Abstract
Gambling disorder (GD) is a behavioral addiction that may be linked to alterations in dopamine (DA) systems. Gambling involves chronic exposure to uncertain reward, which can sensitize the activity of DA systems. Here we explored how combinations of Pavlovian and instrumental uncertainty impact DA sensitization and risky decision-making. Experiment 1: 40 rats underwent 66 uncertainty exposure (UE) sessions during which they responded for saccharin. Animal responding was reinforced according to a fixed or variable (FR/VR) ratio schedule that turned on a conditioned stimulus (CS; light), which predicted saccharin on 50% or 100% of trials. Animals responded under one of the four conditions: FR-CS100% (no uncertainty), VR-CS100%, FR-CS50%, and VR-CS50% (maximal uncertainty). DA sensitization was inferred from an enhanced locomotor response to d-amphetamine (d-AMPH; 0.5 mg/kg) challenge. The rat gambling task (rGT) was used to assess decision-making. Experiment 2: 24 rats received 5 weeks of sensitizing d-AMPH or saline doses, followed by locomotor activity and rGT testing. Experiment 3: Effects of UE and a sensitizing d-AMPH regimen on DA D1, D2, and D3 receptor binding were assessed in 44 rats using autoradiography. Compared to FR-CS100%, VR-CS100% and VR-CS50% rats displayed a greater locomotor response to d-AMPH, and VR-CS50% rats demonstrated riskier decision-making. Chronic d-AMPH-treated rats mirrored the effects of VR-CS50% groups on these two indices. Both VR-CS50% and d-AMPH-treated groups had increased striatal DA D2 receptor binding. These results suggest that chronic uncertainty exposure, similar to exposure to a sensitizing d-AMPH regimen, sensitized the function of DA systems and increased risky decision-making.
Similar content being viewed by others
Introduction
Gambling disorder (GD) is a psychiatric disorder that causes profound personal and social harm [1, 2] and occurs in ~1% of the population [3]. Based on similar risk factors, neural mechanisms, and cognitive impairments, GD was classified as the first behavioral addiction alongside Substance use disorders (SUD) in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition [4, 5]. Although SUD medications have shown promise for GD, especially opioid antagonists [6, 7], no medication has been formally approved for GD [7], possibly due to a lack of a GD animal model.
Chronic drug use can induce neuroplastic changes; for example, repeated exposure to psychostimulant drugs can sensitize the functional activity of the dopamine (DA) systems [8, 9], and this process may play a fundamental role in the development and maintenance of addiction [10,11,12]. Like drugs, uncertain reward delivery increases firing of midbrain DA neurons in non-human primates, with the strongest effect observed under maximally uncertain conditions (50% reward probability) [13]. This closely matches the relative frequency and inconsistency of reward delivery over the course of trials on slot machines [14], suggesting that chronic uncertain reward during gambling could induce drug-like neuroplasticity. Slot machines provide salient cues (spinning reels) to evoke expectation of potential reward delivery on every trial; some slot machines also deliver reward (credits >0) on just under 50% of trials, with no advance information to predict which trial will deliver a winning outcome [14]. Based on evidence from non-human primates [13], slot machines would be expected to increase phasic DA upon unexpected reward delivery (reward prediction error) and tonic DA during the anticipatory interval while reels are spinning (reward anticipation under uncertainty). Because uncertainty of reward delivery is never resolved, this DA activity can persist indefinitely, much as it does with drugs of abuse [15]. Therefore, if GD is a behavioral addiction, chronic exposure to gambling may cause GD symptoms, much like chronic drug exposure causes substance addiction [16].
Uncertainty exposure (UE) enhances the locomotor stimulant effect of d-amphetamine (d-AMPH) in rats [17,18,19], which is an indirect measure of DA sensitization [8, 20, 21]. Specifically, repeated exposure to an uncertain conditioned sucrose reward (light conditioned stimulus (CS) predicted sucrose 50% of time) potentiated locomotor response to a d-AMPH challenge relative to a certain conditioned reward (CS predicted sucrose 100% of time) following repeated d-AMPH doses [22]. Chronic exposure to uncertain saccharin rewards earned on an unpredictable variable ratio (VR) vs. a predictable fixed ratio (FR) schedule of reinforcement also enhanced, or sensitized, locomotor activity [17, 18] and DA release in the ventral striatum/nucleus accumbens (NAc) [19] in response to a d-AMPH challenge. Repeated exposure to reward uncertainty also encouraged risky decision-making on the rat gambling task (rGT) [18].
In people with GD, a d-AMPH challenge evoked greater dorsal striatal DA release when compared to healthy controls, which positively correlated with their (offline) speed of slot machine play, a measure of psychomotor activation [23]. Likewise, subjects classified as pathological gamblers also demonstrate increased risky decision-making on laboratory tests [24,25,26]. Together, these findings implicate uncertainty-induced DA sensitization in the risky decision-making that typifies GD [24, 25].
The acute and chronic pharmacological effects of d-AMPH are mediated by multiple, functionally heterogeneous subregions of the striatum (along with other brain structures) [27,28,29]. The regional neuroplasticity induced by chronic UE and chronic d-AMPH can be assessed with ex vivo autoradiography to quantify DA receptors in these subregions, including the NAc shell and core, and the ventromedial and dorsolateral caudate–putamen.
The present experiments extended the investigation of the relationship between uncertainty, DA sensitization, and risky decision-making. Specifically, we assessed: (a) the combined effects of FR/VR and CS50%/100% components, which more closely approximate the instrumental and Pavlovian uncertainty of slot machine gambling, on d-AMPH-probed locomotor sensitization and rGT decision-making in Experiment 1; (b) effects of a sensitizing regimen of d-AMPH on the same outcome measures in Experiment 2 to see whether the pattern of effects resembled the effects of UE in Experiment 1; and (c) DA D1, D2, and D3 receptor binding in striatal subregions following the UE and d-AMPH regimens in Experiment 3. We predicted increased locomotor activity and riskier choices in VR-CS100%, FR-CS50%, and VR-CS50% rats and chronic d-AMPH-treated rats, when compared to their respective FR-CS100% or saline-treated controls. If chronic UE and d-AMPH cause similar neuroplasticity, this should be evident in congruent subregional changes in DA receptor expression, relative to their respective controls.
Materials and methods
Subjects
Male Sprague-Dawley rats (225–250 g) were pair-housed in a temperature-controlled, reversed 12-h light–dark cycle room (lights off at 0800 hours). All testing occurred during the dark, and animals received water and chow freely unless otherwise stated. Procedures followed Canadian Council on Animal Care guidelines and were approved by the Animal Care Committee at the Centre for Addiction and Mental Health.
Experiment 1: effect of UE on locomotor activity and rGT
Forty rats were randomized to 4 groups that received different UE training: FR-CS100%, VR-CS100%, FR-CS50% and VR-CS50% groups (n = 10/group). These groups were chosen to assess different combinations of instrumental (FR vs. VR) and Pavlovian (CS100% vs. CS50%) uncertainty on locomotor activity and decision-making using the rGT.
Uncertainty exposure
Animals were trained in Med Associates operant conditioning chambers (St. Albans, VT, USA). A red cue light was located 12 cm above a nose-poke hole on the left panel of the right wall of the chamber. A receptacle was centered in the middle panel for delivery of 0.1 ml saccharin solution (0.3% w/v in water; saccharin sodium salt hydrate; Sigma Aldrich, St. Louis, MO, USA) from a 20-ml syringe mounted on an external syringe pump. A house-light was located centrally, near the top of the left wall. The right panel was solid (i.e., no inactive nose-poke hole was present), similar to previous studies [17, 18].
