Abstract
Backgrounds
To investigate the potential mechanism of hypospadias induced by DEHP in rats to reveal the preventative effect of TGF-β1 in hypospadias induced by DEHP via the reduction of EMT.
Methods
Time-mated Sprague-Dawley rats underwent cesarean section, and the penises of male pups were collected after exposure to corn oil or DEHP to establish a rat model of hypospadias and to further study the molecular mechanisms of hypospadias in vivo. In addition, the penises were cultured and treated with MEHP or MEHP+TGF-β1 in vitro. Subsequently, histomorphology and elements in TGF-β/Smad signaling pathway changes were evaluated using scanning electron microscopy, immunofluorescence, polymerase chain reaction, and western blot.
Results
The development of rat penis and urethral seam fusion were delayed after the treatment with DEHP in vivo or MEHP in vitro compared with the Control group. Moreover, TGF-β1, Smad2/Smad3, and the mesenchymal biomarkers, including α-SMA, N-cadherin, and Vimentin, were decreased. However, the epithelial biomarkers, including E-cadherin, ZO-1, β-catenin, and occludin, were increased. In addition, TGF-β1 could relieve all of the above changes.
Conclusion
Gestational DEHP exposure could lead to hypospadias by reducing urethral EMT. Moreover, TGF-β1 could prevent it by regenerating EMT through activating the TGF-β/Smad signal pathway.
Similar content being viewed by others
Introduction
Hypospadias, a common congenital urogenital malformation, is a defect in the normal development of the foreskin, urethra, and ventral aspect of the penis with a morbidity of 1/200–1/300 infant males and has displayed an increasing trend with each year.1,2,3 As is widely known, hypospadias can only be treated by surgery.1 Nevertheless, many unavoidable complications, such as fistula and stricture, remain to threaten the quality of life in these children.4 In addition, its precise etiology is largely unknown. Therefore, seeking the mechanism of hypospadias is urgently needed for prevention. Recent advancements in molecular biology and microarray technology demonstrated that the doubling incidence of hypospadias was potentially related to environmental endocrine disruptors, which might have an estrogen-like or anti-androgen effect and could interfere with the body’s endocrine system to produce adverse developmental, reproductive, neurological, and immune effects in both humans and wildlife.5,6 Diethylhexyl phthalate (DEHP) is a plasticizer, which is used to soften polyvinylchloride plastics and non-polymers, and is a common endocrine disruptor that is largely produced and widely used in China.6 Previous studies have found that many routes of exposure to DEHP, including medical devices, furniture, food, or intake from water and air, were of concern to human health.7,8 Moreover, DEHP is difficult to biodegrade and gradually accumulates, which has an adverse accumulation effect on the offsprings and other organisms in the food chain, resulting in serious harm.9,10 Furthermore, prenatal DEHP exposure had been associated with the formation of congenital hypospadias in multiple animal studies.11,12
Several previous studies have contrasted and analyzed the gene expression levels between these organisms with or without the exposure of DEHP.13,14 The results have showed that exposure to DEHP could decrease the expression level of transforming growth factor (TGF)-β.13,15 The TGF-β family, as a powerful cytokine family, plays a significant role in numerous cell functions, including proliferation, differentiation, migration, and transduction in all tissues.16 Moreover, in the TGF-β/Smad signal pathway, TGF-β could activate Smad protein through phosphorylation, thereby regulating the downstream transforming factors, such as the epithelial–mesenchymal transition (EMT) signal pathway.17 EMT is an important process in urethra embryogenesis. EMT is a fundamental biological process by which epithelial cells shift to mesenchymal cells in order to generate or regenerate tissues. Upon EMT, epithelial cells, losing their cell–cell adhesion and polarity, undergo multiple biological changes that enable them to acquire some mesenchymal characters: non-polarized, lacking intercellular junctions, and moving throughout the extracellular matrix.18,19 Epithelial cells in the urethral seam remodel into mesenchymal cells after urethral plate fusion through EMT, as confirmed by our previous work.20 If disrupted, urethral seam fusion would retard, or even stop, resulting in the formation of hypospadias.21 In addition, EMT is regulated by the TGF-β/Smad signal pathway, and DEHP can suppress TGF-β expression; thus we speculated whether the mechanism of hypospadias induced by DEHP is related to the TGF-β/Smad signal pathway.22
In summary, the objective of our study is to explore the effects of DEHP regulating the TGF-β/Smad signal pathway through the targeting of EMT on the occurrence and development of hypospadias, as well as to evaluate the preventative effect of TGF-β1 in hypospadias induced by DEHP via the reduction of EMT.
