Abstract
In a previously reported longitudinal study of violent ideation (VI) and violent behavior (VB) among 200 youths at clinical high-risk (CHR) for psychosis, we found that VI, hitherto underinvestigated, strongly predicted transition to first-episode psychosis (FEP) and VB, in close temporal proximity. Here, we present participants’ baseline characteristics, examining clinical and demographic correlates of VI and VB. These participants, aged 13–30, were examined at Columbia University Medical Center’s Center of Prevention and Evaluation, using clinical interviews and the structured interview for psychosis-risk syndromes (SIPS). At the onset of our longitudinal study, we gathered demographics, signs and symptoms, and descriptions of VI and VB. One-third of participants reported VI (n = 65, 32.5%) at baseline, experienced as intrusive and ego-dystonic, and associated with higher suspiciousness and overall positive symptoms. Less than one-tenth reported VB within 6 months of baseline (n = 17, 8.5%), which was unrelated to SIPS-positive symptoms, any DSM diagnosis or other clinical characteristic. The period from conversion through post-FEP stabilization may be characterized by heightened risk of behavioral disinhibition and violence. We provide a preliminary model of how violence risk may peak at various points in the course of psychotic illness.
Similar content being viewed by others
Introduction
Schizophrenia and other psychotic disorders are generally preceded by an attenuated or clinical high-risk (CHR) phase, characterized by delusional ideas, perceptual disturbances, and disorganization of thought, with lower levels of conviction, intensity, frequency, and behavioral impact than seen in full-blown psychosis [1]. Such subthreshold positive symptoms are evaluated using the structured interview for psychosis-risk syndromes (SIPS) [2], a measure that delineates an attenuated positive symptom syndrome (APSS). This construct served as the basis for the attenuated psychosis syndrome (APS), included in the current edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) as a condition warranting further research [3]. Both the APS and APSS are highly heterogeneous, with regard to diagnosis, encompassing individuals with possible features of a number of other DSM categories, but who display a specific constellation of symptoms suggestive of potential emergent psychosis. Such persons are uncommon, with an estimated prevalence in the general population as low as 0.3% and an estimated annual incidence of 1/10,000 [4]. Furthermore, relatively few CHR individuals, generally not more than 30–35% in the most robust samples, actually progress to full-blown psychotic illness [1].
A newly emerging line of inquiry suggests that the CHR state may constitute a period of increased risk for violence, a topic of considerable current interest. Although most individuals with mental illness are not dangerous and the majority of violence is committed by people without mental disorders, there is some evidence that positive symptoms of full-blown schizophrenia and other psychoses [5,6,7,8,9], such as delusions and hallucinations, are related to VB [10,11,12,13,14,15]. Nonadherence to medications [16, 17] and poor insight [18] have been shown to mediate this. Nielssen and Large [19], examining the prevalence of homicide in psychosis, reported that approximately 1 in 9000 persons with psychosis who have received treatment commit homicide each year, while 1 homicide occurs for every 629 presentations of first-episode psychosis. Other research suggests that alcohol [20, 21] or drug abuse [22,23,24,25] are the key mediating factors, and may account for more of the risk than psychosis [26,27,28,29,30]. Langeveld et al. [31] prospectively examined violence, as well as multiple clinical characteristics, including substance use, among 178 first-episode participants for 10 years. A decade postbaseline, 20% of participants had been arrested or incarcerated, though most of these events occurred before baseline. At the 10-year follow-up, 15% had exposed others to threats or violence in the prior year. Illegal drug use at baseline and the 5-year mark was predictive of violence in the year preceding endpoint evaluation.
Other possible mediating factors have been identified. A report from the UK National EDEN study [32] suggested that there may be multiple pathways to violence in first-episode psychosis and that lifelong antisocial traits should be considered alongside psychotic symptomatology. A meta-regression analysis of 100 studies by Witt et al. [33] found criminal history, substance, or alcohol use, nonadherence with psychotherapy and medication, poor impulse control, and prior hostile behavior to be associated with violence. Coid et al. [34] particularly implicate paranoid ideation as the link between violence and psychosis.