UE training began after one 25-min habituation session in the chambers. During training, a reinforced nose-poke turned on a red light (CS) for 5 s. Nose-pokes were reinforced according to a FR or VR schedule of reinforcement [17]. The CS was followed by delivery of 0.1 ml saccharin with either 50% or 100% certainty [22]. Thus rats were trained under one of the four regimens: FR-CS100% (no uncertainty), VR-CS100% (instrumental uncertainty), FR-CS50% (Pavlovian uncertainty), and VR-CS50% (maximal uncertainty).
All animals were trained once in the morning, then half of the animals were tested again in the afternoon. The following day, all animals were again tested in the morning and the other half were tested again in the afternoon for a total of 66 sessions. This testing protocol was used as only eight operant chambers were available and previous studies utilized twice-daily testing schedules [18, 19].
For the first 2 sessions, the ratio schedule was set at 1 (i.e., each nose-poke activated the CS and reinforcement was delivered). Then rats transitioned to their respective training groups during which the CS and saccharin reinforcement were delivered according to the FR/VR schedule. When a rat had received 30 saccharin reinforcers on 2 consecutive sessions, its ratio value was increased [17]. The 100% groups were trained on ratios 1, 3, 5, 7, 10, 13, 16, and 20, while 50% groups advanced to schedule 10 only.
The rationale to only train the CS50% groups to a FR/VR ratio 10 schedule was to ensure the number of nose-pokes required to receive saccharin reinforcement was the same between the CS50% and CS100% groups when the final ratio was reached (i.e., CS50% at FR/VR10 and CS100% at FR/VR20). Because the 50% groups had half the opportunities to obtain reinforcement as 100% groups, animals in the 100% groups could obtain the same number of reinforcers with half the responses.
The first 53 sessions were 40 min in duration, and sessions 54–66 were 60 min in duration. An increased session duration was used to provide rats more time to achieve 30 saccharin reinforcers within each session, as some animals were not yet at their final FR/VR schedule. At the end of training, some animals still had not reached the final FR/VR schedule. However, removal of these animals did not statistically alter any results. Therefore, their data were included for all subsequent analyses.
Locomotor activity test
Nineteen days after UE training, locomotor activity was assessed. Testing occurred in clear polycarbonate chambers (45 cm length × 24 cm width × 21 cm height) with 11 infrared photodetectors crossing the bottom of each chamber [18]. Locomotor activity was measured as the number of photocell beam breaks for 60 min on separate sessions following intraperitoneal (i.p.) injections of saline and d-AMPH sulfate (0.5 mg/kg in 1 ml/kg; Sigma Aldrich, St. Louis, MO, USA) [17].
Rat gambling task
Once locomotor testing was completed, animals were food restricted to maintain 85–90% of free-feeding weight and rats were subsequently tested on the rGT.
Rats were tested once daily in Med Associates five-hole operant conditioning chambers (St. Albans, VT, USA) as previously described [18, 30, 31]. The left wall contained five stimulus holes positioned horizontally, with the middle (third) hole not utilized. The right wall had a centered pellet receptacle that could be illuminated and an overhead house-light. Sucrose pellets (Bioserv # F0021; Flemington, NJ, USA) were delivered into the receptacle from an external dispenser.
Animals initially received four forced-choice training sessions during which only one option was presented to the animal on each trial. This ensured that subsequent rGT performance was not biased by limited exposure [18, 30, 31]. Rats were then tested once daily on the rGT for 40 sessions, according to previously described methods (see [18, 30, 31]). A trial began when a rat nose-poked in the illuminated pellet receptacle, initiating a 5-s inter-trial interval (ITI) in darkness, before illumination of the 4 stimulus holes. Failure to respond within 10 s re-illuminated the pellet receptacle (omitted trial), and responses within the 5-s ITI (premature responses) were followed by illumination of the house-light for 5 s before the pellet receptacle light, similar to the 5-choice serial reaction time task [18, 30,31,32].
A response in an illuminated hole within 10 s resulted in delivery of sucrose pellets in the pellet receptacle (rewarded trial) or flashing of the stimulus light for the time-out (punished trial). Since each session was 30-min, longer time-outs decreased the maximum amount of reward that could be obtained. As seen in Table 1, the four stimulus holes were individually assigned to a different pellet option. The advantageous P1 and P2 (1-pellet and 2-pellet, respectively) options maximized the net number of pellets that could be delivered within a session, whereas the disadvantageous P3 and P4 (3-pellet and 4-pellet, respectively) options yielded a greater number of pellets on a rewarded trial but were associated with more frequent and longer time-outs, resulting in fewer total pellets delivered within the session [18, 30].
Rats were randomized to rGT Version A or B, in which stimulus options in A were arranged from left to right as P1, P4, P2, and P3 and options in B were P4, P1, P3, and P2 [18, 30].
Choice preference throughout training was calculated as the average percentage of choice of the advantageous (P1+P2) minus disadvantageous (P3+P4) options in blocks of five consecutive sessions. For the last five sessions (once choice preferences were statistically stable), choice was compared between groups as a Score (%advantageous choice − %disadvantageous choice).
Experiment 2: effect of a sensitizing regimen of d-AMPH on locomotor activity and rGT
Animals were sensitized to d-AMPH or received saline injections (control group) to indirectly compare the impact of behavioral (Experiment 1) and psychostimulant (Experiment 2) sensitizing regimens on locomotor activity and rGT testing.
Following habituation to the facility, 24 rats were mildly food restricted, then trained for 7 sessions on an FR1 training program to teach animals to nose-poke for sucrose pellets. Locomotor activity testing commenced 3 days later.
Locomotor activity test prior to sensitization
Locomotor activity testing duration and apparatus were identical to those described in Experiment 1. Rats assigned to the saline-treated group (n = 12) received single i.p. injections of saline both times during locomotor testing; rats in the d-AMPH-treated group (n = 12) received saline for the first test, then 0.5 mg/kg d-AMPH for the second test.
Sensitizing regimen of d-AMPH
Similar to previous studies [33, 34], over 5 weeks, rats received i.p. injections of saline or d-AMPH (1 ml/kg) in their home cages on Mondays, Wednesdays, and Fridays. The d-AMPH dose started at 1 mg/kg and increased by 1 mg/kg per week to a final dose of 5 mg/kg.
Locomotor activity test following sensitization
Similar to Experiment 1, 17 days elapsed before locomotor activity testing was repeated under identical conditions as before the regimen.
Rat gambling task
Animals were then food restricted to maintain 85–90% of free-feeding weight and rGT testing occurred for 40 sessions, identical to methods described in Experiment 1.
Experiment 3: effects of UE or a sensitizing regimen of d-AMPH on DA receptor binding
To determine whether similar behavioral effects of chronic UE and d-AMPH in Experiments 1 and 2 were accompanied by similar neuroplasticity, we examined posttreatment DA receptor binding in the corresponding test and control groups.
To observe changes following UE, 24 rats were randomized to FR-CS100% and VR-CS50% groups (n = 12/group) and underwent UE training identical to methods described in Experiment 1. A comparison between these groups was chosen as they correspond to minimal and maximal UE, respectively, and because VR-CS50% showed evidence of both locomotor sensitization and increased risky decision-making on the rGT (see “Results,” Supplementary Information).