Material and methods
Ethics statement and animals
Virginal Sprague-Dawley rats were obtained from the Experimental Animal Center of the Chongqing Medical University (Chongqing, China) [SPF, License No.: SCXK (Chongqing) 2017-0001] and raised at the Experimental Animal Center at the Children’s Hospital of Chongqing Medical University (Chongqing, China) [SPF, License No.: SYXK (Chongqing) 2017-0012]. Each female rat was mated with another single male adult rat at 5 p.m. The morning that the vaginal plug found was considered as embryonic day (ED) 0. These rats were housed in polycarbonate cages in a controlled environment with a 12 h light/12 h dark illumination schedule (7:00 a.m. light on/7:00 p.m. light off) and free access to water and food. The study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. All animal experimental procedures were approved by the ethics committee of Chongqing Medical University.
Dose selection and animal model
One hundred and eighty pregnant rats were, respectively, randomly divided into three groups each as follows: (1) Control group (n = 30); (2) DEHP500 group (n = 90); and (3) DEHP750 group (n = 60). Among them, the rats in the Control, DEHP500, and DEHP750 groups were intragastrically administrated with corn oil and DEHP at a dosage of 500 mg/kg/day and 750 mg/kg/day, respectively, from ED 12 to ED 18. Subsequently, on ED 19, all of the dams were anesthetized and the genital tubercle (GT) of male embryos was harvested. The gross image of GT was observed under anatomic microscope to distinguish hypospadiac rats, and the gender of the embryos was confirmed by sexual glands.
Penis culture
In the in vitro experiment, 50 pregnant Sprague-Dawley rats were raised until ED 16. The male pups were cesarean sectioned and their penises were extracted. All penises were divided into three groups: Control, monoethylhexyl phthalate (MEHP), and TGF-β groups. The penises were placed on cellulose membranes supported by stainless steel mesh in 35-mm dishes containing Dulbecco’s modified Eagle’s medium and 50 U/ml penicillin, 25 µg/ml streptomycin, 0.1 mg/ml ascorbic acid, and 10 nM dihydrotestosterone as described by Emily et al.23 and grown for 48 h in an incubator at 37 °C containing air supplemented with 5% CO2. The media of the MEHP group contained 500 µM MEHP, and the media of the TGF-β group contained 500 µM MEHP and 50 ng/ml growth factor TGF-β1.
Moreover, another 20 ED 16 penises were divided into four groups, including Control group (cultured in media containing no additive for 24 h), MEHP group (MEHP 500 µM for 24 h), pre-TGF-β group (MEHP 500 µM+growth factor TGF-β1 50 ng/ml for 24 h), and post-TGF-β group (MEHP 500 µM for 24 h and then TGF-β1 50 ng/ml for the next 24 h), respectively.
All cultured penises were recorded under anatomic microscope.
Scanning electronic microscopy
Penises from these rats in different groups in the in vivo experiment were fixed in glutaraldehyde for 2 days at 4 °C. All of the samples were washed with sodium cacodylate for 1 h, then sequentially dehydrated in 30, 50, 70, 90, and 100% (v/v) ethanol for 5 min each. Finally, specimens were visualized under scanning electron microscope (Hitachi-7500, Japan) after critical-point drying and gold-coating treatments.
Hematoxylin–eosin (HE) staining
The penises were 4% formalin fixed, dehydrated, and paraffin embedded and then serial transverse sectioned. The sections were underwent deparaffinization, hydration in alcohol gradient, and staining with HE successively. Images were observed under optical microscope.
Immunofluorescence—paraffin
After deparaffinization, hydration, and blockage in 5% bovine serum albumin (BSA) at room temperature, paraffin sections were incubated with the primary antibodies E-cadherin (labeling epithelial cells, CST, #14472, USA, 1:50), α-smooth muscle actin (α-SMA; labeling mesenchymal cells, Abcam, ab124964, UK, 1:300), zonula occludens 1 (ZO-1; labeling epithelial cells, Invitrogen, #61-7300, USA, 1:50) N-cadherin (labeling mesenchymal cells, Invitrogen, #33-3900, USA, 1:100), occludin (labeling epithelial cells, Invitrogen, #40-4700, USA, 1:250), and N-cadherin, at 4 °C overnight. On the second day, sections were washed with phosphate-buffered saline (PBS) for 5 min 3 times and then incubated by second antibodies for 1 h at room temperature. The nuclei were stained with 4,6-diamidino-2-phenylindole (DAPI). Samples were recorded under fluorescence microscope. Positively stained cells were counted from all the urethral seam areas of five cross-sections of three male pups in each group.