Violence risk in the CHR phase of psychotic illness has been far less frequently examined. Marshall et al. [35] reported that 24% of 442 CHR individuals described violent content during SIPS interviews, with 12% reporting multiple types of violent content. Such content was associated with more severe positive symptoms, anxiety, negative beliefs about oneself, and being the target of bullying prior to age 16. Notably, violent content was defined to include thoughts of harm to the self by others—that is to say, suspicious concerns with violent content—which constituted the most common subtype. Content surrounding hurting others (11.54%) and perceptual disturbances related to interpersonal violence (3.17%) were less common. Violent content in relation to actual violent behaviors was not investigated.
Recently, we presented results of a longitudinal study of 200 CHR youth, ages 13–30. Each was examined for up to 2 years for VI and VB using the SIPS and clinical interview [36]. Violent content was rated according to categories drawn from the MacArthur Community Violence Interview [29]. VB within the 6 months preceding initial assessment and VI at baseline both very strongly predicted transition to first-episode psychosis (FEP), as well as VB within an average of 1 week (SD = 35 days) following conversion. This promising finding was independent of more than 40 clinical and demographic variables. Moreover, the targets of the participants’ baseline VI were found to be entirely different than those ultimately attacked, perhaps suggesting impulsivity, and loss of executive control with the transition to frank psychosis.
The hypothesis that violence risk may increase as CHR individuals approach conversion to frank psychosis has some independent empirical support. More prominent psychotic symptoms and less insight have been found to increase the risk of violent acts [18, 24, 37]. Moreover, the aforementioned meta-analysis by Nielssen and Large [19] found that 38.5% of homicides committed by individuals with psychotic illness occur during the FEP, prior to first receiving treatment. We know of no reports of a higher prevalence of homicide in the psychosis-risk state. A prior meta-analysis by Fazel et al. [38] also reported that schizophrenia and other psychoses are associated with violence, particularly homicide, and that the relationship between violence (excluding homicide) and psychosis may be largely related to comorbid substance use. However, individual studies considering the temporal relationship between violence and first onset of psychotic symptoms were not examined.
In the present report, we examine the baseline demographic and clinical characteristics of a comparatively large cohort of CHR individuals. Our specific aim was to describe clinical correlates of VI and VB in the 6 months prior to baseline, considering associations with specific signs and symptoms assessed by the SIPS.
Methods
Data were collected at the Center of Prevention and Evaluation (COPE), an outpatient research program for the evaluation and treatment of attenuated positive symptoms at the New York State Psychiatric Institute (NYSPI)/Columbia University Medical Center (CUMC) in New York City. The NYSPI Institutional Review Board approved the research. All adults provided written informed consent, while minors provided written assent, with written informed consent obtained from a parent.
Participants
Potential participants were referred to COPE between 2003 and 2016 by a network of academic centers, private practitioners, clinics, and hospitals, or were self-referred after reviewing the center’s web site, for evaluation of possible emergent psychotic symptoms. Participants were between the ages of 13 and 30 and were required to have symptoms that meet criteria for at least one of the psychosis-risk syndromes delineated in the SIPS (see Supplementary Material for specific definitions). These include the aforementioned APSS, the genetic risk and functional decline syndrome and the brief intermittent psychosis syndrome (BIPS). However, it should be noted that all 200 participants met APSS criteria and none met BIPS criteria. Exclusion criteria included lack of proficiency in English; a current or lifetime DSM psychotic disorder, including affective psychoses; a DSM disorder better accounting for the clinical presentation; I.Q. < 70; medical conditions affecting the central nervous system; marked risk of harm to self or others; unwillingness to participate in research; geographic distance; or a DSM diagnosis of current substance or alcohol abuse or dependence. Use of antipsychotic medication was not exclusionary, provided that there was clear evidence that positive symptoms of an attenuated, but never fully psychoticlevel syndrome were present at medication onset. The study sample is described in Table 1.
