Abstract
Background
A lack of consensus exists as to the timing of kidney biopsy in children with steroid-dependent nephrotic syndrome (SDNS) where minimal change disease (MCD) predominates. This study aimed at examining the applicability of a biomarker-assisted risk score model to select SDNS patients at high risk of focal segmental glomerulosclerosis (FSGS) for biopsy.
Methods
Fifty-five patients with SDNS and biopsy-proven MCD (n = 40) or FSGS (n = 15) were studied. A risk score model was developed with variables consisting of age, sex, eGFR, suPAR levels and percentage of CD8+ memory T cells. Following multivariate regression analysis, total risk score was calculated as sum of the products of odds ratios and corresponding variables. Predictive cut-off point was determined using receiver operator characteristics (ROC) curve analysis.
Results
Plasma suPAR levels in FSGS patients were significantly higher, while percentage of CD45RO+CD8+CD3+ was significantly lower than in MCD patients and controls. ROC analysis suggests the risk score model with threshold score of 16.7 (AUC 0.84, 95% CI 0.72–0.96) was a good predictor of FSGS on biopsy. The 100% PPV cut-off was >24.0, while the 100% NPV was <13.3.
Conclusion
A suPAR and CD8+ memory T cell percentage-based risk score model was developed to stratify SDNS patients for biopsy and for predicting FSGS.
Similar content being viewed by others
Introduction
Minimal change disease (MCD) is the most common histological lesion in renal biopsies of children presenting with idiopathic nephrotic syndrome (INS) while focal segmental glomerulosclerosis (FSGS) is observed in approximately 10% of cases of INS in children aged <6 years and 20–50% of adolescents.1 Current practice in paediatrics involves performing a kidney biopsy when the patient exhibits steroid resistance, as well as in some patients with steroid dependence. FSGS is the most prevalent histologic lesion in steroid-resistant nephrotic syndrome (SRNS) and also the major cause of end-stage kidney disease. On the other hand, MCD, which has a better outcome, is the prominent histology among those with steroid-dependent nephrotic syndrome (SDNS). While the indication for biopsy in SRNS has been established, there is a lack of consensus as to the necessity and timing for biopsy in SDNS, since MCD is the predominant lesion. There is no single proven clinical parameter or biomarker that can predict FSGS in patients with SDNS without a biopsy. The poorer renal outcome associated with FSGS serves as an impetus to search for a rapid, non-invasive, distinct biomarker with potential clinical applications. Such a biomarker would be valuable as a guide for early timing of kidney biopsy and subsequent therapeutic options in patients considered as “high risk” of developing renal insufficiency.
Soluble urokinase-type plasminogen activator receptor (suPAR) is a circulating signalling molecule likely derived from immature myeloid cells.2 It is a receptor for urokinase and a ligand for integrins.3 Studies by Wei et al. proposed suPAR to be a circulating factor in FSGS and ushered new insights into the causes of this proteinuric kidney disease.4 Circulating suPAR binds to podocyte integrins leading to integrin activation and proteinuria either through its elevated levels4 or through its cooperation with other molecules known to be associated with FSGS such as mutated APOL1 proteins or auto-antibodies targeting CD40.5,6 Initial studies have shown that serum suPAR levels were significantly elevated in patients with FSGS with preserved renal function, in contrast to those with MCD and membranous nephropathy.4 Follow-up studies was able to replicate the elevated suPAR in FSGS among patients with mild renal dysfunction. However, more studies are needed to dissect whether the elevated suPAR level seen in FSGS is due to the disease itself (pathogenic) or the reduced renal function per se.7,8,9,10 In particular, a study that investigated the relationship of suPAR with proteinuria in children with primary nephrotic syndrome demonstrated that a relatively higher suPAR level was associated with steroid resistance regardless of pathology, i.e., either FSGS or MCD. This was consistent with the hypothesis that serum suPAR concentration parallels the severity of podocyte injury.11 Additional large patient observational studies identified suPAR to be independent of estimated glomerular filtration rate (eGFR) >90 mL/min/1.73 m2 as well as a strong independent predictor for chronic kidney disease (CKD) incidence and progression.12,13 The precise role for suPAR in FSGS compared to other causes of CKD including diabetic nephropathy is still being investigated.