Immunofluorescence—freezing
All cultured penises were collected and 4% formalin fixed, then 10-µm frozen sections of the cultured penis were obtained with cryostat microtome. After permeabilization in 0.1% Triton X-100 in PBS for 10 min, sections were blocked in 0.5% BSA in PBS for 1 h at room temperature, followed by an overnight incubation of primary antibodies, E-cadherin and α-SMA, at 4 °C. Following a PBS wash, the sections were incubated with Cy3-conjugated goat anti-mouse (CW0145S, China) and 488-conjugated goat anti-rabbit (CW0159S, China) for 1 h at room temperature. The nuclei were stained with DAPI for 1 h. Images were obtained with an A1R confocal microscopy system (Nikon, Tokyo, Japan) and prepared with the Nikon NIS-element AR 4.0 software. Positively stained cells were counted from all the urethral seam areas of five cross-sections of three male pups in each group.
Quantitative real-time polymerase chain reaction (qRT-PCR)
Total mRNA of the penis was isolated using an RNA Extraction Kit (BioTeke, RP1202, China) and quantified by spectrophotometry at 260 nm, then reverted into cDNA by a Reverse Transcription Kit (TAKARA-RR037A, Japan) according to the manufacturer’s recommendations. The optimum annealing temperature (Tm) of each primer was analyzed in a 12.5-μl reaction volume containing 5 μl EmeraldAmp PCR Master Mix (TAKARA-RR300, Japan) using the Real-Time PCR system. Q-PCR was performed to confirm the expression of genes in the TGF-β/Smad signal pathway, including TGF-β1, Smad2, Smad3, Snail, Slug, E-cadherin, occludin, ZO-1, β-catenin, α-SMA, N-cadherin, and Vimentin, according to the manufacturer’s guidelines using SYBR Q-PCR Premix (TAKARA-RR820A, Japan). Q-PCRs were run using the following program: 98 °C, 2 min + (98 °C, 10 s + Tm 30 s + 72 °C, 30 s) × 35 cycles + 72 °C, 2 min. β-Actin was considered as an inner control to calculate the relative expression of those genes. All procedures were repeated three times.
Western blot
Total protein was extracted from the penises and quantitated according to the manufacturer’s specifications. Total protein extract was denatured in buffer at 100 °C for 10 min and separated by sodium dodecyl sulfate–polyacrylamide gel electrophoresis. Protein was transferred to a polyvinylidene fluoride membrane (Millipore, USA). After blocking with 5% fat-free milk, the membrane was incubated with the primary antibodies TGF-β1 (Abcam, ab92486, UK, 1:500), p-Smad2/Smad3 (CST, #8828, USA, 1:1000), Snail+Slug (Abcam, ab180714, UK, 1:1000), E-cadherin (1:1000), ZO-1 (1:1000), occluding (1:1000), β-catenin (Santa, sc-7199, USA, 1:1000), α-SMA (1:5000), N-cadherin (1:5000), Vimentin (Abcam, ab8978, UK, 1:500), and β-actin (Abcam, ab8226, UK, 1:5000) at 4 °C overnight, respectively. On the next day, the membrane was washed and incubated with secondary antibody at room temperature for 2 h, then detected by chemiluminescent reaction (Millipore, USA). The image collection and densitometric analysis were performed using the ImageJ version 1.44 analysis software.
Statistical analysis
All experiments were performed more than three times, and the data of this research were presented as the mean ± SD. Comparisons between groups were analyzed using one-way analysis of variance. A probability level of <0.05 (P < 0.05) was considered significant. The SPSS 22.0 statistical package was employed (SPSS, Inc., Chicago, USA).
Results
DEHP repressed urethral plate fusion, resulting in the formation of hypospadias in rats
After exposure to DEHP, the incidence of hypospadias in fetal male rats was 0.00, 27.58, and 36.21% in the Control, DEHP500, and DEHP750 groups, respectively. To investigate the toxicity effect of DEHP on the rat penis, a scanning electron microscope was used to observe the gross image of the fetal penis. It was a round and straight structure with a clear narrow urethral groove in the ventral part and a well-defined coronary sulcus that divided the shaft and glans penis in the Control group (Fig. 1a). However, in the ventral part of the penis in the DEHP500 group, a wide urethral groove was obvious, and the bilateral prepuce shrank like a quilt covering on the ventral penis (Fig. 1b). In addition, the prepuce could not enclose all of the spongiosum, leaving a V-shaped cleft in the ventral penis in the DEHP750 group (Fig. 1c). Particularly, the urethral opening was on the ventral side of the glans in the DEHP500 group (Fig. 1b) and on the ventral side of the penis in the DEHP750 group (Fig. 1c) but in the center of the glans in the Control group (Fig. 1a). Moreover, a transverse section was stained with HE to show the morphology of the inner structure at the same level of the penis in each group. In the Control group, the urethral plate was completely fused, and the urethra tube was fully formed (Fig. 1d). Nevertheless, in the DEHP500 group, the bilateral urethral plate was just touching, and the primary urethra opened toward the outside (Fig. 1e). In the DEHP750 group, the prepuce was deformed and became very thin compared with the Control group, and the ventral prepuce was missing with a remarkable defect (Fig. 1f). Therefore, we suggested that DEHP could induce the occurrence of hypospadias in rats through delaying urethral plate fusion.