Animals received twice daily 40-min UE training sessions for 54 sessions. For sessions 55–66, rats were trained during single 60-min daily sessions. Similar to Experiment 1, the longer session duration attempted to aid some animals in obtaining the larger FR/VR schedule. Likewise, although some animals still did not reach the highest FR/VR schedule, removal of these animals did not statistically alter any results, therefore their data were included.
After 17 days post-training (a comparable number of days following UE before starting rGT testing in Experiment 1), rats were sacrificed and their brains extracted for autoradiography. The locomotor activity test used in Experiment 1 was omitted to ensure that DA receptor binding reflected changes induced by UE and not by exposure to d-AMPH.
To investigate potential changes in DA receptor binding following d-AMPH sensitization, a second cohort of 20 rats was randomized to saline or d-AMPH treatment (n = 10/group). Identical to the methods described in Experiment 2, rats first received a locomotor activity test prior to sensitization, then were treated with saline or escalating doses of amphetamine for 5 weeks. After 17 days, a second locomotor activity test was conducted in which animals received saline or d-AMPH (0.5 mg/kg i.p.). This second locomotor test was conducted to ensure animals were sensitized to d-AMPH and that the saline group showed no effects of sensitization to the saline injections [35]. Three days later, when d-AMPH had been eliminated from the bloodstream, animals were sacrificed and their brains extracted.
Receptor autoradiography
Rats were sacrificed by decapitation, brains were immediately removed, frozen on dry ice, and stored at −80 °C. Twenty-micron sections were cut on a cryostat, thaw-mounted, and then stored at −80 °C.
Quantitative autoradiography for DA D1, D2, and D3 receptors was performed as previously described [36, 37]. For DA D1 binding, slides were preincubated in 50 mM Tris HCl (pH 7.4) containing 120 mM NaCl, 4 mM MgCl2, 1.5 mM CaCl2, 1 mM EDTA, and 5 mM KCl for 2 h at 24 °C, followed by the same buffer with 2 nM [3H]SCH 23390 (83.2 Ci/mmol; Perkin Elmer, Woodbridge, ON, Canada) at 37 °C for 30 min, with or without 2 µM (+)-butaclamol to define non-specific binding [36]. Slides were then rinsed twice for 5 min in ice-cold buffer, quickly dipped in ice-cold deionized water, air-dried, and exposed to Biomax film (Carestream Health Canada, Vaughn, ON, Canada) for 4 weeks [36].
For DA D2 and D3 receptor binding, slides were preincubated for 2 h at 24 °C under the same buffer conditions as D1, (except KCl was omitted for [3H]PHNO), using 5 nM [3H]raclopride (76.2 Ci/mmol; Perkin Elmer, Woodbridge, ON, Canada), a D2-preferring radioligand, or 2 nM [3H]PHNO (46.8 Ci/mmol; Moravek Inc., Brea, CA, USA), a D3-preferring radioligand [37]. Slides were rinsed twice for 5 min in ice-cold buffer, quickly dipped in ice-cold deionized water, air-dried, and then exposed to Biomax film for 6 weeks. Non-specific binding was determined in the presence of 10 µM sulpiride [37].
The MCID Basic system (InterFocus Imaging, Linton, Cambridge, UK) was utilized for densitometric film analyses, with data expressed as µCi/gT using 3H-calibrated standards. Brain regions of interest included nucleus accumbens core (NAc-C), nucleus accumbens shell (NAc-Sh), dorsolateral caudate–putamen (CPu-DL), and ventromedial caudate–putamen (CPu-VM), identified from Paxinos and Watson [38].
Statistical analyses
Data were analyzed using SPSS version 24.0, with significance acknowledged at p < 0.05, and visualized using SigmaPlot version 11.0. All t tests were two-tailed and corrected upon significance of Levene’s test. All percentage values were arcsine transformed to reduce the impact of a ceiling effect [18, 39].
UE testing
Primary UE training variables were the total number of sessions spent at the highest UE ratio, reinforcers received, nose-pokes completed, and CS presentations on the last 5 UE sessions. UE data were analyzed using Group (4 in Experiment 1, 2 in Experiment 3) × Session (last 5 sessions) analyses of variance (ANOVAs) with post hoc independent t tests or one-way ANOVAs with Dunnett’s t tests on the aggregate 5-session means if the Group effect was significant.
Locomotor testing
Locomotor data were calculated as the number of photocell beam breaks in 60 min for all Experiments. In Experiment 1, data were analyzed with a Group (UE Groups) × Dose (Saline, d-AMPH) ANOVA [17]. Planned contrasts compared each group to FR-CS100% control at each level of Dose; paired t tests compared each group across Dose. Saline- and d-AMPH-treated groups’ locomotor data were individually analyzed using a Test (Before vs. After regimen) × Dose (first vs. second injection) ANOVA and a priori paired t tests for within- and between-group comparisons.
In cases where training-related variables apart from UE (reinforcers received, nose-pokes completed) differed significantly by group, follow-up analyses with the same ANOVA design and planned comparisons were conducted to assess locomotor response when variance due to the potential confounder(s) was controlled statistically using regression residuals. This permitted unambiguous attribution of group differences in the primary outcome variable (beam breaks) to the UE manipulation.
In the case of locomotor responding, the residuals were obtained by regressing the 60-min beam break scores for the saline and for the d-AMPH session onto reinforcers and nose-pokes during UE training (simultaneous entry of total number of reinforcers and nose-pokes across 66 sessions) and saving the unstandardized residual of each analysis. The residual excludes variance contributed by all predictors but retains variance on the dependent variable [40]. The residual scores from these regressions were then analyzed using the original Group (UE groups) × Dose (Saline, d-AMPH) ANOVA design with planned comparisons (t tests) for the difference between each UE group and FR-CS100% control.
Decision-making in rGT
Primary outcome variables from the rGT included advantageous (%P1+%P2) vs. disadvantageous (%P3+%P4) choices (% choice = [choices of an option ÷ trials completed] × 100%) and Score (%choice advantageous − %choice disadvantageous options). Data for 40 rGT sessions were aggregated into 8 blocks of 5 consecutive sessions each. Advantageous rGT choices were analyzed using Group (4 in Experiment 1, 2 in Experiment 2) × Version (A or B) × Block (mean of 5 sessions/Block × 8) ANOVAs and a priori paired t tests on 5-session means of advantageous vs. disadvantageous choices [18]. To assess the final pattern of responding, Score was assessed using Group × Version × Session (last 5 sessions: 36–40) ANOVAs [18] and compared with a priori t tests (saline vs. d-AMPH treated) or planned contrasts (FR-CS100% vs. each UE group) on the 5-session means data. As there were no significant interactions involving Group and Version, data from both versions were combined, in keeping with previous studies [18, 30, 31, 41].
Receptor autoradiography
A priori independent groups’ t tests compared striatal DA receptor radioligand binding in FR-CS100% vs. VR-CS50% and saline- vs. d-AMPH-treated groups.
As in the case of locomotor responses, if group differences emerged in training-related variables apart from UE, the same ANOVA and t tests were repeated when the dependent measures were converted to regression residuals, eliminating variance due to the potential confounder(s) [40]. These analyses, along with analyses of outcomes from other test variables, are reported in Supplementary Information.