On the other hand, there is some evidence of T cell involvement in a subgroup of patients with FSGS. Earlier studies on renal biopsy tissue demonstrated interleukin-2 receptor alpha (IL-2Rα) mRNA expression in 70% of FSGS patients,14 as well as T cell infiltration in children with FSGS compared with other forms of glomerulopathy.15 In an experimental rat model of proteinuria with histological FSGS lesions accompanied by TH2-predominant T cell infiltration,16 CD4+CD25+ T-lymphocyte transfer reduced the proteinuria with regression of FSGS lesions.17
This study aimed to develop a non-invasive risk scoring model with circulating suPAR and lymphocyte subsets, in order to provide a guide to the timing of renal biopsy in paediatric SDNS patients with a high suspicion of FSGS as the underlying aetiology.
Methods
Study design
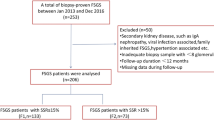
Recruitment of patients with INS is outlined in Fig. 1. A total of 98 consecutive children with SDNS underwent renal biopsy at the Shaw-NKF-NUH Children’s Kidney Center in Singapore between 1996 and 2017 and had the biopsy diagnosis of FSGS or MCD (Fig. 1). Fifty-five (63%) of these children who were still on follow-up after 2008 and consented for research participation were included in the study as the discovery cohort. SDNS was defined as inability to taper off prednisolone therapy without relapse or relapse within 14 days of its discontinuation. Exclusion criteria included patients with eGFR ≤ 60 mL/min/1.73 m2, bacterial sepsis, underlying systemic disease such as lupus nephritis, and secondary causes of FSGS such as genetic mutations and congenital anomalies of the kidney and urinary tract including reflux nephropathy and solitary kidneys. Clinical and demographic characteristics of the patients were obtained, including age at presentation, age at time of study, sex, race, nephrotic status, immunosuppressive drugs prior to biopsy, eGFR (based on the modified Schwartz formula),18 haematuria or hypertension status at biopsy and years from disease onset.
Flowchart showing recruitment of INS patients with SDNS to generate the MeSsAGe risk score model and a separate cohort of patients with SRNS to assess the performance characteristics of the model. A total of 251 cases biopsied between 1996 and 2017 were reviewed. Seventy-nine patients with INS secondary to MN, LN, or HSPN and 19 FSGS patients with eGFR ≤ 60 mL/min/1.73 m2 were excluded. Ninety-eight of the 153 cases with INS due to MCD or FSGS had SDNS, of whom 55 (63%) were still on follow-up after 2008 and consented to the research participation. Another 55 children had SRNS, of whom 32 (58%) were still on follow-up after 2008, and consented to the research. NS nephrotic syndrome, INS idiopathic nephrotic syndrome, MN membranous nephropathy, LN lupus nephritis, HSPN Henoch-Schonlein purpura nephritis, MCD minimal change disease, FSGS focal segmental glomerulosclerosis, eGFR estimated glomerular filtration rate, SDNS steroid-dependent nephrotic syndrome, SRNS steroid-resistant nephrotic syndrome
To assess the performance characteristics of the risk score model in patients with SRNS, 32 additional paediatric patients with SRNS and eGFR > 60 mL/min/1.73 m2 were recruited (Fig. 1). SRNS was defined as failure to achieve complete remission defined by loss of proteinuria (urinary total protein <0.3 g/1.73 m2/day or urine protein:creatinine ratio <0.02 g/mmol or <1+ protein on dipstick for 3 consecutive days) despite therapy with prednisolone at 60 mg/m2/day for 8 weeks. A total of 55 children with SRNS due to either MCD or FSGS were biopsied between 1996 and 2017, of whom 32 (58%) were still on follow-up after 2008, and who fulfilled the inclusion criteria of having normal renal function (eGFR > 60 mL/min/1.73 m2) and consented for research participation. As a baseline comparison for suPAR and lymphocyte subset analysis, 50 age- and sex-matched healthy controls were recruited from the General Nephrology Clinic and comprised patients who had non-glomerular disorders such as mild vesicoureteric reflux and duplex kidneys, with normal renal function (eGFR > 90 mL/min/1.73 m2) and no evidence of albuminuria or urinary tract infection.
