Abstract
Objective
To determine associations of low superior vena cava (SVC) flow (≤55 ml/kg/min) and low right ventricular output (RVO) (≤150 ml/kg/min) in preterm infants.
Design/methods
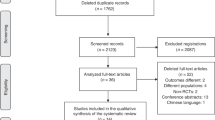
An observational study in infants <30 weeks gestation randomized to receive immediate (<10 s) or delayed cord clamping (DCC) (≥60 s).
Results
The study enrolled 265 infants with a mean (SD) gestation 28 (2) weeks. Eighty-six (33%) infants had low SVC flow and 81 (31%) infants had low RVO. In multivariate analysis, low SVC flow was associated with gestation; low RVO was associated with DCC, gender and 5-minute Apgar; whereas mean RVO was negatively associated with both FiO2 and mean airway pressure (MAP) at 9 h and 24 h. Low SVC flow was associated with ductus arteriosus (DA) treatment. Infants with low RVO had higher mortality on univariate analysis, but this was not significant after adjusting for gestation.
Conclusions
SVC flow was associated with gestation, whilst RVO was associated with placental transfusion, gender, condition at birth, and early respiratory adaptation. Compared to infants with normal values, more infants with low SVC flow were treated for DA, but infants with low RVO had no significant difference in mortality or morbidity.
Similar content being viewed by others
Introduction
Survival of infants born before 30 weeks gestation has improved. However, a significant proportion has some degree of neurodevelopmental disability.1 Hypotension and hypoperfusion of the brain during the immediate postnatal period have been related to cerebral injury in preterm infants.2,3,4 In the first day after birth, when shunts frequently occur across the adapting heart, cardiac input (superior vena cava (SVC) flow) as a measure of systemic blood flow has been reproducibly reported to predict mortality, organ injury including necrotizing enterocolitis, peri/intraventricular hemorrhage (PIVH), and impaired neurodevelopmental outcome.2,3,5,6 Low right and left ventricular outputs are reported to be more common in infants with worsening respiratory diseases.7
There has been significant change in the respiratory management of extremely preterm infants over the last two decades with increasing use of non-invasive ventilation and surfactants.8 The use of antenatal steroid has increased and the incidence of IVH has decreased.9 Mean airway pressure has been reported to be a significant determinant of low SVC flow and low RVO.5,7,10 The incidence of low SVC flow and low RVO has also been reported to decrease over time and speculated to be mainly due to advancement in the respiratory management of the extremely preterm infants.10 The objective of this study is to determine the determinants of low SVC flow and low RVO and its association with adverse clinical outcomes in the era of increased use of antenatal steroids and non-invasive ventilation.
Methods
Setting
This is a nested observation study of the Australian placental transfusion study (APTS) Echo sub-study, a randomized controlled trial (RCT) that investigated the effect of DCC on systemic blood flow in infants <30 weeks gestation (Australia New Zealand Clinical Trials Registry, ACTRN12610000633088).11 The sub-study was conducted in five tertiary neonatal intensive care units in Australia between 17 February 2012 and 30 March 2014. Approval was obtained from the ethics committee at Royal North Shore Hospital, St Leonards, New South Wales.
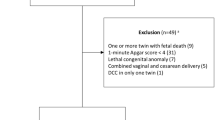
Subjects
Mothers at high risk of delivering before 30 weeks gestation were approached and randomization occurred if informed consent had been obtained. Inclusion criteria were birth <30 weeks gestation with informed consent. The exclusion criterion was ‘no indication or contraindication to placental transfusion in the view of parent or doctor’.
Randomization
Randomization was performed when delivery was considered imminent at an estimated gestation <30 weeks gestation using an interactive voice response system. The computerized randomization system was developed by an independent statistician. The randomization for the main study was by minimization within strata: institution and gestational age (<27 weeks; ≥27 weeks). Each infant of a multiple birth was randomized separately. Randomization into the echocardiography sub-study was a further stratification factor.