Morphology of fetal penis at ED 19. Ventral view of embryonic genital tubercle in the Control group (a), DEHP500 group (b), and DEHP750 group (c) under SEM. Tail and lower limbs were removed. With an increase in the DEHP intervention dosage, a deepening of the ventral urethral groove and ventral shift of the urethral meatus could be seen. Especially in the DEHP750 group, the ventral prepuce was seriously defected and urethral meatus was in the middle shaft of the penis (c). HE staining of transverse sections at the same level of the penis are presented in the respective lower panels (d–f). Urethral plate fusion was delayed following exposure to DEHP (e); in the high dosage group, the urethral seam was totally destroyed and the urethral opening was toward the outside (indicated by the arrow) (e). um urethra meatus, ug urethral groove, us urethral seam, SEM scanning electron microscope, ED embryonic day, HE hematoxylin and eosin.
DEHP decreased the expression level of the EMT signal pathway
Pregnant rats were exposed to DEHP for a week, and then the expression of epithelial and mesenchymal relevant biomarkers was tested. In the Control group, some cells that co-expressed epithelial marker E-cadherin and mesenchymal marker α-SMA, ZO-1 (epithelial marker), and N-cadherin (mesenchymal marker) also confirmed the concurrence phenomenon. In the DEHP500 and DEHP750 groups, few cells expressed epithelial markers and simultaneously expressed mesenchymal markers (Fig. 2a, b). At the same level of the penis transverse section, we showed that DEHP noticeably increased the expression of epithelial protein; in contrast, the mesenchymal expression was downregulated in DEHP-exposed rats (Fig. 2c). In addition, a quantitative analysis of E-cadherin, ZO-1, N-cadherin, and α-SMA also verified these changes by western blot. All results indicated that EMT in urethral development was decreased in a model of hypospadias in these rats (Fig. 2d).
DEHP-induced expression changes of EMT in rat urethral seam. Immunofluorescent staining of urethral seam cells for EMT at ED 19 (a, c). Double immunofluorescence for epithelial marker E-cadherin and mesenchymal marker α-SMA (a, c, e) and epithelial marker ZO-1 and mesenchymal marker N-cadherin (b, d, f). In addition, when merged together, some cells co-expressed epithelial and mesenchymal markers (arrow) in the control group (a, b); however, a few cells positive for double staining were observed in the DEHP group (c–f), and nuclei were counterstained by DAPI. Positively stained cell count was analyzed to explain the significances (b). Western blot was used to analyze the expression of epithelial and mesenchymal markers (d). E-cadherin and ZO-1 expression were distinctly enhanced in the DEHP group compared with the Control group; however, N-cadherin and α-SMA apparently decreased. *p < 0.05 versus Control group, #p < 0.05 versus the DEHP500 group. DEHP diethylhexyl phthalate, EMT epithelial–mesenchymal transition, ED embryonic day, α-SMA α-smooth muscle actin, ZO-1 zonula occludens-1.
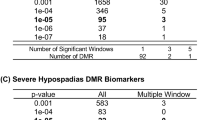
The TGF-β/Smad signaling pathway was inhibited in the rat model of hypospadias
Several signal pathways are involved in EMT. Among them, the TGF-β/Smad signaling pathway is the most pivotal and well known. The above results indicate that the EMT was decreased in a rat model of hypospadias, so we reasonably speculated that the decreased EMT might be regulated by TGF-β/Smad signaling pathway suppression. Through qRT-PCR, we tested that these mRNA expression levels of some factors in the signal pathway, including TGF-β1, Snail, Slug, α-SMA, Vimentin, and N-cadherin, were strikingly downregulated in the DEHP500 and DEHP750 groups compared with the Control group. However, the expression of E-cadherin, ZO-1, β-catenin, and occludin was upregulated. In addition, no significant changes were found in the expression levels of Smad2 and Smad3 (Fig. 3a). In addition, the same results were detected via western blot. Moreover, the expression levels of TGF-β1, p-Smad2/Smad3, Snail, Slug, α-SMA, Vimentin, and N-cadherin were conspicuously downregulated in the DEHP group compared with the Control group; however, E-cadherin, ZO-1, β-catenin, and occludin were upregulated (Fig. 3b). It suggested a role for TGF-β/Smad signal pathway in the reduction of EMT by DEHP.