Measures
The data presented here were collected at baseline. In addition to a general clinical interview, each participant was also evaluated with either the Diagnostic Interview for Genetic Studies [39] or Structured Clinical Interview for DSM-IV-I Disorders, Patient Edition (SCID-I/P); [40]. Those under age 16 completed the Kiddie Schedule for Affective Disorders and Schizophrenia, Present and Lifetime Version (K-SADS-PL) [41].
The SIPS [42], with which all participants were examined, involves a semistructured interview that probes for past and current signs and symptoms of attenuated versus threshold psychotic illness. It defines criteria for psychosis-risk states, as well as threshold psychosis. The measure contains 19 subscales, divided into positive, negative, disorganization, and general symptom components. The critical items for determining attenuated versus full-blown psychosis, are the five positive symptoms: P.1.: unusual thought content/delusional ideas, P.2.: suspiciousness/persecutory ideas, P.3.: grandiose ideas, P.4.: perceptual abnormalities/hallucinations, and P.5.: disorganized communication. These are scored 0–6 according to specific anchors provided for each symptom that distinguish among degrees of frequency, conviction, and behavioral impact: 0, absent; 1, questionably present; 2, mild; 3, moderate; 4, moderately severe; 5, severe, but not psychotic; and 6, psychotic, delusional conviction, at least intermittently. Negative, disorganization, and general signs and symptoms are rated from 0 (absent) to 6 (extreme) (see Supplementary Material for specific subscales).
APSS criteria, satisfied by all participants described here, require that one or more of the 5 positive symptoms occurs at a score of 3–5 and is new or has worsened by 1 or more points in the past 12 months, and no score of 6 on a positive symptom has ever been achieved. SIPS administrators were certified and established scoring consensus.
Frank psychosis is defined by the SIPS as having met criteria for a score of 6 on one or more positive symptoms in one’s lifetime for at least 1 h per day at an average frequency of 4 days per week over one month, and/or serious danger or disorganization as the result of the positive symptom(s).
VI and VB were coded as “present” or “not present.” Information about VB in the 6 months prior to baseline was amassed via the SIPS, the clinical interview, and collateral information from prior records, family members and referral sources. It was defined as any violent or aggressive act, including those with a deadly weapon, any assault producing injury, threat with a deadly weapon in hand, sexual assault, assault producing no injury (e.g., pushing or slapping), or use of a weapon without threats or injury. These were defined based on the categories for violence and other aggressive acts established in the MacArthur Community Violence Interview [29]. In accord with this framework, assault with no injury was categorized as Other Aggressive Acts (OAA). VI encompassed any violent or aggressive fantasies or thoughts directed toward others, intrusive or nonintrusive, which we categorized by adapting the MacArthur interview framework to score VI at baseline in the same manner as VB and OAA.
Statistical analyses
All statistical analyses were performed using SPSS version 22 [43]. Categorical variables were analyzed using the chi-square test of associations and continuous variables with t-tests. The dependent variables were the presences of either VI or VB. A Fisher’s exact p value was calculated for chi-square analyses with small expected cell counts. For tests failing Levene’s test for equality of variance, a corrected test statistic was calculated.
Results
Violent ideation
Approximately, one-third of the sample presented with VI (n = 65, 32.5%; see Table 2), almost uniformly experienced as ego-dystonic and intrusive in nature. To better understand this, ideational content was divided into the subcategories of “severe” violence and ideation related to OAA. Severe VI was defined as thought content involving serious harm to another person, with or without a weapon. Within this category, 20 respondents reported thoughts or mental images of causing serious harm to another with their fists, feet or other body parts. Eighteen described VI of harming another person with a weapon (including guns, knives, saws, and razors), six reported VI that was sexual in nature (rape and sexual assault), and two described VI involving killing others with bombs. In three cases, VI involved causing the death of another person in an unspecified manner. Four respondents described VI in which they caused both serious injury with a weapon and sexual harm. Two endorsed thoughts and mental images of causing serious harm with a weapon and with fire, and one had thoughts of causing serious sexual harm, as well as harm without a weapon.
Ideation related to OAA involves violence toward another that might not result in serious harm. This group (n = 9) included 8 individuals with VI of shoving, slapping, throwing people a short distance, and/or nonserious hitting. One individual reported minor VI of an unspecified nature.
