Abstract
Background
The influence of severity of anemia and cardiac output (CO) on cerebral oxygenation (CrSO2) and on the change in CrSO2 following packed red blood cell (PRBC) transfusion in preterm infants has not been evaluated. The objectives of the current study were to evaluate the effect of pre-transfusion hemoglobin (Hb) and CO-weighted oxygen delivery index (ODI) on CrSO2 and on the post-transfusion CrSO2 change.
Methods
Preterm infants of <32 weeks gestational age (GA) receiving PRBC transfusion were enrolled. Infants received 15 ml/kg PRBC over 3 h. CrSO2 by near-infrared spectroscopy and CO by electrical velocimetry were recorded for 1 h pre-ransfusion and post transfusion. ODI was defined as pre-transfusion Hb × CO.
Results
Thirty infants of 26.6 ± 2.0 weeks GA were studied at 19 ± 12 days. Pre-transfusion Hb was 9.8 ± 0.6 g/dl. Pre-transfusion CrSO2 correlated with pre-transfusion ODI (R2 = 0.1528, p = .044) but not with Hb level. The pre-transfusion to post-transfusion CrSO2 change correlated with pre-transfusion ODI (R2 = 0.1764, p = .029) but not with Hb level. CrSO2 increased from 66 ± 6% to 72 ± 7% post transfusion (p < .001), while arterial oxygen saturation, heart rate, and CO did not change.
Conclusion
In these infants, the pre-transfusion ODI was a better indicator of brain oxygenation and its improvement post transfusion than Hb alone. The role of CO and tissue oxygenation monitoring in assessing the need for transfusion should be evaluated.
Similar content being viewed by others
Introduction
A large proportion of very preterm infants develop anemia during their stay in the neonatal intensive care unit due to insufficient erythropoiesis and frequent blood sampling. Severe anemia may adversely affect organ function due to inadequate oxygen supply to meet the oxygen demand. Currently, physicians use clinical symptoms and/or arbitrary values of hematocrit or hemoglobin (Hb) for defining the severity of anemia and the threshold for its treatment with packed red blood cell (PRBC) transfusion without much evidence for its effect on long-term outcomes.1,2
Previous studies have shown that anemia is associated with decreased regional cerebral oxygen saturation (CrSO2) measured non-invasively by near-infrared spectroscopy (NIRS) in premature infants and transfusion of PRBC results in an increase in CrSO2, reflecting a higher oxygen saturation in the mixed vascular bed of the brain.3,4,5,6
The use of Hb value to define severity of anemia can be questioned since the amount of oxygen delivered to a tissue is not only determined by the oxygen content of blood but also by the amount of blood flowing through the tissues. It is plausible that some of the infants may compensate for the decrease in Hb concentration in blood with an increase in cardiac output (CO).7 The interaction between Hb and CO and its effect on CrSO2 in preterm infants with anemia and PRBC transfusion have not been previously described.
The objectives of the current study were to evaluate the effect of the severity of anemia and the CO-weighted oxygen delivery index (ODI) on pre-transfusion CrSO2 and on the change in CrSO2 post PRBC transfusion.
Methods
The study was conducted at the Project NewBorn Neonatal Intensive Care Unit at Holtz Children’s Hospital of the Jackson Health System – University of Miami Medical Center during March 2014 to June 2017. Preterm infants born at <32 weeks of gestational age (GA) who received clinically indicated blood transfusion for anemia were enrolled.
This observational study was approved by the Institutional Review Board of the University of Miami and the Clinical Trials Office of the Jackson Health System to be conducted with waiver of consent. All data were de-identified.
All infants received irradiated, leukocyte reduced, PRBC volume of 15 ml/kg body weight over a 3-hour period. Pre-transfusion Hb was documented from a clinically indicated blood sample immediately preceding the transfusion. Demographics and other clinical data were collected from the clinical records.
CrSO2 was obtained by NIRS (INVOS 5100, Covidien-Medtronic, Minneapolis, MN, USA) with the neonatal sensor placed above the supraorbital margin and lateral to the midline on the forehead. This device uses a light-emitting diode with near-infrared light at the two wavelengths 730 and 810 nm. The reflected light is detected by two photo detectors placed 3 and 4 cm from the light-emitting diode. The CrSO2 is calculated and displayed as oxygen-saturated Hb as a percentage of total Hb. CO was continuously monitored non-invasively by electrical velocimetry (EV) (Aesculon monitor, Cardiotronic, Osypka Medical, La Jolla, CA, USA). The principles and methods of estimation of CO by EV have been described in detail elsewhere.8,9 In short, EV measures the change in impedance that results from alignment of red blood cell before and after opening of the aortic valve to derive peak aortic acceleration and left ventricular ejection. The monitor provides continuous measurement of CO, stroke volume, and heart rate (HR). Arterial oxygen saturation (SpO2) was continuously measured by pulse oximetry (Radical 7, Masimo, Irvine, CA, USA).