Quantitative analysis of TGF-β/Smad signal pathway of penis at ED 19. qRT-PCR (a) and western blot (b) demonstrated that the TGF-β/Smad signal pathway was inhibited after the treatment of DEHP and TGF-β1. The transcription factors p-Smad2/Smad3, Snail, and Slug and the mesenchymal markers α-SMA, N-cadherin, and Vimentin were significantly downregulated; however, the epithelial markers E-cadherin, ZO-1, occludin, and β-catenin were upregulated. The mRNA expression levels of Smad2 and Smad3 did not have significant differences. *p < 0.05 versus the Control group, #p < 0.05 versus the DEHP500 group. ED embryonic day, Q-PCR quantitative polymerase chain reaction, TGF-β transforming growth factor beta, α-SMA α-smooth muscle actin, ZO-1 zonula occludens 1.
TGF-β1 could relieve EMT reduction in a rat model of hypospadias
Prenatal DEHP exposure could induce the occurrence of hypospadias in rats through delaying urethral plate fusion, while EMT was a significant mechanism during this process. A declining EMT trend was regulated by the TGF-β/Smad pathway. We wondered whether TGF supplement could reverse the formation of hypospadias. In an in vitro penis culture, the embryonic penis was similar in shape to a pagoda and the urethral groove was clearly visible on the ventral part. In the Control group, the orifice was located on the tip of penis, while in the MEHP group, the orifice was on the ventral glans. However, we found that the orifice moved to the tip after the TGF-β1 treatment (Fig. 4a panels (a–c)). At the same level of the transverse section, some cells in the urethral seam were co-expressing E-cadherin and α-SMA, which showed that these cells were undergoing EMT. However, few cells were undergoing EMT after exposure to MEHP. The expression level of the EMT was elevated in association with TGF-β1 activation (Fig. 4a panels d–f, b). Moreover, in the MEHP group, mesenchymal markers of the urethral seam were expressed more strongly than in the Control and TGF groups. The epithelial markers showed an inverse behavior (Fig. 4c). Western blot analysis further showed that the rats treated with TGF-β1 had a reversed DEHP-induced expression change of TGF-β1, Snail+Slug, p-Smad2/Smad3, E-cadherin, ZO-1, occludin, β-catenin, α-SMA, Vimentin, and N-cadherin, that is to say, the expression levels of TGF-β1, p-Smad2/Smad3, Snail, Slug, α-SMA, Vimentin and N-cadherin were notably upregulated in the TGF-β group compared with the MEHP group; however, E-cadherin, ZO-1, β-catenin, and occludin were downregulated (Fig. 4d). Thus a TGF-β1 supplement could lead to EMT recovery via the TGF-β/Smad signaling pathway in urethral seam formation in rats.
TGF-β1 could relieve the EMT reduction induced by MEHP. Morphology of the embryonic penis cultured for 48 h (a) from the Control group (a), MEHP group (b), and TGF-β group (c) under anatomic microscope. The urethral meatus was located in the lower ventral part of the penis in the MEHP group but much further toward the tip of the penis in the Control group and TGF-β group. Double immunofluorescent staining of transverse sections at the same level of the penis are presented in the respective lower panels (d–f). Cells co-expressing E-cadherin (red) and α-SMA (green) were found in the control (d) and TGF-β group (f) (showed as arrows) but not in the MEHP group (e). The positively stained cells between the Control and MEHP groups and between the MEHP and TGF-β groups had significant differences (b). Western blot further measured the expression level of epithelial and mesenchymal markers (c) and the expression change of factors in the TGF-β/Smad signal pathway in the cultured penis (d), which showed that the TGF-β/Smad signal pathway was inhibited when exposed to MEHP but that TGF-β1 could relieve the inhibition. *p < 0.05 versus the Control group, #p < 0.05 versus the MEHP group. um urethral meatus, ug urethral groove, MEHP mono-(2-ethylhexyl)-phthalate, EMT epithelial–mesenchymal transition, α-SMA α-smooth muscle actin, ZO-1 zonula occludens 1.
TGF-β1 could prevent the formation of hypospadias
After the treatment with MEHP or TGF-β1 for different time periods, diverse appearances were recorded under microscope. In the Control group, the urethral groove was clearly visible on the ventral part, and the orifice was located at the tip of the penis (Fig. 5a). However, the orifice was in the ventral glans with an obviously abnormal appearance in the MEHP group (Fig. 5b). In the group co-exposed to MEHP and TGF-β1, the orifice moved to the tip, and the outlook was nearly close to the Control group (Fig. 5c). In the group that was exposed to MEHP and 24 h later treated with TGF-β1, the exterior appearance returned to normal but the orifice remained at the ventral part of penis (Fig. 5d). It suggested that TGF-β1 could prevent the occurrence of hypospadias but could not treat the formed hypospadias.