Intervention
The infant was randomized to either ICC or DCC group. For infants allocated to the ICC group, the cord was clamped within 10 s of delivery. For infants allocated to DCC group, a birth attendant held the baby as low as possible below the level of the introitus or placenta for at least 60 s before the cord was clamped. The babies did not receive any stimulation or inflation breaths. Time of first breath was not recorded.
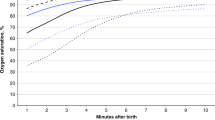
Assessments
All the infants had cardiac ultrasound at 3–6 h, 6–12 h, and 20–28 h of age. The measurements were performed at each study center by clinicians accredited to perform ultrasound. Measures of SVC flow, RVO, DA diameter, and direction of flow were obtained as previously described at each examination.12,13 The quality and the agreement of these measures have been described in a separate publication.14 Flow measures were calculated by obtaining vessel diameter and velocity time integral (VTI) from the pulse wave Doppler signal and the heart rate with the following formula: Output (mL/kg/min) = heart rate × (π × diameter2/4) × VTI / birth weight (kg). Right ventricular diameter was measured at the level of the valve. Individual measures were averaged over at least 5 cardiac cycles. Low SVC flow was defined as ≤55 ml/kg/min from recently reported data8 and low RVO as ≤150 ml/kg/min.11
Infants had blood collected for hemoglobin (Hb) and hematocrit (Hct) at birth from the umbilical cord, or where this was not possible, at admission, and at 6 h of age. Cardiorespiratory variables collected at the time of cardiac ultrasound included mean blood pressure (invasive if arterial line in-situ, otherwise non-invasive), heart rate, type of respiratory support, mean airway pressure (MAP), inspired oxygen (FiO2), and use of nitric oxide. Clinical outcome data collected as part of the main APTS study included death, severe brain injury on postnatal ultrasonography, severe retinopathy of prematurity, necrotizing enterocolitis, late-onset sepsis, or chronic lung disease, each diagnosed by 36 completed weeks of postmenstrual age.15 Severe brain injury on postnatal ultrasonography was defined as intraventricular hemorrhage of grade 3 or 4 or late cerebral abnormality on ultrasonography. Late cerebral abnormality on ultrasonography was defined as echodense intraparenchymal lesions, periventricular leukomalacia, porencephalic cysts, or ventriculomegaly between 14 days after birth and a postmenstrual age of 36 completed weeks. Hypotension was defined as a mean blood pressure (mmHg) below the gestation in weeks for at least 15 min. Detailed definitions are provided in the protocol and publication.15 DA was managed as per the local site protocol. There was no trial protocol for DA management for patients enrolled in the study.
Outcomes
The primary aims of this study were to identify the determinants of low systemic blood flow (SVC flow and RVO) and describe its association with important neonatal morbidities. Demographic and cardiorespiratory variables were explored for their association with measures of low systemic blood flow. The associations between measures of low systemic blood flow and clinical outcome data was explored in a univariate and adjusted analysis.
Statistical analysis
Comparisons for continuous variables were made using 2 sample t-test or Wilcoxon rank sum test, and for categorical variables tests using a chi squared test or Fisher’s exact test, as appropriate. All analyses, both univariate and for the multivariable, used a mixed model approach which accounted for the correlation between measurements within multiple births. In the multivariable analyses for associations with SVC and RVO, variables with a univariate P value < 0.2 were added to the model using a best subset approach and allowing up to 4 predictors to be in the model. P-values < 0.05 were considered statistically significant. Analyses to assess the relationship between cardiac ultrasound measurements at three time points and clinical outcomes using a generalized linear model to account for the within subject correlation, including assessing whether the relationship varied over time. Adjustment for multiple comparison was not performed. A maximum of two variables could be included in these models for outcomes other than low SVC and low RVO due to the low event rate. Analyses were conducted in SAS version 9.3 (Cary, NC).