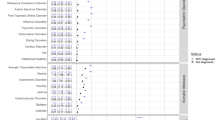
There were no sex or ethnic (i.e., Hispanic vs. non-Hispanic) differences between individuals with and without VI. Interestingly, individuals identifying as Caucasian reported less VI than other racial groups. Those with VI were more likely to have symptoms that met criteria for schizotypal personality disorder (SPD; χ2 (1) = 5.88; p = 0.015), comorbid with the SIPS APSS category, and to report histories of nonsexual trauma (χ2 (1) = 4.93; p = 0.026). Medication status; suicidality, including both suicidal ideation and suicidal behavior; and history of sexual trauma did not distinguish between those with and without VI. Comorbid DSM diagnoses did not significantly differ between those with and without VI.
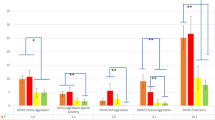
Individuals with VI reported higher degrees of suspiciousness, as well as total overall positive symptoms than those without (see Table 3). A statistical association between VI and SIPS symptom P.1.: unusual thought content/delusional ideas was observed, though this is undoubtedly due to the fact that VI was frequently reported by participants when responding to P.1. inquiries probing for intrusive ideas and a sense of one’s thoughts being out of one’s control.
There was no significant difference in negative symptoms among those with and without VI. Individuals with VI exhibited higher scores for unusual behavior and appearance; more bizarre ideas (e.g., ideas which are not scientifically plausible and are difficult to understand); and higher total disorganization scores. Individuals with VI were also noted to experience more severely dysphoric mood states. Other SIPS symptom subscales were comparable between those with and without VI.
Violent behavior
Evidence and/or self-report of VB in the 6 months preceding baseline were found in less than one-tenth of the sample (n = 17, 8.5%). When present, VB was unrelated to sex, ethnicity, or race. There were no differences in terms of sexual or nonsexual trauma histories, suicidal ideation, suicidal behavior, medication status, or comorbid DSM diagnoses between individuals with and without prebaseline VB. There were no differences between individuals with and without VB with regard to any individual SIPS subscale, or in terms of positive, negative, disorganization, or general symptoms.
Discussion
The present study describes violent behaviors and thoughts reported by 200 young people at clinical high-risk of psychotic illness at the onset of a 2-year longitudinal study. The prospective aspects of the study have been previously described [36]. Here, we explore relationships between violent thoughts at baseline, violent actions in the 6-month period preceding research participation, and psychiatric diagnoses and SIPS interview subscales, advancing our understanding of how psychosis and violence risk may coexist or develop in tandem in certain individuals.
Analyses revealed that thoughts and mental images with violent content, generally experienced as intrusive and ego-dystonic, were common in our sample, occurring in one-third of participants. The content of this ideation was found typically to be severe in nature, involving physical harm to others using one’s body or a weapon. Sexual content was uncommon. Violent thoughts appear to be relatively common in attenuated psychosis. Thus, violent thoughts of this nature may constitute part of the phenomenology of attenuated psychosis, analogous to suicidal thoughts in a significant number of depressed persons. However, actual suicide attempts in depression and violence in the CHR state are far less common. The frequency of VI in our CHR cohort is potentially important: as noted in our previous report, VI was an extremely good predictor in our cohort of both conversion to threshold psychosis and, within an average of seven days (SD = 35 days) postpsychosis onset, violent actions toward others. However, given the potential stigmatization of the already marginalized CHR population, we should emphasize that most individuals in our cohort who described VI never actually progressed to VB. Furthermore, it should be noted that violence among CHR persons may be multidetermined, or entirely unrelated to VI or psychotic symptoms.