Results
Experiment 1: effect of UE on locomotor activity and rGT
There were no significant differences between groups on the number of sessions completed at the highest ratio (Group: F(3,36) = 0.784, p = 0.511; Fig. 1a) or CS presentations (Group: F(3,36) = 2.133, p = 0.113; Fig. 1d). For the number of reinforcers (Fig. 1b) and nose-pokes (Fig. 1c), VR-CS100% rats demonstrated significantly higher mean scores when compared to control FR-CS100% rats (Group: F(3,36) = 6.041, p = 0.002; F(3,36) = 6.121, p = 0.002).
UE training in Experiment 1 rats (n = 10/group) led to no difference in the number of sessions spent at the highest attained ratio (a) or mean CS presentations (d) on the last 5 sessions. However, the VR-CS100% group obtained a significantly higher mean number of reinforcers (b) and completed a higher mean number of nose-pokes (c) when compared to the FR-CS100% group. On the locomotor activity test that followed, a d-amphetamine (d-AMPH; 0.5 mg/kg i.p.) challenge increased locomotor activity in all groups and VR-CS100% rats had a significantly higher d-AMPH response when compared to FR-CS100% group (e). In regard to the saline response, there were no differences between FR-CS100% vs. VR-CS100%/FR-CS50%/VR-CS50% groups. To control for variation in the total number of reinforcers received and nose-pokes completed during training, locomotor activity scores following UE treatment in the four groups of rats (n = 12/group) following acute challenge injections with saline and d-amphetamine (d-AMPH; 0.5 mg/kg, i.p.) were converted to regression residuals. The grand mean for the sample = 0; and individual bars show residualized group means. (f) There were no significant differences among the groups in response to saline; whereas (g) both VR-CS100% and VR-CS50% groups differed significantly from FR-CS100% control (p's < 0.05) when variance from potential confounders was controlled. The data are shown as mean ± standard error. Asterisk (*) represents p ≤ 0.05 for comparisons against FR-CS100% control, while dagger (†) represents p ≤ 0.05 for within-group comparisons.
Locomotor activity test
Following UE, locomotor response was significantly increased in response to d-AMPH challenge vs. Saline (Dose: F(1,36) = 106.246, p < 0.001), with no significant Dose × Group interaction (F(3,36) = 2.600, p = 0.067). Planned contrasts comparing each experimental group to FR-CS100% control in response to the d-AMPH challenge revealed a significant between-group difference for the VR-CS100% group, with no group differences to saline (Fig. 1e).
The ANOVA of regression residuals for d-AMPH and Saline injections yielded a non-significant Group × Dose interaction (F(3,36) = 1.785, p = 0.167). However, a priori tests confirmed a significant difference between VR-CS100% and FR-CS100% (t(36) = 2.22, p < 0.02) and also revealed a significantly greater locomotor response to d-AMPH in VR-CS50% rats vs. FR-CS100% control (t(36) = 2.33, p < 0.02). Residuals for VR-CS100% vs. VR-CS50% did not differ from one another (p > 0.50). Similarly, FR-CS50% rats did not differ significantly from FR-CS100% controls (p > 0.10).
Figure 1f shows data for the saline injection and confirms that groups displayed very similar locomotor performance under drug-free conditions, when variance due to reinforcers received and nose-pokes completed during training was statistically controlled, as was evident from the raw scores (Fig. 1e). In contrast, Fig. 1g shows that, after the d-AMPH challenge, both groups exposed to instrumental UE (VR-CS50% and VR-CS100%) displayed significant locomotor sensitization relative to no uncertainty (FR-CS100%), when extraneous variance was statistically controlled, whereas Pavlovian UE alone (FR-CS50%) was not associated with a significant difference in locomotor response relative to the FR-CS100% control.
Rat gambling task
Group differences were found across blocks of 5 sessions on the choice of advantageous options (Block × Group: F(21,224) = 2.103, p = 0.004). The FR-CS100%, VR-CS100%, and FR-CS50% groups preferred the advantageous to disadvantageous options (Fig. 2a–c), while the VR-CS50% rats did not. Although the VR-CS50% rats initially chose advantageously, they increasingly chose from the disadvantageous options as sessions progressed (Fig. 2d). In addition, analysis of the Score (advantageous − disadvantageous choices) using planned contrasts between FR-CS100% vs. the UE groups on the mean of the last block of 5 sessions revealed a significantly lower score for the VR-CS50% group (Fig. 2e).
Following the locomotor activity test in Experiment 1, (a) FR-CS100%, (b) VR-CS100%, and (c) FR-CS50% groups significantly chose the advantageous over the disadvantageous options across blocks (mean of 5 sessions/block) on the rat gambling task (rGT). Meanwhile, the VR-CS50% rats increasingly chose from the disadvantageous options (d) and had a lower mean score (advantageous − disadvantageous choices) (e) than the control FR-CS100% group. The data are shown as mean ± standard error and asterisk (*) represents p ≤ 0.05 for within-group comparisons, while dagger (†) represents p ≤ 0.05 for comparisons against FR-CS100% control rats.
As shown in Supplementary Information (Fig. S1), the same pattern of significant group differences in advantageous decisions was seen in the analyses of regression residuals. The groups’ choice of each individual pellet option (P1–P4) on the rGT (Table S1), in addition to other measures (Fig. S2, Table S2), is also shown in Supplementary Information.
Experiment 2: effect of a sensitizing regimen of d-AMPH on locomotor activity and rGT
Locomotor activity tests
Saline-treated rats did not demonstrate an increase in locomotor response to saline (Fig. 3a). d-AMPH-treated rats demonstrated a clear increase in locomotor response to acute d-AMPH challenge. Locomotor activity increased following d-AMPH vs. saline on tests before and after chronic dosing (Fig. 3b). Comparisons between tests revealed a significant Test × Dose interaction (F(1,11) = 12.825, p = 0.004). A priori tests confirmed that the response to the second injection at pretreatment and posttreatment did not differ in saline-treated rats (t < 0.30, p > 0.50), whereas the pretreatment–posttreatment increase in response to d-AMPH challenge was significant in chronic d-AMPH-treated rats (t(22) = 10.290, p < 0.0001).
Locomotor activity tests before and after the 5-week regimen in Experiment 2 saline-treated rats (n = 12/group) (a) revealed a significantly lower locomotor response from the first to the second saline injection within each test, with a lower response to the first injection on the test after 5 weeks when compared to before. (b) In turn, chronic d-amphetamine (d-AMPH)-treated rats demonstrated a significantly higher locomotor activity following the d-AMPH challenge (0.5 mg/kg i.p.) within each test and a higher response to d-AMPH after the sensitizing d-AMPH regimen when compared to before. (c) On the rat gambling task (rGT) that followed, saline-treated rats significantly chose the advantageous over the disadvantageous options throughout rGT blocks (mean of 5 consecutive sessions = mean block score), while d-AMPH-treated rats increasingly chose from the disadvantageous options (d) and had a lower mean score (e) at the end of the rGT. The data are shown as mean ± standard error and asterisk (*) represents p ≤ 0.05 for within-group comparisons against previous test or disadvantageous option. Dagger (†) represents p ≤ 0.05 when compared to the previous injection within the same test and double dagger (‡) represents p ≤ 0.05 for between-group comparisons.
Rat gambling task
Differences between saline- and d-AMPH-treated groups on choice of advantageous options across blocks were found (Block × Group: F(7,140) = 3.096, p = 0.005). Saline-treated rats chose significantly more advantageous over disadvantageous options throughout (Fig. 3c), while d-AMPH-treated rats increasingly preferred the disadvantageous options as sessions continued (Fig. 3d). In addition, group Scores (advantageous − disadvantageous choices) differed significantly on the last 5 sessions (Group: F(1,20) = 4.657, p = 0.043), with d-AMPH-treated rats exhibiting a lower mean score (Fig. 3e). Additional measures as in Experiment 1 can also be found in Supplementary Information (Tables S3 and S4, Fig. S3).
