Technology of China National Key Research and Development Program (2016YFC1000203 to J.Z.). The funders have no role in all aspects of the study, including study design, data collection, and analysis, the preparation of the manuscript and the decision for publication.
Shanghai Birth Cohort
Xiaoming Shen6, Hong Huang6, Kun Sun6, Jun Zhang6, Weiye Wang6, Weiping Xu6, Fengxiu Ouyang6, Lin Zhang6, Fei Li6, Yin Huang6, Jinsong Zhang6, Chonghuai Yan6, Lisong Shen6, Yixiao Bao6, Ying Tian7, Weiwei Chen8, Huijuan Zhang8, Chuanliang Tong8, Jian Xu8, Yiwen Zhang9, Fang Jiang9, Xiaodan Yu9, Guangjun Yu10, Jinjin Chen10, Yu Zhang11, Xiaotian Li12, Haidong Cheng12, Qinying Zhang12, Tao Duan13, Jing Hua13 and Hua Peng14
Author information
Authors and Affiliations
Consortia
Contributions
G.H.Z., Y.N.G., X.H., J.Z., F.O., and Z.C.L. conceived the study. M.N.Y., G.H.Z., K.D., W.J.W., Y.D., H.H., H.C.C., Y.N.G., J.Z., F.O., X.L.H., and Z.C.L. contributed to the acquisition of the research data. W.J.W., H.H., and H.C.C. conducted the data analysis. W.J.W., G.H.Z., and H.C.C. conducted the literature review and drafted the manuscript. All authors contributed to data interpretation, revised the article critically for important intellectual content, and approved the final version for publication. Z.C.L. is the guarantor taking full responsibility for the work as a whole.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was approved by the research ethics board of Shanghai Xinhua Hospital (the coordination center, ref no. M2013-010, approved on August 23, 2013).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, MN., Zhang, GH., Du, K. et al. Retinol-binding protein 4, fetal overgrowth and fetal growth factors. Pediatr Res 87, 946–951 (2020). https://doi.org/10.1038/s41390-019-0685-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0685-0