Results also indicated that violent thoughts are generally related to overall positive symptoms, and particularly to suspiciousness. A review by Darrell-Berry et al. [44] of 15 studies examining the relationship between paranoia and violence found that, in the most rigorous investigations, a positive association emerged between these factors. It is intriguing, however, that, in our research, VI was virtually never elicited by questions inquiring about suspicious ideas on the SIPS [36]. It is unclear whether this may relate to the wording of suspiciousness inquiries in the SIPS. However, rather than suggest that CHR persons with some degree of paranoia are more likely to harbor violent thoughts, it may be that both suspiciousness and VI are commonly co-occurring, but not necessarily related, manifestations of a nascent psychotic illness in some individuals. The finding that a history of non-sexual trauma is associated with VI has some support in Marshall et al.'s [35] finding that violent content on the SIPS was linked with more incidents of bullying prior to age 16. The findings that, in our cohort, VI was statistically associated with non-Caucasian race and comorbid SPD have no precedent in the CHR literature. Additional research is needed before meaningful interpretations can be ventured.
By contrast, violent actions in the 6-month period preceding baseline were remarkably uncommon, occurring in less than one-tenth of the cohort. Given that information regarding prebaseline violence was dependent on self-report by participants, as well as collateral information from family members and referrers, it is unclear to what degree information about prebaseline violent acts may be underrepresented, although there are reasons to believe that self and collateral report offer more complete data than official records [29].
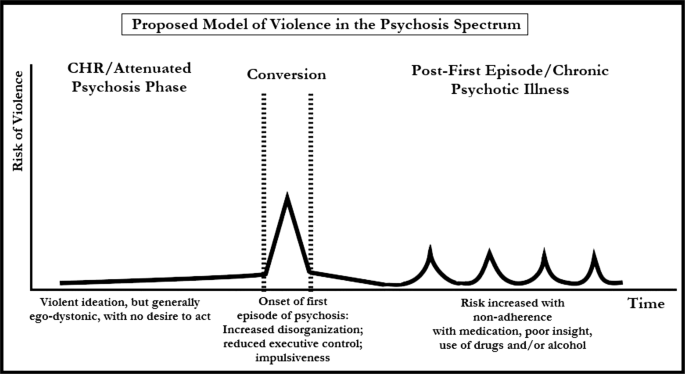
These results demonstrating relationships between VI and positive symptoms are consistent with Marshall et al.’s [35] finding regarding the frequency of violent content in an independent CHR sample, as well as VB in syndromal psychosis [45]. The collective data reveal that individuals with psychotic illness may be at the highest risk for violence around the time of conversion to psychosis through the remission of the FEP. Moreover, some data suggest that periods of intensification of symptoms (e.g., the perihospitalization period) during the chronic state of psychotic illness also represent periods of slightly increased risk for violence, though the risk may not be as high as during the FEP period [29]. Thus, the overall picture, which we have incorporated into a preliminary model (see Fig. 1), suggests that, in the phase of attenuated positive symptoms that generally precedes full-blown psychosis, violent thoughts and mental images are commonly experienced, but are either not acted upon or dismissed as inconsistent with individuals’ actual thoughts and desires. However, such thoughts are strongly associated with later progression to threshold psychosis and subsequent aggression, such that they may constitute critical aspects of assessments of conversion status and violence risk, if independently validated, in future research. Moreover, it is with the conversion to FEP that one is most likely to act out aggressively.
The literature and our research, on balance, suggest that this window of increased risk closes only after the FEP has stabilized, perhaps following a period of treatment. Furthermore, our previously described data tell us that this postconversion aggression is generally unfocused and impulsive in nature, affecting targets other than those initially envisioned by participants in thoughts and mental images [36]. This point is intriguing in light of our finding here that a SIPS index of unusual behavior and appearance was associated with VI in our cohort. The facts may collectively indicate that violence risk is associated with gradual deterioration of executive behavioral controls as one transitions to psychosis. What is unclear is whether the reduced risk after the first episode is related to medications, psychotherapy, the natural progression of the condition, or some other compensatory factor, which warrants further research.