Experiment 3: effects of UE or a sensitizing regimen of d-AMPH on DA receptor binding
Uncertainty exposure
FR-CS100% and VR-CS50% groups did not differ on the total number of sessions completed at the highest ratio (t(17.369) = 1.729, p = 0.101; Fig. 4a), number of reinforcers (Group: F(1,22) = 0.245, p = 0.626; Fig. 4b), or nose-pokes completed (Group: F(1,22) = 0.018, p = 0.894; Fig. 4c) on the last 5 sessions of UE training. However, the VR-CS50% group had a significantly higher mean number of CS presentations when compared to FR-CS100% rats (Group: F(1,22) = 9.657, p = 0.005; Fig. 4d).
Groups (FR-CS100%, VR-CS50%; n = 12/group) trained on uncertainty exposure (UE) for Experiment 3 did not differ on the number of sessions spent at the highest ratio (a), mean number of reinforcers (b), and mean number of nose-pokes (c), with the exception for the mean number of CS presentations (d) on the last 5 sessions. Meanwhile, saline-treated rats (n = 10/group) exposed to locomotor activity tests before and after the 5-week regimen had a significantly lower response on the second saline injection from the first and there were no differences across tests (e). (f) d-AMPH-treated rats demonstrated a significantly higher locomotor activity following the d-AMPH challenge (0.5 mg/kg, i.p.) vs. saline injection on the test after the 5-week regimen, with a significantly higher d-AMPH response after 5 weeks when compared to before. For autoradiography, (i) VR-CS50% rats demonstrated significantly higher dopamine (DA) D2 ([3H]raclopride) receptor binding in the nucleus accumbens core (NAc-C), nucleus accumbens shell (NAc-Sh), dorsolateral caudate–putamen (CPu-DL), and ventromedial caudate–putamen (CPu-VM), while (j) d-AMPH-treated rats revealed a significant increase only in the NAc-Sh. However, there were no differences between groups in the DA D1 ([3H]SCH 23390) (g, h) and D3 ([3H]PHNO) (k, l) receptor bindings in any of the brain regions. The data are shown as mean ± standard error and double dagger (‡) represents p ≤ 0.05 for between-group comparisons. Also, dagger (†) represents p ≤ 0.05 when compared to the previous injection within the same test and asterisk (*) represent p ≤ 0.05 for within-group comparisons against previous test.
Sensitizing regimen of d-AMPH and locomotor activity tests
Saline-treated rats did not exhibit behavioral sensitization (Fig. 4e). Compared to saline-treated rats, d-AMPH-treated rats exhibited locomotor sensitization based on a Test × Dose interaction (F(1,9) = 8.473, p = 0.017). Locomotor response to d-AMPH challenge increased significantly after the 5-week regimen (t(9) = 2.728, p = 0.025), with no corresponding change for the saline injection (Fig. 4f).
Receptor autoradiography
Relative to their control groups, UE-treated and chronic d-AMPH-treated rats showed no difference in D1 receptor [3H]SCH 23390 binding (Fig. 4g, h) or D3 receptor [3H]PHNO binding (Fig. 4k, l) in the four subregions of the striatum (NAc-C, NAc-Sh, CPU-DL, and CPU-VM). Significantly higher D2 receptor [3H]raclopride binding was demonstrated in all four subregions for the VR-CS50% vs. FR-CS100% groups (t(22) ≥ 2.238, p ≤ 0.036; Fig. 4i). A parallel pattern was observed in d-AMPH- vs. saline-treated rats (Fig. 4j), with a significant difference only seen in NAc-Sh (t(18) = 2.655, p = 0.016) but not in other regions (p ≥ 0.088) (Fig. 4j).
Figure 5 shows the autoradiographic images, which illustrate the pattern of [3H]raclopride binding in the striatal subregions for the chronic d-AMPH and VR-CS50% groups relative to their respective controls.
(a) Rats (n = 10/group) chronically exposed to saline or d-amphetamine (d-AMPH) in a 5-week, escalating dose (1–5 mg/kg/day), three times/week injection regimen previously described for Experiment 2; and (b) groups of rats (n = 12/group) chronically exposed to FR-CS100% or VR-CS50% as described for Experiment 1. a, b show that, in both cases, the density of D2-binding sites is markedly greater in the test vs. control groups.
To ensure that the group difference in [3H]raclopride binding for the VR-CS50% vs. FR-CS100% groups was not mediated by the difference in CS presentations during the final 5 sessions of training, regression residuals for [3H]raclopride binding in each striatal subregion were computed controlling for variation in CS presentations. The significant main effect of group and pattern of effects (VR-CS50% > FR-CS100% in each subregion) remained unchanged (see Fig. S4).
Discussion
These experiments extend our investigation of UE as a possible model of how chronic gambling may induce GD symptoms. In Experiment 1, the VR-CS100% and VR-CS50% groups each displayed a greater locomotor response to d-AMPH challenge relative to the FR-CS100% control. These results implicate instrumental uncertainty (VR) in inducing a sensitization-like state. Likewise, these findings align with previous studies that exposed rats to uncertain reward delivery according to a VR schedule of reinforcement and reported a sensitization of d-AMPH-probed locomotor activity compared to rats exposed to a certain FR schedule [17,18,19]. Therefore, chronic unpredictable reward, regardless of antecedent cues, is sufficient to increase d-AMPH-induced behavioral sensitization, an index of DA sensitization [8, 20, 21].
Regarding rGT decision-making, the VR-CS50% group increasingly chose from the disadvantageous options and demonstrated a lower score on the last five sessions when compared to FR-CS100% controls. In contrast, the FR-CS100%, VR-CS100%, and FR-CS50% groups sustained advantageous decision-making throughout testing. The exact same pattern was found when variation due to reinforcers received and nose-pokes committed during training was controlled statistically with regression residuals (Supplementary Information). These findings extend our previous study by Zeeb et al., which showed that rats chronically exposed to a VR schedule of reinforcement engage in risk-taking on the rGT [18].
In the present experiments, we hypothesize that inclusion of a certain CS (CS100%) diminished the ability of a VR schedule of reinforcement in VR-CS100% rats to promote risk-taking. However, animals in the VR-CS50% group demonstrated a preference for the risky, disadvantageous rGT options. Therefore, a certain or uncertain CS schedule (CS50% or 100%) can modify the contribution of UE through a VR schedule on risky decision-making. This finding is important not only because combined Pavlovian and instrumental uncertainty corresponds better to the features of slot machines but also because Pavlovian uncertainty coincides with an escalation of tonic DA between the onset of the CS and delivery of the unpredictable unconditioned stimulus (US), and this process has been suggested to contribute to the reinforcing properties of gambling (e.g., eager anticipation or “suspense”) over and above the effects of unpredictable reward delivery per se (i.e., pleasant surprise) [13]. Moreover, in healthy humans, anticipation of uncertain reward activates the ventral striatum (NAc), whereas delivery and omission of a reward previously associated with a CS activate and inhibit, respectively, the medial prefrontal cortex (mPFC) [42]. Because optimal decision-making relies on interactions between mPFC and ascending DA neurons [43], disturbance of mPFC signaling by chronic random CS–US pairings could impair discriminative responding to signals for reward. Such a disturbance may partly account for the disruptive effects of 50% CS in both the VR-CS50% (increased choice of maximally risky option; P4) and FR-CS50% (increased choice of moderately risky/sub-optimal option; P3) groups on the rGT (see Supplementary Information).