Results
A total of 265 infants with a mean (SD) gestation of 28 (2) weeks and birth weight of 1021 (271) grams participated in the study, with 133 infants randomized to ICC and 132 to DCC. The baseline demographic characteristics of the population are described in Table 1. Complete antenatal steroids were administered to 153 (58%) of the women while all of them received at least one dose of corticosteroid. One hundred and two infants (39%) infants were on CPAP or high flow nasal cannula at 3–6 h which increased to 188 (72%) by 24 h
Infants with low SVC flow were of younger gestation age (27 (2) vs. 28 (2), p < 0.001) while the rest of the demographic and early cardiorespiratory variables were similar (Table 2). Infants with low RVO were of younger gestation age (27 (2) vs. 28 (1), p = 0.01), were more likely to be allocated to DCC (62 vs. 44%, p = 0.009), be male (64 vs. 49%, p = 0.02), and have Apgar score at 5 min < 6 (13.6 vs. 3.8%, p = 0.02) (Table 2). In multivariate analysis, only gestation was associated with low SVC flow (p < 0.001), whereas DCC (p = 0.014), male gender (p = 0.045), and low 5-minute Apgar (p = 0.045) were associated with low RVO.
After correcting for gestation and gender, mean SVC flow over time was not associated with FiO2 (p = 0.52), MAP (p = 0.45), and ductal diameter (p = 0.37) in a repeated measures analysis. As the relationships for mean RVO differed over time, models were fitted at each time separately. After correcting for gestation and gender, mean RVO was significantly decreased with increasing FiO2 at 9 h (p = 0.005) and 24 h (p = 0.002), and similarly with increasing MAP at 9 h (p < 0.001) and 24 h (p < 0.001). There was no association with ductal diameter (all p ≥ 0.05).
Infants with low SVC flow had more blood transfusions (66.3 vs. 46.9%, p = 0.004) and more treatment for DA (53.5 vs. 28.6%, p = 0.002) (Table 3). However, after adjusting for gestation, infants with low SVC flow did not require significantly more blood transfusions (p = 0.29) but still had significantly more treatment for DA (p = 0.04). Infants with low RVO were significantly more likely to die (11.1 vs. 2.7%, p = 0.04) and more likely to have higher hematocrit (51.7 vs. 49.1, p = 0.03) (Table 3). However, the relationship with mortality (p = 0.06) no longer remained significant after adjusting for gestation and DCC. The relationship with hematocrit (p = 0.23) no longer remained significant after adjusting for DCC.
Infants with mean SVC flow ≤55 ml/kg/min compared to infants with mean SVC flow >55 ml/kg/min had similar rates of mortality (13 vs.5%), any IVH (13 vs. 16%), late IVH (7 vs. 11%), IVH grade 3 or 4 (6 vs.4%), and NEC (13 vs. 4%) (Table 4). Infants with mean RVO ≤150 ml/kg/min as compared to infants with mean RVO >150 ml/kg/min had similar rates of mortality (13 vs. 5%), any IVH (29 vs. 14%), late IVH (17 vs. 10%), NEC (0 vs. 5%) but more IVH grade 3 or 4 (17 vs. 3%, p = 0.01) (Table 4). These associations could not be adjusted due to low event rates.
Only 23 infants had 2 or more episodes of low SVC flow and 34 infants had 2 or more episodes of low RVO. Infants with 2 or more episodes of low SVC flow compared to infants with fewer than 2 episodes of low SVC flow had similar rates of mortality (9 vs. 5%), any IVH (17 vs. 16%), late IVH (9 vs. 11%), IVH grade 3 or 4 (4 vs. 4%), and NEC (9 vs. 5%) (Table 4). Infants with 2 or more episodes of low RVO as compared to infants with fewer than 2 episodes of low RVO had similar rates of mortality (12 vs. 4%), any IVH (26 vs. 14%), late IVH (18 vs. 10%), NEC (6 vs. 5%) but more IVH grade 3 or 4 (12 vs. 3%, p = 0.04) (Table 4). These associations could not be adjusted due to low event rates.