Among the limitations of our research is that it was conducted at a single site, reducing the generalizability of our findings, pending attempts at replication. Generalizability may have also been impacted by the elimination of persons with certain clinical features from our CHR sample; specifically, those whose presentations meet criteria for current substance or alcohol abuse or dependence [26, 33] or who were deemed too clinically acute to participate in research (i.e., at imminent risk of violence and requiring evaluation in the emergency room). These exclusions may have significantly affected reports of both past and current violent thoughts and behaviors. Moreover, excluding individuals with histories of substance or alcohol abuse and/or risk of imminent serious aggression may have reduced the number of participants with symptoms associated with comorbid conduct disorder in childhood or antisocial personality disorder in adulthood, which may also have affected the degree of violence in our population. There is some literature to suggest that a history of delinquent behaviors may increase the likelihood of violence in psychotic illness [32, 45]. Additionally, a very small number of individuals did not complete baseline screening beyond the SIPS, such that we have some missing data. It also unclear to what degree social bias may have led to minimization of reporting of VI and VB. Finally, all participants were voluntarily presenting for treatment, which may distinguish this sample from nonhelp-seeking CHR persons.
However, our sample size of 200 participants is comparatively large, as individuals whose symptoms meet criteria for attenuated psychotic illness are decidedly uncommon. Another strength of the study lies in the inclusion of VI, and not solely VB, in the variables we examined. We believe that our collective findings regarding the frequency of VI in the CHR state and its predictive nature may, with time and additional study, offer a promising new window for research and clinical intervention.
Funding and disclosure
This work was supported by the National Institutes of Health: Center for Research Resources and the National Center for Advancing Translational Sciences (grant numbers UL1TR000040, 2KL2RR024157, K23MH066279, R21MH086125, R01P50MH086385, R01MH093398-01, K23MH106746). This project was supported by the Brain and Behavior Research Foundation; Lieber Center for Schizophrenia Research; and the New York State Office of Mental Health Research Foundation for Mental Hygiene.
References
Fusar-Poli P, Borgwardt S, Bechdolf A, Addington J, Richer-Rossler A, Schultze-Lutter F, et al. The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA Psychiatry. 2013;70:107–20.
Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Cannon T, Ventura J, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 2003;29:703–15.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5 edn. Washington, DC: American Psychiatric Association; 2013.
Addington J, Cadenhead KS, Cannon TD, Cornblatt B, McGlashan TH, Perkins DO, et al. North American Prodromal Longitudinal Study: a collaborative multisite approach to prodromal schizophrenia research. Schizophr Bull. 2007;33:665–72.
Douglas KS, Guy LS, Hart SD. Psychosis as a risk factor for violence to others: a meta-analysis. Psychol Bull. 2009;135:679–706.
Hodgins S, Mednick SA, Brennan PA, Schulsinger F, Engberg M. Mental disorder and crime. Evidence from a Danish birth cohort. Arch Gen Psychiatry. 1996;53:489–96.
Lindqvist P, Allebeck P. Schizophrenia and crime. A longitudinal follow-up of 644 schizophrenics in Stockholm. Br J Psychiatry. 1990;157:345–50.
Swanson JW, Swartz MS, Essock SM, Osher FC, Wagner HR, Goodman LA, et al. The social-environmental context of violent behavior in persons treated for severe mental illness. Am J Public Health. 2002;92:1523–31.
Taylor PJ, Bragado-Jimenez MD. Women, psychosis and violence. Int J Law Psychiatry. 2009;32:56–64.
Coid JW, Ullrich S, Kallis C, Keers R, Barker D, Cowden F, et al. The relationship between delusions and violence: findings from the East London first episode psychosis study. JAMA Psychiatry. 2013;70:465–71.
Keers R, Ullrich S, Destavola BL, Coid JW. Association of violence with emergence of persecutory delusions in untreated schizophrenia. Am J Psychiatry. 2014;171:332–9.
McNiel DE, Eisner JP, Binder RL. The relationship between command hallucinations and violence. Psychiatr Serv. 2000;51:1288–92.
Taylor PJ, Leese M, Williams D, Butwell M, Daly R, Larkin E. Mental disorder and violence. A special (high security) hospital study. Br J Psychiatry. 1998;172:218–26.
Ullrich S, Keers R, Coid JW. Delusions, anger, and serious violence: new findings from the MacArthur Violence Risk Assessment Study. Schizophr Bull. 2014;40:1174–81.