Experiment 2 tested whether a sensitizing d-AMPH regimen results in a similar pattern of decision-making as UE did in Experiment 1. First, chronic d-AMPH-treated rats displayed a sensitized locomotor response to d-AMPH, corresponding to the locomotor sensitization seen in the VR-CS100% and VR-CS50% groups in Experiment 1 and other d-AMPH sensitization studies [33, 34, 44, 45]. Second, and more importantly, the d-AMPH-treated group demonstrated suboptimal decision-making. This manifested as a decrease in the proportion of advantageous choices on the rGT and a significantly lower Score compared to saline-treated rats in the last five sessions on the task. Therefore, both repeated VR-CS50% training and d-AMPH sensitization increased risky decision-making. These findings extend recent evidence of increased risk-taking in rats following chronic cocaine exposure [46, 47] and suggest that common neuroplastic changes may contribute to the impaired decision-making observed following chronic exposure to psychostimulants and UE.
Although d-AMPH acts primarily on the DA system, it also modulates norepinephrine and serotonin [48, 49]. Therefore, the acute (i.e., challenge) and chronic effects of d-AMPH in our experiments may reflect alterations in these other systems. Support for the contribution of DA in the UE effects comes from Mascia et al. who detected increased NAc DA release using microdialysis following a d-AMPH challenge in rats chronically exposed to a VR vs. FR schedule [19].
Experiment 3 extended Mascia et al.’s microdialysis findings [19] by investigating changes in DA D1, D2, and D3 receptor binding using autoradiography following UE or a sensitizing regimen of d-AMPH. Both VR-CS50% and d-AMPH-treated rats displayed an increase in striatal DA D2 receptor binding, relative to their respective controls. The difference between the VR-CS50% and FR-CS100% groups was significant in NAc-C, NAc-Sh, CPu-VM, and CPu-DL subregions and in the NAc-Sh for d-AMPH-treated vs. saline-treated groups. A clear pattern of elevated D2 receptor binding was also seen in other striatal subregions (Cohen’s d > 0.69; moderate effect size) for d-AMPH-treated rats.
Selective upregulation of striatal DA D2 receptor following d-AMPH sensitization aligns with previous research that found sensitized behavioral responses to DA D2 receptor agonists, but not to DA D1 receptor agonists, in rats exposed to sensitizing regimens of methamphetamine, cocaine, or d-AMPH [50, 51]. Therefore, increased striatal DA D2 receptor binding may be a reliable feature of psychostimulant sensitization that is also induced by chronic exposure to UE in drug-free rats.
The comparable increase in locomotor activity to a d-AMPH challenge following UE and a d-AMPH regimen indicates a common state of DA sensitization, consistent with the enhanced dorsal striatal DA response to acute d-AMPH seen in humans with GD vs. healthy controls [23]. However, it contrasts with the deficits in stimulant-induced DA release seen in human psychostimulant abusers [52]. Similarly, our discovery of increased striatal DA D2 receptor binding contrasts with the reduction in D2 receptor binding observed in imaging studies of human psychostimulant abusers [52]. Previous research has suggested that dosing may explain different patterns of striatal DA D2 receptor binding. Unlike our study, humans typically administer binge-like doses of psychostimulants, which may promote receptor downregulation and neurotoxicity [53,54,55].
Elevated striatal DA D2 receptor binding in VR-CS50% rats is inconsistent with four positron emission tomographic studies that found no difference in striatal DA D2 binding in humans with GD vs. controls [56,57,58,59]. Trait differences in DA D2 receptor binding may partly account for this. Specifically, impulsivity is inversely related to DA D2 receptor levels in healthy humans and in those with GD [56, 60, 61]. Thus elevated impulsivity (lower D2) may have offset potential gambling-related DA D2 receptor upregulation when scores were aggregated across individuals with GD, resulting in no net difference in GD vs. control groups. Isolating variance in D2 receptor expression due to traits (genes, impulsivity) vs. syndrome-related factors (gambling exposure, GD) is an important consideration for future mechanistic and clinically oriented research in GD.
Collectively, the three experiments demonstrate a parallel effect of UE and a sensitizing d-AMPH regimen on GD-like risky decision-making and DA-related neuroplasticity. The validity of our UE regimen is supported by previous research showing that the payoff schedule on a commercial slot machine closely approximates maximal uncertainty (50% rewarded trials) [14]. The CS50% manipulation approximates the “window of uncertainty” from which a winning configuration on a slot machine may (e.g., five cherries) or may not (e.g., four cherries and a lemon) emerge. The FR/VR manipulation approximates the inconsistent delivery of reward for a given number of instrumental responses, i.e., spins on a slot machine (lever pulls or button presses).
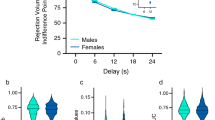
Our experiments are limited by the relatively modest sample sizes and sole use of male subjects. Since females with GD start gambling at a later age and display more rapid onset of symptoms [62, 63], it would be important in future studies to determine whether sex differences exist in response to UE. In addition, the imperfect correspondence between UE and real-world gambling must be acknowledged. First, although the high ratio VR schedule employed here delivers reward quasi-randomly, slot machines deliver reward on a random schedule [64], which may result in less pronounced anticipation of reward than VR. Second, although omission of an expected reward during UE is mildly stressful [65], it likely does not match the averseness of large monetary losses experienced during gambling. Third, our UE procedure lacks the real-world gambling feature of jackpots, which could be incorporated in future studies. In fact, research with non-human primates has shown that DA release is more strongly influenced by variability of reward size over trials than by the total reward delivered [13]. Fourth, questions remain about the site of DA sensitization following UE exposure (ventral vs. dorsal striatum), as DA transmission in both regions has been implicated in GD [23, 58, 59]. Finally, it is unclear whether the increased DA D2 receptor binding observed in VR-CS50% and chronic d-AMPH-treated rats applies to presynaptic and/or postsynaptic receptors [66, 67].
Despite these limitations, our findings show that response-based/instrumental uncertainty (VR) induces a sensitization of DA function, while its combination with cue-based/Pavlovian uncertainty in the VR-CS50% group promotes risky decision-making, analogous to that observed after chronic d-AMPH exposure. However, instrumental uncertainty when combined with a certain CS (CS100%) in the VR-CS100% condition does not encourage disadvantageous choices. This suggests that VR’s effect on decision-making is affected by the uncertainty/certainty associated with the CS. Collectively, our findings provide strong empirical support for the parallel role of DA in the effects of chronic gambling-like uncertainty and chronic d-AMPH on locomotor sensitization, risky decision-making, and DA receptor binding. Our experiments indicate that chronic exposure to uncertainty effectively models key features of GD and may serve as an animal model for future screening of medications for individuals with GD.
Funding and disclosure
This work was funded by a grant to MHZ, PJF, and FDZ from the International Center for Responsible Gaming. Some of the data were presented during the 10th Annual Canadian Neuroscience Meeting hosted by the Canadian Association for Neuroscience (May, 2016; Toronto, Ontario) and the 17th Annual National Center for Responsible Gaming Conference on Gambling and Addiction (September, 2016; Las Vegas, Nevada). FDZ was also supported by a Canadian Institutes of Health Research Postdoctoral Fellowship and MHZ currently holds an NCRG grant All the authors have no competing financial interests to report in relation to this work.