Discussion
This is the largest multicentre, prospective study investigating the determinants and associations of low systemic blood flow in infants born <30 weeks gestation. Low SVC flow was only associated with lower gestation, whilst low RVO was associated with male gender, DCC, and low 5-minute Apgar score. Mean RVO was associated with both FiO2 and mean airway pressure (MAP) at 9 h and 24 h. Infants with low SVC flow were more likely to need treatment for DA, whereas infants with low RVO had no significant difference in mortality and morbidity.
Several studies have identified risk factors for the development of low SVC flow. Preterm infants developing low SVC flow are less likely to have completed antenatal steroids, less likely to be born to a mother on antihypertensive medication,16,17 are of a lower gestational age, have a larger DA,5,16,17,18 need a higher MAP and are more likely on invasive ventilation.5,16,17,19 We found gestation to be the only significant determinant of low SVC. Our population had a high rate of antenatal steroid use and most of the infants were managed with brief invasive ventilation and lower mean airway pressures, as well as a lower incidence of very low SVC flow (≤40 ml/kg/min) on which previous observations were made.3,5,6
Kluckow and Evans were the first to publish data on adverse neonatal outcomes in infants with low SVC flow. They studied 126 babies <30 weeks’ gestation with serial measurements of Doppler echocardiography and cerebral ultrasound at 5, 12, 24, and 48 h of age.5 Lowest SVC flow (<30 ml/kg/min) and the number of recordings of SVC flow <30 ml/kg/min in the first 24 h of life was significantly associated with late intraventricular hemorrhage. Other studies have subsequently linked low SVC flow to other adverse short-term outcomes including oliguria, hyperkalaemia, retinopathy of prematurity and necrotizing enterocolitis.6,20,21,22 Hunt et al. published three-year developmental outcomes from preterms with low SVC flow after birth and found that the average SVC flow on day one of life was inversely correlated with the risk of death and disability.2 A subsequent study published in 2007 showed that preterm neonates who had low SVC flow went on to have significantly poorer outcomes across a range of neurodevelopmental areas as well as overall increased morbidity and mortality.20
However, two cohort studies recently published did not find an association between SVC flow in the first 2–3 days of life and adverse outcomes including IVH.10,23 Our study results of no significant association between low SVC (≤55 ml/kg/min) and any of the important clinical neonatal morbidities including IVH and PVL are consistent with these studies. There are several potential reasons for this including timing of cardiac ultrasound measurement, definitions for low SVC flow, incidence of low SVC flow, time of detection of IVH, improved obstetric care and increasing use of less invasive ventilation of preterm infants.24 Early and late P/IVH have distinct and different risk factors. Early P/IVH was reported to be associated with vaginal delivery and low one minute Apgar score, whereas late P/IVH was associated with antecedent low SVC flow in the first day.3 We did not have the information on early and late IVH separately for our cohort. The incidence of low SVC flow is observed to be decreasing over the last 15 years.4,10,11,24 In the current study, incidence of low SVC flow defined as ≤55 ml/kg/min was 32% and defined as <41 ml/kg/min was 11%, which is consistent with the recently reported studies.10,25
RVO has been reported to be affected by ductal diameter, foraminal shunting, and worsening respiratory disease reflected by higher FiO2 and mean airway pressure.7 Atrial shunting was not measured in the current study. Our results are consistent with this study with infants with low RVO needing higher FiO2 and MAP at 9 and 24 h. We also found gestation, male gender, low Apgar score at 5 mins, and DCC to be significantly associated with low RVO. There have been no other studies to our knowledge on determinants of low RVO. The babies included in the Evans cohort were preterm infants that were all mechanically ventilated at 24 h, whilst the current study had only 20% of the population ventilated by 24 h. Associations of low RVO with morbidities at discharge have not been reported before. Infants with low RVO did not have increased morbidities including CLD. However, they were more likely to die (11.1 vs. 2.7%, p = 0.04) on a univariate analysis. However, after adjusting for gestation and DCC, these no longer remained significant.