Data were collected continuously for 1-h prior and 1 h after blood transfusion. To avoid the influence of episodes of hypoxemia, the CrSO2 and CO values corresponding to SpO2 of at least 90% were included in the analysis. Measured CrSO2 and CO data were used to calculate the mean value for each individual patient for the pre- and post-transfusion periods. The pre-transfusion ODI was calculated as the product of pre-transfusion Hb and the mean pre-transfusion CO for each infant [ODI = Hb (g/dl) × CO (l/kg/min)].
Within-subject comparisons of continuous variables was done by paired t test. Regression analysis was used to model the relationship and evaluate the correlation between two continuous variables. A p value <.05 was considered significant. Analysis was done using SPSS 25 Statistical Package (IBM Corporation, Armonk, NY, USA).
Results
Thirty preterm infants with GA of 26.6 ± 2.03 weeks were studied at postnatal age of 19 ± 12 days. Pre-transfusion Hb was 9.8 ± 0.6 g/dl, and all infants received 15 ml/kg of PRBC. Demographic and baseline pre-transfusion data are shown in Table 1. These infants were otherwise hemodynamically stable and not acutely ill at the time of the study.
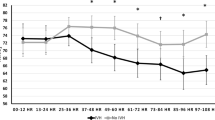
The pre-transfusion CrSO2 did not correlate with the pre-transfusion Hb level (R2 = .018, p = .475) as shown in Fig. 1a, but it correlated significantly with the pre-transfusion ODI (R2 = .153, p = .044) (Fig. 1b).
Correlation of pre-transfusion CrSO2 with pre-transfusion Hb and oxygen delivery index. The pre-transfusion CrSO2 did not correlate with the Hb level (R2 = .018, p = .475, a). In contrast, there was a significant correlation between pre-transfusion CrSO2 and the oxygen delivery index calculated as the product of Hb and CO (R2 = 0.153, p = .044, b)
The pre- to post-transfusion change in CrSO2 did not correlate with the pre-transfusion Hb level (R2 = .030, p = .361) (Fig. 2a). In contrast, the change in CrSO2 correlated negatively with the pre-transfusion ODI (R2 = .177, p = .029) (Fig. 2b).
Correlation of the change in CrSO2 after transfusion with the pre-transfusion Hb and oxygen delivery index. The pre- to post-transfusion percent change in CrSO2 did not correlate with the pre-transfusion Hb level (R2 = .030, p = .361, a). In contrast, the percent change in CrSO2 correlated significantly with the pre-transfusion oxygen delivery index (Hb×CO) (R2 = .177, p = .029, b)
The pre-transfusion CrSO2 or the pre- to post-transfusion change in CrSO2 did not correlate with the pre-transfusion CO (R2 = .131, p = .064 and R2 = .124, p = .072, respectively).
The mean CrSO2 increased from a pre-transfusion value of 66 ± 6.2 to 72 ± 6.6% after transfusion (p < .001). There was no significant difference in mean SpO2 with corresponding decrease in SpO2-CrSO2 gradient after transfusion. CO data could not be obtained in three infants due to technical problems. CO and HR measurements obtained in 27 infants showed they did not change with transfusion (Table 2).
Discussion
In this study, the pre-transfusion Hb level did not correlate with CrSO2 or with the increase in CrSO2 with transfusion. In contrast, the CO-weighted ODI (product of Hb and CO) had a significant influence on both the pre-transfusion CrSO2 and the increase in CrSO2 following PRBC transfusion.
The increase in CrSO2 with PRBC transfusion shown in the current study is consistent with previous reports.4,5 The finding of lack of correlation between pre-transfusion Hb level and CrSO2 in the present study is in disagreement with a previous report.10 This difference may be related to the higher pre-transfusion level and a narrower range of Hb in the infants enrolled in the present study. The observation of a positive correlation between the pre-transfusion ODI and CrSO2 suggests that some anemic infants have the ability to compensate for the reduced oxygen content by increasing brain and systemic blood flow, as reported earlier.11 This compensatory mechanism could also explain the observation of a correlation between the increase in CrSO2 with PRBC transfusion and the pre-transfusion ODI but not with Hb alone. However, it is unknown if these findings apply to infants with lower Hb levels than those in the present study.
EV has been used as a non-invasive method for continuous monitoring of CO with recent data showing correlation with measurements by echocardiography and thermodilution in preterm infants.12,13,14 Some of these studies have also raised concerns about the accuracy of EV for CO measurement in preterm infants related to the presence of patent ductus arteriosus (PDA) and the interference by high-frequency oscillation ventilators. Although the effect of a PDA is not conclusive12,15 and none of the enrolled infants was receiving treatment for PDA at the time of the study, the effect of a PDA on the accuracy of CO measurement cannot be ruled out. None of the infants in the present study was on high-frequency ventilation.