Informed consent and assent were obtained from the parents and patients. This study was approved by the Institutional Ethics Review Committee, Domain Specific Review Boards, National Healthcare Group, Singapore (2007/00459 and 2011/00408) and conducted in accordance with the approved guidelines and regulations.
suPAR measurement
Blood samples were collected in EDTA tubes from the study subjects. Plasma was obtained within 30 min of sample collection, aliquoted and stored at −80 °C until assay. Plasma suPAR concentration was determined using Quantikine Human uPAR Immunoassay (R&D Systems, Inc, Minneapolis, MN) according to the manufacturer’s protocol. Fifty microlitres of standard or samples were added to wells pre-coated with mouse monoclonal antibody (mAb) specific for human uPAR and incubated for 2 h. All plasma samples were diluted five-fold. The wells were washed four times and subsequently incubated for 2 h with 200 μL of horseradish peroxidase-labelled polyclonal antibody specific for uPAR. Following another four washes, 200 μL of substrate solution containing tetramethylbenzidine and hydrogen peroxide was added for colour development and this was stopped after 30 min by adding 50 μL of 2 N sulphuric acid. The optical density was measured at 450 nm with wavelength subtraction at 540 nm using a microplate reader (Bio-Rad Laboratories Inc, Hercules, CA). The intra-assay and inter-assay variability for the suPAR measurements were 2.9% and 7.7%, respectively.
Lymphocyte subset phenotyping
The following mouse IgG1, κ isotype control and mouse anti-human mAbs were purchased from Becton Dickinson (Franklin Lakes, NJ): Fluorescein isothiocyanate-conjugated IgG1, CD19 and CD45RA; phycoerythrin-conjugated IgG1, CD16, CD45RO and CD56; peridin chlorophyll protein-conjugated IgG1, CD3 and CD4; allophycocyanin-conjugated IgG1 and CD25; V450-conjugated CD3; and V500-conjugated mouse IgG1 and CD8. Lymphocyte subset staining was performed by the lysed whole-blood method as described previously.19 Data analysis for determination of the percentage of positive cells was performed using the CellQuest™ Pro software (Becton Dickinson).
Statistical analysis
Statistical analysis was performed using the SPSS software (version 20.0 for Windows©, SPSS Inc, Chicago, IL). Data were expressed as median and interquartile range. Univariate comparison between MCD and FSGS was performed using chi-square test for categorical variables and Mann–Whitney U test for continuous variables. Bonferroni correction was carried out for multiple subset comparisons. Multivariate analysis was performed using binary logistic regression to examine the association between biopsy outcome and clinical and demographic indicators. Receiver-operating characteristic (ROC) curve analysis was used to determine utility of the individual markers for predicting biopsy outcome. Binary logistic regression was performed to evaluate the combined utility of the significant markers in predicting biopsy outcome.
A risk score predictive model was developed with categorical variables consisting of the demographic parameters (sex and age), eGFR, as well as plasma suPAR level and percentage of CD8+ memory T cells. suPAR and CD8+ memory T cells were assigned as 1 for values from 0 to 25th percentile, 2 for 25th to 50th percentile, 3 for 50th to 75th percentile and 4 for 75th to 100th percentile; eGFR was assigned a value of 0 for eGFR > 90 mL/min/1.73 m2 or 1 for eGFR ≤ 90 mL/min/1.73 m2. The weights for each variable in the model were based on the odds ratios (ORs) from the multivariate logistic regression. Total risk score was defined as sum of the products of ORs and the corresponding variables. A predictive cut-off point was determined using the ROC curve analysis. A P value <0.05 was considered statistically significant.
Results
Baseline characteristics
Fifty-five consecutive patients with SDNS (median age 13 years, range 2–33 years), age of onset of nephrotic syndrome 1–15 years with biopsy-proven MCD (n = 40) and FSGS (n = 15) were studied. There was no significant difference between MCD and FSGS in terms of age of first presentation, age at time of sampling, sex, race, nephrotic status, medication prior to biopsy, haematuria or hypertension at biopsy and years from disease onset on both univariate and multivariate analysis (Table 1). However, the proportion of FSGS patients (26.7%) with eGFR between 60 and 90 mL/min/1.73 m2 was significantly greater than MCD patients (5%) only on univariate analysis (P = 0.04).
Altered suPAR levels and memory T cells in FSGS patients
The plasma suPAR levels in FSGS patients [2272.4 (1993.4, 3369.0) pg/mL] were significantly higher compared with MCD that in patients [1891.5 (1566.0, 2256.4) pg/mL] (P = 0.02) and healthy controls [1806.6 (1545.0, 2068.5) pg/mL] (P = 0.001) (Fig. 2a). Among the lymphocyte subsets studied (Table 2), only the percentage of CD8+ memory T cells (CD45RO+CD8+CD3+) in FSGS patients [17.1 (13.0, 25.5)%] was significantly lower compared with that in MCD patients [32.0 (19.0, 42.7)%] (P = 0.02) and healthy controls [30.8 (19.4, 38.8)%] (P = 0.007) (Fig. 2b). After applying Bonferroni correction for the number of subsets being analysed, the differences between FSGS patients and controls remained significant (P = 0.02). Although the percentage of CD8+ naive (CD45RA) T cells was significantly higher in FSGS patients [79.3 (71.1, 83.1)%] compared with that in MCD patients [71.8 (58.4, 80.0)%] (P = 0.04), this did not reach statistical significant compared with controls [73.0 (63.8, 80.7)%].