Bartels SJ, Drake RE, Wallach MA, Freeman DH. Characteristic hostility in schizophrenic outpatients. Schizophr Bull. 1991;17:163–71.
Elbogen EB, Van Dorn RA, Swanson JW, Swartz MS, Monahan J. Treatment engagement and violence risk in mental disorders. Br J Psychiatry. 2006;189:354–60.
Yesavage JA. Inpatient violence and the schizophrenic patient: an inverse correlation between danger-related events and neuroleptic levels. Biol Psychiatry. 1982;17:1331–7.
Buckley PF, Hrouda DR, Friedman L, Noffsinger SG, Resnick PJ, Camlin-Shingler K. Insight and its relationship to violent behavior in patients with schizophrenia. Am J Psychiatry. 2004;161:1712–4.
Nielssen O, Large M. Rates of homicide during the first episode of psychosis and after treatment: a systematic review and meta-analysis. Schizophr Bull. 2010;36:702–12.
Eronen M, Tiihonen J, Hakola P. Schizophrenia and homicidal behavior. Schizophr Bull. 1996;22:83–89.
Rasanen P, Tiihonen J, Isohanni M, Rantakallio P, Lehtonen J, Moring J. Schizophrenia, alcohol abuse, and violent behavior: a 26-year followup study of an unselected birth cohort. Schizophr Bull. 1998;24:437–41.
Elbogen EB, Johnson SC. The intricate link between violence and mental disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2009;66:152–61.
Rolin SA, Marino LA, Pope LG, Compton MT, Lee RJ, Rosenfeld B, et al. (2018). Recent violence and legal involvement among young adults with early psychosis enrolled in Coordinated Specialty Care. Early Interv Psychiatry 1–9. E-pub ahead May 9, 2018, https://doi.org/10.1111/eip.12675.
Swartz MS, Swanson JW, Hiday VA, Borum R, Wagner HR, Burns BJ. Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. Am J Psychiatry. 1998;155:226–31.
Arseneault L, Moffitt TE, Caspi A, Taylor PJ, Silva PA. Mental disorders and violence in a total birth cohort: results from the Dunedin Study. Arch Gen Psychiatry. 2000;57:979–86.
Fazel S, Langstrom N, Hjern A, Grann M, Lichtenstein P. Schizophrenia, substance abuse, and violent crime. J Am Med Assoc. 2009b;301:2016–23.
Foley SR, Kelly BD, Clarke M, McTigue O, Gervin M, Kamali M, et al. Incidence and clinical correlates of aggression and violence at presentation in patients with first episode psychosis. Schizophr Res. 2005;72:161–8.
Appelbaum PS, Robbins PC, Monahan J. Violence and delusions: data from the MacArthur Violence Risk Assessment Study. Am J Psychiatry. 2000;157:566–72.
Steadman HJ, Mulvey EP, Monahan J, Robbins PC, Appelbaum PS, Grisso T, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55:393–401.
Chang WC, Chan SS, Hui CL, Chan SK, Lee EH, Chen EY. Prevalence and risk factors for violent behavior in young people presenting with first-episode psychosis in Hong Kong: a 3-year follow-up study. Aust N Z J Psychiatry. 2015;49:914–22.
Langeveld J, Bjørkly S, Auestad B, Barder H, Evensen J, Ten Velden Hegelstad W, et al. Treatment and violent behavior in persons with first episode psychosis during a 10-year prospective follow-up study. Schizophr Res. 2014;156:272–6.
Winsper C, Singh SP, Marwaha S, Amos T, Lester H, Everard L, et al. Pathways to violent behavior during first-episode psychosis: a report from the UK National EDEN Study. JAMA Psychiatry. 2013;70:1287–93.
Witt K, van Dorn R, Fazel S. Risk factors for violence in psychosis: systematic review and meta-regression analysis of 110 studies. PloS ONE. 2013;8:e55942.
Coid JW, Ullrich S, Bebbington P, Fazel S, Keers R. Paranoid ideation and violence: meta-analysis of individual subject data of 7 population surveys. Schizophr Bull. 2016;42:907–15.