This secondary analysis of the APTS echo sub-study reporting the association between measures of systemic blood flow and clinical outcomes is the largest of its kind. The study population reflects contemporary practice. The study finding should be interpreted considering interobserver variability between multiple observers acquiring functional ultrasound images at study sites. Interobserver variability for SVC flow and RVO has been reported in a separate publication and is consistent with that previously reported.26 The nominally statistically significant associations must be interpreted with caution as no adjustment were made for multiple comparisons.
In this sub-study, DCC was associated with decreased blood transfusion, increased peak hematocrit and peak bilirubin in the first 7 day. None of the infants with DCC had an exchange transfusion. Other neonatal morbidities and mortality remained similar between the two groups. This study was not powered to detect differences in the clinical outcomes. The clinical outcomes of the main APTS trial and the systematic review of similar trials should inform practices in relation to cord clamping practices and incorporated into preterm resuscitation guidelines.15,27
Conclusions
Low SVC flow was only associated with lower gestation, whilst low RVO was associated with male gender, DCC and low 5-minute Apgar score. Mean RVO was negatively associated with both FiO2 and mean airway pressure (MAP) at 9 h and 24 h. Compared to infants with normal values, more infants with low SVC flow were treated for DA, but infants with low RVO had no significant difference in mortality or morbidity.
Change history
15 April 2019
A correction to this paper has been published and can be accessed via a link at the top of the paper.
References
Saigal, S. & Doyle, L. W. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet 371, 261–269 (2008).
Hunt, R. W. et al. Low superior vena cava flow and neurodevelopment at 3 years in very preterm infants. J. Pediatr. 145, 588–592 (2004).
Osborn, D. A., Evans, N. & Kluckow, M. Hemodynamic and antecedent risk factors of early and late periventricular/intraventricular hemorrhage in premature infants. Pediatrics 112(1 Pt 1), 33–39 (2003).
Batton, B. et al. Blood pressure, anti-hypotensive therapy, and neurodevelopment in extremely preterm infants. J. Pediatr. 154, 351–357 (2009). 357e1.
Kluckow, M. & Evans, N. Low superior vena cava flow and intraventricular haemorrhage in preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. 82, F188–F194 (2000).
Miletin, J. & Dempsey, E. M. Low superior vena cava flow on day 1 and adverse outcome in the very low birthweight infant. Arch. Dis. Child. Fetal Neonatal Ed. 93, F368–F371 (2008).
Evans, N. & Kluckow, M. Early determinants of right and left ventricular output in ventilated preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. 74, F88–F94 (1996).
Glass, H. C. et al. Outcomes for extremely premature infants. Anesth. Analg. 120, 1337–1351 (2015).
Fanaroff, A. A., Hack, M. & Walsh, M. C. The NICHD neonatal research network: changes in practice and outcomes during the first 15 years. Semin. Perinatol. 27, 281–287 (2003).
Holberton, J. R. et al. The diagnostic value of a single measurement of superior vena cava flow in the first 24 h of life in very preterm infants. Eur. J. Pediatr. 171, 1489–1495 (2012).
Popat, H. et al. Effect of delayed cord clamping on systemic blood flow: a randomized controlled trial. J. Pediatr. 178, 81–86 (2016). e2.
Alverson, D. C. Neonatal cardiac output measurement using pulsed Doppler ultrasound. Clin. Perinatol. 12, 101–127 (1985).
Kluckow, M. & Evans, N. Superior vena cava flow in newborn infants: a novel marker of systemic blood flow. Arch. Dis. Child. Fetal Neonatal Ed. 82, F182–F187 (2000).
Popat, H. et al. Interobserver agreement and image quality of functional cardiac ultrasound measures used in a randomised trial of delayed cord clamping in preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. 103, F257–F263 (2018).
Tarnow-Mordi, W. et al. Delayed versus immediate cord clamping in preterm infants. N. Engl. J. Med. 377, 2445–2455 (2017).