Plasma soluble urokinase-type plasminogen activator receptor (suPAR) levels and percentage of CD8+ memory T cells in healthy controls (c), steroid-dependent nephrotic syndrome patients with minimal change disease (MCD), and focal segmental glomerulosclerosis (FSGS). Elevated plasma suPAR concentration (a) and decreased percentage of CD45RO+CD8+CD3+ (b) in FSGS (n = 15) compared with MCD (n = 40) and healthy controls (n = 50)
While the percentage of CD4+ naive (CD45RA) and memory (CD45RO) T cells were significantly different both in MCD patients (P = 0.001) and FSGS patients (P < 0.05) compared with controls, they could not differentiate between MCD and FSGS patients (Table 2). Similarly, there was no difference in the percentage of CD25+CD4+CD3+ cells in MCD and FSGS patients though the percentage of this subset in MCD was significantly higher than in controls (P = 0.003) (Table 2). There was no difference in the percentage of B cells, T cells and natural killer cells, as well as helper T cell (CD4+CD3+), cytotoxic T cell (CD8+CD3+) and regulatory T cell subsets, in MCD and FSGS patients.
Predictive model for renal biopsy (MeSsAGe)
To identify the markers that might provide a threshold for performing a renal biopsy to diagnose FSGS in children with SDNS, an ROC analysis was initially done using the variables that were significantly different on univariate analysis (Table 3). Although eGFR, plasma suPAR levels and percentage of CD8+ memory T cells were significant on univariate analysis, ROC analysis showed that eGFR (AUC 0.61, 95% confidence interval (CI) 0.43–0.79), suPAR (AUC 0.69, 95% CI 0.53–0.85) and CD8+ memory T cells (AUC 0.73, 95% CI 0.57–0.88) alone were not sufficient in predicting biopsy outcome in children with SDNS. Combining eGFR and CD45RO (AUC 0.76, 95% CI 0.61–0.92) or eGFR and suPAR (AUC 0.71, 95% CI 0.54–0.87) did not improve the predictive characteristics. However, combining suPAR, eGFR and CD8+ memory T cells improved the predictive performance (AUC 0.82, 95% CI 0.69–0.95).
A risk score predictive model (MeSsAGe) for renal biopsy was subsequently generated factoring in quartiles of CD8+Memory T cells (CD45RO+CD8+CD3+), Sex, quartiles of plasma suPAR levels, Age and Glomerular filtration rate. Plasma suPAR levels were categorized as follows: 25th quartile 1597 pg/mL, 50th quartile 2021 pg/mL, and 75th quartile 2459 pg/mL, while the percentage of CD8+ memory T cells were categorized as follows: 25th quartile 16.1%, 50th quartile 24.6%, and 75th quartile 39.7%.
The total risk score was obtained by summing the products of OR and the corresponding variable as follows:
Total risk score = 3.2 × Male + 8.5 × Age [7–18 years] + 12.7 × Age [≥19 years] + 1.6 × suPAR [≥75th quartiles] + 6.0 × eGFR [60–90 mL/min/1.73 m2] + 10.7 × CD45RO+CD8+CD3+ [≤25th quartiles] + 11.0 × CD45RO+CD8+CD3+ [25th–50th quartiles] + 1.6 × CD45RO+CD8+CD3+ [50th–75th quartiles]
This model yielded a minimum value of 0 and maximum value of 34.5 giving a threshold risk score of 16.7 (AUC 0.84, 95% CI 0.72–0.96) with a sensitivity and specificity of 85.7% and 67.6% respectively, and a positive predictive value (PPV) and negative predictive value (NPV) of 52.2% and 92.0%, respectively. The 100% PPV cut-off was >24.0, while the 100% NPV was <13.3.