References
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edition. Washington, DC: American Psychiatric Publishing; 2013.
Grant JE, Odlaug BL, Chamberlain SR. Neural and psychological underpinnings of gambling disorder: a review. Prog Neuropsychopharmacol Biol Psychiatry. 2016;65:188–93.
Hodgins DC, Stea JN, Grant JE. Gambling disorders. Lancet. 2011;378:1874–84.
Frascella J, Potenza MN, Brown LL, Childress AR. Shared brain vulnerabilities open the way for nonsubstance addictions: carving addiction at a new joint? Ann NY Acad Sci. 2010;1187:294–315.
Petry NM, Blanco C, Auriacombe M, Borges G, Bucholz K, Crowley TJ, et al. An overview of and rationale for changes proposed for pathological gambling in DSM-5. J Gambl Stud. 2014;30:493–502.
Menchon JM, Mestre-Bach G, Steward T, Fernández-Aranda F, Jiménez-Murcia S. An overview of gambling disorder: from treatment approaches to risk factors. F1000Res. 2018;7:434.
Yip SW, Potenza MN. Treatment of gambling disorders. Curr Treat Options Psychiatry. 2014;1:189–203.
Paulson PE, Robinson TE. Amphetamine-induced time-dependent sensitization of dopamine neurotransmission in the dorsal and ventral striatum: a microdialysis study in behaving rats. Synapse. 1995;19:56–65.
Boileau I, Dagher A, Leyton M, Gunn RN, Baker GB, Diksic M, et al. Modeling sensitization to stimulants in humans: an [11C]raclopride/positron emission tomography study in healthy men. Arch Gen Psychiatry. 2006;63:1386–95.
Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Brain Res Rev. 1993;18:247–91.
Robinson TE, Berridge KC. Review. The incentive sensitization theory of addiction: some current issues. Philos Trans R Soc Lond B Biol Sci. 2008;363:3137–46.
Berridge KC, Robinson TE. Liking, wanting, and the incentive-sensitization theory of addiction. Am Psychol. 2016;71:670–9.
Fiorillo CD, Tobler PN, Schultz W. Discrete coding of reward probability and uncertainty by dopamine neurons. Science. 2003;299:1898–902.
Tremblay AM, Desmond RC, Poulos CX, Zack M. Haloperidol modifies instrumental aspects of slot machine gambling in pathological gamblers and healthy controls. Addict Biol. 2011;16:467–84.
Redish AD. Addiction as a computational process gone awry. Science. 2004;306:1944–7.
Volkow N, Li TK. The neuroscience of addiction. Nat Neurosci. 2005;8:1429.
Singer BF, Scott-Railton J, Vezina P. Unpredictable saccharin reinforcement enhances locomotor responding to amphetamine. Behav Brain Res. 2012;226:340–4.
Zeeb FD, Li Z, Fisher DC, Zack MH, Fletcher PJ. Uncertainty exposure causes behavioural sensitization and increases risky decision-making in male rats: toward modelling gambling disorder. J Psychiatry Neurosci. 2017;42:404–13.
Mascia P, Neugebauer NM, Brown J, Bubula N, Nesbitt KM, Kennedy RT, et al. Exposure to conditions of uncertainty promotes the pursuit of amphetamine. Neuropsychopharmacology. 2019;44:274–80.
Robinson TE, Becker JB. Enduring changes in brain and behavior produced by chronic amphetamine administration: a review and evaluation of animal models of amphetamine psychosis. Brain Res. 1986;396:157–98.
Vanderschuren LJMJ, Pierce RC. Sensitization processes in drug addiction. In: Self DW, Staley Gottschalk JK, editors. Behavioral neuroscience of drug addiction, vol. 3. Berlin, Heidelberg: Springer; 2010. p. 179–95.
Zack M, Featherstone RE, Mathewson S, Fletcher PJ. Chronic exposure to a gambling-like schedule of reward predictive stimuli can promote sensitization to amphetamine in rats. Front Behav Neurosci. 2014;8:1–15.
Boileau I, Payer D, Chugani B, Lobo DSS, Houle S, Wilson AA, et al. In vivo evidence for greater amphetamine-induced dopamine release in pathological gambling: a positron emission tomography study with [(11)C]-(+)-PHNO. Mol Psychiatry. 2014;19:1305–13.
Ciccarelli M, Griffiths MD, Nigro G, Cosenza M. Decision making, cognitive distortions and emotional distress: a comparison between pathological gamblers and healthy controls. J Behav Ther Exp Psychiatry. 2017;54:204–10.
Goudriaan AE, Oosterlaan J, de Beurs E, van den Brink W. Decision making in pathological gambling: a comparison between pathological gamblers, alcohol dependents, persons with Tourette syndrome, and normal controls. Cogn Brain Res. 2005;23:137–51.
Krmpotich T, Mikulich-Gilbertson S, Sakai J, Thompson L, Banich MT, Tanabe J. Impaired decision-making, higher impulsivity, and drug severity in substance dependence and pathological gambling. J Addiction Med. 2015;9:273.
Di Chiara G, Tanda G, Frau R, Carboni E. On the preferential release of dopamine in the nucleus accumbens by amphetamine: further evidence obtained by vertically implanted concentric dialysis probes. Psychopharmacology. 1993;112:398–402.
Pierce RC, Kalivas PW. A circuitry model of the expression of behavioral sensitization to amphetamine-like psychostimulants. Brain Res Rev. 1997;25:192–216.
Wolf ME, Sun X, Mangiavacchi S, Chao SZ. Psychomotor stimulants and neuronal plasticity. Neuropharmacology. 2004;47:61–79.
Zeeb FD, Robbins TW, Winstanley CA. Serotonergic and dopaminergic modulation of gambling behavior as assessed using a novel rat gambling task. Neuropsychopharmacology. 2009;34:2329–43.
Zeeb FD, Winstanley CA. Functional disconnection of the orbitofrontal cortex and basolateral amygdala impairs acquisition of a rat gambling task and disrupts animals’ ability to alter decision-making behavior after reinforcer devaluation. J Neurosci. 2013;33:6434–43.
Robbins TW. The 5-choice serial reaction time task: behavioural pharmacology and functional neurochemistry. Psychopharmacology. 2002;163:362–80.
Featherstone RE, Rizos Z, Kapur S, Fletcher PJ. A sensitizing regimen of amphetamine that disrupts attentional set-shifting does not disrupt working or long-term memory. Behav Brain Res. 2008;189:170–9.
Fletcher PJ, Tenn CC, Rizos Z, Lovic V, Kapur S. Sensitization to amphetamine, but not PCP, impairs attentional set shifting: reversal by a D1 receptor agonist injected into the medial prefrontal cortex. Psychopharmacology. 2005;183:190–200.
Fletcher PJ, Li Z, Coen KM, Lê AD. Acquisition of nicotine self-administration in amphetamine and phencyclidine models of schizophrenia: a role for stress? Schizophr Res. 2018;194:98–106.
Sasaki T, Kennedy JL, Nobrega JN. Regional brain changes in [3H]SCH 23390 binding to dopamine D1, receptors after long-term haloperidol treatment: lack of correspondence with the development of vacuous chewing movements. Behav Brain Res. 1998;90:125–32.
Nobrega JN, Seeman P. Dopamine D2 receptors mapped in rat brain with [3H](+)PHNO. Synapse. 1994;17:167–72.