TGF-β1 could prevent the formation of hypospadias induced by MEHP but could not remedy it. a In the Control group, the ventral urethral groove was clearly visible, and the urethral meatus opening was at the tip of the penis. b In the MEHP group, the penis crimpled without bilateral prepuce folds and the meatus was transferred ventrally following exposure to MEHP. c In the pre-TGF-β1 group, the outlook, meatus, and urethral groove were close to the Control after TGF-β1 rehabilitation. d In the post-TGF-β1 group, the exterior appearance approached normal with a pagoda feature; however, the meatus was similar to that in the MEHP group, locating ventrally. um urethral meatus, ug urethral groove.
Discussion
DEHP, one of the most commonly used plasticizers, is an ingredient in toys, medical tubing, blood storage bags, and cosmetics.24 DEHP has also been shown to exert adverse effects on the reproductive organs, liver, and kidney.25 In the pediatric population, numerous studies have reported that DEHP was found to induce a wide range of developmental and reproductive toxicities in the urogenital system of the fetus and significantly correlated with the occurrence of some congenital diseases, such as hypospadias and cryptorchidism.13,25,26,27,28,29 Gene mutation and endocrine disruption were taken into consideration as reasons.3 However, the concrete mechanism is not clear. Thus we investigated the mechanism by which DEHP induces hypospadias in rats and found a preventative effect of TGF-β1 in hypospadias induced by DEHP via the reduction of EMT.
The urethral plate is thought to be the signal center of the urethra, and perturbation of its development can induce congenital malformations.30 In this study, we first detected the morphology changes of the fetal rat penis and discovered that the ventral prepuce was malformed and the urethral meatus ventrally migrated. In addition, the transverse sections also showed urethral seam fusion retardation after exposure to DEHP in utero. In other words, the key process of hypospadias induced by DEHP focuses on the urethral plate and leads to the inhibition of urethral seam formation.21
Epithelial cell remodeling of the urethral plate is involved in urethral seam formation when urethral plate cells remodel into mesenchymal cells, resulting in urethral seam formation.20,21 We found that EMT played an important role in urethral seam formation.20 Therefore, whether urethral seam malformation is caused by aberrations of the EMT in urethral seam remains unknown. EMT is a pivotal process in urethral embryogenesis.20,21 Through the EMT, the urethral plate fuses and urethral seam forms to develop an intact urethra, which was confirmed by our previous study.20 EMT change was then investigated in our study. Using immunofluorescence staining and western blot, we revealed that both the expression levels of the EMT signal pathway and mesenchymal marker expression were downregulated in the DEHP group. The rat model of hypospadias showed that it decreased the EMT signal pathway, leading to urethral seam dysplasia.
Furthermore, we questioned how EMT was regulated in fetal hypospadiac rats. A variety of signal pathways could mediate EMT, such as TGF-β, Shh, Wnt, and others.31 Several researchers have found that TGF-β was decreased after DEHP treatment.13,22,32 Moreover, the expression of TGF-β1 was localized to the urethral epithelium, which suggested its involvement in urethral seam formation.33 Therefore, we presumed that the TGF-β/Smad signal pathway might play a greater role in EMT. With western blot, we verified that TGF-β1 and the TGF-β/Smad signal pathway were indeed downregulated in rats after exposure to DEHP. In vitro, the cultured penis with lesser EMT showed the ventral urethral meatus and a suppressed TGF-β/Smad signal pathway after adding MEHP (the DEHP metabolite, no need for liver and kidney metabolism). When supplied with TGF-β1, the EMT and other relevant signal pathways recovered. The above results indicate that DEHP could lead to the formation of hypospadias in rats by inhibiting urethral EMT through the TGF-β/Smad signaling pathway. In addition, TGF-β1 is a major regulator of the EMT process.
Several previous studies have found that TGF-β1 had lower expression in the prepuce of patients with hypospadias, which was in accordance with our results.17,34 We detected that the downregulated TGF-β1 inhibited EMT in urethral fetal development. Similarly, hypospadias in patients with a low expression level of TGF-β1 in clinical practice may also be caused by EMT reduction. Combined with this study, we found that, if EMT was interrupted, hypospadias would occur. Several researches have reported the relationship between hypospadias and TGF-β1.17,34 Baskin et al.35 suggested that TGF-β signaling was important for the induction and regulation of urethral tube development using gene array. In addition, the relevant proteins in the TGF-β signaling pathway might be involved in regulating palate fusion in mammals.33 Ulrich verified that the EMT is a multigenic cellular response to TGF-β superfamily members and not another signal pathway.36 In accordance with this study, those findings predicted that TGF-β1 was a candidate gene of hypospadias. This might provide new insight into the mechanism of hypospadias.