Discriminatory performance characteristics of the MeSsAGe risk score model in patients with SRNS
To evaluate the accuracy of the predictive model, we calculated the risk scores in a separate cohort of patients with SRNS (median age 13 years, range 3–24 years) with biopsy-proven MCD (n = 13) and FSGS (n = 19). Using the threshold value from the risk score model, 80.0% (16 out of 20) of the patients with scores ≥16.7 had FSGS, whereas 75.0% (9 out of 12) of the patients with score <16.7 had MCD. With the 100% PPV cut-off derived from the risk score model, 85.7% (6 out of 7) of the patients with scores >24 had FSGS, while the 100% NPV cut-off yielded 71.4% (5 out of 7) of the patients with scores <13.3 who had MCD.
Discussion
There is a need to re-evaluate the indications for biopsy in children with SDNS in order to identify those patients with probable FSGS that may need more aggressive immunosuppressive treatment to achieve sustained remission. A biomarker-assisted risk score model if validated may reduce the need for renal biopsy in SDNS patients deemed likely to have MCD.
The significance of low eGFR at diagnosis cannot be discounted as it portends a poor renal outcome among patients with FSGS.20,21,22,23,24 This was consistent with the 1978 International Study of Kidney Disease in Children report, which showed that serum creatinine at the time of diagnosis can differentiate fairly well between patients with FSGS and MCD.25 In contrast, Alshami et al. did not find eGFR to be an accurate predictor of FSGS but non-response to steroids at 6 weeks did, which was not surprising as FSGS is the predominant lesion in SRNS.26 Renal function in children with SDNS is usually not significantly impaired, with eGFR > 60 mL/min/1.73 m2. There is a scarcity of data regarding the use of eGFR to predict FSGS in children with SDNS. In our study, we showed that eGFR between 60 and 90 mL/min/1.73 m2 prior to biopsy, was significantly associated with the diagnosis of FSGS on renal biopsy.
suPAR is derived from uPAR as the cleaved product of an enzymatic process after removal of the GPI anchor releasing it from the cell membrane or as a secretory isoform of uPAR. suPAR itself can be further processed to remove domain 1, thus suPAR can possess multiple forms. Elevation of suPAR levels has been associated notably with several inflammatory conditions as well as different cancers. In kidney rodent models, suPAR has been identified as a circulating factor causing glomerular disease2,4 but not after short-term infusion.27 Mechanistically, high levels of suPAR allows activation of podocyte β3-integrin, which is sufficient to drive podocyte foot process effacement, proteinuria and initiation of FSGS. suPAR’s signalling capacity is enhanced by podocyte injurious molecules such as mutated APOL1 protein or anti-CD40 autoantibodies.5,6
In a kidney transplant recipient with recurrent FSGS and very high suPAR levels, improvement in proteinuria was demonstrated following transient reduction of suPAR levels through plasmapheresis and immuno-adsorption.28 Subsequent studies in 10 patients with recurrent FSGS posttransplantation also showed stabilization of proteinuria following plasmapheresis, with decrease in suPAR levels associated with reduction in podocyte β3-integrin activation.29 As plasmapheresis removes many circulating factors, it remains to be seen whether suPAR is indeed the factor responsible for recurrence of FSGS posttransplantation. Additionally, elevated urinary suPAR levels have also been implicated in recurrent cases of FSGS after transplantation, suggesting a possible prognostic role.30 Based on the clinical and experimental data on the role of suPAR as a permeability factor on the glomerular filtration barrier, it is conceivable that suPAR may be involved in the pathogenesis of FSGS. Conflicting results on suPAR levels in FSGS are attributed at least in part to decreased renal function, inflammatory status, timing of sampling whether in nephrotic relapse or remission, effect of storage, technical variations between laboratories for suPAR measurement and differences in the assay for serum or plasma samples as serum levels are generally higher than plasma levels.31,32,33 In this study where all patients had eGFR > 60 mL/min/1.73 m2, we demonstrated that SDNS patients with FSGS on renal biopsy had significantly higher plasma suPAR levels compared with patients with MCD.
Early studies suggest that CD45RO may have a role in childhood INS. The percentage of CD4+ and CD8+ memory T cells in children (between 4 and 12 years of age) with INS in relapse were reported to be significantly higher than controls.34 About 40% of these children had MCD proven on renal biopsy. In another study, the percentage of CD4+ memory T cells prior to steroid treatment was shown to be lower in children with steroid-sensitive nephrotic syndrome (between 2 and 9 years of age) compared with SRNS.35 However, a recent study in adults with new onset idiopathic MCD showed no significant difference in the percentage of CD4+ and CD8+ T cells compared with controls.36 In our cohort of SDNS patients, the percentage of CD4+ memory T cells was significantly higher in both MCD and FSGS compared with controls, excluding it as a useful marker to differentiate between MCD and FSGS in our patients with SDNS.