Paxinos G, Watson C. The rat brain in stereotaxic coordinates. 4th ed. New York: Academic Press; 1998.
McDonald JH. Handbook of biological statistics. 3rd edn. Baltimore, MD: Sparky House Publishing; 2014.
McNamee R. Regression modelling and other methods to control confounding. Occup Environ Med. 2005;62:500–6.
Zeeb FD, Wong AC, Winstanley CA. Differential effects of environmental enrichment, social-housing, and isolation-rearing on a rat gambling task: dissociations between impulsive action and risky decision-making. Psychopharmacology. 2013;225:381–95.
Knutson B, Fong GW, Bennett SM, Adams CM, Hommer D. A region of mesial prefrontal cortex tracks monetarily rewarding outcomes: characterization with rapid event-related fMRI. Neuroimage. 2003;18:263–72.
Popescu AT, Zhou MR, Poo MM. Phasic dopamine release in the medial prefrontal cortex enhances stimulus discrimination. Proc Natl Acad Sci USA. 2016;113:E3169–76.
Tenn CC, Fletcher PJ, Kapur S. Amphetamine-sensitized animals show a sensorimotor gating and neurochemical abnormality similar to that of schizophrenia. Schizophr Res. 2003;64:103–14.
Tenn CC, Kapur S, Fletcher PJ. Sensitization to amphetamine, but not phencyclidine, disrupts prepulse inhibition and latent inhibition. Psychopharmacology. 2005;180:366–76.
Cocker PJ, Rotge J-Y, Daniel M-L, Belin-Rauscent A, Belin D. Impaired decision making following escalation of cocaine self-administration predicts vulnerability to relapse in rats. Addict Biol. 2019. https://doi.org/10.1111/adb12738.
Kim WY, Cho BR, Kwak MJ, Kim J-H. Interaction between trait and housing condition produces differential decision-making toward risk choice in a rat gambling task. Sci Rep. 2017;7:5718.
Heal DJ, Smith SL, Gosden J, Nutt DJ. Amphetamine, past and present – a pharmacological and clinical perspective. J Psychopharmacol. 2013;27:479–96.
Wood S, Sage JR, Shuman T, Anagnostaras SG. Psychostimulants and cognition: a continuum of behavioral and cognitive activation. Pharm Rev. 2014;66:193–221.
Ujike H, Akiyama K, Otsuki S. D-2 but not D-1 dopamine agonists produce augmented behavioral response in rats after subchronic treatment with methamphetamine or cocaine. Psychopharmacology. 1990;102:459–64.
Vanderschuren LJ, Schoffelmeer AN, Mulder AH, De Vries TJ. Dopaminergic mechanisms mediating the long-term expression of locomotor sensitization following pre-exposure to morphine or amphetamine. Psychopharmacology. 1999;143:244–53.
Ashok AH, Mizuno Y, Volkow ND, Howes OD. Association of stimulant use with dopaminergic alterations in users of cocaine, amphetamine, or methamphetamine: a systematic review and meta-analysis. JAMA Psychiatry. 2017;74:511–9.
Thanos PK, Kim R, Delis F, Rocco MJ, Cho J, Volkow ND. Effects of chronic methamphetamine on psychomotor and cognitive functions and dopamine signaling in the brain. Behav Brain Res. 2017;320:282–90.
Ginovart N, Farde L, Halldin C, Swahn CG. Changes in striatal D2-receptor density following chronic treatment with amphetamine as assessed with PET in nonhuman primates. Synapse. 1999;31:154–62.
Villemagne V, Yuan J, Wong DF, Dannals RF, Hatzidimitriou G, Mathews WB, et al. Brain dopamine neurotoxicity in baboons treated with doses of methamphetamine comparable to those recreationally abused by humans: evidence from [11C]WIN-35,428 positron emission tomography studies and direct in vitro determinations. J Neurosci. 1998;18:419–27.
Clark L, Stokes PR, Wu K, Michalczuk R, Benecke A, Watson BJ, et al. Striatal dopamine D2/D3 receptor binding in pathological gambling is correlated with mood-related impulsivity. Neuroimage. 2012;63:40–6.
Boileau I, Payer D, Chugani B, Lobo D, Behzadi A, Rusjan PM, et al. The D2/3dopamine receptor in pathological gambling: a positron emission tomography study with [11C]-()-propyl-hexahydro-naphtho-oxazin and [11C]raclopride. Addiction. 2013;108:953–63.
Joutsa J, Johansson J, Niemelä S, Ollikainen A, Hirvonen MM, Piepponen P, et al. Mesolimbic dopamine release is linked to symptom severity in pathological gambling. Neuroimage. 2012;60:1992–9.
Linnet J, Møller A, Peterson E, Gjedde A, Doudet D. Dopamine release in ventral striatum during Iowa Gambling Task performance is associated with increased excitement levels in pathological gambling. Addiction. 2011;106:383–90.
Buckholtz JW, Treadway MT, Cowan RL, Woodward ND, Li R, Ansari MS, et al. Dopaminergic network differences in human impulsivity. Science. 2010;329:532.
Trifilieff P, Martinez D. Imaging addiction: D2 receptors and dopamine signaling in the striatum as biomarkers for impulsivity. Neuropharmacology. 2014;76(Pt B):498–509.
Tavares H, Martins SS, Lobo DS, Silveira CM, Gentil V, Hodgins DC. Factors at play in faster progression for female pathological gamblers: an exploratory analysis. J Clin Psychiatry. 2003;64:433–8.
Grant JE, Odlaug BL, Mooney ME. Telescoping phenomenon in pathological gambling: association with gender and comorbidities. J Nerv Ment Dis. 2012;200:996–8.
Haw J. Random-ratio schedules of reinforcement: the role of early wins and unreinforced trials. J Gambl Issues. 2008;21:56–67.
Vindas MA, Sørensen C, Johansen IB, Folkedal O, Höglund E, Khan UW, et al. Coping with unpredictability: dopaminergic and neurotrophic responses to omission of expected reward in Atlantic salmon (Salmo salar L.). PLoS ONE. 2014;9:e85543.
Anzalone A, Lizardi-Ortiz JE, Ramos M, De Mei C, Hopf FW, Iaccarino C, et al. Dual control of dopamine synthesis and release by presynaptic and postsynaptic dopamine D2 receptors. J Neurosci. 2012;32:9023–34.
Trifilieff P, Feng B, Urizar E, Winiger V, Ward RD, Taylor KM, et al. Increasing dopamine D2 receptor expression in the adult nucleus accumbens enhances motivation. Mol Psychiatry. 2013;18:1025–33.
Acknowledgements
We would like to thank Zhaoxia Li (Biopsychology Laboratory) for the collection of data for Experiment 3, Tony Ji (Biopsychology Laboratory) for slicing of the brains, and Roger Raymond (Behavioural Neurobiology Laboratory) for performing the autoradiography procedures.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Fugariu, V., Zack, M.H., Nobrega, J.N. et al. Effects of exposure to chronic uncertainty and a sensitizing regimen of amphetamine injections on locomotion, decision-making, and dopamine receptors in rats. Neuropsychopharmacol. 45, 811–822 (2020). https://doi.org/10.1038/s41386-020-0599-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-020-0599-x
This article is cited by
-
Investigating the Relationship Between Attention-Deficit Hyperactivity Disorder, Obligatory Exercise and Exercise Addiction
International Journal of Mental Health and Addiction (2023)