From the results above, we could predict the exact effect of TGF-β1 in preventing hypospadias. In addition, we questioned whether TGF-β1 can relieve the formation of hypospadias. After exposure to MEHP followed by treatment with TGF-β1, the ventrally transferred meatus was not strikingly reversed to the tip. Thus TGF-β1 could not rectify the established malformation of hypospadias. However, the outlook of the penis slightly returned to normal. In brief, we could not conclude a treatment effect for TGF-β1 in hypospadias induced by MEHP. The intervention time point and dosage of TGF-β1 could impact treatment outcomes. Therefore, we need to continue to explore the therapeutic application of TGF-β1 in the formation of hypospadias in our next work.
Through in vivo and in vitro experiments, we identified the following mechanisms involved in hypospadias: abnormalities in urethral seam formation and remodeling could explain the occurrence of hypospadias, and urethral seam malformation was caused by EMT reduction that was regulated by the TGF-β/Smad signal pathway, which could be prevented by TGF-β1. Therefore, we speculated that TGF-β1 was a major regulator of the EMT process in urethral fetal development.
In conclusion, EMT plays an important role in urethral seam fusion. Once disrupted, hypospadias would occur, and gestational DEHP exposure could lead to hypospadias through inhibiting urethral EMT mediated by the TGF-β/Smad signal pathway. In addition, TGF-β1 could relieve the EMT reduction through activating TGF-β/Smad signal pathway, showing that TGF-β1 might help prevent the occurrence of hypospadias by regenerating EMT through activating TGF-β/Smad signal pathway. Therefore, we suggest that TGF-β1 is a pivotal gene involved in the formation of hypospadias (Fig. 6).
The mechanism of hypospadias induced by DEHP in rats. The mechanism of hypospadias induced by DEHP was unknown (a → d). DEHP entered the body through various routes (a); gestational DEHP exposure could inhibit urethral EMT mediated by the TGF-β/Smad signal pathway (b); decreased EMT would lead to retardation of urethral seam fusion (c), eventually resulting in the occurrence of hypospadias (d). DEHP diethylhexyl phthalate, EMT epithelial–mesenchymal transition, TGF-β transforming growth factor beta.
References
Rübben, I. & Stein, R. [Hypospadias: insights and challenges]. Urol. A 56, 1256–1265 (2017).
Bouty, A. et al. The genetic and environmental factors underlying hypospadias. Sex. Dev. 9, 239–259 (2015).
Carmichael, S. L., Shaw, G. M. & Lammer, E. J. Environmental and genetic contributors to hypospadias: a review of the epidemiologic evidence. Birth Defects Res. A Clin. Mol. Teratol. 94, 499–510 (2012).
Craig, J. R. et al. Management of adults with prior failed hypospadias surgery. Transl. Androl. Urol. 3, 196–204 (2014).
Unüvar, T. & Büyükgebiz, A. Fetal and neonatal endocrine disruptors. J. Clin. Res. Pediatr. Endocrinol. 4, 51–60 (2012).
Hu, G. X. et al. Phthalate-induced testicular dysgenesis syndrome: Leydig cell influence. Trends Endocrinol. Metab. 20, 139–145 (2009).
Santangeli, S. et al. Effects of diisononyl phthalate on Danio rerio reproduction. Environ. Pollut. 231, 1051–1062 (2017).
Liu, L. et al. Phthalate metabolites related to infertile biomarkers and infertility in Chinese men. Environ. Pollut. 231, 291–300 (2017).
Halden, R. U. Plastics and health risks. Annu. Rev. Public Health 31, 179–194 (2010).
Heudorf, U., Mersch-Sundermann, V. & Angerer, J. Phthalates: toxicology and exposure. Int. J. Hyg. Environ. Health 210, 623–634 (2007).
Swan, S. H. et al. First trimester phthalate exposure and anogenital distance in newborns. Hum. Reprod. 30, 963–972 (2015).
Li, M. et al. Dose-related effect by maternal exposure to di-(2-ethylhexyl) phthalate plasticizer on inducing hypospadiac male rats. Environ. Toxicol. Pharmacol. 35, 55–60 (2013).
Posnack, N. G. et al. Gene expression profiling of DEHP-treated cardiomyocytes reveals potential causes of phthalate arrhythmogenicity. Toxicology 279, 54–64 (2011).
Kamstra, J. H. et al. Differential DNA methylation at conserved non-genic elements and evidence for transgenerational inheritance following developmental exposure to mono(2-ethylhexyl) phthalate and 5-azacytidine in zebrafish. Epigenetics Chromatin 10, 20 (2017).
Deutschle, T. et al. A controlled challenge study on di(2-ethylhexyl) phthalate (DEHP) in house dust and the immune response in human nasal mucosa of allergic subjects. Environ. Health Perspect. 116, 1487–1493 (2008).
Connolly, E. C., Freimuth, J. & Akhurst, R. J. Complexities of TGF-β targeted cancer therapy. Int. J. Biol. Sci. 8, 964–978 (2012).