To date, there has been no reported studies on the role of memory T cells in patients with FSGS. In our cohort of SDNS patients with FSGS, the percentage of CD8+ memory T cells was significantly lower than that in MCD patients and healthy controls. CD45RO+ T cells are the main cells producing interferon (IFN)-γ, IL-4 and IL-17.37 CD45RA−CD8+ and CD45RO+CD8+ T cells have been shown to produce more IFN-γ, IL-2 and tumour necrosis factor-β than the naive CD8+ T cells.38 Recently, we reported a subgroup of FSGS patient with decreased IFN-γ production upon phorbol myristate acetate/ionophore stimulation.19 This subgroup of FSGS patients responded favourably to rituximab treatment, suggesting the possible immunological basis for rituximab treatment in FSGS. The decreased percentage of CD45RO+CD8+ cells in SDNS patients with FSGS in our current study further supports the presence of a subgroup of FSGS patients with defective T cell response.
Although eGFR between 60 and 90 mL/min/1.73 m2, high plasma suPAR levels and low percentage of CD8+ memory T cells were associated with FSGS in our study, none performed well individually in predicting biopsy outcome. This was consistent with findings from Wada et al. where the AUC-ROC of suPAR was only 0.684, suggesting that suPAR alone may not be sufficient to differentiate FSGS from MCD in adults.39 Combining the three markers improved the predictor performance characteristics as shown in Table 3.
We therefore derived a risk score model that could predict a subset of SDNS patients with FSGS as the probable histologic lesion using the two biomarkers (plasma suPAR levels and CD8+ memory T cells). eGFR was included in the model to adjust for the relationship between eGFR and suPAR levels, although all our patients had eGFR > 60 mL/min/1.73 m2. Demographic parameters were also included in order to correct for the potential sex- and age-dependent effects on CD8+ memory T cells. Additionally, sex and age have been shown to be predictors of poor renal outcome and response to therapy in other paediatric and adult studies.20,21,22,23,40 As this study focused only on patients with SDNS, steroid sensitivity was not included in the risk model.
In this model, we identified a threshold risk score of >24.0 as having a PPV of 100% and <13.3 with a 100% NPV. Therefore based on our model, a patient with a risk score of <13.3 will most likely have MCD, obviating the need for a kidney biopsy. This comprises patients aged <18 years with an eGFR of > 90 mL/min/1.73 m2 and percentage of CD8+ memory T cells >39.7%. On the other hand, FSGS is the most likely diagnosis on renal biopsy if the patients are >7 years of age with an eGFR between 60 and 90 mL/min/1.73 m2 and percentage of CD8+ memory T cells <24.6%. For patients with percentage of CD8+ memory T cells between 24.6 and 39.7%, inclusion of suPAR levels in the risk score model will help to improve the predictive value for FSGS, justifying the need for renal biopsy. In fact, a large cohort study in children with CKD showed that high suPAR levels were associated with progression of renal disease,13 consistent with what has been observed in the adult patient population.12
This risk model is useful in clinical practice as it makes it easier to justify the indication and timing of kidney biopsy, a procedure deemed to be safe but still invasive and that causes a lot of anxiety in the parents and the patients. The applicability of the results of this study may be limited by its small sample size. We therefore proceeded to test this model in a separate cohort of patients with SRNS. Our risk score model fared equally well in terms of predictive (80.0%) accuracy for FSGS, although in patients with SRNS this is a moot point, since renal biopsy is recommended for all of these patients in our centre.
In conclusion, we have developed a risk score model to stratify children with SDNS for renal biopsy using biomarkers associated with the disease. Patients with a risk score of >24.0 should undergo kidney biopsy as there is a high likelihood of FSGS on histology. We recognize the limitations of overgeneralization of these findings based on our single study population. There is hence a need to test the risk score model in a separate large validation cohort of patients with SDNS. This risk score model, if validated, may help in early diagnosis of FSGS in patients with SDNS and therefore guide the selection of alternative immunosuppressive therapy minimizing the toxic effects of prolonged use of high-dose steroids and before progressive renal injury ensues.
References
Hogg, R., Middleton, J. & Vehaskari, V. M. Focal segmental glomerulosclerosis--epidemiology aspects in children and adults. Pediatr. Nephrol. 22, 183–186 (2007).
Hahm, E. et al. Bone marrow-derived immature myeloid cells are a main source of circulating suPAR contributing to proteinuric kidney disease. Nat. Med. 23, 100–106 (2017).