The current study highlights the limitations of using only the Hb level as threshold for PRBC transfusion rather than a marker of tissue oxygen delivery. The inadequacy of Hb as a single indicator of tissue oxygenation could be one of the reasons that studies comparing different Hb cut-off values for PRBC transfusion failed to show a significant effect on long-term neurodevelopmental outcome.1,2 It is plausible that non-invasive CO and regional tissue oxygenation monitoring may provide an additional insight into the infant’s compensatory mechanisms in face of anemia.
In conclusion, the pre-transfusion cardiac output-weighted ODI was a better indicator of brain oxygenation and its improvement after PRBC transfusion than Hb alone. The possible role of continuous non-invasive cardiac output and tissue oxygenation monitoring in assessing the need for transfusion in premature infants should be further evaluated.
References
Whyte, R. & Kirpalani, H. Low versus high haemoglobin concentration threshold for blood transfusion for preventing morbidity and mortality in very low birth weight infants. Cochrane Database Syst. Rev. CD000512 (2011). https://doi.org/10.1002/14651858.CD000512.pub2.
Whyte, R. K. et al. Neurodevelopmental outcome of extremely low birth weight infants randomly assigned to restrictive or liberal hemoglobin thresholds for blood transfusion. Pediatrics 123, 207–213 (2009).
Sandal, G. et al. Assessment of red blood cell transfusion and transfusion duration on cerebral and mesenteric oxygenation using near-infrared spectroscopy in preterm infants with symptomatic anemia. Transfusion 54, 1100–1105 (2014).
Seidel, D. et al. Changes in regional tissue oxygenation saturation and desaturations after red blood cell transfusion in preterm infants. J. Perinatol. 33, 282–287 (2013).
Bailey, S. M. et al. Packed red blood cell transfusion increases regional cerebral and splanchnic tissue oxygen saturation in anemic symptomatic preterm infants. Am. J. Perinatol. 27, 445–453 (2010).
Whitehead, H. V. et al. Anemia of prematurity and cerebral near-infrared spectroscopy: should transfusion thresholds in preterm infants be revised? J. Perinatol. 38, 1022–1029 (2018).
Alkalay, A. L. et al. Hemodynamic changes in anemic premature infants: are we allowing the hematocrits to fall too low? Pediatrics 112, 838–845 (2003).
Grollmuss, O. & Gonzalez, P. Non-invasive cardiac output measurement in low and very low birth weight infants: a method comparison. Front. Pediatr. 2, 16 (2014).
Osypka, M. J. & Bernstein, D. P. Electrophysiologic principles and theory of stroke volume determination by thoracic electrical bioimpedance. AACN Clin. Issues 10, 385–399 (1999).
van Hoften, J. C. et al. Cerebral tissue oxygen saturation and extraction in preterm infants before and after blood transfusion. Arch. Dis. Child. Fetal Neonatal Ed. 95, F352–F358 (2010).
Pryds, O. & Greisen, G. Effect of PaCO2 and haemoglobin concentration on day to day variation of CBF in preterm neonates. Acta Paediatr. Scand. Suppl. 360, 33–36 (1989).
Song, R. et al. The use of electrical cardiometry for continuous cardiac output monitoring in preterm neonates: a validation study. Am. J. Perinatol. 31, 1105–1110 (2014).
Noori, S. et al. Continuous non-invasive cardiac output measurements in the neonate by electrical velocimetry: a comparison with echocardiography. Arch. Dis. Child. Fetal Neonatal Ed. 97, F340–F343 (2012).
Norozi, K. et al. Electrical velocimetry for measuring cardiac output in children with congenital heart disease. Br. J. Anaesth. 100, 88–94 (2008).
Blohm, M. E. et al. Effect of patent ductus arteriosus and patent foramen ovale on left ventricular stroke volume measurement by electrical velocimetry in comparison to transthoracic echocardiography in neonates. J. Clin. Monit. Comput. 31, 589–598 (2017).
Acknowledgments
This work was supported by the University of Miami Project NewBorn. Unrestricted equipment support was provided by Covidien/Medtronic and Cardiotronic/Osypka Medical.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jain, D., D’Ugard, C., Bancalari, E. et al. Cerebral oxygenation in preterm infants receiving transfusion. Pediatr Res 85, 786–789 (2019). https://doi.org/10.1038/s41390-018-0266-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0266-7
This article is cited by
-
Early brain and abdominal oxygenation in extremely low birth weight infants
Pediatric Research (2022)
-
Transfusion prevention using erythropoietin, parenteral sucrose iron, and fewer phlebotomies in infants born at ≤30 weeks gestation at a high altitude center: a 10-year experience
Journal of Perinatology (2021)