Osborn, D., Evans, N. & Kluckow, M. Randomized trial of dobutamine versus dopamine in preterm infants with low systemic blood flow. J. Pediatr. 140, 183–191 (2002).
Osborn, D. A., Evans, N. & Kluckow, M. Left ventricular contractility in extremely premature infants in the first day and response to inotropes. Pediatr. Res. 61, 335–340 (2007).
Osborn, D. A., Evans, N. & Kluckow, M. Effect of early targeted indomethacin on the ductus arteriosus and blood flow to the upper body and brain in the preterm infant. Arch. Dis. Child. Fetal Neonatal Ed. 88, F477–F482 (2003).
Miletin, J., Pichova, K. & Dempsey, E. M. Bedside detection of low systemic flow in the very low birth weight infant on day 1 of life. Eur. J. Pediatr. 168, 809–813 (2009).
Osborn, D. A. et al. Low superior vena cava flow and effect of inotropes on neurodevelopment to 3 years in preterm infants. Pediatrics 120, 372–380 (2007).
Cerbo, R. M. et al. Near-infrared spectroscopy monitoring, superior vena cava flow, and neurodevelopmental outcome at 2 years in a cohort of very low-birth-weight infants. Am. J. Perinatol. 33, 1093–1098 (2016).
Kluckow, M. & Evans, N. Low systemic blood flow and hyperkalemia in preterm infants. J. Pediatr. 139, 227–232 (2001).
Bates, S. et al. Superior vena cava flow and intraventricular haemorrhage in extremely preterm infants. J. Matern. Fetal Neonatal Med. 29, 1581–1587 (2016).
McGovern, M. & Miletin, J. A review of superior vena cava flow measurement in the neonate by functional echocardiography. Acta Paediatr. 106, 22–29 (2017).
Lakkundi, A., Wright, I. & de Waal, K. Transitional hemodynamics in preterm infants with a respiratory management strategy directed at avoidance of mechanical ventilation. Early Hum. Dev. 90, 409–412 (2014).
Popat, H. et al. Interobserver agreement and image quality of functional cardiac ultrasound measures used in a randomised trial of delayed cord clamping in preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. 103, F257–F263 (2017).
Fogarty, M. et al. Delayed vs early umbilical cord clamping for preterm infants: a systematic review and meta-analysis. Am. J. Obstet. Gynecol. 218, 1–18 (2018).
Acknowledgements
We thank the parents and clinicians who gave their support to the conduct of the study, as well as Rebecca Brown for assistance with data management.
Funding
National Health and Medical Council project grant 571309
Author information
Authors and Affiliations
Contributions
H.P. participated in study design, patient recruitment, data analysis, data interpretation, and drafted the initial manuscript. K.P.R. participated in study design, data collection, and data analysis. A.K. participated in study design, data collection, and data analysis. L.S. supervised the project design and participated in data collection. N.E. participated in the design of the study and participated in patient recruitment and data acquisition. A.G. participated in the design of the study and participated in patient recruitment and data acquisition. M.K. participated in the design of the study and participated in patient recruitment and data acquisition. S.S. participated in patient recruitment and data acquisition. K.d.W. participated in the design of the study and participated in patient recruitment and data acquisition. W.T.-M. conceptualized and designed the study and participated in data analysis and interpretation. D.O. conceptualized and designed the study, participated in patient recruitment, data analysis and interpretation, and drafted the initial manuscript. All authors revised it critically for important intellectual content, approved the final manuscript as submitted, and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Popat, H., Robledo, K.P., Kirby, A. et al. Associations of measures of systemic blood flow used in a randomized trial of delayed cord clamping in preterm infants. Pediatr Res 86, 71–76 (2019). https://doi.org/10.1038/s41390-019-0348-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0348-1
This article is cited by
-
Intraventricular hemorrhage prediction in premature neonates in the era of hemodynamics monitoring: a prospective cohort study
European Journal of Pediatrics (2022)