Marshall C, Deighton S, Cadenhead KS, Cannon TD, Cornblatt BA, McGlashan TH, et al. The violent content in attenuated psychotic symptoms. Psychiatry Res. 2016;242:61–66.
Brucato G, Appelbaum PS, Lieberman JA, Wall MM, Feng T, Masucci MD, et al. A longitudinal study of violent behavior in a psychosis-risk cohort. Neuropsychopharmacology. 2018;43:264–71.
Arango C, Barba AC, Gonzalez-Salvador T, Ordoriez AC. Violence in inpatients with schizophrenia: a prospective study. Schizophr Bull. 1999;25:493–503.
Fazel S, Gulati G, Linsell L, Geddes JR, Grann M. Schizophrenia and violence: systematic review and meta-analysis. PLoS Med. 2009a;6:e1000120.
Nurnberger JI Jr, Blejar MC, Kaufmann CA, York-Cooler C, Simpson SG, Harkavy-Friedman J, et al. Diagnostic interview for genetic studies. Rationale, unique features, and training. Arch General Psychiatry. 1994;51:849–59.
First MB, Spitzer RL, Gibbon M, Williams JBW (2002). Structured clinical interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P). New York: Biometrics Research, NYSPI.
Kaufman JB, Birmaher D, Brent D, Rao U, Ryan N. Kiddie-Sads-Present and Lifetime Version (K-SADS-PL). Pittsburgh, PA: University of Pittsburgh Department of Psychiatry; 1996.
McGlashan TH, Miller TJ, Woods SW, Hoffman RE, Davidson LA. A scale for the assessment of prodromal symptoms and states. In: Miller TJ, Mednick SA, McGlashan TH, Liberger J, Johannessen JO, (editors). Early Intervention in Psychotic Disorders. Dordrecht, The Netherlands: Kluwer Academic Publishers; 2001. p. 135–49.
IBM Corporation. IBM SPSS Statistics for Windows. 22.0 edn. Armonk, NY: IBM Corporation; 2013.
Darrell-Berry H, Berry K, Bucci S. The relationship between paranoia and aggression in psychosis: a systematic review. Schizophr Res. 2016;172:169–76.
Swanson JW, Swartz MS, Van Dorn RA, Elbogen EB, Wagner HR, Rosenheck RA, et al. A national study of violent behavior in persons with schizophrenia. Arch Gen Psychiatry. 2006;63:490–9.
Acknowledgments
We acknowledge the individuals who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
R.G. acknowledges receiving research support from Otsuka, Allergan/Forest, BioAvantex, and Genentech. J.L. has received support administered through his institution in the form of funding or medication supplies for investigator initiated research from Lilly, Denovo, Biomarin, Novartis, Taisho, Teva, Alkermes, and Boehringer Ingelheim, and is a member of the advisory board of Intracellular Therapies and Pierre Fabre. He neither accepts nor receives any personal financial remuneration for consulting, advisory board or research activities. He holds a patent from Repligen and receives royalty payments from “SHRINKS: The Untold Story of Psychiatry.” The remaining authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Brucato, G., Appelbaum, P.S., Masucci, M.D. et al. Prevalence and phenomenology of violent ideation and behavior among 200 young people at clinical high-risk for psychosis: an emerging model of violence and psychotic illness. Neuropsychopharmacol. 44, 907–914 (2019). https://doi.org/10.1038/s41386-018-0304-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-018-0304-5
This article is cited by
-
Psychometric properties of an Arabic translation of the long (12 items) and short (7 items) forms of the Violent Ideations Scale (VIS) in a non-clinical sample of adolescents
BMC Psychiatry (2024)
-
Feasibility and Utility of Different Approaches to Violence Risk Assessment for Young Adults Receiving Treatment for Early Psychosis
Community Mental Health Journal (2022)
-
Bullying in clinical high risk for psychosis participants from the NAPLS-3 cohort
Social Psychiatry and Psychiatric Epidemiology (2022)
-
The Impact of Increasing Community-Directed State Mental Health Agency Expenditures on Violent Crime
Community Mental Health Journal (2022)