Kubiczkova, L. et al. TGF-β - an excellent servant but a bad master. J. Transl. Med. 10, 183 (2012).
Larue, L. & Bellacosa, A. Epithelial-mesenchymal transition in development and cancer: role of phosphatidylinositol 3’ kinase/AKT pathways. Oncogene 24, 7443–7454 (2005).
Thompson, E. W., Newgreen, D. F. & Tarin, D. Carcinoma invasion and metastasis: a role for epithelial-mesenchymal transition. Cancer Res. 65, 5991–5995 (2005). Discussion 5995.
Zhou, Y. et al. Epithelial-mesenchymal transformation and apoptosis in rat urethra development. Pediatr. Res. 82, 1073–1079 (2017).
Baskin, L. S. et al. Urethral seam formation and hypospadias. Cell Tissue Res. 305, 379–387 (2001).
Shen, M. et al. Transforming growth factor β1 signaling coincides with epithelial-mesenchymal transition and fibroblast-to-myofibroblast transdifferentiation in the development of adenomyosis in mice. Hum. Reprod. 31, 355–369 (2016).
Morgan, E. A. et al. Loss of Bmp7 and Fgf8 signaling in Hoxa13-mutant mice causes hypospadia. Development 130, 3095–3109 (2003).
Koo, H. J. & Lee, B. M. Estimated exposure to phthalates in cosmetics and risk assessment. J. Toxicol. Environ. Health A 67, 1901–1914 (2004).
Huber, W. W., Grasl-Kraupp, B. & Schulte-Hermann, R. Hepatocarcinogenic potential of di(2-ethylhexyl)phthalate in rodents and its implications on human risk. Crit. Rev. Toxicol. 26, 365–481 (1996).
Barlow, N. J. & Foster, P. M. Pathogenesis of male reproductive tract lesions from gestation through adulthood following in utero exposure to Di(n-butyl) phthalate. Toxicol. Pathol. 31, 397–410 (2003).
Do, R. P. et al. Non-monotonic dose effects of in utero exposure to di(2-ethylhexyl) phthalate (DEHP) on testicular and serum testosterone and anogenital distance in male mouse fetuses. Reprod. Toxicol. 34, 614–621 (2012).
Koch, H. M., Preuss, R. & Angerer, J. Di(2-ethylhexyl)phthalate (DEHP): human metabolism and internal exposure–an update and latest results. Int. J. Androl. 29, 155–165 (2006). Discussion 181–185.
Mahood, I. K. et al. Abnormal Leydig Cell aggregation in the fetal testis of rats exposed to di (n-butyl) phthalate and its possible role in testicular dysgenesis. Endocrinology 146, 613–623 (2005).
Haraguchi, R. et al. Unique functions of Sonic hedgehog signaling during external genitalia development. Development 128, 4241–4250 (2001).
Zhang, J., Tian, X. J. & Xing, J. Signal transduction pathways of EMT induced by TGF-β, SHH, and WNT and their crosstalks. J. Clin. Med. 5, E41 (2016).
Liu, X. et al. Di(2-ethylhexyl) phthalate (DEHP) increases transforming growth factor-beta1 expression in fetal mouse genital tubercles. J. Toxicol. Environ. Health A 71, 1289–1294 (2008).
Willingham, E. & Baskin, L. S. Candidate genes and their response to environmental agents in the etiology of hypospadias. Nat. Clin. Pract. Urol. 4, 270–279 (2007).
Chen, T. et al. Mutation screening of BMP4, BMP7, HOXA4 and HOXB6 genes in Chinese patients with hypospadias. Eur. J. Hum. Genet. 15, 23–28 (2007).
Baskin, L. S. et al. Cellular signaling in the bladder. Front. Biosci. 2, d592–d595 (1997).
Valcourt, U. et al. TGF-beta and the Smad signaling pathway support transcriptomic reprogramming during epithelial-mesenchymal cell transition. Mol. Biol. Cell 16, 1987–2002 (2005).
Acknowledgements
This study was supported by the National Natural Science Foundation of China (grant 81771566) and the National Natural Science Foundation of China (grant 81970571).
Author contributions
X.L. and G.W. conceived and designed the experiments; Yue Zhou performed the experiments; Yue Zhou analyzed the data; C.L. and L.S. contributed reagents/materials/analysis tools; Yue Zhou and X.L. wrote the paper. F.H., Y.L., D.L., and Yu Zhou assisted to perform the experiment.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, Y., Huang, F., Liu, Y. et al. TGF-β1 relieves epithelial–mesenchymal transition reduction in hypospadias induced by DEHP in rats. Pediatr Res 87, 639–646 (2020). https://doi.org/10.1038/s41390-019-0622-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0622-2