Blasi, F. & Carmeliet, P. uPAR: a versatile signalling orchestrator. Nat. Rev. Mol. Cell Biol. 3, 932–943 (2002).
Wei, C. et al. Circulating urokinase receptor as a cause of focal segmental glomerulosclerosis. Nat. Med. 17, 952–960 (2011).
Hayek, S. S. et al. A tripartite complex of suPAR, APOL1 risk variants and alphavbeta3 integrin on podocytes mediates chronic kidney disease. Nat. Med. 23, 945–953 (2017).
Delville, M. et al. A circulating antibody panel for pretransplant prediction of FSGS recurrence after kidney transplantation. Sci. Transl. Med. 6, 256ra136 (2014).
Wei, C. et al. Circulating suPAR in two cohorts of primary FSGS. J. Am. Soc. Nephrol. 23, 2051–2059 (2012).
Li, F. et al. Relationship between serum soluble urokinase plasminogen activator receptor level and steroid responsiveness in FSGS. Clin. J. Am. Soc. Nephrol. 9, 1903–1911 (2014).
Meijers, B. K. & Reiser, J. Reassessing the reassessment of suPAR in glomerular disease. Front. Med. 1, 59 (2014).
Huang, J. et al. Plasma soluble urokinase receptor levels are increased but do not distinguish primary from secondary focal segmental glomerulosclerosis. Kidney Int. 84, 366–372 (2013).
Peng, Z. et al. Serum suPAR levels help differentiate steroid resistance from steroid-sensitive nephrotic syndrome in children. Pediatr. Nephrol. 30, 301–307 (2015).
Hayek, S. S. et al. Soluble urokinase receptor and chronic kidney disease. N. Engl. J. Med. 373, 1916–1925 (2015).
Schaefer, F. et al. Association of serum soluble urokinase receptor levels with progression of kidney disease in children. JAMA Pediatr. 171, e172914 (2017).
Strehlau, J. et al. Activated intrarenal transcription of CTL-effectors and TGF-beta1 in children with focal segmental glomerulosclerosis. Kidney Int. 61, 90–95 (2002).
Benz, K. et al. Characterisation of renal immune cell infiltrates in children with nephrotic syndrome. Pediatr. Nephrol. 25, 1291–1298 (2010).
Le Berre, L. et al. Renal macrophage activation and Th2 polarization precedes the development of nephrotic syndrome in Buffalo/Mna rats. Kidney Int. 68, 2079–2090 (2005).
Le Berre, L. et al. Induction of T regulatory cells attenuates idiopathic nephrotic syndrome. J. Am. Soc. Nephrol. 20, 57–67 (2009).
Schwartz, G. J. & Work, D. F. Measurement and estimation of GFR in children and adolescents. Clin. J. Am. Soc. Nephrol. 4, 1832–1843 (2009).
Chan, C. Y. et al. T lymphocyte activation markers as predictors of responsiveness to rituximab among patients with FSGS. Clin. J. Am. Soc. Nephrol. 11, 1360–1368 (2016).
Abrantes, M. M. et al. Predictive factors of chronic kidney disease in primary focal segmental glomerulosclerosis. Pediatr. Nephrol. 21, 1003–1012 (2006).
Alexopoulos, E., Stangou, M., Papagianni, A., Pantzaki, A. & Papadimitriou, M. Factors influencing the course and the response to treatment in primary focal segmental glomerulosclerosis. Nephrol. Dial. Transplant. 15, 1348–1356 (2000).
Chitalia, V. C., Wells, J. E., Robson, R. A., Searle, M. & Lynn, K. L. Predicting renal survival in primary focal glomerulosclerosis from the time of presentation. Kidney Int. 56, 2236–2242 (1999).
Rydel, J. J., Korbet, S. M., Borok, R. Z. & Schwartz, M. M. Focal segmental glomerular sclerosis in adults: presentation, course, and response to treatment. Am. J. Kidney Dis. 25, 534–542 (1995).
Velosa, J. A., Holley, K. E., Torres, V. E. & Offord, K. P. Significance of proteinuria on the outcome of renal function in patients with focal segmental glomerulosclerosis. Mayo Clin. Proc. 58, 568–577 (1983).
Nephrotic syndrome in children: prediction of histopathology from clinical and laboratory characteristics at time of diagnosis. A report of the International Study of Kidney Disease in Children. Kidney Int. 13, 159–165 (1978).
Alshami, A. et al. Indications for kidney biopsy in idiopathic childhood nephrotic syndrome. Pediatr Nephrol. 32, 1897–1905 (2017).
Cathelin, D. et al. Administration of recombinant soluble urokinase receptor per se is not sufficient to induce podocyte alterations and proteinuria in mice. J. Am. Soc. Nephrol. 25, 1662–1668 (2014).
Morath, C. et al. Management of severe recurrent focal segmental glomerulosclerosis through circulating soluble urokinase receptor modification. Am. J. Ther. 20, 226–229 (2013).
Staeck, O. et al. Recurrent primary focal segmental glomerulosclerosis managed with intensified plasma exchange and concomitant monitoring of soluble urokinase-type plasminogen activator receptor-mediated podocyte beta3-integrin activation. Transplantation 99, 2593–2597 (2015).
Franco Palacios, C. R. et al. Urine but not serum soluble urokinase receptor (suPAR) may identify cases of recurrent FSGS in kidney transplant candidates. Transplantation 96, 394–399 (2013).
Riisbro, R., Christensen, I. J., Hogdall, C., Brunner, N. & Hogdall, E. Soluble urokinase plasminogen activator receptor measurements: influence of sample handling. Int. J. Biol. Markers 16, 233–239 (2001).
Sever, S., Trachtman, H., Wei, C. & Reiser, J. Is there clinical value in measuring suPAR levels in FSGS? Clin. J. Am. Soc. Nephrol. 8, 1273–1275 (2013).
Sier, C. F. et al. Presence of urokinase-type plasminogen activator receptor in urine of cancer patients and its possible clinical relevance. Lab. Investig. 79, 717–722 (1999).
Yan, K. et al. The increase of memory T cell subsets in children with idiopathic nephrotic syndrome. Nephron 79, 274–278 (1998).
Stachowski, J. et al. Th1/Th2 balance and CD45-positive T cell subsets in primary nephrotic syndrome. Pediatr. Nephrol. 14, 779–785 (2000).
Salcido-Ochoa, F. et al. Analysis of T cell subsets in adult primary/idiopathic minimal change disease: a pilot study. Int. J. Nephrol. 2017, 3095425 (2017).
Krawczyk, C. M., Shen, H. & Pearce, E. J. Functional plasticity in memory T helper cell responses. J. Immunol. 178, 4080–4088 (2007).
Adamthwaite, D. & Cooley, M. A. CD8+T-cell subsets defined by expression of CD45 isoforms differ in their capacity to produce IL-2, IFN-gamma and TNF-beta. Immunology 81, 253–260 (1994).
Wada, T. et al. A multicenter cross-sectional study of circulating soluble urokinase receptor in Japanese patients with glomerular disease. Kidney Int. 85, 641–648 (2014).
Chun, M. J., Korbet, S. M., Schwartz, M. M. & Lewis, E. J. Focal segmental glomerulosclerosis in nephrotic adults: presentation, prognosis, and response to therapy of the histologic variants. J. Am. Soc. Nephrol. 15, 2169–2177 (2004).
Funding
This work was supported by grants from the Singapore Immunology Network (SIgN) and the National Medical Research Council (NMRC), Singapore.
Author information
Authors and Affiliations
Contributions
C.-Y.C. performed the experiments, analysed data and wrote the paper. L.P.R. collected the patient samples and analysed the clinical data and wrote the paper. Y.-H.C. provided critical advice to statistical analysis. M.A.Q. and M.T. collected the patient samples and maintained the clinical database. W.-S.Y., I.D.L. and P.Y.-W.L. provided intellectual input and recruited subjects. A.H.-L.L. and P.-H.T. provided input on renal pathology. C.W., J.R. and S.K.B. provided critical input for preparation of the manuscript. K.-H.N. and H.-K.Y. conceptualized the experiments, recruited subjects, provided input for analysis and interpretation of data and wrote the paper. All authors read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
J.R. is inventor on pending and issued patents related to antiproteinuric therapies targeting suPAR. He stands to gain royalties from present and future commercialization. He is also cofounder and advisor to TRISAQ, a biotechnology company. C.W. has a pending patent on suPAR in diabetes. He stands to gain royalties from future commercialization products concerning this application. The other authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chan, CY., Resontoc, L.P., Qader, M.A. et al. MeSsAGe risk score: tool for renal biopsy decision in steroid-dependent nephrotic syndrome. Pediatr Res 85, 477–483 (2019). https://doi.org/10.1038/s41390-019-0277-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0277-z